Urodynamic Parameters and Continence Outcomes in Asymptomatic Patients with Ileal Orthotopic Neobladder: A Systematic Review and Metanalysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Information Sources, Search Strategy and Selection Process
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection Process and Data Items
2.4. Effect Measures
2.5. Synthesis Methods
2.6. Reporting Bias Assessment
3. Results
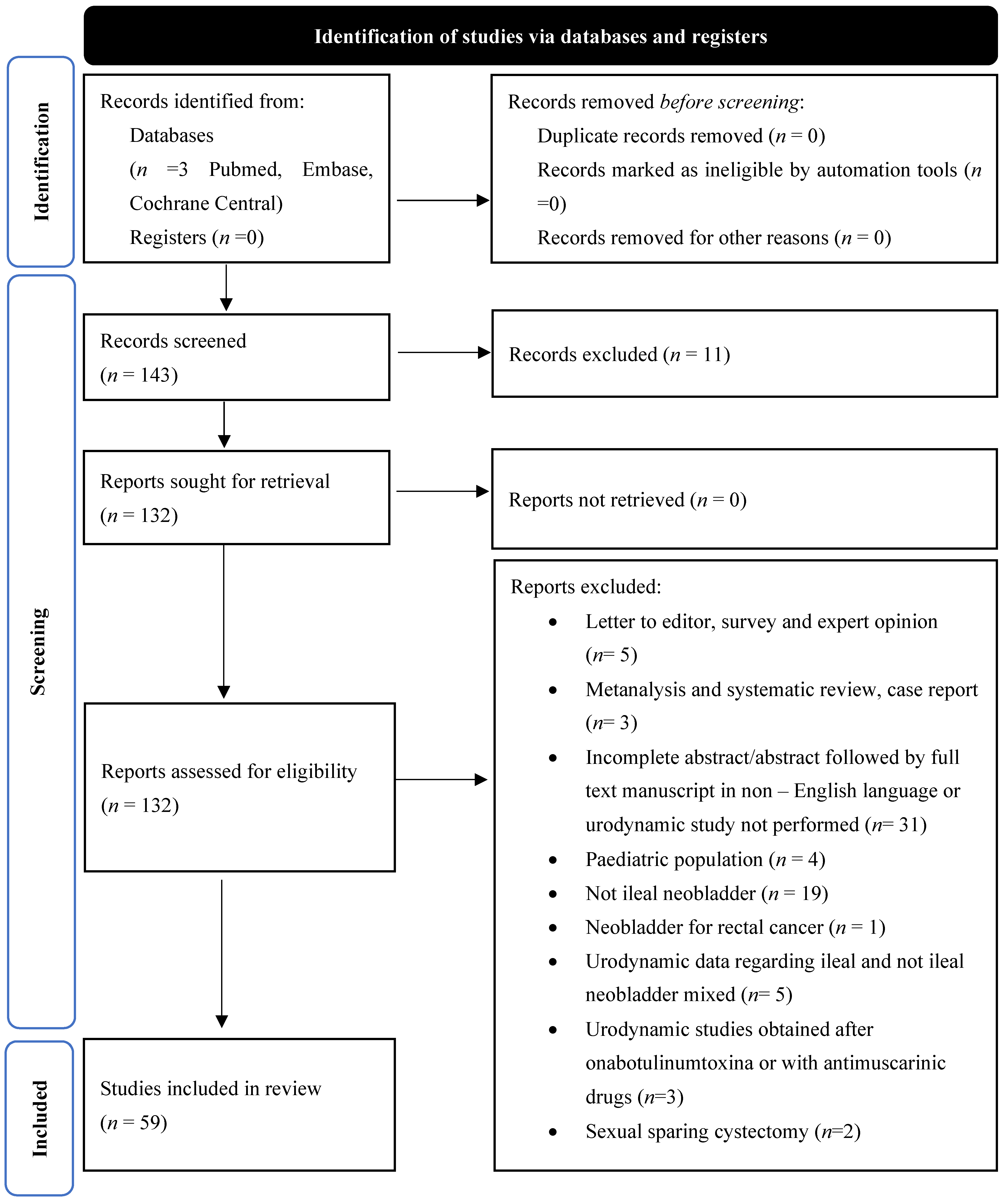
3.1. Study Selection
3.2. Study Characteristics
3.2.1. General Aspects
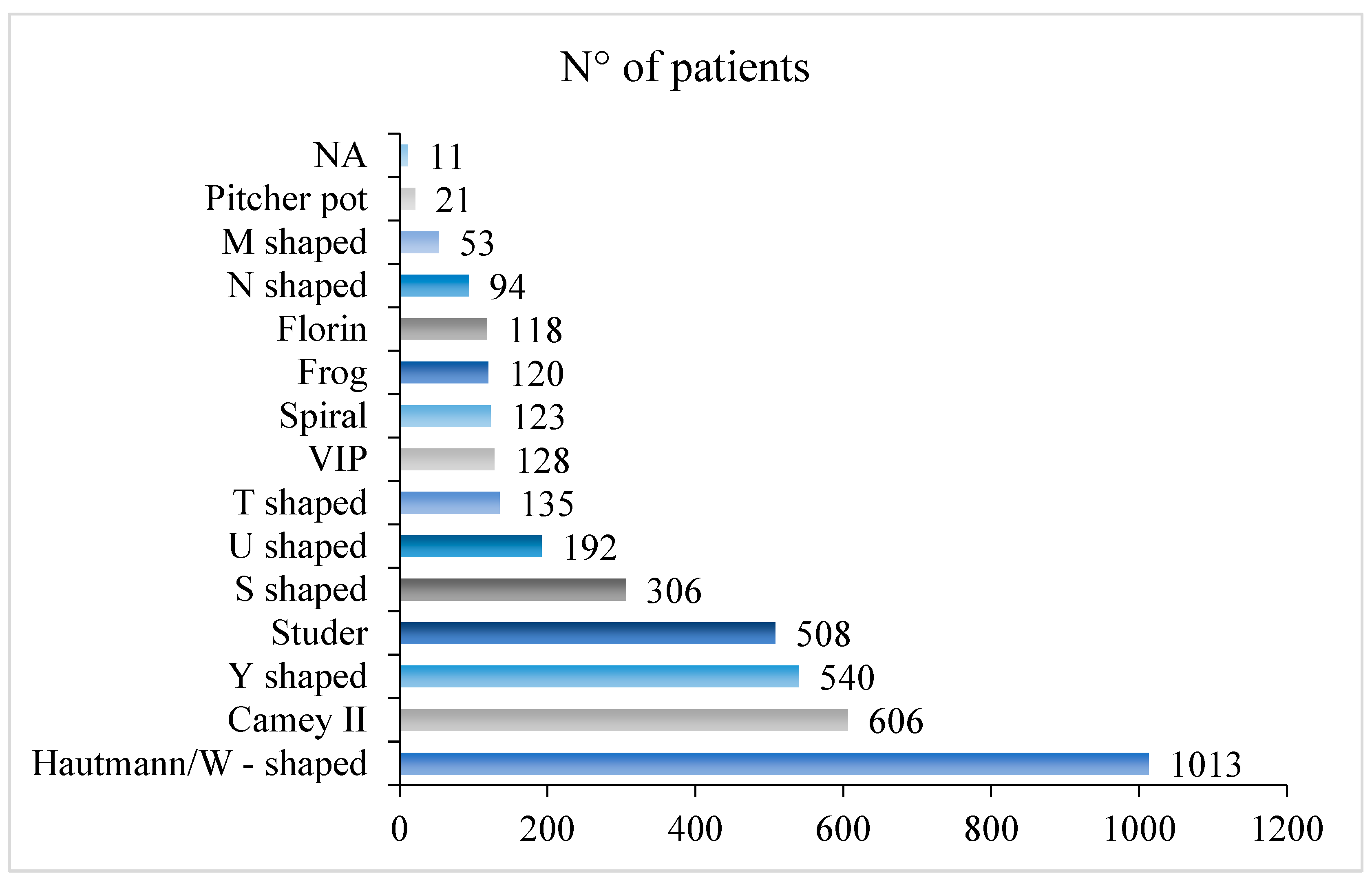
3.2.2. Surgical and Technical Aspects
3.2.3. Continence and Urodynamic Data
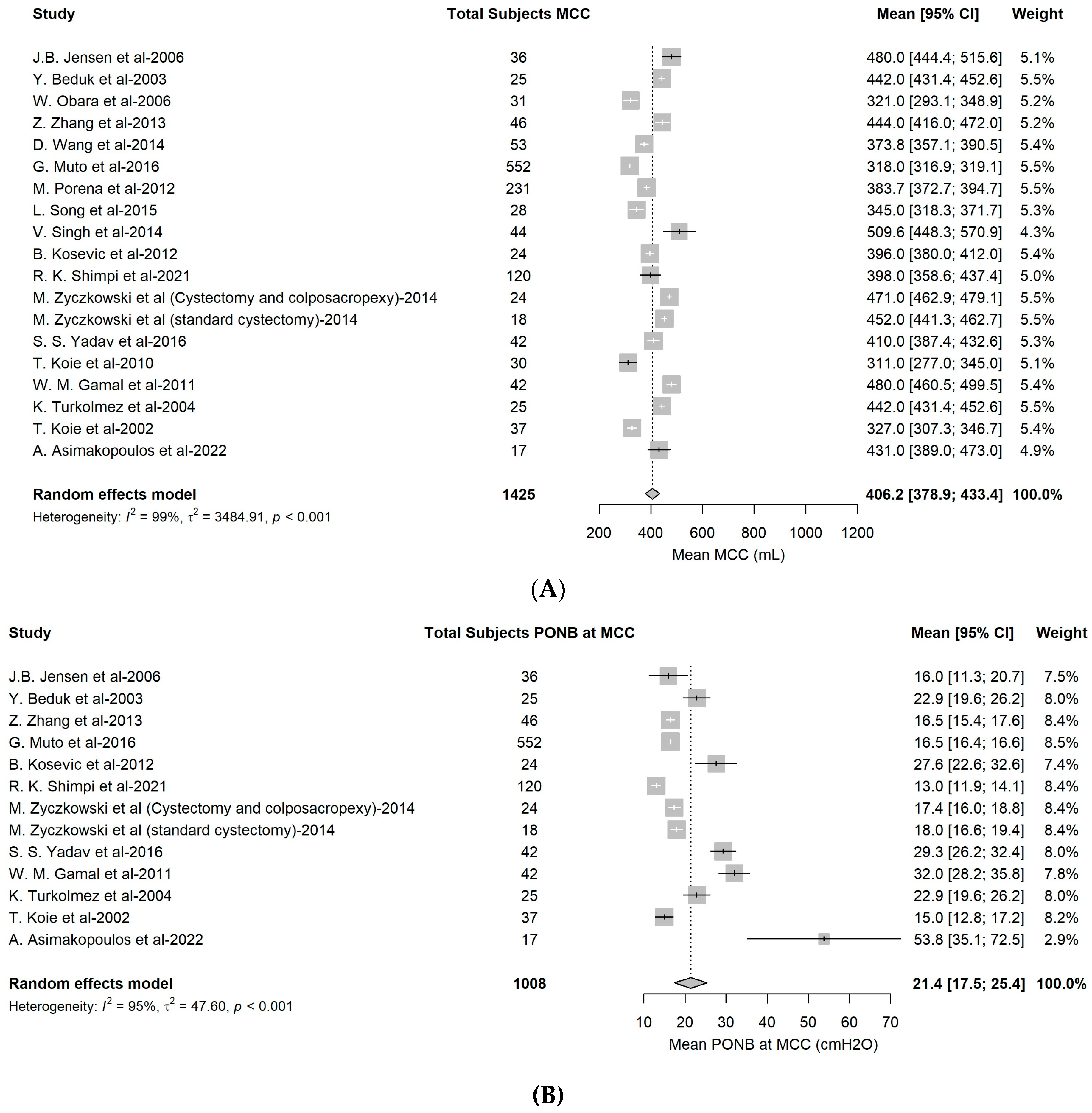
3.3. Meta-Analysis of UDS Data
Subgroup Analysis and Sensitivity Analysis for UDS Data
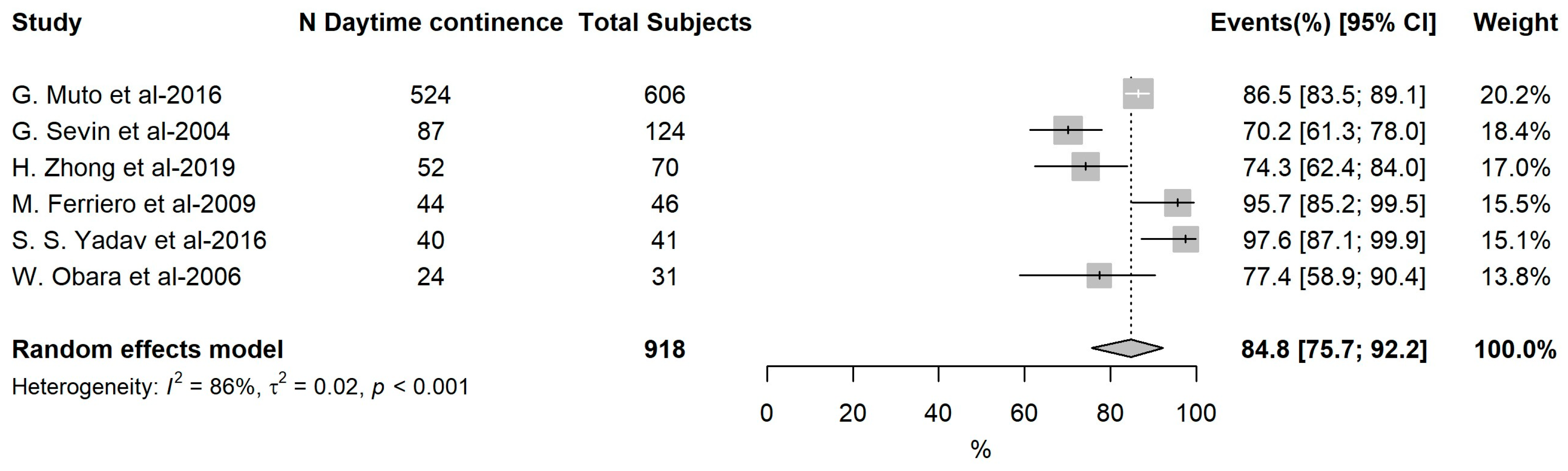
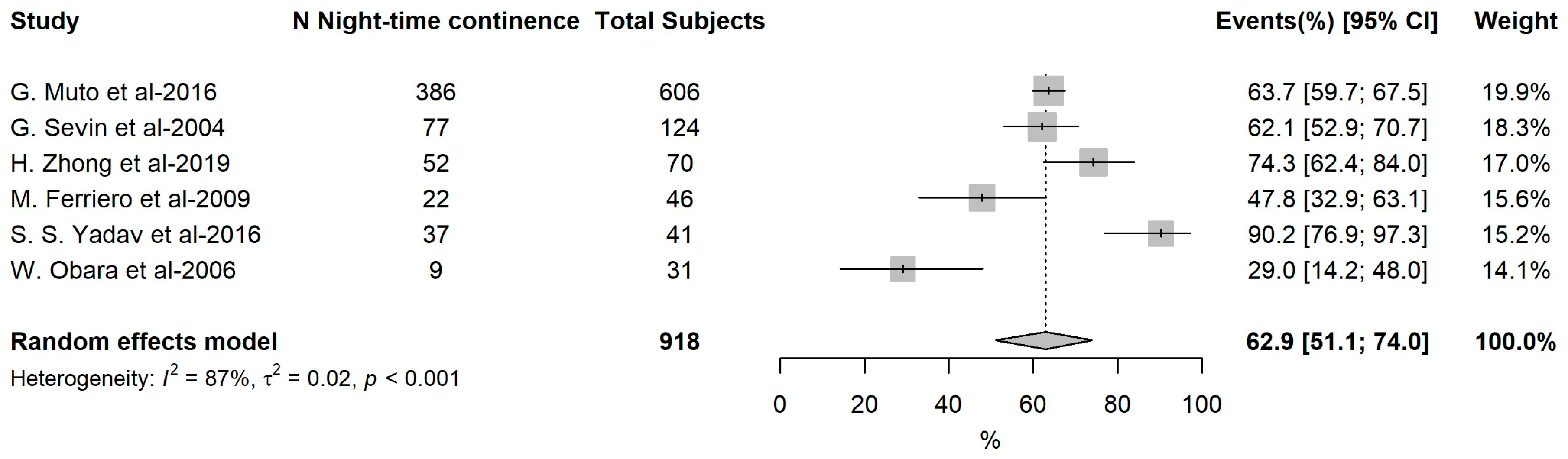
3.4. Meta-Analysis of Continence Outcomes
Subgroup Analysis and Sensitivity Analysis for Continence Data
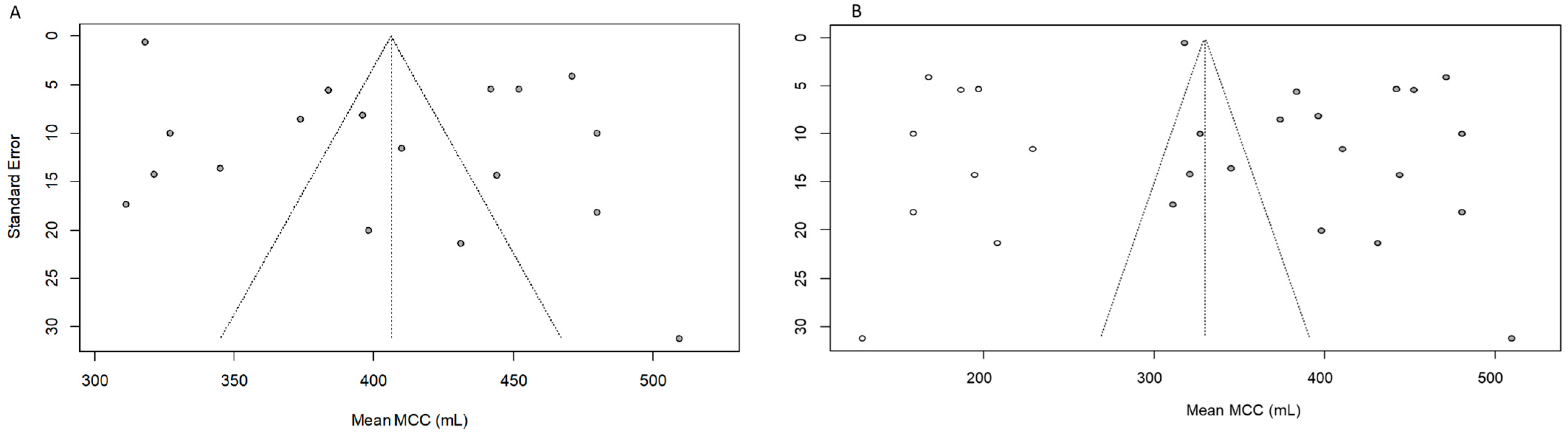
3.5. Reporting Biases of Metanalysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Analysis Specification | N° of Studies | Estimated Pooled Mean | 95% CI | I2 | psubgroup Value |
|---|---|---|---|---|---|
| MCC | |||||
| ONB Type | <0.001 | ||||
| W-Hautmann | 5 | 432.3 | 406.0; 458.6 | 89.1% | |
| Studer | 4 | 436.8 | 357.5; 516.1 | 97.2% | |
| Camey II | 1 | 318.0 | 316.9; 319.2 | - | |
| Y Shape | 2 | 402.8 | 357.3; 448.3 | 78.1% | |
| PONB at MCC | |||||
| ONB Type | <0.001 | ||||
| W-Hautmann | 5 | 23.8 | 19.4; 28.2 | 84.0% | |
| Studer | 1 | 16.5 | 16.4; 16.7 | -- | |
| Camey II | 2 | 17.7 | 16.7; 18.7 | 0.0% | |
| Y Shape | 1 | 53.8 | 35.1; 72.5 | -- | |
| Analysis Specification | N° of Studies | Estimated Pooled Proportion (%) | 95% CI | I2 | psubgroup Value |
|---|---|---|---|---|---|
| Daytime continence | |||||
| ONB Type | 0.019 | ||||
| W-Hautmann | 4 | 91.0% | 74.8–99.6% | 91.2% | |
| Studer | 2 | 74.7% | 64.1–84.1% | 0.0% | |
| Camey II | 1 | 86.5% | 83.6–89.1% | -- | |
| Y Shape | 5 | 75.1% | 60.3–87.5% | 88.9% | |
| Night-time continence | |||||
| ONB Type | 0.691 | ||||
| W-Hautmann | 4 | 53.0% | 15.9–88.2% | 97.5% | |
| Studer | 2 | 47.0% | 15.3–79.3% | 88.6% | |
| Camey II | 1 | 64.0% | 59.8–67.5% | -- | |
| Y Shape | 5 | 67.0% | 52.8–79.6% | 86.2% | |
Appendix B

References
- Hautmann, R.E. Urinary diversion: Ileal conduit to neobladder. J. Urol. 2003, 169, 834–842. [Google Scholar] [CrossRef] [PubMed]
- Minervini, A.; Serni, S.; Vittori, G.; Masieri, L.; Siena, G.; Lanciotti, M.; Lapini, A.; Gacci, M.; Carini, M. Current indications and results of orthotopic ileal neobladder for bladder cancer. Expert Rev. Anticancer Ther. 2014, 14, 419–430. [Google Scholar] [CrossRef]
- Steers, W.D. Voiding dysfunction in the orthotopic neobladder. World J. Urol. 2000, 18, 330–337. [Google Scholar] [CrossRef]
- Alfred Witjes, J.; Max Bruins, H.; Carrión, A.; Cathomas, R.; Compérat, E.; Efstathiou, J.A.; Fietkau, R.; Gakis, G.; Lorch, A.; Martini, A.; et al. European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2023 Guidelines. Eur. Urol. 2024, 85, 17–31, Erratum in Eur. Urol. 2024. [Google Scholar] [CrossRef]
- Chang, S.S.; Bochner, B.H.; Chou, R.; Dreicer, R.; Kamat, A.M.; Lerner, S.P.; Lotan, Y.; Meeks, J.J.; Michalski, J.M.; Morgan, T.M.; et al. Treatment of Non-Metastatic Muscle-Invasive Bladder Cancer: AUA/ASCO/ASTRO/SUO Guideline. J. Urol. 2017, 198, 552–559. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar]
- Apostolos, M.; Georgios, D.; Spyridon, K.; Georgios, G.; Ioannis, V.; Stavros, I.; Konstantinos, H.; Dimitrios, H. Comparison Between Ambulatory and Conventional Urodynamics of the Modified Orthotopic Hautmann Neobladder. Int. Neurourol. J. 2015, 19, 265–271. [Google Scholar] [CrossRef][Green Version]
- Zhou, X.; Zheng, J.; He, P.; Zhang, J.; Wang, C.; Zheng, J.; Li, X.; Lang, L.; Zhou, Z.; Chen, Z. Refinement Surgical Technique, and Perioperative and Functional Outcomes in Patients With Robotic Intracorporeal Hautmann Orthotopic Neobladder. Urology 2020, 138, 45–51. [Google Scholar] [CrossRef]
- Niu, Y.N.; Xing, N.Z.; Zhou, Z.D. Orthotopic T pouch ileal neobladder: Evaluations of urodynamics and upper urinary tract functions. Zhonghua Yi Xue Za Zhi 2010, 90, 3099–3102. [Google Scholar]
- Porena, M.; Mearini, L.; Zucchi, A.; Zingaro, M.D.; Mearini, E.; Giannantoni, A. Perugia ileal neobladder: Functional results and complications. World J. Urol. 2012, 30, 747–752. [Google Scholar] [CrossRef]
- Jensen, J.B.; Lundbeck, F.; Jensen, K.M. Complications and neobladder function of the Hautmann orthotopic ileal neobladder. BJU Int. 2006, 98, 1289–1294. [Google Scholar] [CrossRef]
- Singh, U.P.; Jena, R.; Madhavan, K.; Kumar, N.; Sureka, S.K.; Srivastava, A. Radical cystectomy and W-shaped ileal orthotopic neobladder reconstruction with serosa-lined tunneled ureteroileal anastomoses: A critical analysis of the short-term voiding patterns and urodynamic and functional outcomes. Indian J. Urol. 2019, 35, 121–128. [Google Scholar]
- Satkunasivam, R.; Santomauro, M.; Chopra, S.; Plotner, E.; Cai, J.; Miranda, G.; Salibian, S.; Aron, M.; Ginsberg, D.; Daneshmand, S.; et al. Robotic Intracorporeal Orthotopic Neobladder: Urodynamic Outcomes, Urinary Function, and Health-related Quality of Life. Eur. Urol. 2016, 69, 247–253. [Google Scholar] [CrossRef]
- Zhong, H.; Shen, Y.; Yao, Z.; Chen, X.; Gao, J.; Xiang, A.; Wang, W. Long-term outcome of spiral ileal neobladder with orthotopic ureteral reimplantation. Int. Urol. Nephrol. 2020, 52, 41–49. [Google Scholar] [CrossRef]
- Shimpi, R.K.; Patel, D.N.; Raval, K.; Shah, P.; Shah, B. Study of modified technique of ileal neobladder-Frog neobladder. Urol. Ann. 2021, 13, 19–23. [Google Scholar]
- Fontana, D.; Bellina, M.; Fasolis, G.; Frea, B.; Scarpa, R.M.; Mari, M.; Rolle, L.; Destefanis, P. Y-neobladder: An easy, fast, and reliable procedure. Urology 2004, 63, 699–703. [Google Scholar] [CrossRef]
- Koie, T.; Hatakeyama, S.; Yoneyama, T.; Ishimura, H.; Yamato, T.; Ohyama, C. Experience and functional outcome of modified ileal neobladder in 95 patients. Int. J. Urol. 2006, 13, 1175–1179. [Google Scholar] [CrossRef]
- El-Helaly, H.A.; Saifelnasr, M.K.; Mohamed, K.M.; Abdelaziz, A.S.; Youssof, H.A. Outcome of orthotopic sigmoid versus ileal neobladder reconstruction. Urol. Ann. 2019, 11, 204–210. [Google Scholar]
- Zhang, Z.; Qi, H.; Zhou, R.; Jin, X. Early and late urodynamic assessment of the orthotopic N-shaped neobladder. Oncol. Lett. 2013, 6, 1053–1056. [Google Scholar] [CrossRef]
- Checcucci, E.; Manfredi, M.; Sica, M.; Amparore, D.; De Cillis, S.; Volpi, G.; Granato, S.; Carbonaro, B.; Piramide, F.; Meziere, J.; et al. Robot-assisted-radical-cystectomy with total intracorporeal Y neobladder: Analysis of postoperative complications and functional outcomes with urodynamics findings. Eur. J. Surg. Oncol. 2022, 48, 694–702. [Google Scholar] [CrossRef]
- Barapatre, Y.R.; Agarwal, M.M.; Mavuduru, R.; Sharma, S.K.; Kumar, S.; Singh, S.K.; Mandal, A.K. Short-Term Functional and Urodynamic Outcome of W-ileal Orthotopic Neobladder with Serosa-Lined Tunneled Uretero-Ileal Anastomosis. Low Urin. Tract Symptoms 2014, 6, 26–34. [Google Scholar] [CrossRef]
- Singh, V.; Mandal, S.; Patil, S.; Sinha, R.J.; Gupta, D.K.; Sankhwar, S.N. Urodynamic and continence assessment of orthotropic neobladder reconstruction following radical cystectomy in bladder cancer; a prospective, blinded North Indian tertiary care experience. S. Asian J. Cancer 2014, 3, 223–226. [Google Scholar] [CrossRef]
- Grobet-Jeandin, E.; Benamran, D.; Pinar, U.; Beirnaert, J.; Parra, J.; Vaessen, C.; Seisen, T.; Rouprêt, M.; Phé, V. Urodynamic assessment and quality of life outcomes of robot-assisted totally intracorporeal radical cystectomy and orthotopic neobladder for bladder cancer: A preliminary study. World J. Urol. 2022, 40, 2535–2541. [Google Scholar] [CrossRef]
- Marim, G.; Bal, K.; Balci, U.; Girgin, C.; Dinçel, C. Long-term urodynamic and functional analysis of orthotopic "W" ileal neobladder following radical cystectomy. Int. Urol. Nephrol. 2008, 40, 629–636. [Google Scholar] [CrossRef]
- Yadav, S.S.; Gangkak, G.; Mathur, R.; Yadav, R.G.; Tomar, V. Long-term Functional, Urodynamic, and Metabolic Outcome of a Modified Orthotopic Neobladder Created With a Short Ileal Segment: Our 5-year Experience. Urology 2016, 94, 167–172. [Google Scholar] [CrossRef]
- Koie, T.; Hatakeyama, S.; Yoneyama, T.; Hashimoto, Y.; Kamimura, N.; Ohyama, C. Uterus-, fallopian tube-, ovary-, and vagina-sparing cystectomy followed by U-shaped ileal neobladder construction for female bladder cancer patients: Oncological and functional outcomes. Urology 2010, 75, 1499–1503. [Google Scholar] [CrossRef]
- Muto, G.; Collura, D.; Simone, G.; Muto, G.L.; Rosso, R.; Giacobbe, A.; Castelli, E. Stapled orthotopic ileal neobladder after radical cystectomy for bladder cancer: Functional results and complications over a 20-year period. Eur. J. Surg. Oncol. 2016, 42, 412–418. [Google Scholar] [CrossRef]
- Khan, A.; Vuppalapati, J.K.; Sarath, L.R.; Mujeeburahiman, M.; D’souza, N. Functional outcome of robotic-assisted intracorporeal versus extracorporeal neobladder following radical cystectomy: Initial experience. Urol. Ann. 2021, 13, 9–13. [Google Scholar]
- Sevin, G.; Soyupek, S.; Armağan, A.; Hoşcan, M.B.; Oksay, T. Ileal orthotopic neobladder (modified Hautmann) via a shorter detubularized ileal segment: Experience and results. BJU Int. 2004, 94, 355–359. [Google Scholar] [CrossRef]
- Hassan, A.A.; Elgamal, S.A.; Sabaa, M.A.; Salem, K.A.; Elmateet, M.S. Evaluation of direct versus non-refluxing technique and functional results in orthotopic Y-ileal neobladder after 12 years of follow up. Int. J. Urol. 2007, 14, 300–304. [Google Scholar] [CrossRef]
- Nam, J.K.; Kim, T.N.; Park, S.W.; Lee, S.D.; Chung, M.K. The Studer orthotopic neobladder: Long-term (more than 10 years) functional outcomes, urodynamic features, and complications. Yonsei Med. J. 2013, 54, 690–695. [Google Scholar] [CrossRef]
- Minervini, A.; Vanacore, D.; Vittori, G.; Milanesi, M.; Tuccio, A.; Siena, G.; Campi, R.; Mari, A.; Gavazzi, A.; Carini, M. Florence robotic intracorporeal neobladder (FloRIN): A new reconfiguration strategy developed following the IDEAL guidelines. BJU Int. 2018, 121, 313–317. [Google Scholar] [CrossRef]
- Dellis, A.E.; Papatsoris, A.G.; Skolarikos, A.A.; Varkarakis, I.M.; Deliveliotis, C.N. Modified S-ileal neobladder for continent urinary diversion: Functional and urodynamic results after 20 years of follow-up. Urol. Int. 2014, 93, 43–48. [Google Scholar] [CrossRef]
- Bedük, Y.; Türkölmez, K.; Baltaci, S.; Göğüş, C. Comparison of clinical and urodynamic outcome in orthotopic ileocaecal and ileal neobladder. Eur. Urol. 2003, 43, 258–262. [Google Scholar] [CrossRef]
- Kim, K.H.; Yoon, H.S.; Song, W.; Choo, H.J.; Yoon, H.; Chung, W.S.; Sim, B.S.; Lee, D.H. Cluster analysis identifies three urodynamic patterns in patients with orthotopic neobladder reconstruction. PLoS ONE 2017, 12, e0185255. [Google Scholar] [CrossRef] [PubMed]
- Nagahama, K.; Yamada, T.; Ichiyanagi, N.; Sakai, Y.; Kamata, S.; Fukuda, H.; Tanizawa, A.; Watanabe, T.; Saitoh, H.; Horiuchi, S.; et al. Functional and urodynamic characteristics in patients with ileal neobladder. Hinyokika Kiyo 2002, 48, 1–6. [Google Scholar] [PubMed]
- Dos Reis, R.B.; Machado, R.D.; Faria, E.F.; Cassini, M.; Kaplan, S. Modified technique for the creation of an orthotopic neobladder in patients with shortened mesentery: Making up the difference between the bladder and the urethral stump. Urology 2011, 78, 1430–1434. [Google Scholar] [CrossRef] [PubMed]
- Muto, S.; Kamiyama, Y.; Ide, H.; Okada, H.; Saito, K.; Nishio, K.; Tokiwa, S.; Kaminaga, T.; Furui, S.; Horie, S. Real-time MRI of orthotopic ileal neobladder voiding: Preliminary findings. Eur. Urol. 2008, 53, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Ferriero, M.; Simone, G.; Rocchegiani, A.; Buscarini, M.; Papalia, R.; Alcini, A.; Flammia, G.P.; Gallucci, M. Early and late urodynamic assessment of Padua ileal bladder. Urology. 2009, 73, 1357–1362. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.G.; Zhong, H.; Yu, B.; Tang, J.E.; Chen, Y.; Cao, M.; Jin, X.D. Modified orthotopic spiral ileal bladder substitution: Surgical technique and long-term results. Urol. Oncol. 2013, 31, 1599–1605. [Google Scholar] [CrossRef] [PubMed]
- Gamal, W.M.; Osman, M.M.; Hammady, A.; Eldahshoury, M.; Moursy, E.; Hussein, M.M.; Abuzeid, A. Modified N-shaped ileal neobladder after radical cystectomy. Urol. Oncol. 2011, 29, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Obara, W.; Isurugi, K.; Kudo, D.; Takata, R.; Kato, K.; Kanehira, M.; Iwasaki, K.; Tanji, S.; Konda, R.; Fujioka, T. Eight year experience with Studer ileal neobladder. Jpn. J. Clin. Oncol. 2006, 36, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Crivellaro, S.; Mami, E.; Wald, C.; Smith, J.J.; Kocjancic, E.; Stoffel, J.; Bresette, J.; Libertino, J.A. Correlation between urodynamic function and 3D cat scan anatomy in neobladders: Does it exist? Neurourol. Urodyn. 2009, 28, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Rawal, S.; Kumar, P.; Kaul, R.; Raghunath, S.K.; Julka, S. The ‘pitcher pot’ ileal neobladder: Early experiences. Jpn. J. Clin. Oncol. 2006, 36, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Bayraktar, Z.; Sevin, G.; Gurbuz, G.; Taşci, A.I. Ileal orthotopic neobladder in women: The first experiences from Turkey and our modifications. Int. Urol. Nephrol. 2001, 32, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Kosević, B.; Aleksić, P.; Milović, N.; Banfevit, V.; Stamenković, D.; Nikolić, I.; Jovanović, M.; Milosević, R. Urodynamic characteristics of the modified orthotopic ileal neobladder. Vojnosanit. Pregl. 2012, 69, 253–256. [Google Scholar] [CrossRef]
- Constantinides, C.; Manousakas, T.; Chrisofos, M.; Giannopoulos, A. Orthotopic bladder substitution after radical cystectomy: 5 years of experience with a novel personal modification of the ileal s pouch. J. Urol. 2001, 166, 532–537. [Google Scholar] [CrossRef]
- Khafagy, M.; Shaheed, F.A.; Moneim, T.A. Ileocaecal vs ileal neobladder after radical cystectomy in patients with bladder cancer: A comparative study. BJU Int. 2006, 97, 799–804. [Google Scholar] [CrossRef]
- Chen, Z.; Lu, G.; Li, X.; Li, X.; Fang, Q.; Ji, H.; Yan, J.; Zhou, Z.; Pan, J.; Fu, W.; et al. Better compliance contributes to better nocturnal continence with orthotopic ileal neobladder than ileocolonic neobladder after radical cystectomy for bladder cancer. Urology 2009, 73, 838–843; discussion 843–844. [Google Scholar] [CrossRef] [PubMed]
- Palleschi, G.; Pastore, A.L.; Ripoli, A.; Silvestri, L.; Petrozza, V.; Carbone, A. Videourodynamic evaluation of intracorporeally reconstructed orthotopic U-shaped ileal neobladders. Urology 2015, 85, 883–889. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fang, D.B.; Cai, S.L.; Jin, X.D.; Chen, J.; Jin, B.Y.; Zheng, X.Y.; Wang, C.J.; Tan, F.Q.; Wang, S.; Shen, B.H.; et al. Hand-assisted-drawing-needle running suture with a curved needle: An effective technique to create a W-ileal neobladder. Chin. Med. J. Engl. 2012, 125, 2225–2227. [Google Scholar]
- Schrier, B.P.; Laguna, M.P.; van der Pal, F.; Isorna, S.; Witjes, J.A. Comparison of orthotopic sigmoid and ileal neobladders: Continence and urodynamic parameters. Eur. Urol. 2005, 47, 679–685. [Google Scholar] [CrossRef]
- Wang, D.; Li, L.J.; Liu, J.; Qiu, M.X. Long-term urodynamic evaluation of laparoscopic radical cystectomy with orthotopic ileal neobladder for bladder cancer. Oncol. Lett. 2014, 8, 1031–1034. [Google Scholar] [CrossRef]
- Song, L.; Xing, N.; Niu, Y.; Zhang, J.; Tian, X.; Wang, J. Mid-long-term follow-up of radical cystectomy with orthotopic ileal neobladder in women patients with bladder carcinoma. Zhonghua Yi Xue Za Zhi 2014, 94, 932–934. [Google Scholar] [PubMed]
- Honeck, P.; Bolenz, C.; Wendt-Nordahl, G.; Alken, P.; Michel, M.S. Outcome of sigmoid compared to ileal orthotopic bladder substitution in terms of micturition and defecation parameters in an 8-year long-term follow-up. Urol. Int. 2009, 83, 277–280. [Google Scholar] [CrossRef]
- Skolarikos, A.; Deliveliotis, C.; Alargof, E.; Ferakis, N.; Protogerou, V.; Dimopoulos, C. Modified ileal neobladder for continent urinary diversion: Functional results after 9 years of experience. J. Urol. 2004, 171 6 Pt 1, 2298–2301. [Google Scholar] [CrossRef]
- Koie, T.; Kawaguchi, T.; Takahashi, N. Orthotopic ileal neobladder reconstruction using a modified Goodwin method: Functional outcome in 37 patients. Hinyokika Kiyo 2002, 48, 407–413. [Google Scholar] [PubMed]
- Caproni, N.; Ligabue, G.; Mami, E.; Torricelli, P. Reconstructed urinary bladder following radical cystectomy for bladder cancer. Multidetector CT evaluation of normal findings and complications. Radiol. Med. 2006, 111, 1134–1145. [Google Scholar] [CrossRef]
- El-Bahnasawy, M.S.; Osman, Y.; Gomha, M.A.; Shaaban, A.A. Persistent and occasional nocturnal enuresis in orthotopic urinary diversion: Is there a urodynamic difference? BJU Int. 2005, 96, 1373–1377. [Google Scholar] [CrossRef]
- Życzkowski, M.; Muskała, B.; Kaletka, Z.; Bryniarski, P.; Nowakowski, K.; Bogacki, R.; Paradysz, A. Sacrocolpopexy with polypropylene tape as valuable surgical modification during cystectomy with orthotopic ileal bladder: Functional results. Biomed. Res. Int. 2015, 2015, 306191. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.Y.; Zhou, C.W.; Liu, Y.Q. Laparoscopic radical cystectomy with orthotopic ileal neobladder in the treatment of invasive bladder cancer. Zhonghua Zhong Liu Za Zhi 2012, 34, 793–796. [Google Scholar]
- Türkölmez, K.; Baltaci, S.; Göğüş, C.; Bedük, Y.; Göğüş, O. Results of the ureteral reimplantation with serous-lined extramural tunnel in orthotopic ileal W-neobladder. Int. J. Urol. 2004, 11, 368–373. [Google Scholar] [CrossRef]
- Osman, Y.; Abol-Enein, H.; Nabeeh, A.; Gaballah, M.; Bazeed, M. Long-term results of a prospective randomized study comparing two different antireflux techniques in orthotopic bladder substitution. Eur. Urol. 2004, 45, 82–86. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Gubbiotti, M.; Agrò, E.F.; Morini, E.; Giommoni, V.; Piechaud, T.; Gaston, R.; Annino, F. “Bordeaux Neobladder”: First Evaluation of the Urodynamic Outcomes. Eur. Urol. Open Sci. 2022, 47, 102–109. [Google Scholar] [CrossRef]
- Di Maida, F.; Grosso, A.A.; Tasso, G.; Gemma, L.; Lambertini, L.; Nardoni, S.; Mari, A.; Tuccio, A.; Vittori, G.; Masieri, L.; et al. Robot assisted radical cystectomy with Florence Robotic Intracorporeal Neobladder (FloRIN): Functional and urodynamic features compared with a contemporary series of open Vescica Ileale Padovana (VIP). Eur. J. Surg. Oncol. 2022, 48, 1854–1861. [Google Scholar] [CrossRef]
- Cerruto, M.A.; D’Elia, C.; Siracusano, S.; Gedeshi, X.; Mariotto, A.; Iafrate, M.; Niero, M.; Lonardi, C.; Bassi, P.; Belgrano, E.; et al. Systematic review and meta-analysis of non RCT’s on health related quality of life after radical cystectomy using validated questionnaires: Better results with orthotopic neobladder versus ileal conduit. Eur. J. Surg. Oncol. 2016, 42, 343–360. [Google Scholar] [CrossRef]
- Rosier, P.F.W.M.; Schaefer, W.; Lose, G.; Goldman, H.B.; Guralnick, M.; Eustice, S.; Dickinson, T.; Hashim, H. International Continence Society Good Urodynamic Practices and Terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol. Urodyn. 2017, 36, 1243–1260. [Google Scholar] [CrossRef]
- Nolte, S.; Liegl, G.; Petersen, M.A.; Aaronson, N.K.; Costantini, A.; Fayers, P.M.; Groenvold, M.; Holzner, B.; Johnson, C.D.; Kemmler, G.; et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur. J. Cancer 2019, 107, 153–163. [Google Scholar] [CrossRef]
- Leandri, P.; Rossignol, G.; Gautier, J.R.; Quintens, H.; Lasserre, E.; Caissel, J. Ileal low-pressure bladder replacement: Camey type II. Stapling technique and preliminary results (57 cases, 1987–1989). Eur. Urol. 1990, 18, 161–165. [Google Scholar]
- Hinman, F., Jr. Selection of intestinal segments for bladder substitution: Physical and physiological characteristics. J. Urol. 1988, 139, 519–523. [Google Scholar] [CrossRef]
- Hautmann, R.E.; Volkmer, B.G.; Schumacher, M.C.; Gschwend, J.E.; Studer, U.E. Long-term results of standard procedures in urology: The ileal neobladder. World J. Urol. 2006, 24, 305–314. [Google Scholar] [CrossRef]
- Murray, K.S.; Arther, A.R.; Zuk, K.P.; Lee, E.K.; Lopez-Corona, E.; Holzbeierlein, J.M. Can we predict the need for clean intermittent catheterization after orthotopic neobladder construction? Indian J. Urol. 2015, 31, 333–338. [Google Scholar] [CrossRef] [PubMed]



| Baseline Characteristics |
|---|
|
| Functional parameters |
|
| Free uroflowmetry |
|
| UDS parameters |
|
| Authors | Years of Pubblications | Type of The Studies | Main Study Endpoints | N° of Patients | IRB Approval * | Continence Data | UDS Data ** |
|---|---|---|---|---|---|---|---|
| M Apostolos et al. [7] | 2015 | Retrospective study | To determine accuracy of UDS in neobladder | 32 | No | Yes | Yes |
| X Zhou et al. [8] | 2020 | Randomized Clinical trial | Perioperative and function outcome intracorporeal ONB | 40 | Yes | Yes | Yes |
| Y N Niu et al. [9] | 2010 | Abstract | To evaluate function and upper tract functioning in T neobladder series | 90 | No | Yes | Yes |
| M Porena et al. [10] | 2012 | Retrospective longitudinal study | Long—term functional outcome on ON | 237 | No | Yes | Yes |
| J B Jensen et al. [11] | 2006 | Retrospective study | Complication and functional outcome of the Hautmann neobladder | 67 | No | Yes | Yes |
| U P Singh et al. [12] | 2019 | Prospective study | Short term voiding and urodynamic outcome of W shaped iON | 41 | No | Yes | Yes |
| R Satkunasivam et al. [13] | 2015 | Prospective study | Functional, QoL and bladder cancer specific features of iONB | 107 | Yes | Yes | Yes |
| H Zhong et al. [14] | 2019 | Retrospective study | UDS and QoL outcome in iON with orthotopic ureteral reimplantation | 72 | Yes | Yes | Yes |
| R K Shimpi et al. [15] | 2021 | Prospective single center study | To evaluate Frog ileal neobladder | 120 | Yes | Yes | Yes |
| D Fontana et al. [16] | 2004 | Retrospective study | Clinical and functional outcome of Y shaped ON | 53 | No | Yes | Yes |
| T Koie et al. [17] | 2006 | Retrospective study | Advantage of the Goodwin method in modified ON | 95 | No | Yes | No |
| H A El—Helaly et al. [18] | 2019 | Retrospective study | Clinical outcomes between sigmoid and ileal neobladder | 27 | No | Yes | Yes |
| Z Zhang et al. [19] | 2013 | Retrospective study | UDS of N shaped ileal neobladder for 12 months | 52 | No | Yes | Yes |
| Grobet-Jeandin E et al. [20] | 2021 | Retrospective observational study | Urodynamic assessment and quality of life outcomes in a rONB | 14 | Yes | Yes | Yes |
| Y R Barapatre et al. [21] | 2013 | Prospective study | UDS outcome of W shaped iON with serosa—lined tunnel uretero—ileal anastomosis | 17 | Yes | Yes | Yes |
| V Singh et al. [22] | 2014 | Prospective non randomized trial | UDS and functional outcomes in orthotopic sigmoid vs. iON | 44 | Yes | Yes | Yes |
| Checcucci E et al. [23] | 2021 | Prospective controlled trial | Postoperative complications and functional and UDS outcomes in a case series | 90 | No | Yes | Yes |
| G Marim et al. [24] | 2007 | Retrospective Follow—up study | Long term functional outcomes and UDS of W—shaped iON | 20 | No | Yes | Yes |
| S S Yadav et al. [25] | 2016 | Prospective study | Long term functional, urodynamic, and metabolic outcomes of neobladder | 42 | Yes | Yes | Yes |
| T Koie et al. [26] | 2010 | Retrospective cohort study | Oncological and voiding functional outcomes after ON | 30 | No | Yes | Yes |
| G Muto et al. [27] | 2016 | Retrospective study | Outcomes of large series of stapled ileal orthotopic neobladder | 606 | No | Yes | Yes |
| A Khan et al. [28] | 2021 | Retrospective study | Functional outcomes of intracorporeal vs. extracorporeal neobladder | 40 | No | Yes | Yes |
| G Sevin et al. [29] | 2004 | Retrospective study | 10 years—Clinical, urodynamic, functional, radiological, and metabolic outcomes of ON | 124 | No | Yes | Yes |
| A A Hassan et al. [30] | 2007 | Retrospective follow—up study | Functional results of Y shaped ON with antireflux ureteral reimplantation | 120 | No | Yes | Yes |
| JK Nam et al. [31] | 2013 | Retrospective follow—up study | >10 years postoperatively functional outcomes and UDS in a Studer neobladder | 19 | No | Yes | Yes |
| A Minervini et al. [32] | 2017 | Retrospective study | UDS outcomes in robotic intracorporeal neobladder configuration | 18 | No | Yes | No |
| A E Dellis et al. [33] | 2014 | Prospective study | Continence and urodynamic findings after modified S ileal neobladder | 208 | Yes | Yes | Yes |
| Y Bedük et al. [34] | 2003 | Retrospective follow—up | Clinical and UDS in ileocecal and ileal bladder substitution | 36 | No | Yes | Yes |
| K H Kim et al. [35] | 2017 | Retrospective study | Voiding pattern in patients with orthotopic neobladder | 142 | No | Yes | No |
| K Nagahama et al. [36] | 2002 | Abstract (article in Korean) | Urodynamic and functional outcome in Hautmann ileal neobladder | 19 | No | Yes | No |
| R B dos Reis et al. [37] | 2011 | Retrospective study | ON reconstruction in patients with shortened mesentery | 5 | No | Yes | Yes |
| S Muto et al. [38] | 2007 | Retrospective case control study | Changes in neobladder configuration during real time MRI | 10 | No | No | Yes |
| M Ferriero et al. [39] | 2009 | Retrospective comparative study | Data of Padual ileal neobladder series | 46 | No | Yes | Yes |
| W Wang et al. [40] | 2012 | Retrospective follow—up study | Modified spiral orthotopic ileal neobladder | 51 | Yes | Yes | Yes |
| W M Gamal et al. [41] | 2011 | Retrospective study | Feasibility and outcomes of the N shaped pouch | 42 | No | Yes | Yes |
| W Obara et al. [42] | 2006 | Retrospective study | Feasibility of Studer ON for aged patients | 31 | No | Yes | Yes |
| S Crivellaro et al. [43] | 2009 | Retrospective study | Functional and anatomical differences among three ON using 3D CT and videoUDS | 12 | No | Yes | Yes |
| S Rawal et al. [44] | 2006 | Retrospective study | Initial results of a newly modification of Studer neobladder | 21 | No | Yes | Yes |
| Z Bayraktar et al. [45] | 2001 | Retrospective study | UDS of 8 female patients with iON | 8 | No | Yes | No |
| B Kosevic et al. [46] | 2012 | Prospective clinical trial | UDS of modified orthotopic ileal neobladder | 24 | No | No | Yes |
| C Constantinides et al. [47] | 2001 | Retrospective study | 5-year experience in a modification of S ileal pouch | 43 | No | Yes | Yes |
| M Khafagy et al. [48] | 2006 | Randomized controlled trial | To compare ileocecal orthotopic bladder vs. iON | 29 | No | Yes | No |
| Z Chen et al. [49] | 2009 | Randomized controlled trial | Continence after creation of orthotopic ileocolonic and iON | 38 | No | Yes | Yes |
| G Palleschi et al. [50] | 2015 | Retrospective study | Functional outcome of laparoscopic cystectomy and intracorporeal iON | 30 | No | Yes | Yes |
| D B Fang et al. [51] | 2012 | Retrospective study | Functional result of W ileal neobladder by a hand—assisted- drawing—needle running suture | 347 | No | Yes | Yes |
| B P Schrier et al. [52] | 2005 | Retrospective study | Continence rates and UDS in ileal vs. sigmoid neobladder | 62 | No | Yes | Yes |
| D Wang et al. [53] | 2014 | Prospective observational | UDS after laparoscopic radical cystectomy and iON | 53 | Yes | No | Yes |
| L Song et al. [54] | 2014 | Abstract | Functional outcomes of iON in women | 28 | No | Yes | No |
| P Honeck et al. [55] | 2009 | Retrospective follow—up study | Long term outcomes of sigmoid neobladder vs. iON | 10 | No | Yes | Yes |
| A Skolarikos et al. [56] | 2004 | Retrospective study | Continence status and UDS in ON | 55 | No | Yes | Yes |
| T Koie et al. [57] | 2002 | Retrospective follow—up study | Surgical and functional outcomes using a modified Goodwin technique | 37 | No | Yes | Yes |
| N Caproni et al. [58] | 2006 | Retrospective follow—up study | Morphofunctional evaluation of orthotopic reservoir using TC | 30 | No | No | Yes |
| M S El—Bahnasawy et al. [59] | 2005 | Retrospective study | UDS in patients with detubularized urinary diversion with enuresis | 25 | No | No | Yes |
| M Zyczkowski et al. [60] | 2015 | Randomized Clinical trial open label | Functional result in surgical modification iON | 42 | No | No | Yes |
| S Y Wang et al. [61] | 2012 | Retrospective Follow—up study | Outcome of laparoscopic radical cystectomy | 11 | No | No | Yes |
| K Türkölmez et al. [62] | 2004 | Retrospective study | Outcomes in W—shaped ON using ureteral anastomosis—serous lined extramural tunnel | 42 | No | Yes | No |
| Y Osman et al. [63] | 2004 | Prospective controlled trial | Long term outcomes in two reflux prevention technique in ileal neobladder | 30 | No | Yes | No |
| A Asimakopoulos et al. [64] | 2022 | Prospective clinical study | Urodynamic features and continence of the iYNB and (HRQoL) outcomes | 26 | Yes | Yes | Yes |
| Di Maida F et al. [65] | 2022 | Prospective controlled trial | Functional and urodynamic features of Florin neobladder vs. VIP | 158 | Yes | Yes | Yes |
| Technical Issues | N° (%) | |
|---|---|---|
| Ureteral—neobladder anastomosis | End—to—end | 132 (3.3) |
| Side—to—side | 3620 (91.2) | |
| NA | 215 (5.4) | |
| Antireflux ureter anastomosis | Yes | 1381 (34.8) |
| No | 1322 (33.3) | |
| NA | 1265 (31.9) | |
| Crossing of the left ureter | Yes | 999 (25.2) |
| No | 2821 (71.0) | |
| NA | 148 (3.7) | |
| Stenting of reimplanted ureter | Transabdominal | 505 (12.7) |
| Transurethral | 1633 (41.2) | |
| NA | 1830 (46.1) | |
| Pouch configuration | Suture | 1166 (29.4) |
| Stapler | 1175 (29.6) | |
| NA | 1627 (41.0) | |
| Urethro—neobladder anastomosis | At the start of reconstruction | 137 (54.4) |
| After reconstruction | 1382 (34.8) | |
| NA | 2449 (61.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asimakopoulos, A.D.; Finazzi Agrò, E.; Piechaud, T.; Gakis, G.; Gaston, R.; Rosato, E. Urodynamic Parameters and Continence Outcomes in Asymptomatic Patients with Ileal Orthotopic Neobladder: A Systematic Review and Metanalysis. Cancers 2024, 16, 1253. https://doi.org/10.3390/cancers16071253
Asimakopoulos AD, Finazzi Agrò E, Piechaud T, Gakis G, Gaston R, Rosato E. Urodynamic Parameters and Continence Outcomes in Asymptomatic Patients with Ileal Orthotopic Neobladder: A Systematic Review and Metanalysis. Cancers. 2024; 16(7):1253. https://doi.org/10.3390/cancers16071253
Chicago/Turabian StyleAsimakopoulos, Anastasios D., Enrico Finazzi Agrò, Thierry Piechaud, Georgios Gakis, Richard Gaston, and Eleonora Rosato. 2024. "Urodynamic Parameters and Continence Outcomes in Asymptomatic Patients with Ileal Orthotopic Neobladder: A Systematic Review and Metanalysis" Cancers 16, no. 7: 1253. https://doi.org/10.3390/cancers16071253
APA StyleAsimakopoulos, A. D., Finazzi Agrò, E., Piechaud, T., Gakis, G., Gaston, R., & Rosato, E. (2024). Urodynamic Parameters and Continence Outcomes in Asymptomatic Patients with Ileal Orthotopic Neobladder: A Systematic Review and Metanalysis. Cancers, 16(7), 1253. https://doi.org/10.3390/cancers16071253





