Simple Summary
Cancer increases the risk of venous thrombosis (VTE) and anticoagulant therapy is often used to treat this condition. Therefore, it is essential to identify risk factors for bleeding events in these patients. In our study, we used data from the Rising-VTE/NEJ037 study, which involved Japanese patients with advanced lung cancer, to calculate these risk factors. We found that complications with VTE were the most significant risk factor. This finding underscores the importance of carefully assessing the risks and benefits before starting anticoagulant therapy in patients with cancer. Our research aims to inform safer treatment strategies for patients with advanced lung cancer, which could have meaningful implications for their care and treatment approaches in the research community.
Abstract
Despite the occurrence of various hemorrhagic events during advanced lung cancer treatment, few researchers have reported on their risk factors. Moreover, the development of cancer-related thromboembolism indicates anticoagulant use. However, adverse events such as bleeding should be monitored. In this study, we aimed to identify factors that influence the onset of hemorrhagic events in patients with lung cancer. The Rising-VTE/NEJ037 study was a multicenter, prospective, observational study. A total of 1008 patients with lung cancer who were unsuitable for radical resection or radiation were enrolled and followed up for 2 years. Multivariate analysis using a Cox proportional hazard model was performed to compare the outcomes of the time to the onset of hemorrhagic events for 2 years after registration. Hemorrhagic events occurred in 115 patients (11.4%), with 35 (30.4%) experiencing major bleeding. Significant risk factors included venous thromboembolism (VTE) (hazard ratio [HR]: 4.003, p < 0.001) and an Eastern Cooperative Oncology Group Performance Status score of 1 (HR: 2.476, p < 0.001). Factors that significantly reduced hemorrhagic event risk were female sex (HR: 0.454, p = 0.002) and M1a status (HR: 0.542, p = 0.038). VTE is a risk factor for hemorrhagic events in patients with advanced lung cancer, and risks associated with anticoagulant therapy should be considered.
1. Introduction
Venous thromboembolism (VTE) is a common medical complication in patients with cancer, and the risk of VTE development is 4–20 times greater in patients with cancer than in those without cancer [1,2,3,4,5]. In addition, lung cancer has a high risk of VTE [2]. The incidence of VTE increases with chemotherapy [6,7]. There are also reports that active cancers are associated with VTE in approximately 20% of cases [8,9]. In addition, there are reports that cancer patients with VTE have a worse prognosis and higher mortality rate than those without VTE [7,10]. Anticoagulation therapy is important in the treatment of VTE, but it can cause bleeding side effects, and individual bleeding risks must be considered when using this therapy. Treating venous thromboembolism in patients with cancer is particularly challenging due to the increased risks of both recurrent thrombosis and bleeding compared to patients without cancer [11]. Studies have shown the effectiveness of low-molecular-weight heparin and vitamin K antagonists in managing cancer-associated VTE [11,12,13,14,15]. Additionally, direct oral anticoagulant agents have been reported to be as effective as vitamin K antagonists for treating VTE, with a lower risk of bleeding events [16,17,18]. In the Hokusai VTE cancer trial, of the 522 patients treated with edoxaban for cancer-related VTE, 36 (6.9%) had major bleeding, and 76 (14.6%) had clinically relevant non-major bleeding [19]. We conducted the Rising-VTE/NEJ037 study, a multicenter prospective observational study on patients with lung cancer, and 2 years after enrollment, 9.9% of patients had developed VTE, of which 75% were asymptomatic [20]. The dataset of the Rising-VTE/NEJ037 study was used to analyze the bleeding risk in Japanese patients with advanced lung cancer. In addition, the HAS-BLED and VTE-BLEED scores are known to be indicators of bleeding risk [21,22]. HAS-BLED and VTE-BLEED scores were also calculated to compare existing scoring for bleeding events and identify risk factors in this study.
2. Materials and Methods
This study was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice Guidelines. The study protocol was approved by the Shimane University Institutional Review Board, based on the Clinical Trials Act enacted in Japan in 2017 and published in the Japan Registry of Clinical Trials (jRCTs061180025). Written informed consent was obtained from all patients.
2.1. Patients
Data were collected and examined as part of a multicenter prospective observational study in Japan. The enrolment period of the study was from June 2016 to August 2018. The main enrollment criteria were as follows: patients aged 20 years or older, those with lung cancer for which radical resection or radiation therapy was difficult, those with Eastern Cooperative Oncology Group Performance Status (ECOG PS) scores of 0–3, and those expected to survive for six months or longer. There were no exclusion criteria for case enrollment. Edoxaban, a direct oral anticoagulant, was administered to patients diagnosed with VTE at enrollment [20]. Exclusion criteria for edoxaban administration were patients with hypersensitivity to edoxaban, decreased renal function (creatinine clearance <30 mL/min), liver disease with coagulation abnormalities, and those who have already undergone surgical treatment or treatment for recently diagnosed VTE. If the exclusion criteria for edoxaban administration were met for patients with VTE, anticoagulation therapy was administered at the discretion of the attending physician.
2.2. Bleeding Events
Bleeding events were assessed according to the International Society on Thrombosis and Hemostasis criteria [23]. Clinically evident bleeding that met at least one of the following conditions was considered major bleeding: decrease in hemoglobin level by ≥2 g/dL, transfusion of ≥2 units (500 mL/unit) of packed red blood cells or whole blood, bleeding in critical areas (intracranial bleeding, intraspinal bleeding, intraocular bleeding, pericardial bleeding, intra-articular bleeding, intramuscular bleeding accompanied by compartment syndrome, and retroperitoneal bleeding), and fatal bleeding. Meanwhile, bleeding that did not meet the criteria for major bleeding but was deemed clinically important at the discretion of the attending physician, for example, gastrointestinal bleeding or hemoptysis that does not meet the definition of major bleeding, was considered clinically relevant non-major bleeding. If a bleeding event occurred, treatment was performed at the discretion of each attending physician.
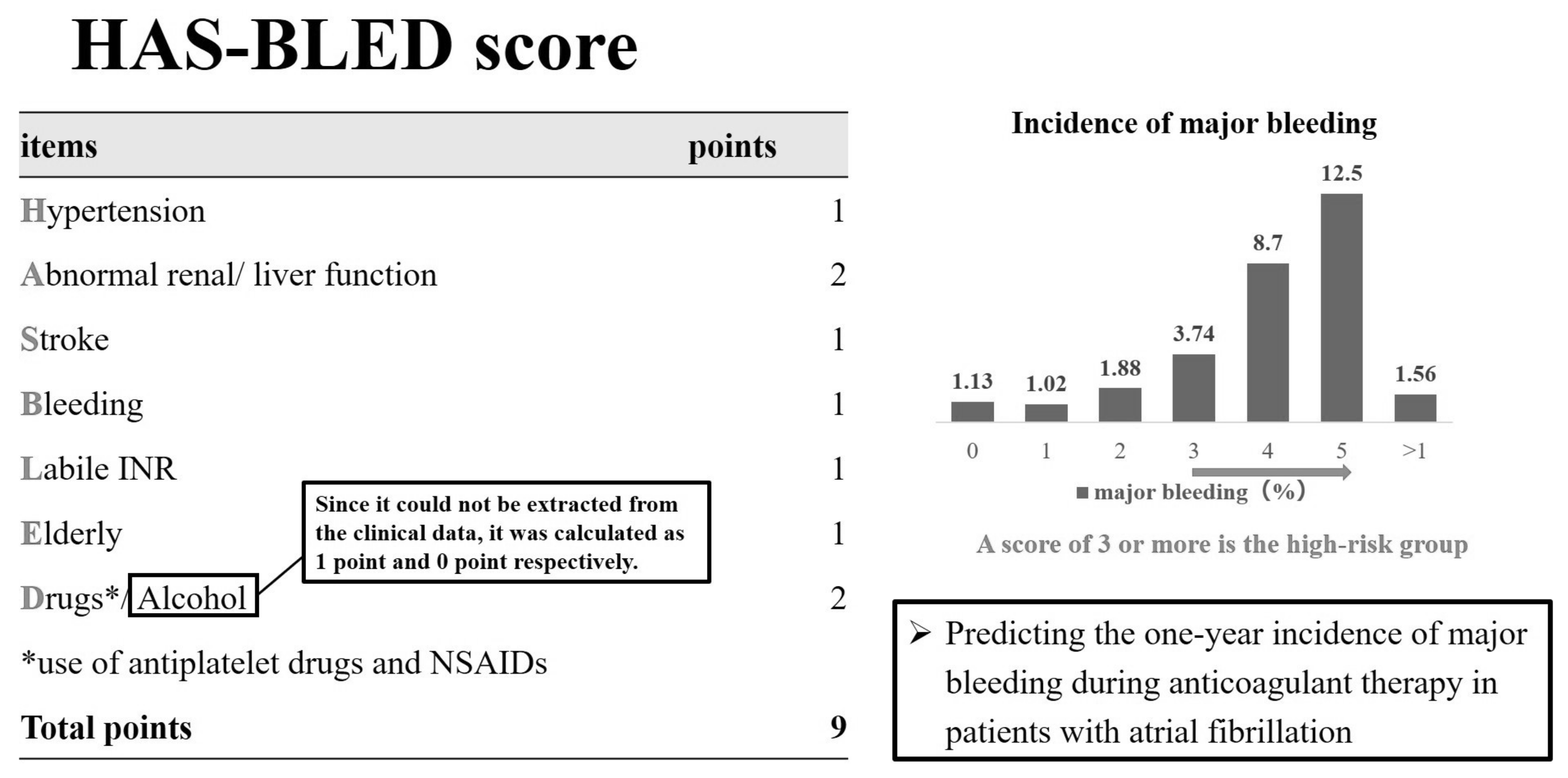
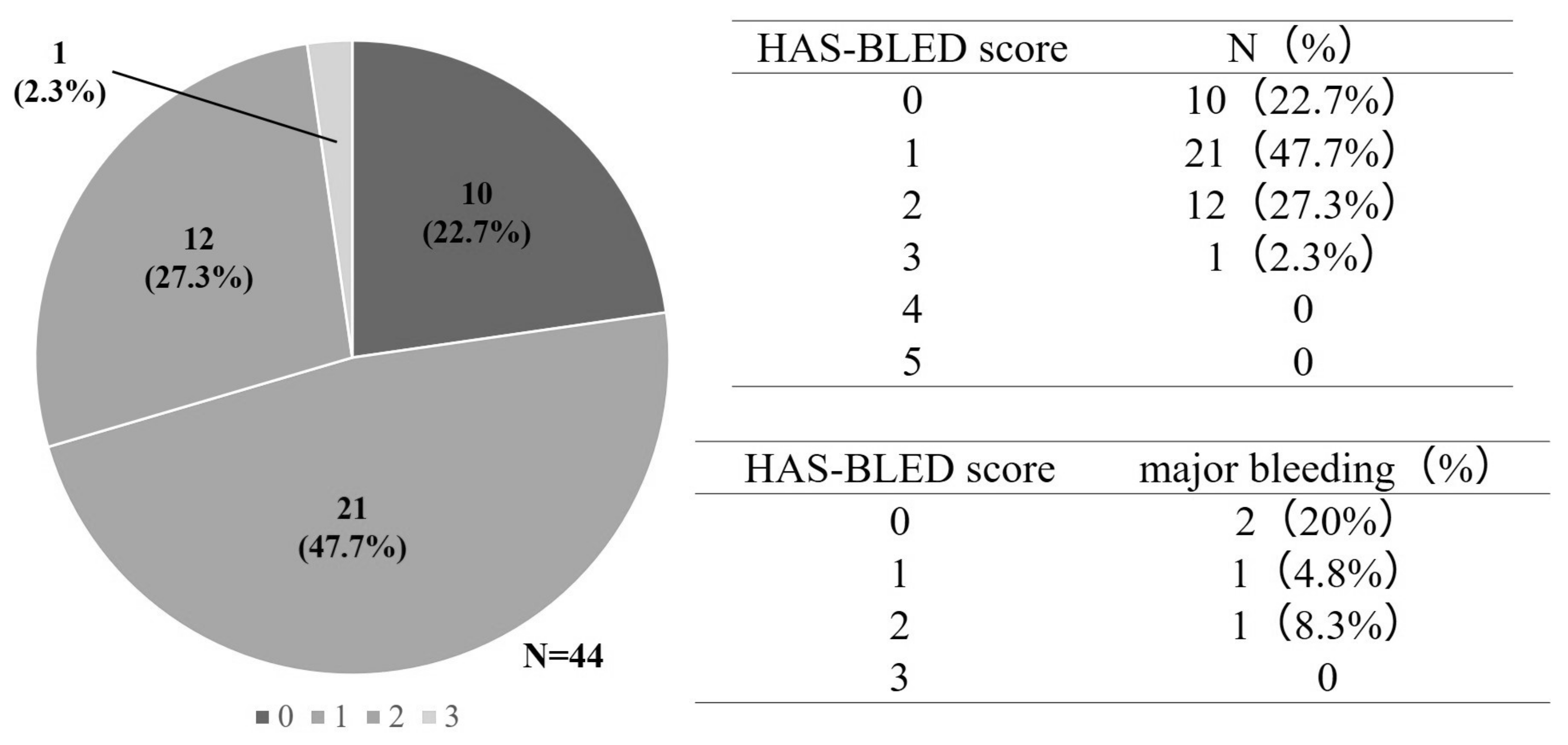
2.3. Hypertension, Abnormal Liver/Renal Function, Stroke History, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly (HAS-BLED) Score
For patients with atrial fibrillation, the HAS-BLED score is known to predict the risk of bleeding side effects during the oral administration of anticoagulants [21]. Abnormal renal/liver function, risk of stroke, bleeding history or predisposition, labile international normalized ratio, old age (>65 years), and drug/alcohol use are used to predict the risk of developing a major bleeding event, with a maximum of nine points. The incidence rates of major bleeding events for these factors were 1.1%, 1.0%, 1.9%, 3.7%, 8.7%, and 12.5%, respectively (range: 0–5 points), and patients with a score of ≥3 were regarded as having a high risk for major bleeding events. To compare the risk of bleeding due to edoxaban and that associated with lung cancer, we used the HAS-BLED score, which has been validated in patients with atrial fibrillation. The history of HAS-BLED events or predisposition, labile international normalized ratio, age (>65 years), and drug/alcohol use were calculated using data from the Rising-VTE/NEJ037 study. In this study, for the edoxaban group, we were unable to calculate the history of alcohol. Therefore, alcohol history was calculated as 1 point and 0 points (Figure 1).
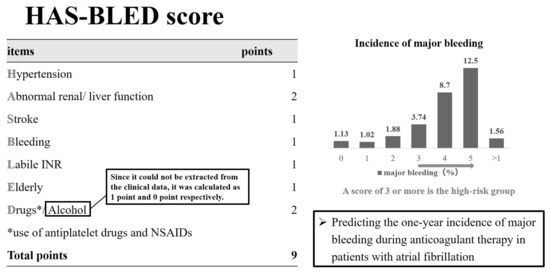
Figure 1.
Hypertension, abnormal liver/renal function, stroke history, bleeding (HAS-BLED) score.
2.4. Venous Thromboembolic Disease and Bleeding (VTE-BLEED) Score
According to the VTE-BLEED score, all the patients fell under the high-risk group because all cases registered in this study were active cancers [22]. Therefore, only the HAS-BLED scores were used in this study.
2.5. Statistical Analyses
Data from the Rising-VTE/NEJ037 dataset were subjected to multivariate analysis using the Cox proportional hazards model with “the time to onset of a bleeding event” as the outcome. All statistical analyses were performed using SPSS Statistics version 24.0 (IBM Japan, Ltd., Tokyo, Japan). We used the Cox proportional hazards model to examine the risk of bleeding in Japanese patients with advanced lung cancer. p values < 0.05 were considered to be statistically significant.
3. Results
3.1. Patients’ Characteristics and Bleeding Events
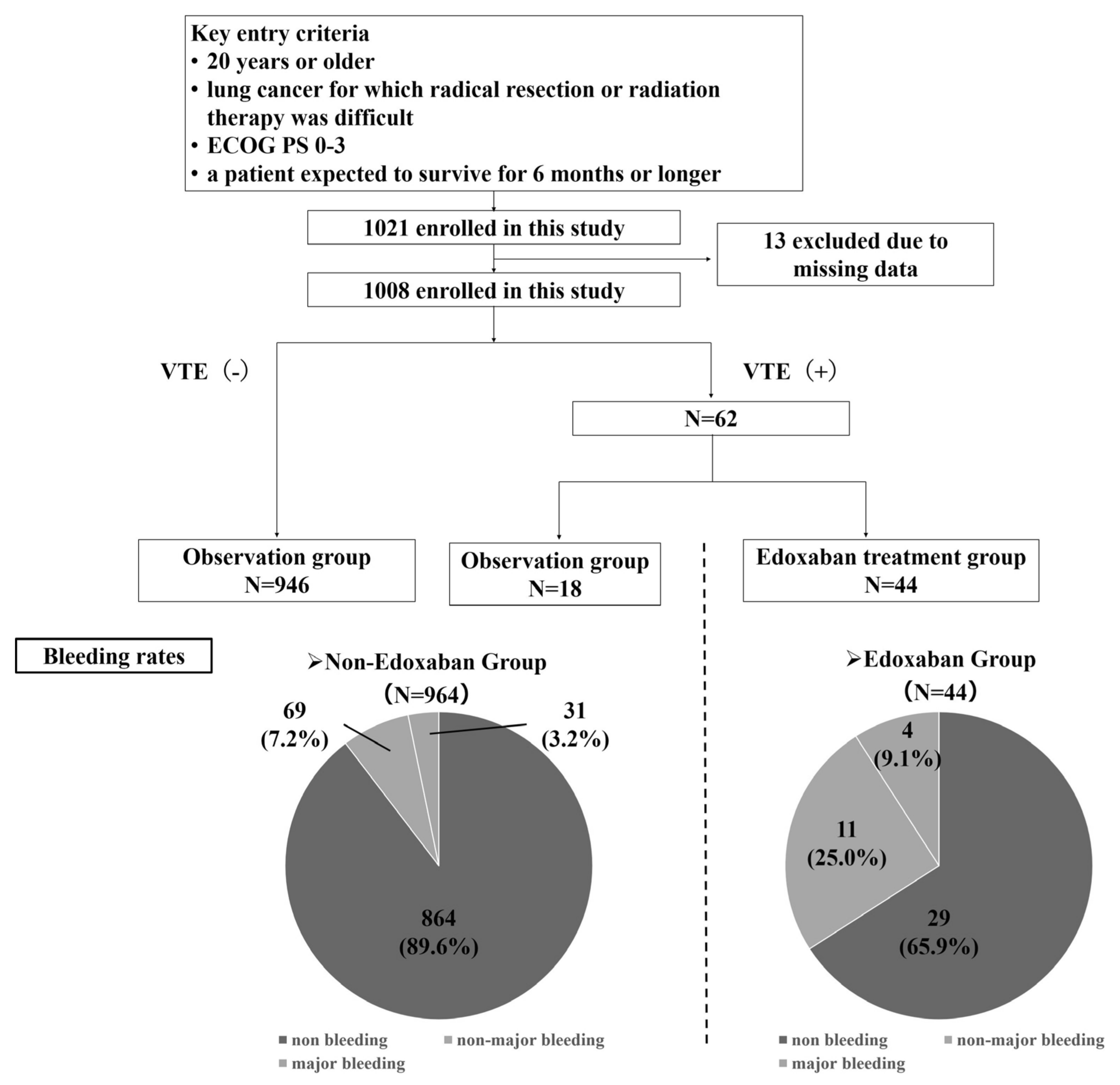
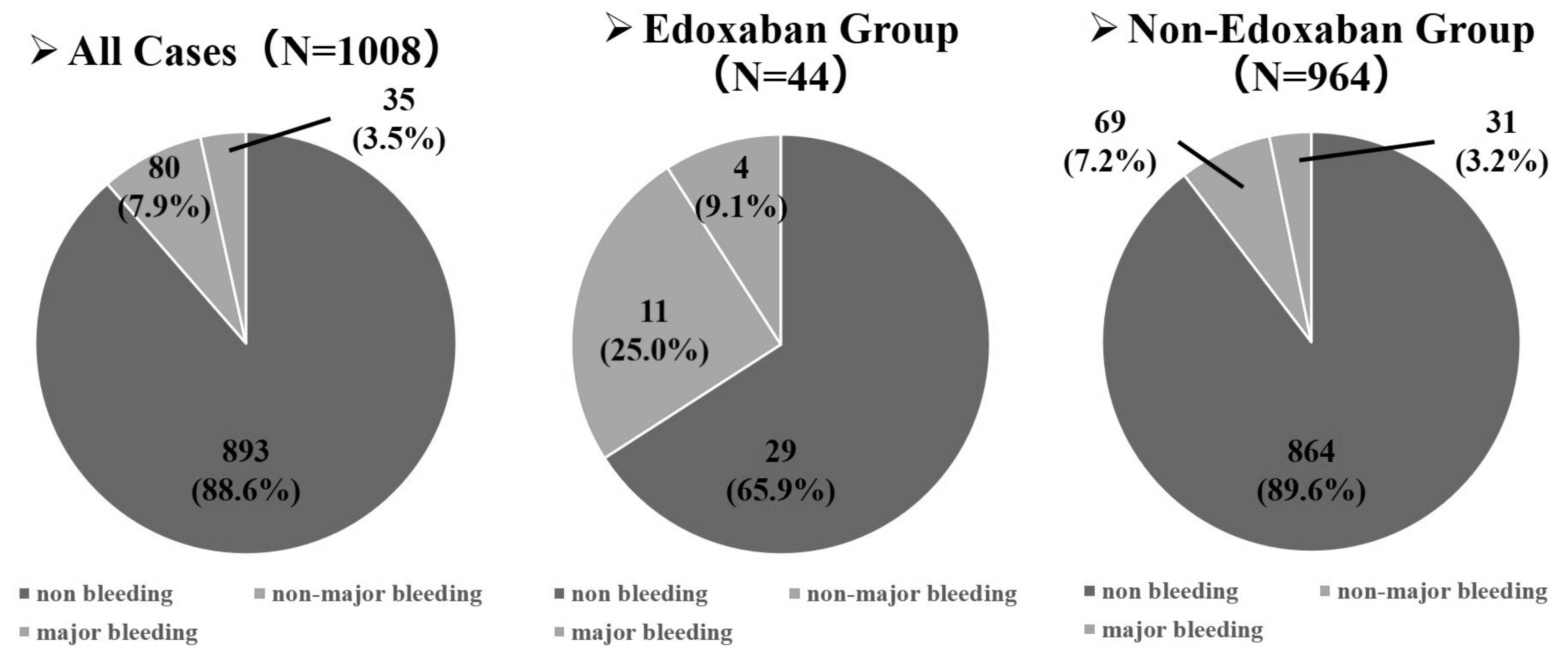
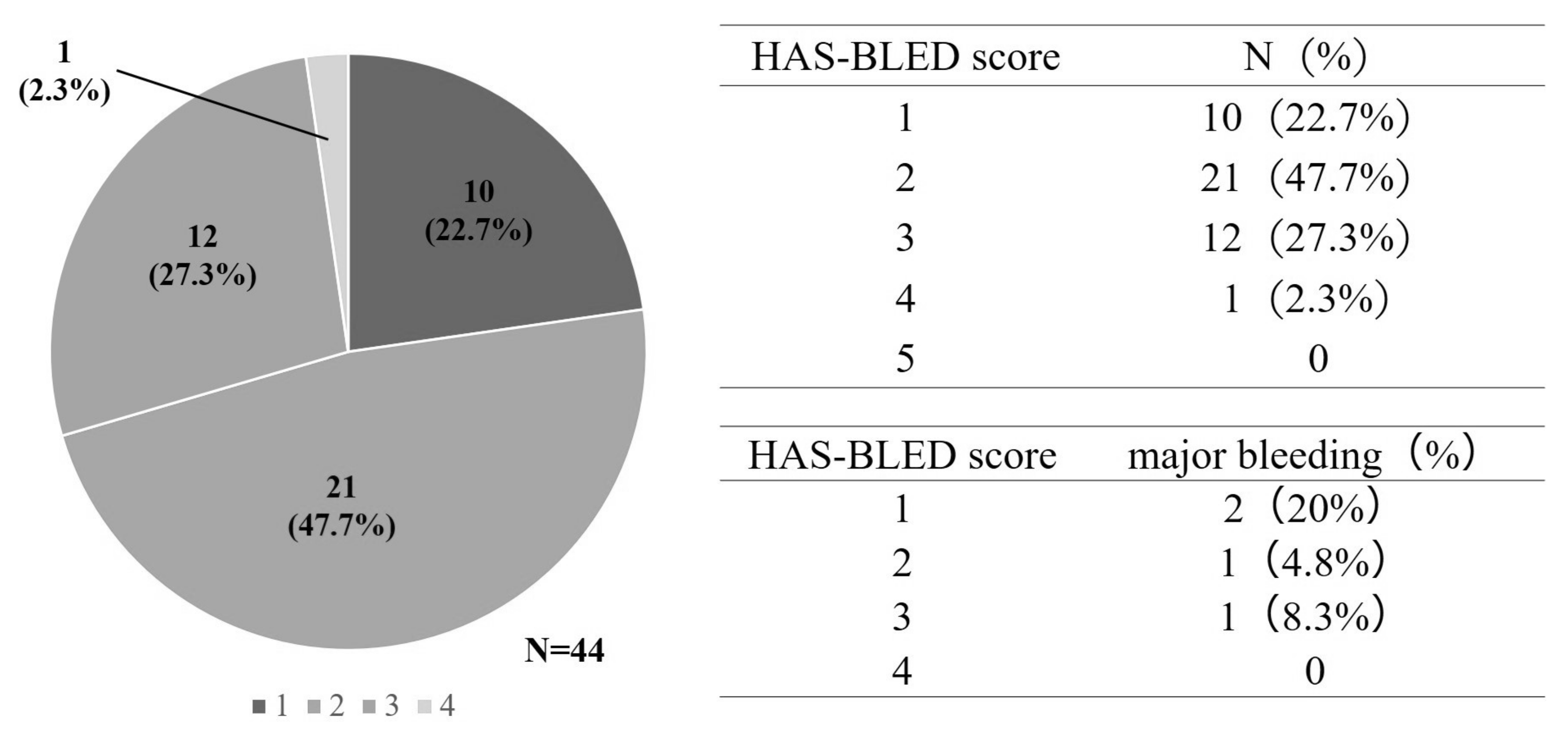
A total of 1021 patients were enrolled from 35 Japanese hospitals, and 13 were excluded due to missing data. Finally, 1008 patients were included. The median age of the enrolled patients was 70 (range, 30–94) years, and most were male (714 patients, 70.8%) and had good ECOG PS (0–1, 80.6%). The most common histological subtype of lung cancer was adenocarcinoma (641 patients, 63.6%). Disease stage was assessed according to the Union for International Cancer Control, 7th edition, tumor-node-metastasis staging system for lung cancer [24]; M1a, b stage IV disease accounted for 80% of all cases [11]. At the initial diagnosis, 62 patients had VTE, of which 44 were treated with edoxaban (Figure 2). Further, 115 (11.4%) had bleeding events: 80 were non-major bleeding events, and 35 were major bleeding events. In the group that had VTE and received edoxaban treatment (44 patients), bleeding events occurred in 15 patients, with major bleeding events in four. Of the 964 patients who did not receive edoxaban, bleeding events occurred in 100 (10.4%). Major bleeding events occurred in 31 patients (Figure 3).
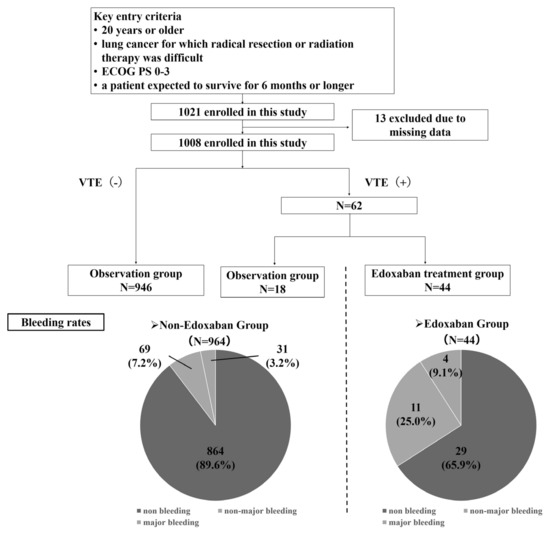
Figure 2.
Cluster classification for venous thromboembolism (VTE) screening.
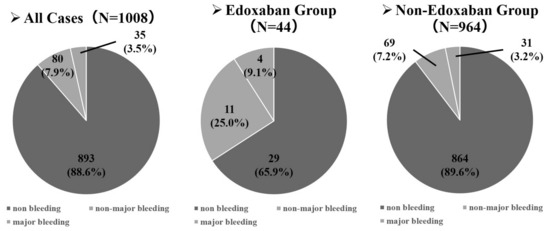
Figure 3.
The rates of bleeding events and major bleeding events.
Patient characteristics between the groups with and without bleeding/hemorrhagic events (Table 1). In the group with bleeding events, the proportion of males was slightly greater, proportion of patients with ECOG PS 1 score was higher, and proportion of patients with squamous cell carcinoma was higher. Additionally, complications of atrial fibrillation and history of anticoagulant use were slightly more common in the group with bleeding events.

Table 1.
Patient characteristics in groups with and without bleeding/hemorrhagic events.
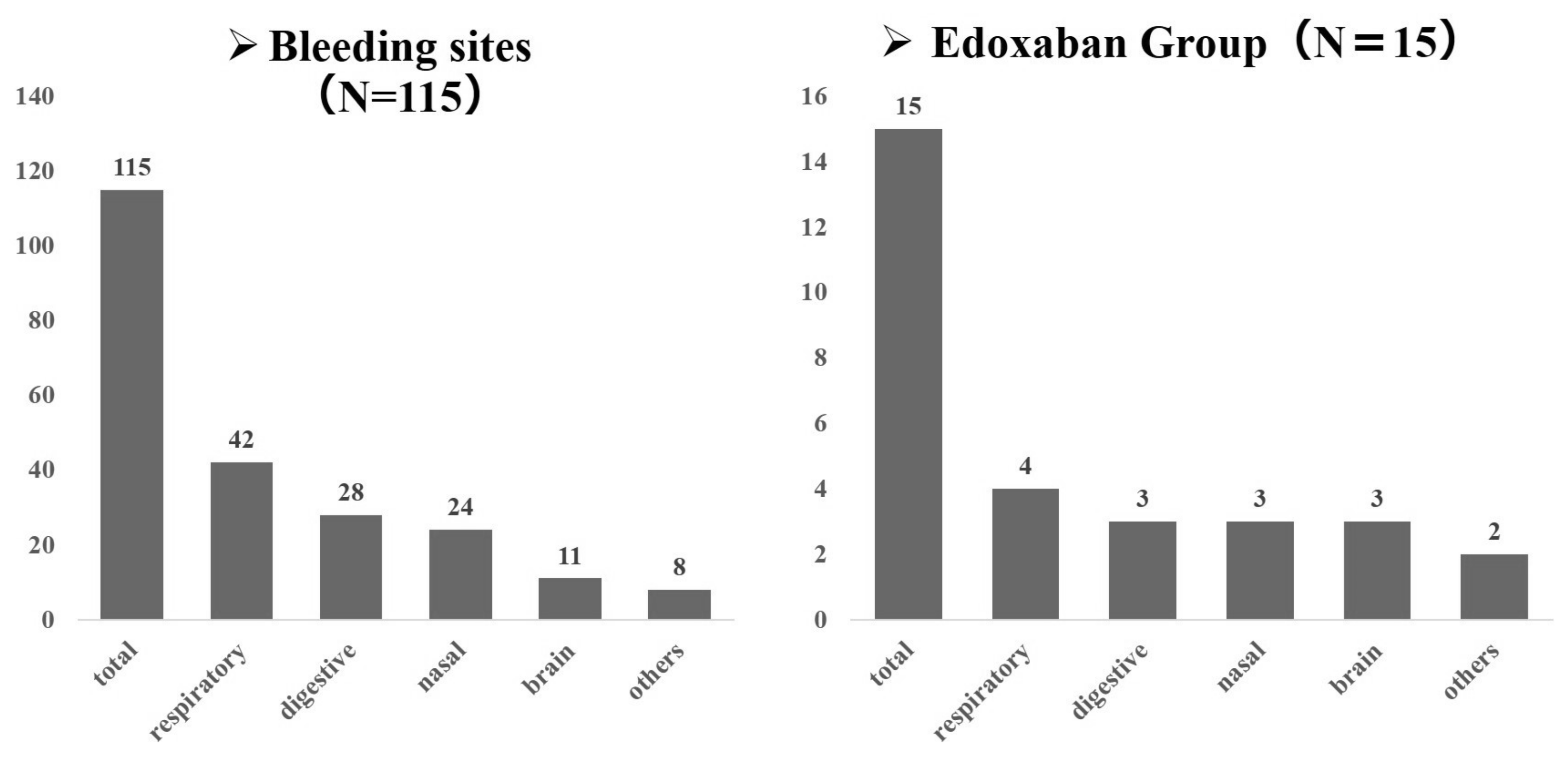
3.2. Bleeding Site
The most common site of bleeding was the respiratory system, as observed in 42 of 115 patients. The gastrointestinal system was the next most frequent site, followed by the nose. The distribution of bleeding sites was uniform in the edoxaban group (Figure 4).
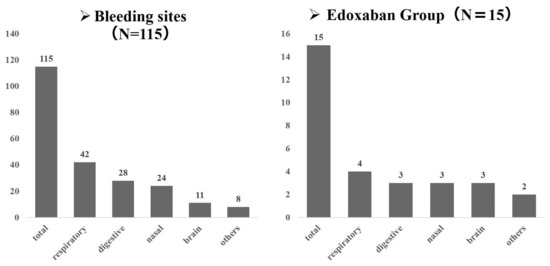
Figure 4.
The distribution of bleeding sites.
3.3. Multivariate Analysis
We performed multivariate analysis using the Cox proportional hazards model with the time to the onset of a bleeding event as the outcome (Table 2). The factors that significantly increased the risk of hemorrhagic events were VTE and an ECOG PS of 1. The factors that significantly reduced the risk of hemorrhagic events were female sex and pleural dissemination (M1a). In particular, among patients with VTE, the hazard ratio for hemorrhagic events was as high as 4.003.

Table 2.
Results of the multivariate analysis of factors influencing bleeding events in patients with lung cancer.
3.4. HAS-BLED Score
Edoxaban was administered only to patients with no previous history of anticoagulant therapy. As the treatment of atrial fibrillation included anticoagulant therapy, it can be inferred that no patients in the edoxaban group had atrial fibrillation.
When drinking history was set at 0 points, the HAS-BLED score was 0 points for 10 patients, 1 point for 21 patients, 2 points for 12 patients, and 3 points for one patient. Only one patient in the edoxaban group had a HAS-BLED score ≥3 points. Major bleeding events occurred in two patients at 0 points, one patient at 1 point, and one patient at 2 points (Figure 5). When drinking history was set at 1 point, the HAS-BLED score was 1 point for 10 patients, 2 points for 21 patients, 3 points for 12 patients, and 4 points for one patient. There was only one patient with a HAS-BLED score of ≥4 points in the edoxaban group. Major bleeding events occurred in two patients at 1 point, one patient at 2 points, and one patient at 3 points (Figure 6).
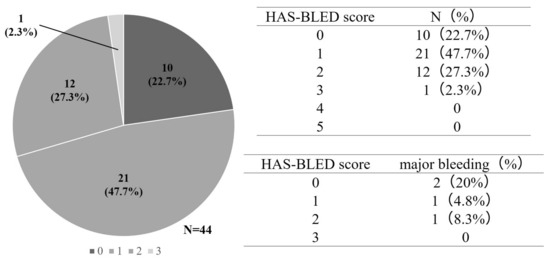
Figure 5.
Hypertension, abnormal liver/renal function, stroke history, bleeding history or predisposition, labile INR, elderly, drugs/alcohol concomitantly.
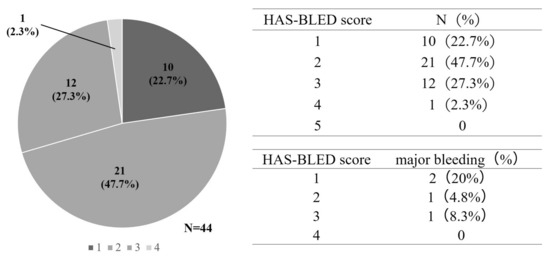
Figure 6.
Hypertension, abnormal liver/renal function, stroke history, bleeding (HAS-BLED) scores when drinking history is set at 0 point (A) and when drinking history is set at 1 point.
4. Discussion
The Rising-VTE/NEJ037 study is one of the largest prospective observational studies of venous thrombosis and hemorrhagic events in Japanese patients with advanced lung cancer. Using the results of the Rising-VTE/NEJ037 study, we performed a post hoc analysis to evaluate the risk factors for bleeding events in Japanese patients with advanced lung cancer. To our knowledge, our study is the first to analyze the risk factors for bleeding events in patients with advanced lung cancer using large-scale data from a prospective observational study. In the Rising-VTE/NEJ037 study, the median overall survival was 24.0 months (95% confidence interval [CI]: 16.8–not estimable) in the group complicated by VTE and treated with edoxaban and 19.2 months (95% CI: 16.8–21.6) in the observation group, indicating no significant difference in survival time (p = 0.793) among the two groups [20]. This indicates that VTE treatment may contribute to improving the prognosis of patients with advanced lung cancer; it is crucial to consider the risks versus benefits of bleeding events and to administer the treatment with due caution.
Studies have shown that cancer patients are more prone to bleeding events compared to non-cancer patients [25,26,27]. Identifying risk factors for these bleeding events in cancer patients is paramount. VTE complications were found to be the largest risk factor for bleeding events in Japanese patients with advanced lung cancer. In addition, female sex and M1a status were associated with a reduction in bleeding events. Further, 44 of the 62 patients with VTE were taking edoxaban, which may have been a significant risk factor for bleeding events.
A high bleeding rate was observed in the group with a HAS-BLED score of ≤2, which was a low-risk group, suggesting that VTE complicating advanced lung cancer is a bleeding risk factor. Active cancer was reported to be a major predictor of recurrent VTE and bleeding [28]. A previous report examined the incidence of VTE and risk factors for bleeding events across cancer types and reported that the VTE complication rate for patients with solid tumors was 5.9% and that VTE complication was a risk factor for increased bleeding events in the multivariate analysis, similar to the results of our study (hazard ratio [HR], 2.39; 95% confidence interval [CI], 1.32–4.31; p = 0.004) [28]. Lung cancer was also listed as a risk factor for increased bleeding events (HR, 1.77; 95% CI, 1.01–3.11; p = 0.046) [29]. Cancer and VTE are diseases that are presumed to have already developed coagulation system abnormalities, which are expected to increase the risk of bleeding; however, the detailed underlying mechanism remains unknown. ECOG PS 1 is another factor that increases the risk of bleeding, and we considered the possibility that more bleeding events occurred in the symptomatic patient population than in patients with ECOG PS 0. Furthermore, in this study, no patients had platelet counts <20,000 at the time of enrollment, and no cases required platelet transfusions owing to chemotherapy. Therefore, it was considered that low platelets were unlikely to be a risk factor for bleeding events.
Conversely, the factors that reduced bleeding events were female sex and pleural dissemination (M1a), possibly because of the lower prevalence of smoking in women. Regarding the group with pleural dissemination (M1a), it is thought that the risk of bleeding events was reduced because distant metastasis was not likely to be involved in the pulmonary/bronchial expenditure of blood, which is a concern for bleeding events in lung cancer.
Limitations
This study had some limitations. First, this study investigated the risk factors for bleeding events in Japanese patients with advanced lung cancer; however, the underlying mechanisms are unknown. Therefore, we are currently conducting studies to elucidate the mechanisms involved in thrombus formation and bleeding. Second, this bleeding risk was internally validated in patients enrolled in the Rising-VTE/NEJ037 study, however, external validity was not demonstrated. Third, all patients enrolled in this study were Japanese, and whether this risk factor is the same for other ethnicities is unclear. In addition, it is known that Japanese people generally have a high rate of driver gene mutations for lung cancer; therefore, the bleeding tendencies of Japanese patients may be different from those of patients of other ethnicities. Fourth, a large proportion of patients with VTE were treated with edoxaban, and we strongly believe that VTE complications mostly contributed to the bleeding events, although edoxaban may also have contributed. Fifth, although there has been research on the pharmacokinetics of edoxaban in EGFR gene mutation-positive patients using some of the patients enrolled in the Rising-VTE/NEJ037 study [30], measuring pharmacokinetics and blood levels in all patients was not possible. Future large-scale, multi-center, longitudinal studies with diverse population samples should be conducted in real-world settings and with standardized scales to confirm the generalizability of our findings and to add to the evidence database to extract valuable results. We are currently preparing a prospective study for external validation; we also aim to evaluate the risk factors for bleeding events.
5. Conclusions
In Japanese patients with advanced lung cancer, complications with VTE were observed to increase the risk of bleeding the most. Anticoagulant therapy is sometimes performed for patients with advanced lung cancer complicated by VTE; however, the indication for treatment must be determined after fully considering the risk of bleeding. In the future, we would like to consider creating a scoring system for bleeding risk when using anticoagulant therapy for patients with advanced lung cancer.
Author Contributions
Conceptualization, K.K. (Keita Kawakado) and Y.T.; methodology, K.K. (Keita Kawakado) and Y.T.; investigation, K.K. (Keita Kawakado) and Y.T.; resources, K.K. (Keita Kawakado), Y.T., T.H., M.Y., N.I., K.F., T.K., K.K. (Kunihiko Kobayashi) and T.I.; data curation, K.K. (Keita Kawakado) and Y.T.; writing—original draft preparation, K.K. (Keita Kawakado); writing—review and editing, K.K. (Keita Kawakado), Y.T., T.H., M.Y., N.I., K.F., T.K., K.K. (Kunihiko Kobayashi) and T.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Daiichi Sankyo Co., Ltd. [LIXMD-15003].
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Shimane University (protocol code 2015 and date of approval was 30 November 2015), based on the Clinical Trials Act enacted in Japan in 2017.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data availability is restricted due to privacy and ethical restrictions.
Acknowledgments
We thank all our patients and their families and all the site investigators for their cooperation. We also thank Hiroyuki Kuroda and Megumi Nakamura for organizing the Image Assessment Committee and Takashi Yoshioka and Teruhisa Azuma for organizing the Safety Monitoring Committee.
Conflicts of Interest
Tsubata was supported by Daiichi Sankyo Co., Ltd. The other authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Key, N.S.; Khorana, A.A.; Kuderer, N.M.; Bohlke, K.; Lee, A.Y.Y.; Arcelus, J.I.; Wong, S.L.; Balaban, E.P.; Flowers, C.R.; Francis, C.W.; et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2020, 38, 496–520. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.A.; Francis, C.W.; Culakova, E.; Kuderer, N.M.; Lyman, G.H. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J. Thromb. Haemost. 2007, 5, 632–634. [Google Scholar] [CrossRef] [PubMed]
- Timp, J.F.; Braekkan, S.K.; Versteeg, H.H.; Cannegieter, S.C. Epidemiology of cancer-associated venous thrombosis. Blood 2013, 122, 1712–1723. [Google Scholar] [CrossRef] [PubMed]
- Ay, C.; Pabinger, I.; Cohen, A.T. Cancer-associated venous thromboembolism: Burden, mechanisms, and management. Thromb. Haemost. 2017, 117, 219–230. [Google Scholar] [CrossRef]
- Elyamany, G.; Alzahrani, A.M.; Bukhary, E. Cancer-associated thrombosis: An overview. Clin. Med. Insights Oncol. 2014, 8, 129–137. [Google Scholar] [CrossRef]
- Moore, R.A.; Adel, N.; Riedel, E.; Bhutani, M.; Feldman, D.R.; Tabbara, N.E.; Soff, G.; Parameswaran, R.; Hassoun, H. High incidence of thromboembolic events in patients treated with cisplatin-based chemotherapy: A large retrospective analysis. J. Clin. Oncol. 2011, 29, 3466–3473. [Google Scholar] [CrossRef]
- Fernandes, C.J.; Morinaga, L.T.K.; Alves, J.L.; Castro, M.A.; Calderaro, D.; Jardim, C.V.P.; Souza, R. Cancer-associated thrombosis: The when, how and why. Eur. Respir. Rev. 2019, 28, 180119. [Google Scholar] [CrossRef]
- Heit, J.A.; Spencer, F.A.; White, R.H. The epidemiology of venous thromboembolism. J. Thromb. Thrombolysis 2016, 41, 3–14. [Google Scholar] [CrossRef]
- Laporte, S.; Mismetti, P.; Décousus, H.; Uresandi, F.; Otero, R.; Lobo, J.L. Clinical predictors for fatal pulmonary embolism in 15,520 patients with venous thromboembolism: Findings from the Registro Informatizado de la Enfermedad TromboEmbolica venosa (RIETE). Regist. Circ. 2008, 117, 1711–1716. [Google Scholar] [CrossRef]
- Qi, Y.; Hu, X.; Chen, J.; Ying, X.; Shi, Y. The risk factors of VTE and survival prognosis of patients with malignant cancer: Implication for nursing and treatment. Clin. Appl. Thromb. Hemost. 2020, 26, 1076029620971053. [Google Scholar] [CrossRef]
- Farge, D.; Debourdeau, P.; Beckers, M.; Baglin, C.; Bauersachs, R.M.; Brenner, B.; Brilhante, D.; Falanga, A.; Gerotzafias, G.T.; Büller, H.R.; et al. International clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. J. Thromb. Haemost. 2013, 11, 56–70. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y.; Levine, M.N.; Baker, R.I.; Bowden, C.; Kakkar, A.K.; Prins, M.; Rickles, F.R.; Julian, J.A.; Haley, S.; Kovacs, M.J.; et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N. Engl. J. Med. 2003, 349, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.Y.Y.; Kamphuisen, P.W.; Meyer, G.; Bauersachs, R.; Janas, M.S.; Jarner, M.F.; Khorana, A.A. CATCH Investigators. Tinzaparin vs warfarin for treatment of acute venous thromboembolism in patients with active cancer: A randomized clinical trial. JAMA 2015, 314, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Bohlke, K.; Falanga, A.; American Society of Clinical Oncology. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J. Oncol. Pract. 2015, 11, e442–e444. [Google Scholar] [CrossRef] [PubMed]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef] [PubMed]
- Van Es, N.; Coppens, M.; Schulman, S.; Middeldorp, S.; Büller, H.R. Direct oral anticoagulants compared with vitamin K antagonists for acute venous thromboembolism: Evidence from phase 3 trials. Blood 2014, 124, 1968–1975. [Google Scholar] [CrossRef] [PubMed]
- Bleker, S.M.A.; Brekelmans, M.P.A.; Eerenberg, E.S.; Cohen, A.T.; Middeldorp, S.; Raskob, G.; Büller, H.R. Clinical impact of major bleeding in patients with venous thromboembolism treated with factor Xa inhibitors or vitamin K antagonists: An individual patient data meta-analysis. Thromb. Haemost. 2017, 117, 1944–1951. [Google Scholar] [PubMed]
- Stefano, B.; Elisa, R.; Dimitriy, A.; Valeria, C.; Alessandra, M.; Afroditi, A.; Maria, D.G.; Cinzia, C.; Marco, M.; Mariano, C. Risk and Management of Bleeding Complications with Direct Oral Anticoagulants in Patients with Atrial Fibrillation and Venous Thromboembolism: A Narrative Review. Adv. Ther. 2023, 40, 41–66. [Google Scholar]
- Raskob, G.E.; van Es, N.; Verhamme, P.; Carrier, M.; Di Nisio, M.; Garcia, D.; Grosso, M.A.; Kakkar, A.K.; Kovacs, M.J.; Mercuri, M.F.; et al. Edoxaban for the treatment of cancer-associated venous thromboembolism. N. Engl. J. Med. 2018, 378, 615–624. [Google Scholar] [CrossRef]
- Tsubata, Y.; Hotta, T.; Hamai, K.; Furuya, N.; Yokoyama, T.; Saito, R.; Nakamura, A.; Masuda, T.; Hamaguchi, M.; Kuyama, S.; et al. Incidence of venous thromboembolism in advanced lung cancer and efficacy and safety of direct oral anticoagulants: A multicenter, prospective, observational study (Rising-VTE/NEJ037 study). Ther. Adv. Med. Oncol. 2022, 14, 17588359221110171. [Google Scholar] [CrossRef]
- Pisters, R.; Lane, D.A.; Nieuwlaat, R.; de Vos, C.B.; Crijns, H.J.; Lip, G.Y. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The euro Heart Survey. Chest 2010, 138, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; Hösel, V.; Clemens, A.; Yollo, W.D.; Tilke, C.; Schulman, S.; Lankeit, M.; Konstantinides, S.V. Prediction of bleeding events in patients with venous thromboembolism on stable anticoagulation treatment. Eur. Respir. J. 2016, 48, 1369–1376. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.A.; O’Connell, C.; Agnelli, G.; Liebman, H.A.; Lee, A.Y.; Subcommittee on Hemostasis and Malignancy of the SSC of the ISTH. Incidental venous thromboembolism in oncology patients. J. Thromb. Haemost. 2012, 10, 2602–2604. [Google Scholar] [CrossRef] [PubMed]
- Goldstraw, P.; Crowley, J.; Chansky, K.; Giroux, D.J.; Groome, P.A.; Rami-Porta, R.; Postmus, P.E.; Rusch, V.; Sobin, L.; International Association for the Study of Lung Cancer International Staging Committee; et al. The IASLC Lung Cancer Staging Project: Proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J. Thorac. Oncol. 2007, 2, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; Huisman, M.V. How I assess and manage the risk of bleeding in patients treated for venous thromboembolism. Blood 2020, 135, 724–734. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, C.; Escalante, C.P.; Goldhaber, S.Z.; McBane, R.; Connors, J.M.; Raskob, G.E. Treatment of Cancer-Associated Venous Thromboembolism with Low-Molecular-Weight Heparin or Direct Oral Anticoagulants: Patient Selection, Controversies, and Caveats. Oncologist 2021, 26, e8–e16. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Carrier, M.; Ay, C.; Di Nisio, M.; Hicks, L.K.; Khorana, A.A.; Leavitt, A.D.; Lee, A.Y.Y.; Macbeth, F.; Morgan, R.L.; et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: Prevention and treatment in patients with cancer. Blood Adv. 2021, 5, 927–974. [Google Scholar] [CrossRef] [PubMed]
- Chee, C.E.; Ashrani, A.A.; Marks, R.S.; Petterson, T.M.; Bailey, K.R.; Melton, L.J., 3rd; Heit, J.A. Predictors of venous thromboembolism recurrence and bleeding among active cancer patients: A population-based cohort study. Blood 2014, 123, 3972–3978. [Google Scholar] [CrossRef]
- Ohashi, Y.; Ikeda, M.; Kunitoh, H.; Sasako, M.; Okusaka, T.; Mukai, H.; Fujiwara, K.; Nakamura, M.; Oba, M.S.; Kimura, T.; et al. One-year incidence of venous thromboembolism, bleeding, and death in patients with solid tumors newly initiating cancer treatment: Results from the Cancer-VTE Registry. Thromb. Res. 2022, 213, 203–213. [Google Scholar] [CrossRef]
- Hotta, T.; Tsubata, Y.; Hamai, K.; Tanino, A.; Kobayashi, M.; Nakamura, A.; Sugisaka, J.; Hongoh, M.; Ishihara, N.; Ishikawa, N.; et al. Pharmacokinetics of edoxaban in EGFR-mutated non-small cell lung cancer patients with venous thromboembolism. Respir. Investig. 2021, 59, 327–334. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).