Association of Insulin-like Growth Factor-1 with Bone Mineral Density in Survivors of Childhood Acute Leukemia
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Clinical Data
2.3. Biochemical Parameters
2.4. Radiological Data
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients
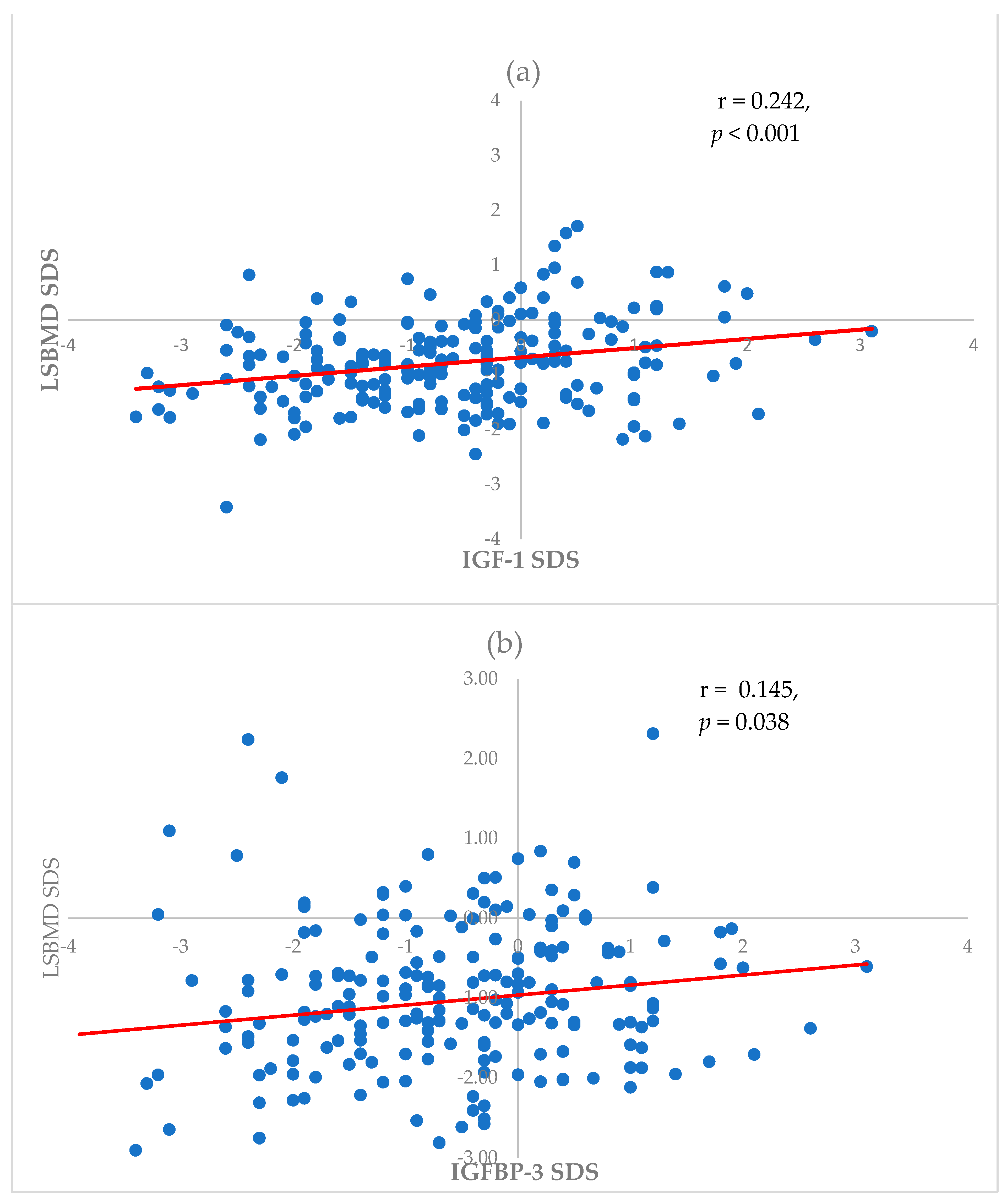
3.2. Association of LSBMD SDS with Baseline Characteristics, Bone Markers, and IGF-1
3.3. Risk Factors Associated with Low BMD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, H.J.; Moon, E.K.; Yoon, J.Y.; Oh, C.M.; Jung, K.W.; Park, B.K.; Shin, H.Y.; Won, Y.J. Incidence and Survival of Childhood Cancer in Korea. Cancer Res. Treat. 2016, 48, 869–882. [Google Scholar] [CrossRef] [PubMed]
- van der Sluis, I.M.; van den Heuvel-Eibrink, M.M.; Hahlen, K.; Krenning, E.P.; de Muinck Keizer-Schrama, S.M. Altered bone mineral density and body composition, and increased fracture risk in childhood acute lymphoblastic leukemia. J. Pediatr. 2002, 141, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Mostoufi-Moab, S.; Halton, J. Bone morbidity in childhood leukemia: Epidemiology, mechanisms, diagnosis, and treatment. Curr. Osteoporos. Rep. 2014, 12, 300–312. [Google Scholar] [CrossRef] [PubMed]
- Jang, M.J.; Shin, C.; Kim, S.; Lee, J.W.; Chung, N.-G.; Cho, B.; Jung, M.H.; Suh, B.-K.; Ahn, M.B. Factors affecting bone mineral density in children and adolescents with secondary osteoporosis. Ann. Pediatr. Endocrinol. Metab. 2023, 28, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Mostoufi-Moab, S.; Ward, L.M. Skeletal Morbidity in Children and Adolescents during and following Cancer Therapy. Horm. Res. Paediatr. 2019, 91, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Siminoski, K.; Alos, N.; Halton, J.; Ho, J.; Cummings, E.A.; Shenouda, N.; Matzinger, M.A.; Lentle, B.; Jaremko, J.L.; et al. Impact of Vertebral Fractures and Glucocorticoid Exposure on Height Deficits in Children During Treatment of Leukemia. J. Clin. Endocrinol. Metab. 2019, 104, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Cummings, E.A.; Ma, J.; Fernandez, C.V.; Halton, J.; Alos, N.; Miettunen, P.M.; Jaremko, J.L.; Ho, J.; Shenouda, N.; Matzinger, M.A.; et al. Incident Vertebral Fractures in Children With Leukemia During the Four Years Following Diagnosis. J. Clin. Endocrinol. Metab. 2015, 100, 3408–3417. [Google Scholar] [CrossRef] [PubMed]
- Guss, C.E.; McAllister, A.; Gordon, C.M. DXA in Children and Adolescents. J. Clin. Densitom. 2021, 24, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Wheater, G.; Elshahaly, M.; Tuck, S.P.; Datta, H.K.; van Laar, J.M. The clinical utility of bone marker measurements in osteoporosis. J. Transl. Med. 2013, 11, 201. [Google Scholar] [CrossRef]
- Bishop, N.; Arundel, P.; Clark, E.; Dimitri, P.; Farr, J.; Jones, G.; Makitie, O.; Munns, C.F.; Shaw, N.; International Society of Clinical, D. Fracture prediction and the definition of osteoporosis in children and adolescents: The ISCD 2013 Pediatric Official Positions. J. Clin. Densitom. 2014, 17, 275–280. [Google Scholar] [CrossRef]
- Lee, Y.A.; Kwon, A.; Kim, J.H.; Nam, H.K.; Yoo, J.H.; Lim, J.S.; Cho, S.Y.; Cho, W.K.; Shim, K.S. Clinical practice guidelines for optimizing bone health in Korean children and adolescents. Ann. Pediatr. Endocrinol. Metab. 2022, 27, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Langlois, J.A.; Rosen, C.J.; Visser, M.; Hannan, M.T.; Harris, T.; Wilson, P.W.; Kiel, D.P. Association between insulin-like growth factor I and bone mineral density in older women and men: The Framingham Heart Study. J. Clin. Endocrinol. Metab. 1998, 83, 4257–4262. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Wan, Z.H.; Cheng, S.L.; Michaelsson, K.; Larsson, S.C. Insulin-like Growth Factor-1, Bone Mineral Density, and Fracture: A Mendelian Randomization Study. J. Clin. Endocrinol. Metab. 2021, 106, e1552–e1558. [Google Scholar] [CrossRef] [PubMed]
- Kanazawa, I.; Notsu, M.; Miyake, H.; Tanaka, K.; Sugimoto, T. Assessment using serum insulin-like growth factor-I and bone mineral density is useful for detecting prevalent vertebral fractures in patients with type 2 diabetes mellitus. Osteoporos. Int. 2018, 29, 2527–2535. [Google Scholar] [CrossRef] [PubMed]
- Kawai, M.; Rosen, C.J. The insulin-like growth factor system in bone: Basic and clinical implications. Endocrinol. Metab. Clin. N. Am. 2012, 41, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Rusinska, A.; Chlebna-Sokol, D. Insulin-like growth factor-I and mineral metabolism markers in children with idiopathic decrease in bone mass. Clin. Chim. Acta 2006, 366, 257–263. [Google Scholar] [CrossRef]
- Garnett, S.P.; Hogler, W.; Blades, B.; Baur, L.A.; Peat, J.; Lee, J.; Cowell, C.T. Relation between hormones and body composition, including bone, in prepubertal children. Am. J. Clin. Nutr. 2004, 80, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Moreira-Andrés, M.N.; Papapietro, K.; Cañizo, F.J.; Rejas, J.; Larrodera, L.; Hawkins, F.G. Correlations between bone mineral density, insulin-like growth factor I and auxological variables. Eur. J. Endocrinol. 1995, 132, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Yun, S.; Hwang, S.S.; Shim, J.O.; Chae, H.W.; Lee, Y.J.; Lee, J.H.; Kim, S.C.; Lim, D.; Yang, S.W.; et al. The 2017 Korean National Growth Charts for children and adolescents: Development, improvement, and prospects. Korean J. Pediatr. 2018, 61, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Hyun, S.E.; Lee, B.C.; Suh, B.K.; Chung, S.C.; Ko, C.W.; Kim, H.S.; Lee, K.H.; Yang, S.W.; Shin, C.H.; Hwang, J.S.; et al. Reference values for serum levels of insulin-like growth factor-I and insulin-like growth factor binding protein-3 in Korean children and adolescents. Clin. Biochem. 2012, 45, 16–21. [Google Scholar] [CrossRef]
- Yang, L.; Grey, V. Pediatric reference intervals for bone markers. Clin. Biochem. 2006, 39, 561–568. [Google Scholar] [CrossRef]
- Cho, S.-M.; Lee, S.-G.; Kim, H.S.; Kim, J.-H. Establishing pediatric reference intervals for 13 biochemical analytes derived from normal subjects in a pediatric endocrinology clinic in Korea. Clin. Biochem. 2014, 47, 268–271. [Google Scholar] [CrossRef]
- Genant, H.K.; Wu, C.Y.; van Kuijk, C.; Nevitt, M.C. Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 1993, 8, 1137–1148. [Google Scholar] [CrossRef] [PubMed]
- Yi, K.H.; Hwang, J.S.; Kim, E.Y.; Lee, J.A.; Kim, D.H.; Lim, J.S. Reference values for bone mineral density according to age with body size adjustment in Korean children and adolescents. J. Bone Miner. Metab. 2013, 32, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Heaney, R.P.; Abrams, S.; Dawson-Hughes, B.; Looker, A.; Marcus, R.; Matkovic, V.; Weaver, C. Peak bone mass. Osteoporos. Int. 2000, 11, 985–1009. [Google Scholar] [CrossRef] [PubMed]
- Paviglianiti, A. Endocrine and Metabolic Disorders after Hematopoietic Cell Transplantation. Turk. J. Haematol. 2020, 37, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.M.; Ma, J.; Lang, B.; Ho, J.; Alos, N.; Matzinger, M.A.; Shenouda, N.; Lentle, B.; Jaremko, J.L.; Wilson, B.; et al. Bone Morbidity and Recovery in Children with Acute Lymphoblastic Leukemia: Results of a Six-Year Prospective Cohort Study. J. Bone Miner. Res. 2018, 33, 1435–1443. [Google Scholar] [CrossRef] [PubMed]
- Geusens, P.P.; Boonen, S. Osteoporosis and the growth hormone-insulin-like growth factor axis. Horm. Res. 2002, 58 (Suppl. S3), 49–55. [Google Scholar] [CrossRef] [PubMed]
- Garnero, P.; Sornay-Rendu, E.; Delmas, P.D. Low serum IGF-1 and occurrence of osteoporotic fractures in postmenopausal women. Lancet 2000, 355, 898–899. [Google Scholar] [CrossRef]
- Vandenput, L.; Sjogren, K.; Svensson, J.; Ohlsson, C. The role of IGF-1 for fracture risk in men. Front. Endocrinol. 2012, 3, 51. [Google Scholar] [CrossRef]
- Swolin-Eide, D.; Andersson, B.; Hellgren, G.; Magnusson, P.; Albertsson-Wikland, K. Variation of bone acquisition during growth hormone treatment in children can be explained by proteomic biomarkers, bone formation markers, body composition and nutritional factors. Bone 2018, 116, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Lanes, R.; Gunczler, P.; Esaa, S.; Weisinger, J.R. The effect of short- and long-term growth hormone treatment on bone mineral density and bone metabolism of prepubertal children with idiopathic short stature: A 3-year study. Clin. Endocrinol. 2002, 57, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Savendahl, L.; Polak, M.; Backeljauw, P.; Blair, J.C.; Miller, B.S.; Rohrer, T.R.; Hokken-Koelega, A.; Pietropoli, A.; Kelepouris, N.; Ross, J. Long-Term Safety of Growth Hormone Treatment in Childhood: Two Large Observational Studies: NordiNet IOS and ANSWER. J. Clin. Endocrinol. Metab. 2021, 106, 1728–1741. [Google Scholar] [CrossRef] [PubMed]
- Pollock, N.I.; Cohen, L.E. Growth Hormone Deficiency and Treatment in Childhood Cancer Survivors. Front. Endocrinol. 2021, 12, 745932. [Google Scholar] [CrossRef] [PubMed]
- Shin, C.; Jang, M.J.; Kim, S.; Lee, J.W.; Chung, N.-G.; Cho, B.; Jung, M.H.; Suh, B.-K.; Ahn, M.B. Short-term effect of growth hormone treatment in childhood leukemia survivors with growth hormone deficiency. Ann. Pediatr. Endocrinol. Metab. 2023, 28, 116–123. [Google Scholar] [CrossRef] [PubMed]
- van der Sluis, I.M.; Boot, A.M.; Nauta, J.; Hop, W.C.; de Jong, M.C.; Lilien, M.R.; Groothoff, J.W.; van Wijk, A.E.; Pols, H.A.; Hokken-Koelega, A.C.; et al. Bone density and body composition in chronic renal failure: Effects of growth hormone treatment. Pediatr. Nephrol. 2000, 15, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Van Dyck, M.; Gyssels, A.; Proesmans, W.; Nijs, J.; Eeckels, R. Growth hormone treatment enhances bone mineralisation in children with chronic renal failure. Eur. J. Pediatr. 2001, 160, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Sklar, C.A.; Antal, Z.; Chemaitilly, W.; Cohen, L.E.; Follin, C.; Meacham, L.R.; Murad, M.H. Hypothalamic-Pituitary and Growth Disorders in Survivors of Childhood Cancer: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2018, 103, 2761–2784. [Google Scholar] [CrossRef] [PubMed]
- Ciancia, S.; Hogler, W.; Sakkers, R.J.B.; Appelman-Dijkstra, N.M.; Boot, A.M.; Sas, T.C.J.; Renes, J.S. Osteoporosis in children and adolescents: How to treat and monitor? Eur. J. Pediatr. 2023, 182, 501–511. [Google Scholar] [CrossRef]
- Simm, P.J.; Biggin, A.; Zacharin, M.R.; Rodda, C.P.; Tham, E.; Siafarikas, A.; Jefferies, C.; Hofman, P.L.; Jensen, D.E.; Woodhead, H.; et al. Consensus guidelines on the use of bisphosphonate therapy in children and adolescents. J. Paediatr. Child. Health 2018, 54, 223–233. [Google Scholar] [CrossRef]
- Khosla, S.; Bilezikian, J.P.; Dempster, D.W.; Lewiecki, E.M.; Miller, P.D.; Neer, R.M.; Recker, R.R.; Shane, E.; Shoback, D.; Potts, J.T. Benefits and risks of bisphosphonate therapy for osteoporosis. J. Clin. Endocrinol. Metab. 2012, 97, 2272–2282. [Google Scholar] [CrossRef] [PubMed]
- Joseph, F.; Ahmad, A.M.; Ul-Haq, M.; Durham, B.H.; Whittingham, P.; Fraser, W.D.; Vora, J.P. Effects of growth hormone administration on bone mineral metabolism, PTH sensitivity and PTH secretory rhythm in postmenopausal women with established osteoporosis. J. Bone Miner. Res. 2008, 23, 721–729. [Google Scholar] [CrossRef] [PubMed]
- Wüster, C.; Härle, U.; Rehn, U.; Müller, C.; Knauf, K.; Köppler, D.; Schwabe, C.; Ziegler, R. Benefits of growth hormone treatment on bone metabolism, bone density and bone strength in growth hormone deficiency and osteoporosis. Growth Horm. IGF Res. 1998, 8 (Suppl. A), 87–94. [Google Scholar] [CrossRef] [PubMed]
- Bikle, D.D.; Tahimic, C.; Chang, W.; Wang, Y.; Philippou, A.; Barton, E.R. Role of IGF-I signaling in muscle bone interactions. Bone 2015, 80, 79–88. [Google Scholar] [CrossRef]
- Clegg, A.; Hassan-Smith, Z. Frailty and the endocrine system. Lancet Diabetes Endocrinol. 2018, 6, 743–752. [Google Scholar] [CrossRef]
| Male (n = 120) | Female (n = 94) | p-Value | |
|---|---|---|---|
| At leukemia diagnosis | |||
| Age, year | 8.31 ± 4.093 | 8.47 ± 4.415 | 0.777 |
| Height SDS | 0.31 ± 2.518 | 0.05 ± 2.382 | 0.461 |
| Weight SDS | 0.06 ± 2.392 | 0.10 ± 1.952 | 0.902 |
| BMI SDS | −0.05 ± 1.371 | −0.05 ± 1.437 | 0.980 |
| Leukemia category | |||
| Lymphoblastic | 92 (76.7%) | 69 (73.4%) | 0.562 |
| Myeloid | 25 (20.8%) | 25 (26.6%) | 0.323 |
| Juvenile myelomonocytic | 3 (2.5%) | 0 (0) | 0.123 |
| Transplantation, n (%) | 58 (55.2%) | 47 (50%) | 0.891 |
| Total body irradiation | 43 (36.4%) | 32 (35.2%) | 0.849 |
| At DXA examination | |||
| Age | 12.50 ± 3.335 | 12.65 ± 3.403 | 0.763 |
| BMI SDS | 0.018 ± 2.450 | 0.018 ± 1.540 | 0.998 |
| IGF-1 SDS | −0.651 ± 0.769 | −0.971 ± 0.813 | 0.040 |
| IGFBP3 SDS | −0.897 ± 1.215 | −1.142 ± 1.110 | 0.140 |
| aBMD, g/cm2 | 0.825 ± 0.189 | 0.853 ± 0.213 | 0.407 |
| LSBMD SDS | −0.683 ± 1.556 | −0.616 ± 1.363 | 0.973 |
| Low BMD, n (%) | 15 (12.5%) | 17 (18.1%) | 0.256 |
| VF, n (%) | 30 (25.2%) | 25 (26.9%) | 0.783 |
| Risk Factors | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| β | SE | p-Value | β | SE | p-Value | |
| At leukemia diagnosis | ||||||
| Age | −0.06 | 0.024 | 0.012 | −0.049 | 0.024 | 0.043 |
| BMI SDS | 0.125 | 0.05 | 0.014 | |||
| Transplantation | −0.497 | 0.199 | 0.013 | |||
| TBI | −0.529 | 0.207 | 0.011 | |||
| At DXA examination | ||||||
| BMI SDS | 0.315 | 0.062 | <0.001 | 0.244 | 0.065 | <0.001 |
| Calcium | 0.415 | 0.27 | 0.125 | |||
| 25OHD | 0.003 | 0.011 | 0.967 | |||
| IGF-1 SDS | 0.154 | 0.059 | 0.010 | 0.124 | 0.06 | 0.041 |
| IGFBP-3 SDS | 0.054 | 0.057 | 0.347 | |||
| LSBMD SDS ≤ −2.0 (n = 32) | LSBMD SDS > −2.0 (n = 182) | p-Value | |
|---|---|---|---|
| Age at leukemia diagnosis | 9.53 ± 3.750 | 8.18 ± 4.247 | 0.092 |
| Transplantation | 21 (65.6%) | 84 (46.2%) | 0.055 |
| TBI | 16 (51.6%) | 59 (33.1%) | 0.067 |
| Height SDS | −1.278 ± 1.450 | −0.235 ± 1.340 | <0.001 |
| Weight SDS | −1.319 ± 1.742 | 0.028 ± 1.860 | <0.001 |
| BMI SDS | −0.838 ± 1.936 | 0.168 ± 2.088 | 0.012 |
| Calcium (mg/dL) | 9.30 ± 0.420 | 9.43 ± 0.376 | 0.075 |
| Phosphorus (mg/dL) | 4.22 ± 0.687 | 4.47 ± 0.646 | 0.043 |
| ALP (U/L) | 158.28 ± 88.935 | 167.16 ± 94.497 | 0.639 |
| Bone-specific ALP (µg/L) | 60.83 ± 43.205 | 60.12 ± 39.029 | 0.960 |
| Calcitriol (ng/mL) | 109.62 ± 452.432 | 21.04 ± 10.053 | 0.337 |
| PTH (pg/mL) | 39.93 ± 17.913 | 45.87 ± 25.528 | 0.461 |
| IGF-1 SDS | −1.23 ± 0.817 | −0.72 ± 0.779 | 0.001 |
| IGFBP-3 SDS | −1.16 ± 1.732 | −0.92 ± 1.777 | 0.494 |
| aBMD (g/cm2) | 0.702 ± 0.151 | 0.860 ± 0.199 | <0.001 |
| Risk Factors | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Exp(B) | 95% CI | p-Value | Exp(B) | 95% CI | p-Value | |
| At leukemia diagnosis | ||||||
| Age | 1.081 | 0.987–1.183 | 0.092 | |||
| BMI SDS | 0.098 | 0.800–1.200 | 0.842 | |||
| Transplantation | 2.227 | 1.015–4.886 | 0.046 | 1.493 | 0.595–3.482 | 0.419 |
| TBI | 2.151 | 0.215–1.004 | 0.051 | |||
| At DXA examination | ||||||
| BMI SDS | 0.64 | 0.486–0.844 | 0.002 | 0.674 | 0.504–0.901 | 0.008 |
| Calcium | 0.41 | 0.153–1.101 | 0.077 | |||
| 25OHD | 0.98 | 0.935–1.027 | 0.403 | |||
| IGF-1 SDS | 0.759 | 0.599–0.963 | 0.023 | 0.762 | 0.584–0.994 | 0.045 |
| IGFBP-3 SDS | 0.921 | 0.730–1.163 | 0.490 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Yoo, J.W.; Lee, J.W.; Jung, M.H.; Cho, B.; Suh, B.-K.; Ahn, M.B.; Chung, N.-G. Association of Insulin-like Growth Factor-1 with Bone Mineral Density in Survivors of Childhood Acute Leukemia. Cancers 2024, 16, 1296. https://doi.org/10.3390/cancers16071296
Kim S, Yoo JW, Lee JW, Jung MH, Cho B, Suh B-K, Ahn MB, Chung N-G. Association of Insulin-like Growth Factor-1 with Bone Mineral Density in Survivors of Childhood Acute Leukemia. Cancers. 2024; 16(7):1296. https://doi.org/10.3390/cancers16071296
Chicago/Turabian StyleKim, Seulki, Jae Won Yoo, Jae Wook Lee, Min Ho Jung, Bin Cho, Byng-Kyu Suh, Moon Bae Ahn, and Nack-Gyun Chung. 2024. "Association of Insulin-like Growth Factor-1 with Bone Mineral Density in Survivors of Childhood Acute Leukemia" Cancers 16, no. 7: 1296. https://doi.org/10.3390/cancers16071296
APA StyleKim, S., Yoo, J. W., Lee, J. W., Jung, M. H., Cho, B., Suh, B.-K., Ahn, M. B., & Chung, N.-G. (2024). Association of Insulin-like Growth Factor-1 with Bone Mineral Density in Survivors of Childhood Acute Leukemia. Cancers, 16(7), 1296. https://doi.org/10.3390/cancers16071296








