Late Local Recurrence after Neoadjuvant Therapy and Radical Resection for Locally Advanced Rectal Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Patient Population
2.2. Neoadjuvant Radiochemotherapy
2.3. Surgery
2.4. Local Recurrence
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Bujko, K.; Nowacki, M.P.; Nasierowska-Guttmejer, A.; Michalski, W.; Bębenek, M.; Pudełko, M.; Kryj, M.; Olędzki, J.; Szmeja, J.; Słuszniak, J.; et al. Sphincter Preservation Following Preoperative Radiotherapy for Rectal Cancer: Report of a Randomised Trial Comparing Short-Term Radiotherapy vs. Conventionally Fractionated Radiochemotherapy. Radiother. Oncol. 2004, 72, 15–24. [Google Scholar] [CrossRef]
- Sauer, R.; Becker, H.; Hohenberger, W.; Rödel, C.; Wittekind, C.; Fietkau, R.; Martus, P.; Tschmelitsch, J.; Hager, E.; Hess, C.F.; et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N. Engl. J. Med. 2004, 21, 1731–1740. [Google Scholar] [CrossRef] [PubMed]
- Ding, P.; Liska, D.; Tang, P.; Shia, J.; Saltz, L.; Goodman, K.; Downey, R.J.; Nash, G.M.; Temple, L.K.; Paty, P.B.; et al. Pulmonary Recurrence Predominates after Combined Modality Therapy for Rectal Cancer: An Original Retrospective Study. Ann. Surg. 2012, 256, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Van Gijn, W.; Marijnen, C.A.M.; Nagtegaal, I.D.; Kranenbarg, E.M.K.; Putter, H.; Wiggers, T.; Rutten, H.J.T.; Påhlman, L.; Glimelius, B.; Van de Velde, C.J.H. Preoperative Radiotherapy Combined with Total Mesorectal Excision for Resectable Rectal Cancer: 12-Year Follow-up of the Multicentre, Randomised Controlled TME Trial. Lancet Oncol. 2011, 12, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Kjeldsen, B.J.; Kronborg, O.; Fenger, C.; Jørgensen, O.D. A Prospective Randomized Study of Follow-up after Radical Surgery for Colorectal Cancer. Br. J. Surg. 1997, 84, 666–669. [Google Scholar] [CrossRef] [PubMed]
- Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft—Deutsche Krebshilfe—AWMF). S3-Leitlinie Kolorektales Karzinom, Langversion 2.1; AWMF Registernummer 021/007OL; Deutsche Krebshilfe: Bonn, Germany, 2019; pp. 1–328. [Google Scholar]
- Chang, G.J.; Ikoma, N.; You, Y.N.; Bednarski, B.K.; Rodriguez-Bigas, M.A.; Eng, C.; Das, P.; Kopetz, S.; Messick, C.; Skibber, J.M. Impact of Recurrence and Salvage Surgery on Survival after Multidisciplinary Treatment of Rectal Cancer. J. Clin. Oncol. 2017, 35, 2631. [Google Scholar] [CrossRef]
- Salega, A. Outcome nach neoadjuvanter Therapie beim lokal fortgeschrittenen Rektumkarzinom. Ph.D. Thesis, Eberhard Karl University of Tubingen, Tübingen, Germany, 2022. [Google Scholar] [CrossRef]
- Marr, R.; Birbeck, K.; Garvican, J.; Macklin, C.P.; Tiffin, N.J.; Parsons, W.J.; Dixon, M.F.; Mapstone, N.P.; Sebag-Montefiore, D.; Scott, N.; et al. The Modern Abdominoperineal Excision: The next Challenge after Total Mesorectal Excision. Ann. Surg. 2005, 242, 74–82. [Google Scholar] [CrossRef]
- Valentini, V.; Van Stiphout, R.G.P.M.; Lammering, G.; Gambacorta, M.A.; Barba, M.C.; Bebenek, M.; Bonnetain, F.; Bosset, J.F.; Bujko, K.; Cionini, L.; et al. Nomograms for Predicting Local Recurrence, Distant Metastases, and Overall Survival for Patients with Locally Advanced Rectal Cancer on the Basis of European Randomized Clinical Trials. J. Clin. Oncol. 2011, 29, 3163–3172. [Google Scholar] [CrossRef]
- Quirke, P.; Steele, R.; Monson, J.; Grieve, R.; Khanna, S.; Couture, J.; O’Callaghan, C.; Myint, A.S.; Bessell, E.; Thompson, L.C.; et al. Effect of the Plane of Surgery Achieved on Local Recurrence in Patients with Operable Rectal Cancer: A Prospective Study Using Data from the MRC CR07 and NCIC-CTG CO16 Randomised Clinical Trial. Lancet 2009, 373, 821–828. [Google Scholar] [CrossRef]
- Nagtegaal, I.D.; van de Velde, C.J.H.; Marijnen, C.A.M.; van Krieken, J.H.J.M.; Quirke, P. Low Rectal Cancer: A Call for a Change of Approach in Abdominoperineal Resection. J. Clin. Oncol. 2005, 23, 9257–9264. [Google Scholar] [CrossRef] [PubMed]
- Sugihara, K.; Kobayashi, H.; Kato, T.; Mori, T.; Mochizuki, H.; Kameoka, S.; Shirouzu, K.; Muto, T. Indication and Benefit of Pelvic Sidewall Dissection for Rectal Cancer. Dis. Colon Rectum 2006, 49, 1663–1672. [Google Scholar] [CrossRef]
- Christou, N.; Meyer, J.; Toso, C.; Ris, F.; Buchs, N.C. Lateral Lymph Node Dissection for Low Rectal Cancer: Is It Necessary? World J. Gastroenterol. 2019, 25, 4294–4299. [Google Scholar] [CrossRef] [PubMed]
- Ueno, M.; Oya, M.; Azekura, K.; Yamaguchi, T.; Muto, T. Incidence and Prognostic Significance of Lateral Lymph Node Metastasis in Patients with Advanced Low Rectal Cancer. J. Br. Surg. 2005, 92, 756–763. [Google Scholar] [CrossRef]
- Fujita, S.; Mizusawa, J.; Kanemitsu, Y.; Ito, M.; Kinugasa, Y.; Komori, K.; Ohue, M.; Ota, M.; Akazai, Y.; Shiozawa, M.; et al. Mesorectal Excision with or Without Lateral Lymph Node Dissection for Clinical Stage II/III Lower Rectal Cancer (JCOG0212). Ann. Surg. 2017, 266, 201–207. [Google Scholar] [CrossRef]
- Seo, S.I.; Lim, S.-B.; Yoon, Y.S.; Kim, C.W.; Yu, C.S.; Kim, T.W.; Kim, J.H.; Kim, J.C. Comparison of Recurrence Patterns between ≤5 Years and >5 Years after Curative Operations in Colorectal Cancer Patients. J. Surg. Oncol. 2013, 108, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Kuo, L.J.; Liu, M.C.; Jian, J.J.M.; Horng, C.F.; Cheng, T.I.; Chen, C.M.; Fang, W.T.; Chung, Y.L. Is Final TNM Staging a Predictor for Survival in Locally Advanced Rectal Cancer after Preoperative Chemoradiation Therapy? Ann. Surg. Oncol. 2007, 14, 2766–2772. [Google Scholar] [CrossRef]
- Quah, H.-M.; Chou, J.F.; Gonen, M.; Shia, J.; Schrag, D.; Saltz, L.B.; Goodman, K.A.; Minsky, B.D.; Wong, W.D.; Weiser, M.R. Pathologic Stage Is Most Prognostic of Disease-Free Survival in Locally Advanced Rectal Cancer Patients after Preoperative Chemoradiation. Cancer 2008, 113, 57–64. [Google Scholar] [CrossRef]
- Patel, U.B.; Taylor, F.; Blomqvist, L.; George, C.; Evans, H.; Tekkis, P.; Quirke, P.; Sebag-Montefiore, D.; Moran, B.; Heald, R.; et al. Magnetic Resonance Imaging-Detected Tumor Response for Locally Advanced Rectal Cancer Predicts Survival Outcomes: MERCURY Experience. J. Clin. Oncol. 2011, 29, 3753–3760. [Google Scholar] [CrossRef]
- Wibe, A.; Rendedal, P.R.; Svensson, E.; Norstein, J.; Eide, T.J.; Myrvold, H.E.; Søreide, O. Prognostic Significance of the Circumferential Resection Margin Following Total Mesorectal Excision for Rectal Cancer. Br. J. Surg. 2002, 89, 327–334. [Google Scholar] [CrossRef]
- Van Gijn, W.; Van Stiphout, R.G.P.M.; Van de Velde, C.J.H.; Valentini, V.; Lammering, G.; Gambacorta, M.A.; Påhlman, L.; Bujko, K.; Lambin, P. Nomograms to Predict Survival and the Risk for Developing Local or Distant Recurrence in Patients with Rectal Cancer Treated with Optional Short-Term Radiotherapy. Ann. Oncol. 2015, 26, 928–935. [Google Scholar] [CrossRef] [PubMed]
- Bahadoer, R.R.; Dijkstra, E.A.; van Etten, B.; Marijnen, C.A.M.; Putter, H.; Kranenbarg, E.M.K.; Roodvoets, A.G.H.; Nagtegaal, I.D.; Beets-Tan, R.G.H.; Blomqvist, L.K.; et al. Short-Course Radiotherapy Followed by Chemotherapy before Total Mesorectal Excision (TME) versus Preoperative Chemoradiotherapy, TME, and Optional Adjuvant Chemotherapy in Locally Advanced Rectal Cancer (RAPIDO): A Randomised, Open-Label, Phase 3 Trial. Lancet Oncol. 2021, 22, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Conroy, T.; Bosset, J.-F.; Etienne, P.-L.; Rio, E.; François, É.; Mesgouez-Nebout, N.; Vendrely, V.; Artignan, X.; Bouché, O.; Gargot, D.; et al. Neoadjuvant Chemotherapy with FOLFIRINOX and Preoperative Chemoradiotherapy for Patients with Locally Advanced Rectal Cancer (UNICANCER-PRODIGE 23): A Multicentre, Randomised, Open-Label, Phase 3 Trial; The Lancet Oncology: Cambridge, MA, USA, 2021. [Google Scholar]
- Couwenberg, A.M.; Varvoglis, D.N.; Grieb, B.C.; Marijnen, C.A.M.; Ciombor, K.K.; Guillem, J.G. New Opportunities for Minimizing Toxicity in Rectal Cancer Management. Am. Soc. Clin. Oncol. Educ. Book 2023, 43, e389558. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, E.A.; Nilsson, P.J.; Hospers, G.A.P.; Bahadoer, R.R.; Meershoek-Klein Kranenbarg, E.; Roodvoets, A.G.H.; Putter, H.; Berglund, Å.; Cervantes, A.; Crolla, R.M.P.H.; et al. Locoregional Failure During and After Short-Course Radiotherapy Followed by Chemotherapy and Surgery Compared With Long-Course Chemoradiotherapy and Surgery. Ann. Surg. 2023, 278, e766–e772. [Google Scholar] [CrossRef]
- Solomon, M.J.; Brown, K.G.M.; Koh, C.E.; Lee, P.; Austin, K.K.S.; Masya, L. Lateral Pelvic Compartment Excision during Pelvic Exenteration. Br. J. Surg. 2015, 102, 1710–1717. [Google Scholar] [CrossRef]
- Bhangu, A.; Mohammed Ali, S.; Brown, G.; Nicholls, R.J.; Tekkis, P. Indications and Outcome of Pelvic Exenteration for Locally Advanced Primary and Recurrent Rectal Cancer. Ann. Surg. 2014, 259, 315–322. [Google Scholar] [CrossRef]





| Patient Characteristics | |
|---|---|
| Number of Patients | 188 |
| Age (years, median) | 63 (32–88) |
| Follow-up (months, median) | 88.5 |
| Distance from anal verge < 6 cm | 75 (40%) |
| Sphincter preservation | 149 (81%) |
| Sex | |
| Male | 104 (55%) |
| Female | 84 (45%) |
| Comorbidities | |
| Arterial hypertension | 70 (37%) |
| Diabetes | 19 (10%) |
| Obesity | 21 (11%) |
| Inpatient stay (days, mean) | 17.3 (7–80) |
| Complications | |
| Wound infection | 29 (15%) |
| Anastomotic leak | 27 (14%) |
| Stoma-associated complications | 15 (8%) |
| Pathological Stage | |
|---|---|
| ypT stage | |
| ypT0 | 32 (17%) |
| ypT1 | 17 (9%) |
| ypT2 | 56 (30%) |
| ypT3 | 77 (41%) |
| ypT4 | 6 (3%) |
| ypN stage | |
| ypN+ | 44 (24%) |
| ypN− | 144 (77%) |
| UICC stage | |
| Stadium 0 | 30 (16%) |
| Stadium I | 60 (32%) |
| Stadium IIa | 49 (26%) |
| Stadium IIb | 4 (2%) |
| Stadium IIIa | 12 (6%) |
| Stadium IIIb | 20 (11%) |
| Stadium IIIc | 10 (5%) |
| Stadium IV | 3 (2%) |
| Patients with Recurrence | |
|---|---|
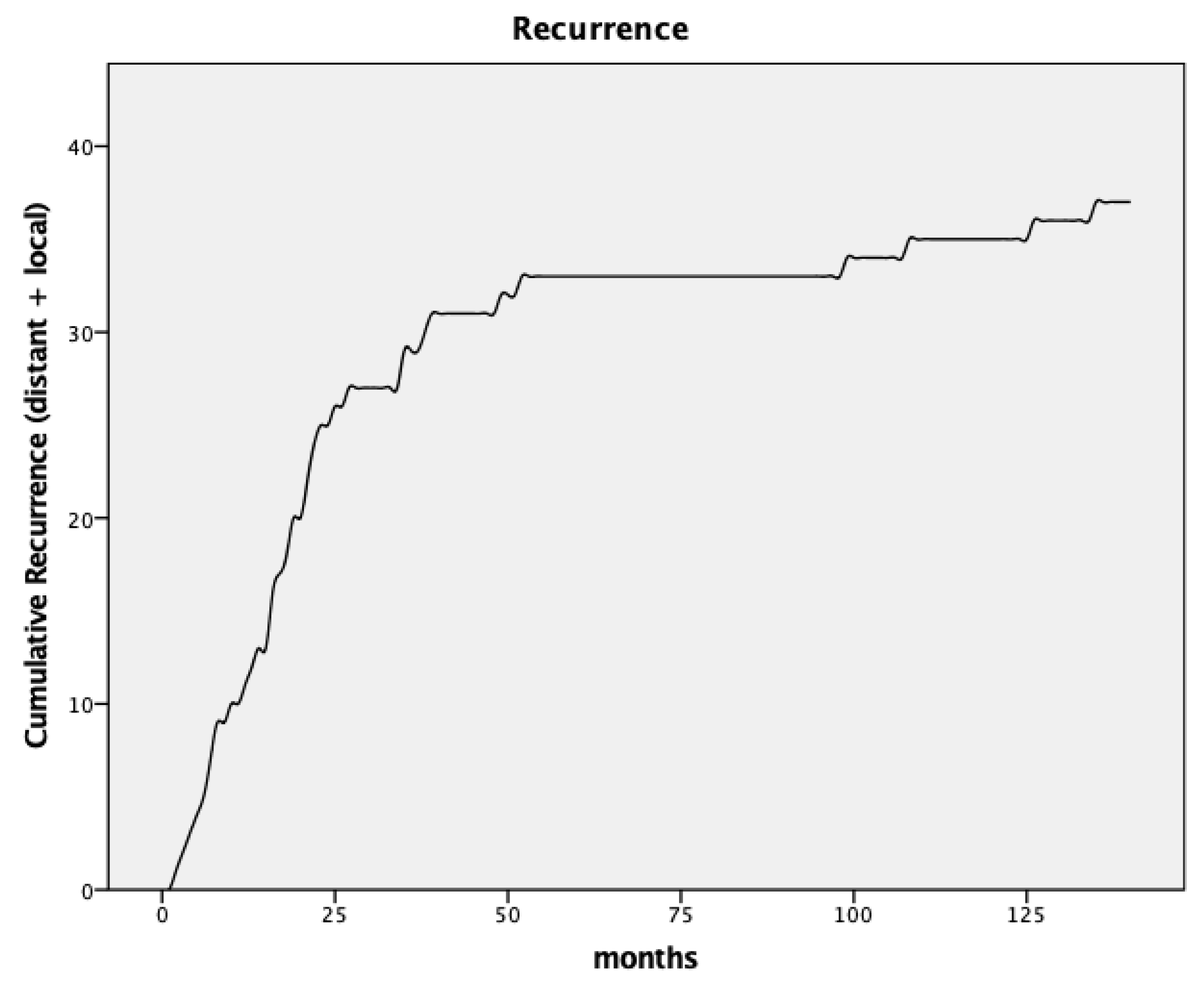
| Total recurrences | 38 (20.2%) |
| Patients with liver metastases | 12 (6.4%) |
| Patients with lung metastases | 7 (3.7%) |
| Patients with local recurrence | 15 (8%) |
| Patients with multiple sites of recurrence | 3 (1.6%) |
| Time to recurrence (months, median) | 19 |
| Distant metastases | 17 |
| Local recurrences | 23 |
| Local recurrences (cumulative) | 15 |
| <5 years of follow-up | 11 (5.9%) |
| 5–8 years of follow-up | 11 (5.9%) |
| >8 years of follow-up | 15 (8%) |
| Age | Sex | Stage | Time to Recurrence | Location of Recurrence |
|---|---|---|---|---|
| 50 years | Female | ypT3ypN2a | 6 months | Lateral/nodal |
| 68 years | Female | ypT2ypN0 | 12 months | Presacral |
| 59 years | Female | ypT2ypN0 | 14 months | Presacral |
| 77 years | Female | ypT4ypN0 | 15 months | Presacral |
| 61 years | Male | ypT3ypN1 | 16 months | Presacral |
| 75 years | Female | ypT3ypN2a | 21 months | Anterior compartment |
| 46 years | Male | ypT3ypN2 | 22 months | Presacral |
| 49 years | Female | ypT3ypN2 | 23 months | Presacral |
| 81 years | Male | ypT2ypN0 | 35 months | Presacral |
| 75 years | Male | ypT3ypN0 | 39 months | Presacral |
| 58 years | Male | ypT2ypN0 | 49 months | Presacral |
| 73 years | Female | ypT2ypN0 | 99 months | Endoluminal |
| 68 years | Female | ypT2ypN0 | 108 months | Anterior compartment |
| 68 years | Male | ypT3ypN0 | 126 months | Presacral |
| 76 years | Male | ypT2ypN1 | 135 months | Lateral/nodal |
| Survival | ||||
|---|---|---|---|---|
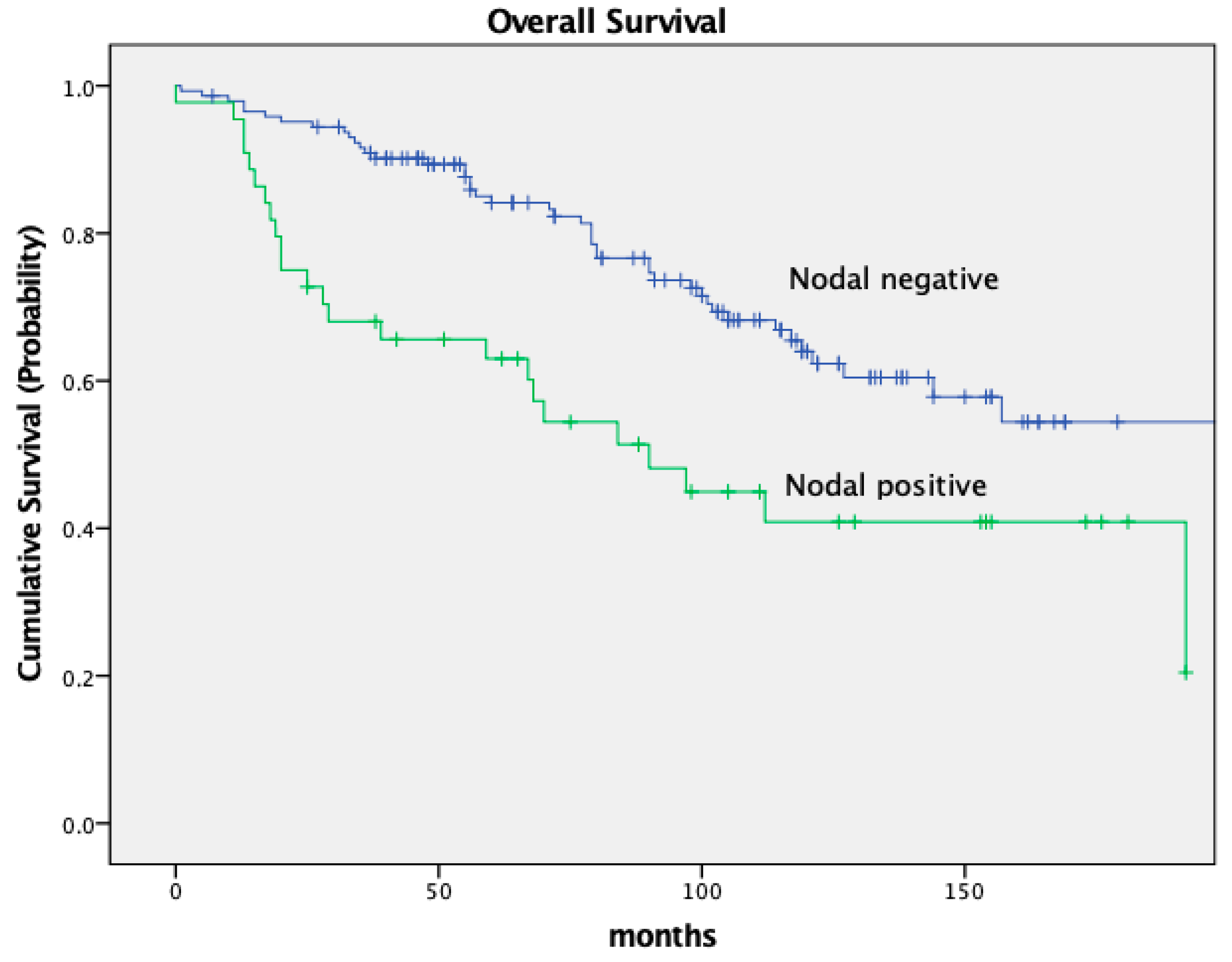
| n | 5-Year OS | 10-Year OS | p | |
| All patients | 188 | 79.2% | 58.5% | |
| Nodal Status | p = 0.001 | |||
| ypN− | 144 (76.6%) | 84.1% | 64.0% | |
| ypN+ | 44 (23.4%) | 63.0% | 40.9% | |
| Recurrence | p < 0.001 | |||
| No recurrence | 150 (79.8%) | 89.6% | 66.0% | |
| Recurrence | 38 (20.2%) | 41.3% | 26.7% | |
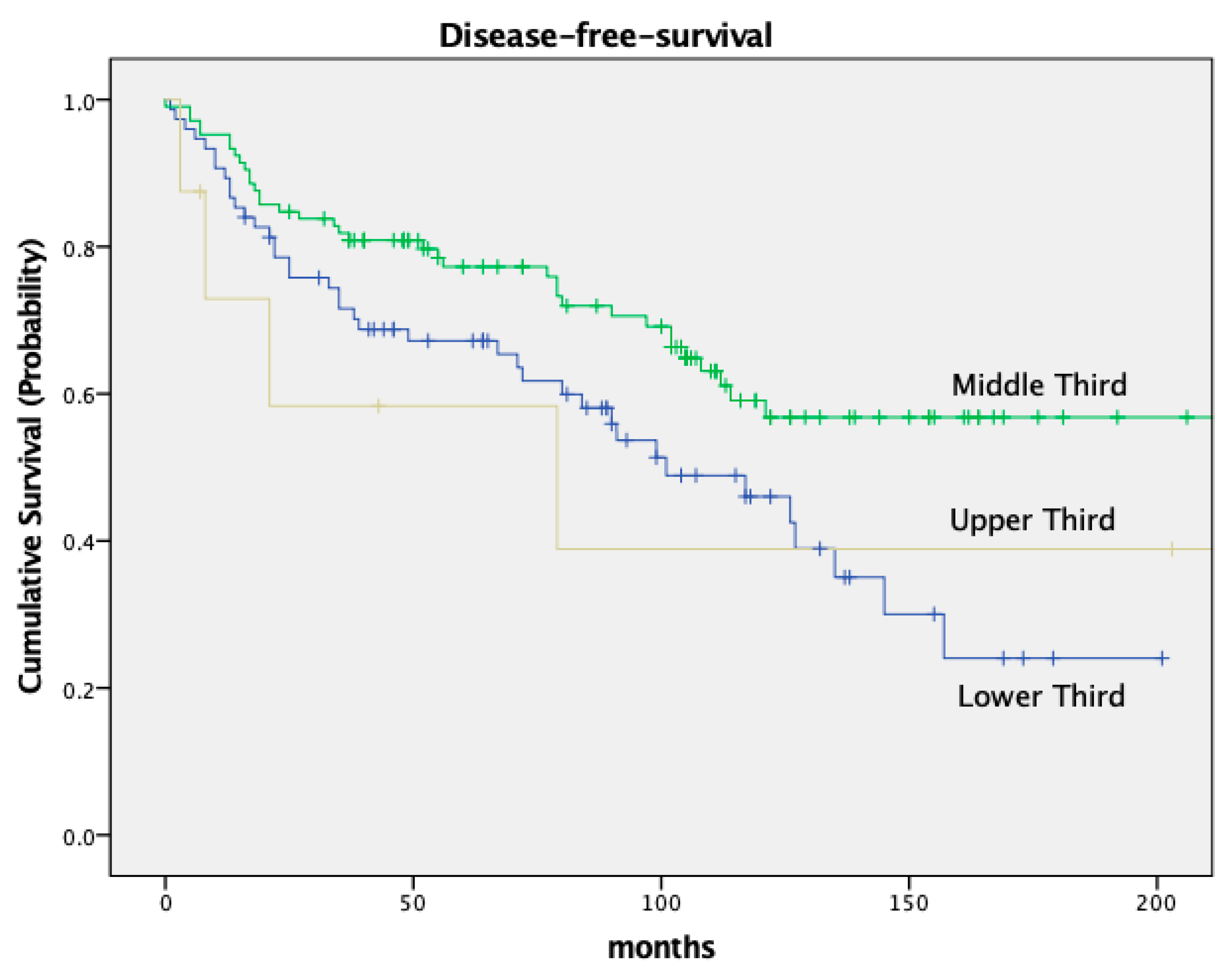
| Location | p = 0.03 | |||
| Upper third | 8 (4.3%) | 85.7% | 58.3% | |
| Middle third | 105 (55.9%) | 83.8% | 77.3% | |
| Lower Third | 75 (39.9%) | 72.1% | 67.2% | |
| T stage | p = 0.063 | |||
| ypT0 | 32 (17.0%) | 86.4% | 60.6% | |
| ypT1 | 17 (9.0%) | 100% | 80.8% | |
| ypT2 | 56 (29.8%) | 79.2% | 59.4% | |
| ypT3 | 77 (41.0%) | 72.7% | 50.8% | |
| ypT4 | 6 (3.2%) | 60% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salega, A.; Münch, M.; Renner, P.; Thon, K.-P.; Steurer, W.; Mönch, D.; Koch, J.; Maaß, A.; Schlitt, H.J.; Dahlke, M.-H.; et al. Late Local Recurrence after Neoadjuvant Therapy and Radical Resection for Locally Advanced Rectal Cancer. Cancers 2024, 16, 448. https://doi.org/10.3390/cancers16020448
Salega A, Münch M, Renner P, Thon K-P, Steurer W, Mönch D, Koch J, Maaß A, Schlitt HJ, Dahlke M-H, et al. Late Local Recurrence after Neoadjuvant Therapy and Radical Resection for Locally Advanced Rectal Cancer. Cancers. 2024; 16(2):448. https://doi.org/10.3390/cancers16020448
Chicago/Turabian StyleSalega, Adrian, Marina Münch, Philipp Renner, Klaus-Peter Thon, Wolfgang Steurer, Dina Mönch, Jana Koch, Annika Maaß, Hans Jürgen Schlitt, Marc-Hendrik Dahlke, and et al. 2024. "Late Local Recurrence after Neoadjuvant Therapy and Radical Resection for Locally Advanced Rectal Cancer" Cancers 16, no. 2: 448. https://doi.org/10.3390/cancers16020448
APA StyleSalega, A., Münch, M., Renner, P., Thon, K.-P., Steurer, W., Mönch, D., Koch, J., Maaß, A., Schlitt, H. J., Dahlke, M.-H., & Leibold, T. (2024). Late Local Recurrence after Neoadjuvant Therapy and Radical Resection for Locally Advanced Rectal Cancer. Cancers, 16(2), 448. https://doi.org/10.3390/cancers16020448






