Processing and Quality Control of Masks: A Review
Abstract
:1. Introduction
2. Types of Applied Materials in Face Mask Production
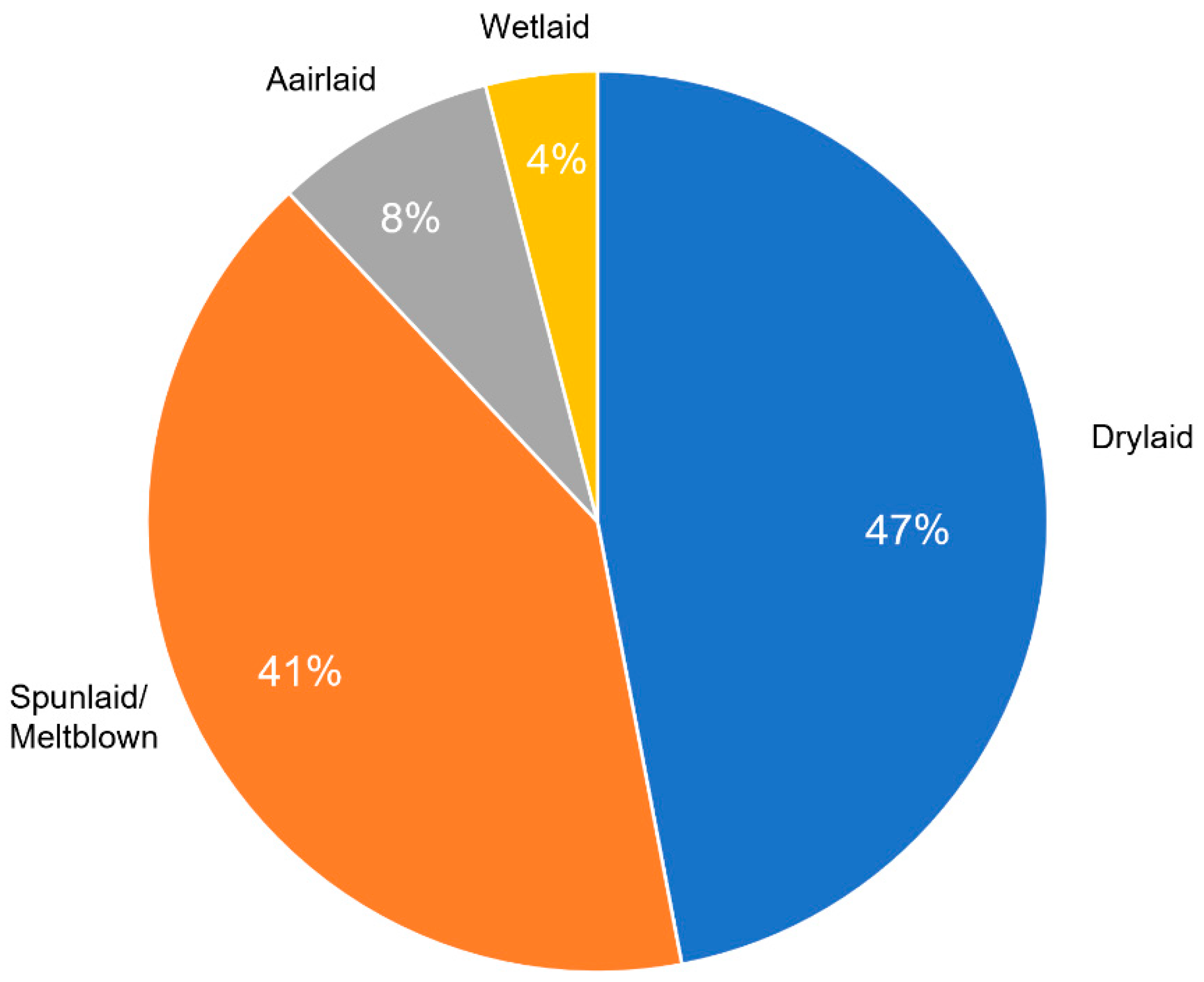
Characteristic of Non-Woven Fabrics
3. Classification of Face Masks
4. Primary Techniques of Processing
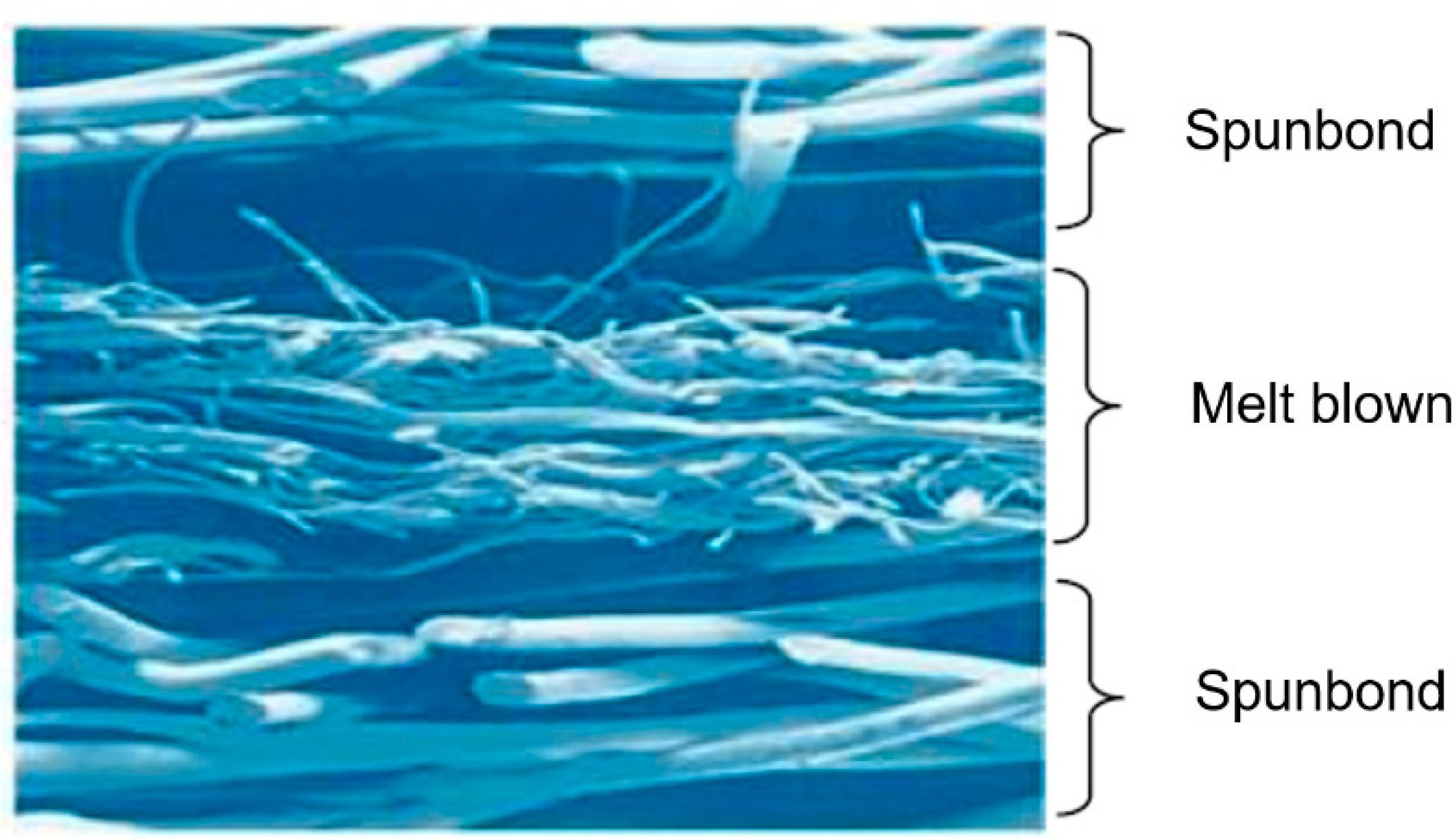
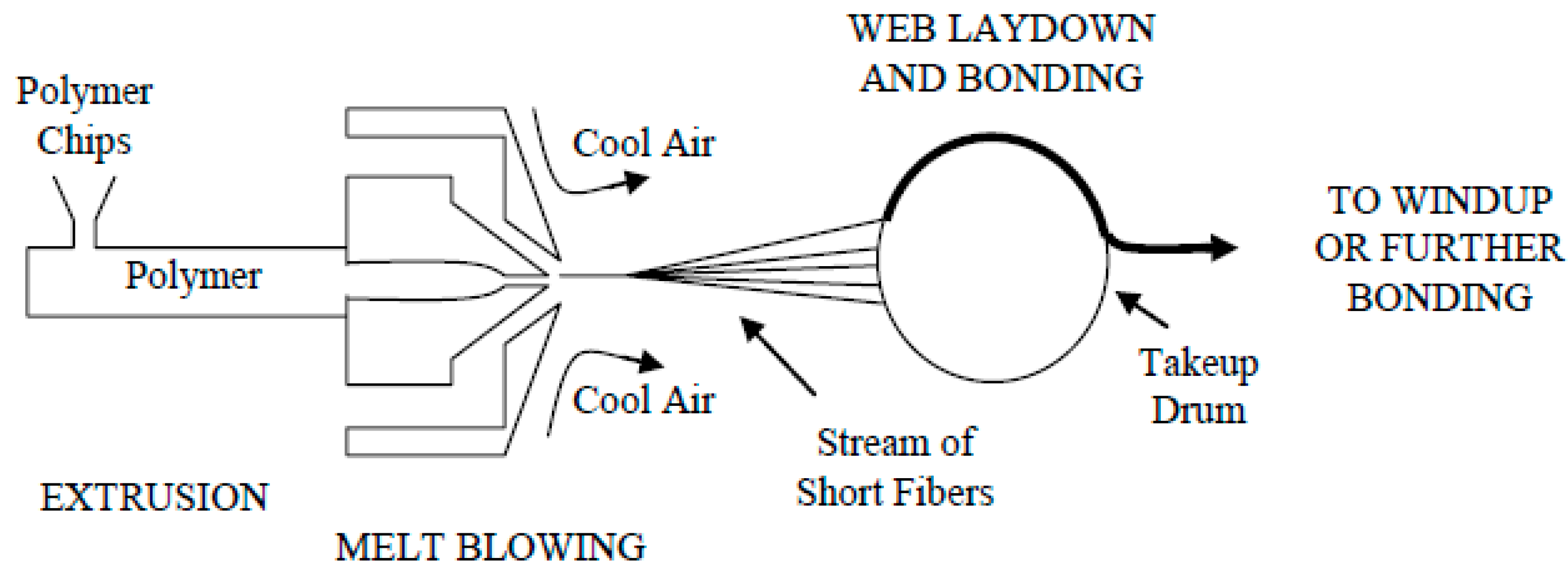
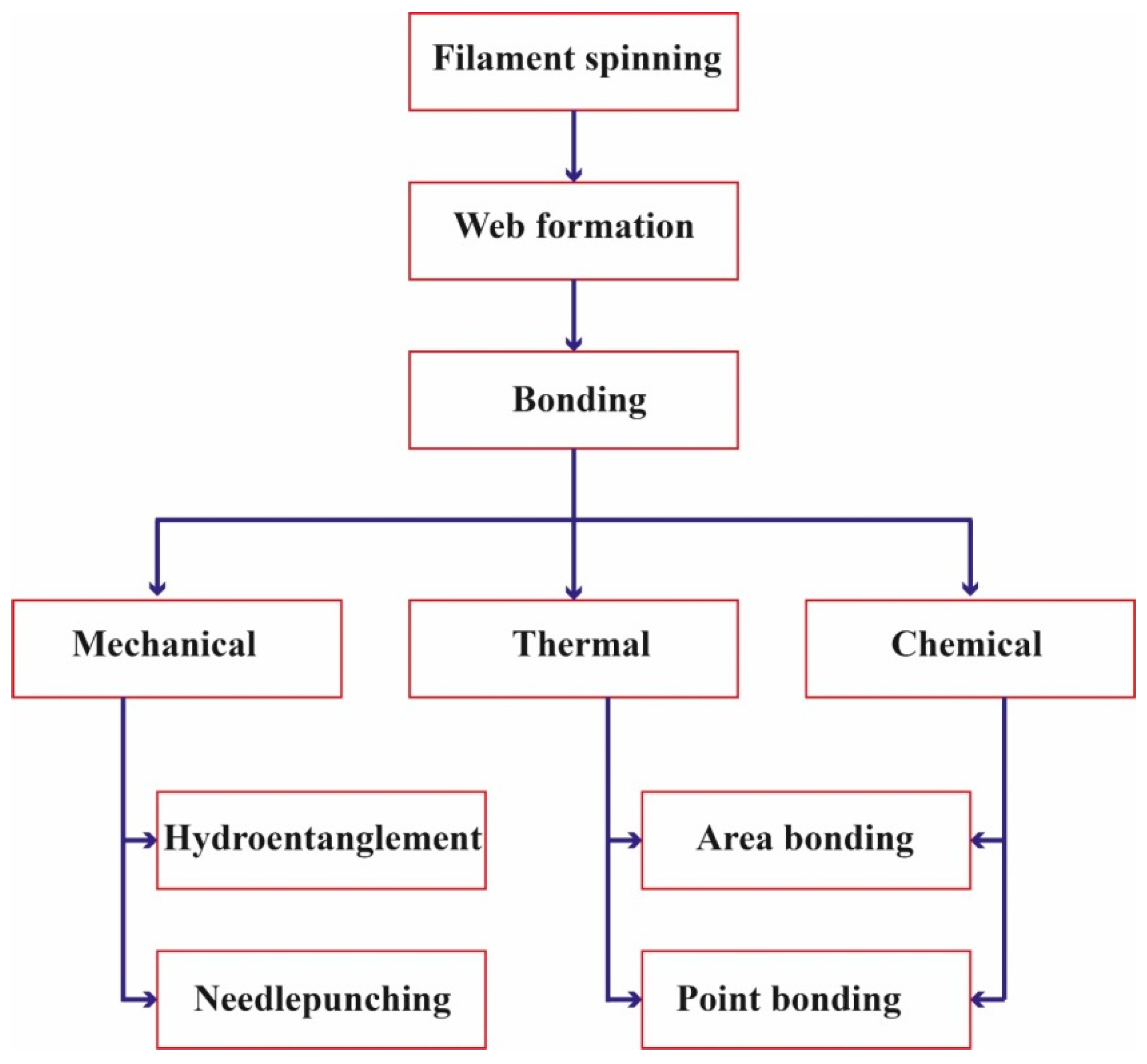
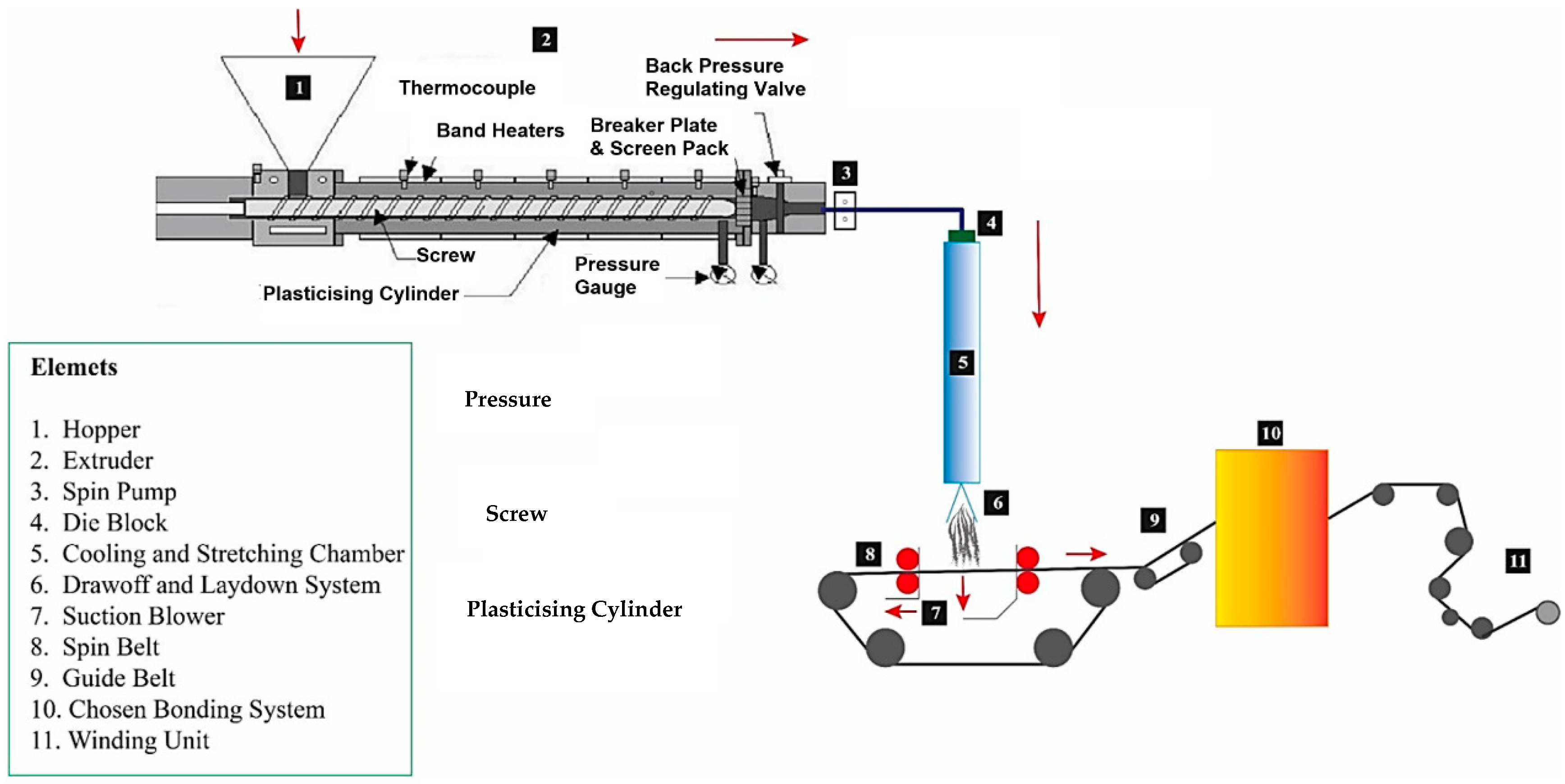
4.1. Meltblown Process and Spunlaid Technology
4.2. Meltblown Process
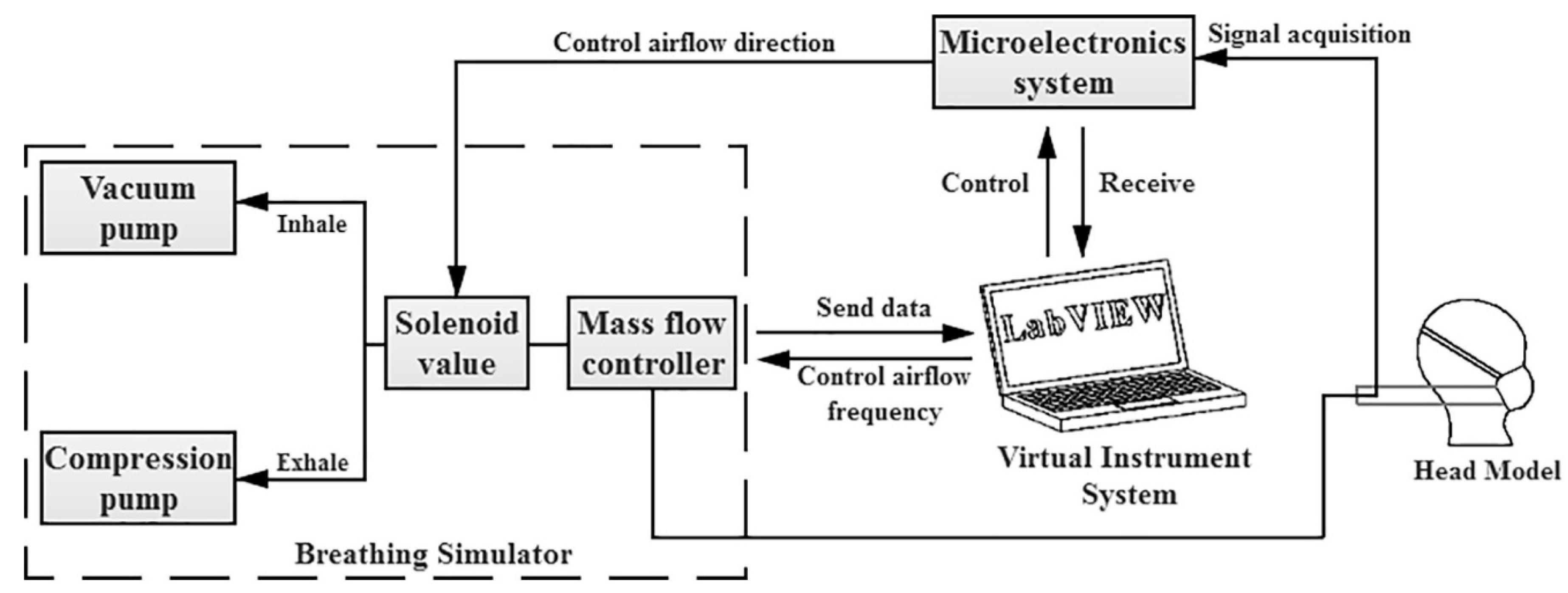
4.3. Drylaid Technology
4.4. Wetlaid and Airlaid Technology
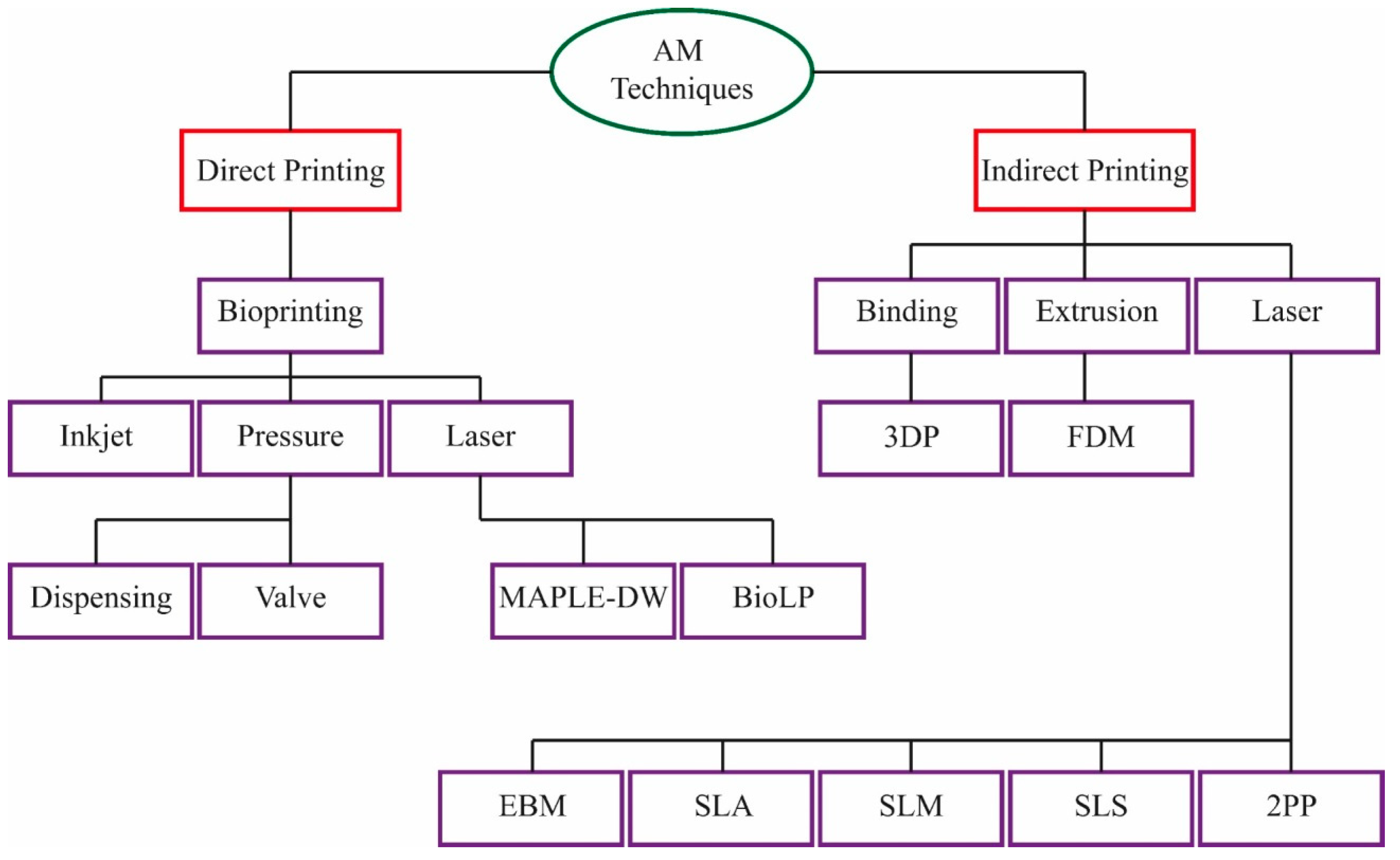
5. Additive Manufacturing (AM) of Face Masks
6. Standards in Quality Controls of Face Masks
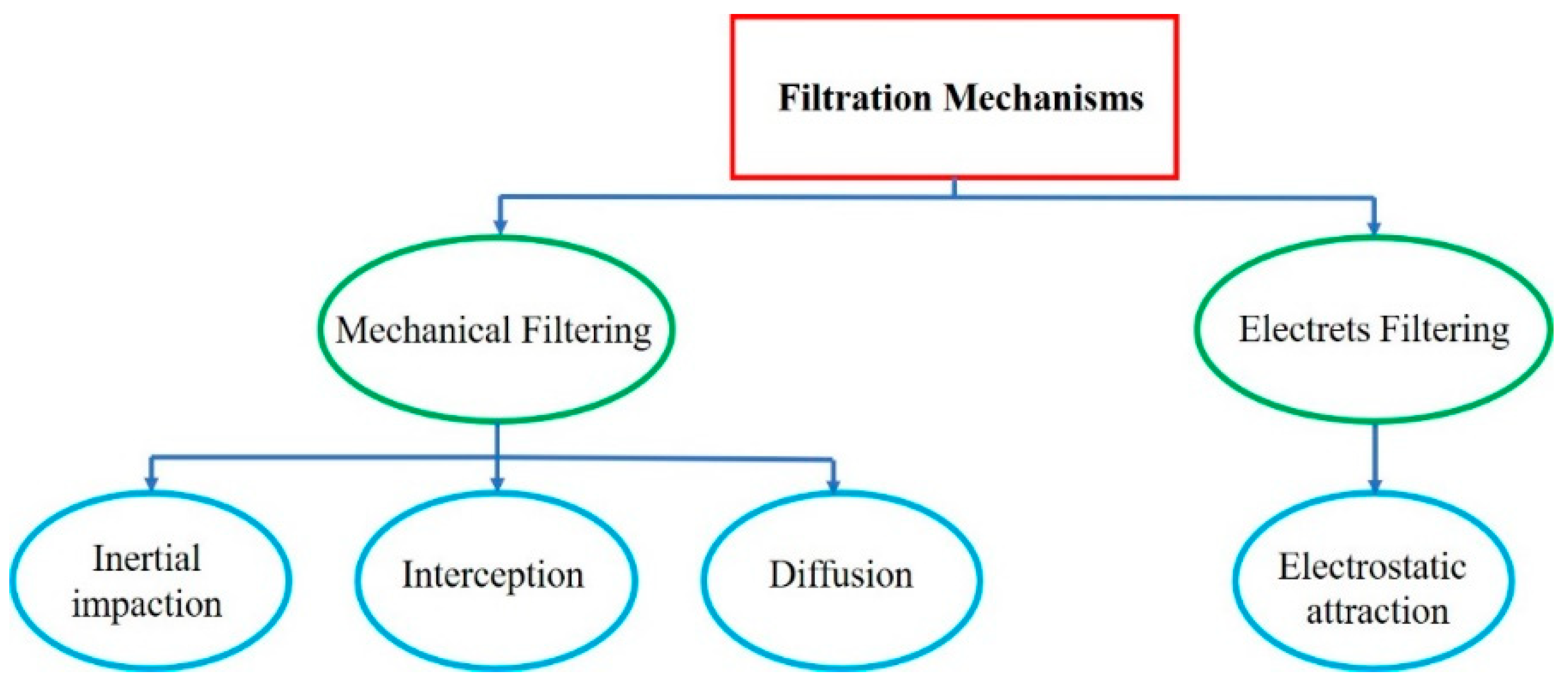
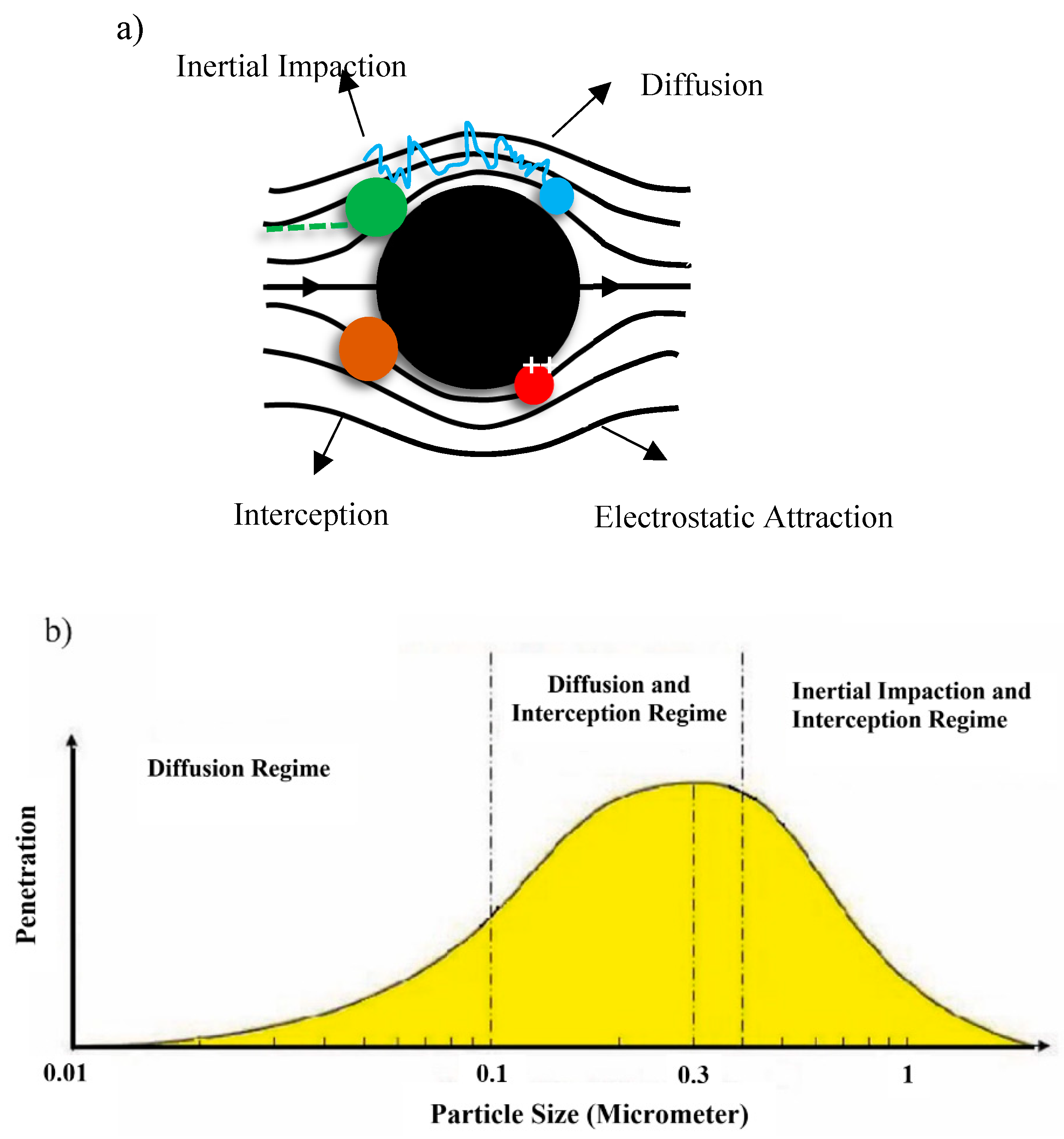
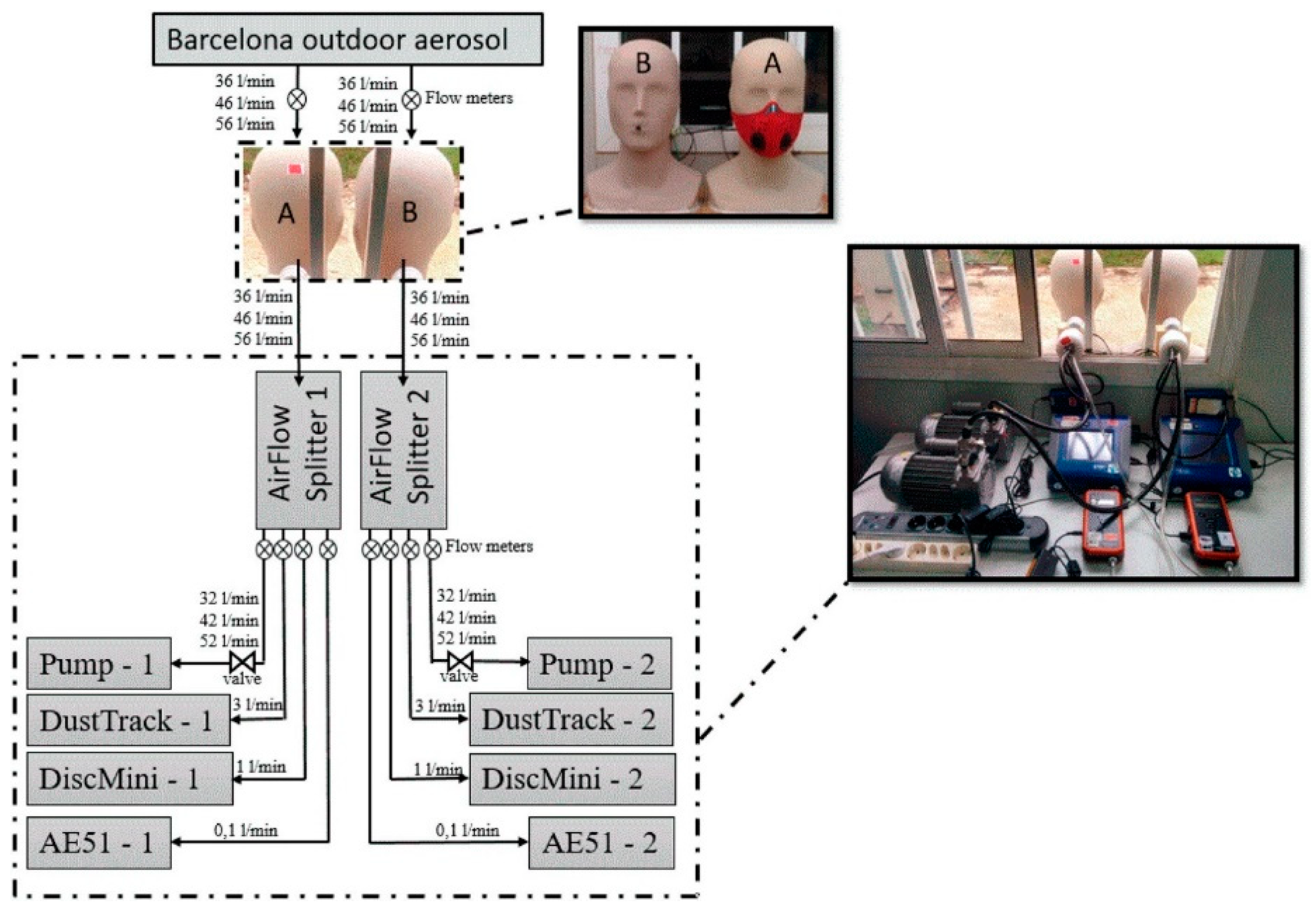
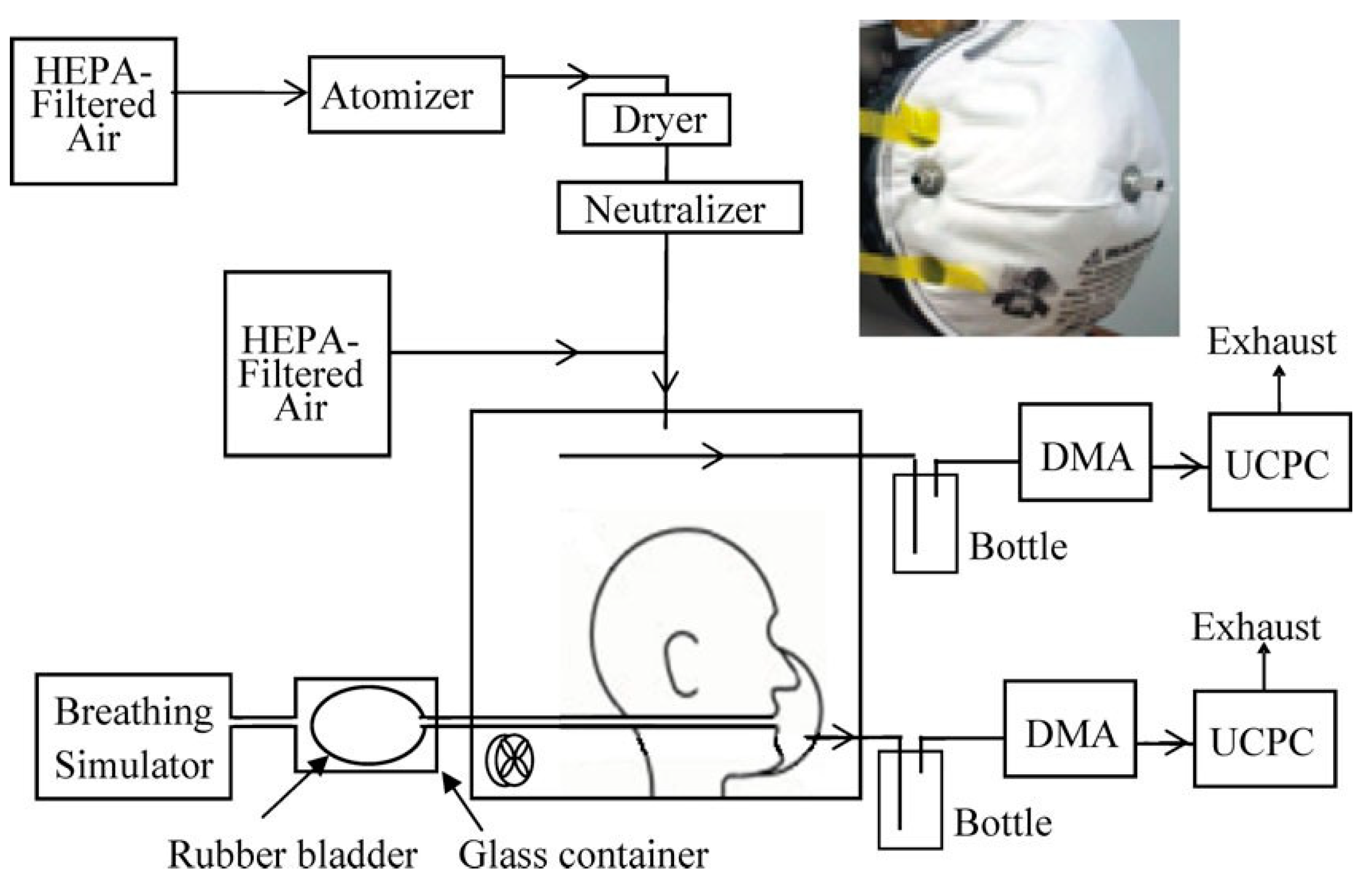
7. Filtration Performance (FP) Tests
8. Leakage Test
9. Dynamic Breathing Resistance (DBR) Test
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tcharkhtchi, A.; Abbasnezhad, N.; Seydani, M.Z.; Zirak, N.; Farzaneh, S.; Shirinbayan, M. An overview of filtration efficiency through the masks: Mechanisms of the aerosols penetration. Bioact. Mater. 2021, 6, 106–122. [Google Scholar] [CrossRef] [PubMed]
- Montano, L.; Donato, F.; Bianco, P.M.; Lettieri, G.; Guglielmino, A.; Motta, O.; Bonapace, I.M.; Piscopo, M. Semen quality as a potential susceptibility indicator to SARS-CoV-2 insults in polluted areas. Environ. Sci. Pollut. Res. 2021, 28, 37031–37040. [Google Scholar] [CrossRef] [PubMed]
- Montano, L.; Donato, F.; Bianco, P.; Lettieri, G.; Guglielmino, A.; Motta, O.; Bonapace, I.; Piscopo, M. Air pollution and COVID-19: A possible dangerous synergy for male fertility. Int. J. Environ. Res. Public Health 2021, 18, 6846. [Google Scholar] [CrossRef] [PubMed]
- Bunyan, D.; Ritchie, L.; Jenkins, D.; Coia, J.E. Respiratory and facial protection: A critical review of recent literature. J. Hosp. Infect. 2013, 85, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Aragaw, T.A. Surgical face masks as a potential source for microplastic pollution in the COVID-19 scenario. Mar. Pollut. Bull. 2020, 159, 111517. [Google Scholar] [CrossRef]
- Akalin, M.; Usta, I.; Kocak, D.; Ozen, M.S. Investigation of the filtration properties of medical masks. Med. Healthc. Text. 2010, 93–97. [Google Scholar] [CrossRef]
- Mahdavi, A. Efficiency Measurement of N95 Filtering Facepiece Respirators against Ultrafine Particles under Cyclic and Constant Flows; Concordia University: Montreal, QC, Canada, 2013. [Google Scholar]
- Smith, J.D.; MacDougall, C.C.; Johnstone, J.; Copes, R.A.; Schwartz, B.; Garber, G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: A systematic review and meta-analysis. Cmaj Can. Med. Assoc. 2016, 188, 567–574. [Google Scholar] [CrossRef] [Green Version]
- Yuasa, H.; Kumita, M.; Honda, T.; Kimura, K.; Nozaki, K.; Emi, H.; Otani, Y. Breathing simulator of workers for respirator performance test. Ind. Health 2014. [Google Scholar] [CrossRef] [Green Version]
- O’Dowd, K.; Nair, K.M.; Forouzandeh, P.; Mathew, S.; Grant, J.; Moran, R.; Bartlett, J.; Bird, J.; Pillai, S.C. Face masks and respirators in the fight against the COVID-19 pandemic: A review of current materials, advances and future perspectives. Materials 2020, 13, 3363. [Google Scholar] [CrossRef]
- Chellamani, K.P.; Veerasubramanian, D.; Balaji, R.S.V. Surgical face masks: Manufacturing methods and classification. J. Acad. Ind. Res. 2013, 2, 320–324. [Google Scholar]
- Kocak, D.; Akalin, M.; Usta, I.; Merdan, N. New approach to produce absorbent pads for new end uses. Med. Text. Biomater. Healthc. 2006, 320–326. [Google Scholar] [CrossRef]
- Hall, D.M.; Adanur, S.; Broughton, RM., Jr. Natural and man made fibers. In Wellingt Sears Handb Ind Text, 1st ed.; CRC Press New Holland: Boca Rat, FL, USA, 1995; pp. 37–52. [Google Scholar]
- Lou, C.-W.; Lin, C.-W.; Chen, Y.-S.; Yao, C.-H.; Lin, Z.-S.; Chao, C.-Y.; Lin, J.-H. Properties evaluation of tencel/cotton nonwoven fabric coated with chitosan for wound dressing. Text. Res. J. 2008, 78, 248–253. [Google Scholar] [CrossRef]
- Dias, T. Electronic Textiles: Smart Fabrics and Wearable Technology; Woodhead Publishing: Sawston, UK, 2015. [Google Scholar]
- Karthik, T.; Rathinamoorthy, R. Nonwovens: Process, Structure, Properties and Applications; WPI Publishing: Worcester, MA, USA, 2017. [Google Scholar]
- Rengasamy, S.; Eimer, B.; Shaffer, R.E. Simple respiratory protection—Evaluation of the filtration performance of cloth masks and common fabric materials against 20–1000 nm size particles. Ann. Occup. Hyg. 2010, 54, 789–798. [Google Scholar] [PubMed] [Green Version]
- Milton, D.K.; Fabian, M.P.; Cowling, B.J.; Grantham, M.L.; McDevitt, J.J. Influenza virus aerosols in human exhaled breath: Particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013, 9, e1003205. [Google Scholar] [CrossRef] [Green Version]
- Bałazy, A.; Toivola, M.; Adhikari, A.; Sivasubramani, S.K.; Reponen, T.; Grinshpun, S.A. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am. J. Infect. Control 2006, 34, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Dreger, R.W.; Jones, R.L.; Petersen, S.R. Effects of the self-contained breathing apparatus and fire protective clothing on maximal oxygen uptake. Ergonomics 2006, 49, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Atangana, E.; Atangana, A. Facemasks simple but powerful weapons to protect against COVID-19 spread: Can they have sides effects? Results Phys. 2020, 19, 103425. [Google Scholar] [CrossRef]
- Ji, D.; Fan, L.; Li, X.; Ramakrishna, S. Addressing the worldwide shortages of face masks. BMC Mater. 2020, 2, 1–11. [Google Scholar] [CrossRef]
- Sipahl, H.; Bayram, F.E.O.; Palabiyik, S.S.; Bayram, D.; Aydin, A. Investigation of the biocompatibility of surgical masks. Pteridines. Sciendo 2018, 29, 80–86. [Google Scholar]
- Suikkanen, T. Analytics for the Modified Kraft Pulps. Master’s Thesis, LUT University, Lappeenranta, Finland, 2015. [Google Scholar]
- Montefusco, A.F. The use of Nonwovens in air filtration. Filtr. Sep. 2005, 42, 30–31. [Google Scholar] [CrossRef]
- Fu, J.; Yamaguchi, M.; Muroga, S.; Tanaka, T.; Okamura, C.; Obi, L.; Kato, K. Development of meltblown non-woven fabric type non-magnetic noise suppressor. In Proceedings of the 2016 Asia-Pacific Symposium on Electromagnetic Compatibility (APEMC), Shenzhen, China, 17–21 May 2016; pp. 656–658. [Google Scholar]
- Malkan, S.R. An overview of spunbonding and meltblowing technologies. Tappi J. 1995, 78, 185–190. [Google Scholar]
- Turbak, A.F. Nonwovens: Theory, Process, Performance, and Testing; TAPPI PRESS: Atlanta, Georgia, 1993. [Google Scholar]
- McCulloch, J.G. The history of the development of melt blowing technology. Int. Nonwovens J. 1999, 1558925099OS-800123. [Google Scholar] [CrossRef] [Green Version]
- Jirsák, O.; Wadsworth, L.C. Nonwoven Textiles; Carolina Academic Press: Durham, NC, USA, 1999. [Google Scholar]
- Červík, R. Netkané Filtrační Textilie pro Čištění Kapalin; Univerzita Tomáše Bati ve Zlíně: Zlin, Czech, 2020. [Google Scholar]
- Dutton, K.C. Overview and analysis of the meltblown process and parameters. J. Text. Apparel. Technol. Manag. 2009, 6. [Google Scholar]
- Drabek, J.; Zatloukal, M. Meltblown technology for production of polymeric microfibers/nanofibers: A review. Phys. Fluids 2019, 31, 91301. [Google Scholar] [CrossRef]
- Wilson, A. The formation of dry, wet, spunlaid and other types of nonwovens. Appl. Nonwovens Tech. Text. 2010, 3–17. [Google Scholar]
- Lichstein, B.M. The Nonwovens Handbook; INDA, Association of the Nonwoven Fabrics Industry: New York, NY, USA, 1988. [Google Scholar]
- Midha, V.K.; Dakuri, A. Spun bonding technology and fabric properties: A review. J. Text. Eng. Fash. Technol. 2017, 1, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Patel, B.M.; Bhrambhatt, D. Nonwoven technology. Text. Technol. 2008, 1–54. [Google Scholar]
- Rezaie, H.R.; Rizi, H.B.; Khamseh, M.M.R.; Öchsner, A. 3D-Printing Technologies for Dental Material Processing. Rev. Dent. Mater. 2020, 201–210. [Google Scholar]
- Li, L.; Sun, Q.; Bellehumeur, C.; Gu, P. Solid Freeform Fabrication Symposium; The University of Texas at Austin: Austin, Texas, 2001; pp. 400–407. [Google Scholar]
- Gray, R.W.; Baird, D.G.; Bøhn, J.H. Effects of processing conditions on short TLCP fiber reinforced FDM parts. Rapid Prototyp. J. 1998, 4. [Google Scholar] [CrossRef]
- Rezaie, H.R.; Rizi, H.B.; Khamseh, M.M.R.; Öchsner, A. A Review on Dental Materials; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- González-Henríquez, C.M.; Sarabia-Vallejos, M.A.; Rodríguez Hernandez, J. Antimicrobial polymers for additive manufacturing. Int. J. Mol. Sci. 2019, 20, 1210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zuniga, J.M. 3D printed antibacterial prostheses. Appl. Sci. 2018, 8, 1651. [Google Scholar] [CrossRef] [Green Version]
- Zuniga, J.M.; Cortes, A. The role of additive manufacturing and antimicrobial polymers in the COVID-19 pandemic. Expert Rev. Med. Devices 2020, 17, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Barnard, D.L.; Kumaki, Y. Recent developments in anti-severe acute respiratory syndrome coronavirus chemotherapy. Future Virol. 2011, 6, 615–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Branson, R.D. A single ventilator for multiple simulated patients to meet disaster surge. Acad. Emerg. Med. 2006, 13, 1352–1353. [Google Scholar] [CrossRef] [PubMed]
- Borkow, G.; Zhou, S.S.; Page, T.; Gabbay, J. A novel anti-influenza copper oxide containing respiratory face mask. PLoS ONE 2010, 5, e11295. [Google Scholar] [CrossRef] [Green Version]
- Khurana, S.; Singh, P.; Sinha, T.P.; Bhoi, S.; Mathur, P. Low-cost production of handrubs and face shields in developing countries fighting the COVID19 pandemic. Am. J. Infect. Control 2020, 48, 726–727. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, L.; Marcianò, A.; Cicciù, M.; Oteri, G. 3D printing beyond dentistry during COVID 19 epidemic: A technical note for producing connectors to breathing devices. Prosthesis 2020, 2, 46–52. [Google Scholar] [CrossRef] [Green Version]
- Wesemann, C.; Pieralli, S.; Fretwurst, T.; Nold, J.; Nelson, K.; Schmelzeisen, R.; Hellwig, E.; Spies, B.C. 3-D printed protective equipment during COVID-19 pandemic. Materials 2020, 13, 1997. [Google Scholar] [CrossRef]
- Cazon, A.; Aizpurua, J.; Paterson, A.; Bibb, R.; Campbell, R.I. Customised design and manufacture of protective face masks combining a practitioner-friendly modelling approach and low-cost devices for digitising and additive manufacturing: This paper analyses the viability of replacing conventional practice with AM me. Virtual Phys. Prototyp. 2014, 9, 251–261. [Google Scholar] [CrossRef] [Green Version]
- Swennen, G.R.J.; Pottel, L.; Haers, P.E. Custom-made 3D-printed face masks in case of pandemic crisis situations with a lack of commercially available FFP2/3 masks. Int. J. Oral Maxillofac. Surg. 2020, 49, 673–677. [Google Scholar] [CrossRef]
- Provenzano, D.; Rao, Y.J.; Mitic, K.; Obaid, S.N.; Pierce, D.; Huckenpahler, J; Berger, J.; Goyal, S.; Loew, M.H. Rapid Prototyping of Reusable 3D-Printed N95 Equivalent Respirators at the George Washington University; MDPI AG: Basel, Switzerland, 2020. [Google Scholar]
- Hinds, W.C. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles; John Wiley & Sons: Hoboken, NJ, USA, 1999. [Google Scholar]
- Haghighat, F.; Bahloul, A.; Lara, J.; Mostofi, R.; Mahdavi, A. Development of a procedure to measure the effectiveness of N95 respirator filters against nanoparticles. Stud. Res. Pro. R-754 2012. [Google Scholar]
- Mostofi, R.; Wang, B.; Haghighat, F.; Bahloul, A.; Jaime, L. Performance of mechanical filters and respirators for capturing nanoparticles―Limitations and future direction. Ind Health. Natl. Inst. Occup. Saf. Health 2010, 48, 296–304. [Google Scholar]
- Mahdavi, A.; Haghighat, F.; Bahloul, A.; Brochot, C.; Ostiguy, C. Particle loading time and humidity effects on the efficiency of an N95 filtering facepiece respirator model under constant and inhalation cyclic flows. Ann. Occup. Hyg. 2015, 59, 629–640. [Google Scholar]
- Pacitto, A.; Amato, F.; Salmatonidis, A.; Moreno, T.; Alastuey, A.; Reche, C.; Buonanno, G.; Benito, C.; Querol, X. Effectiveness of commercial face masks to reduce personal PM exposure. Sci. Total Environ. 2019, 650, 1582–1590. [Google Scholar] [CrossRef]
- Ingle, M.A.; Talmale, G.R. Respiratory mask selection and leakage detection system based on canny edge detection operator. Procedia Comput. Sci. 2016, 78, 323–329. [Google Scholar] [CrossRef] [Green Version]
- Guha, S.; McCaffrey, B.; Hariharan, P.; Myers, M.R. Quantification of leakage of sub-micron aerosols through surgical masks and facemasks for pediatric use. J. Occup. Environ. Hyg. 2017, 14, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Rengasamy, S.; Eimer, B.C.; Szalajda, J. A quantitative assessment of the total inward leakage of NaCl aerosol representing submicron-size bioaerosol through N95 filtering facepiece respirators and surgical masks. J. Occup. Environ. Hyg. 2014, 11, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Yao, B.; Wang, Y.; Ye, X.; Zhang, F.; Peng, Y. Impact of structural features on dynamic breathing resistance of healthcare face mask. Sci. Total Environ. 2019, 689, 743–753. [Google Scholar] [CrossRef]





| Characteristic | Disposable Non-Woven | REUSABLE | |
|---|---|---|---|
| Traditional Textile | Micro-Porous Textile | ||
| Mechanical behavior | 1 | 2 | 3 |
| Resistance to bacterial penetration | 3 | 1 | 2 |
| Resistance to liquid penetration | 3 | 1 | 2 |
| Flexibility | 3 | 1 | 2 |
| Remark: 1–3 represent poor to best criteria of properties. | |||
| Types | Pros and Cons | Appearance |
|---|---|---|
| Basic Cloth face masks | Easily fabrication, cost-effective and simplest type of face mask. The starting materials could be clothes sweatshirts, T-shirts, etc. However, not much applicability for aerosols with diameters of 20–1000 nm compared to the other types. |  |
| Surgical face masks (SFMs) | This type serves the wearer for protection against fluid stream and bacteria capturing. It has three layers, with a role of filtering media, moisture absorbance, and water repelling. The effectiveness of this type is similar to the N95 respirator. However, they are not capable of reducing the emission of small-size droplets. |  |
| N95 respirator | Known as electrets filters in the group of filtering facepiece respirators (FFR), with surgical and standard sorts, they filter particles with diameters of 0.3 µm with 95% efficiency. It has a ventilator fan and four layers of materials of non-woven polypropylene for outer/inner layers and modacrylic, non-woven polypropylene metlblown for middle ones. However, N95 respirators are not applicable for sufficient protection against aerosols with diameters of less than 300 nm. |  |
| P100 respirator/gas mask | This is another type of filtering facepiece respirator (FFR), with a particle-filtering efficiency and penetration of 99.97% and 0.03%, respectively. In addition, this type is better than N95 respirators in terms of less leakage and keeping a standard form in changing temperature and humidity. |  |
| Self-contained breathing apparatus (SCBA) | This type of mask is equipped with an air supply that is normally applied for firefighting protection that resists forms of airborne contamination. However, it limits the mobility of the user and restricts workplace moments. |  |
| Full face respirator | This is made from rigid plastic materials with transparent parts for observation, which are fabricated for the aim of breathing trouble treatment. There are different types with respect to the size and shapes: air-purifying respirators (APR) and atmosphere-supplying respirators (ASR). Face supplies for holding the masks are made of adaptable elastomeric materials to well cover the face. Another element is straps that hold the mask body on the user head for the aim of leakage prevention. However, based on wearer behavior, these elements, especially the straps, can be broken. |  |
| Full-length face shield | This kind of mask contains elastic headbands to cover the head and a transparent rigid polymeric (polycarbonate) full-length face shield. This could protect the user from liquid infected splashes in sneezing. |  |
| Level of Protection | Characteristic of Each Level |
|---|---|
| Level 1 (Low barrier) |
|
| Level 2 (Moderate barrier) |
|
| Level 3 (High barrier) |
|
| Machine Parameters | Process | Material |
|---|---|---|
| Air velocity Air pressure Air temperature Die temperature Air flow rate Melt flow index | Polymer temperature Air temperature Die temperature Die hole size Die set-back Web collection type | Polymer forms (granules, chips) Polymer type Polymer degradation Polymer additives Melt viscosity - |
| Evaluation | Type I a | Type II a | Type IIR b |
|---|---|---|---|
| Bacterial filtration efficiency (BEF), % | ≥95 | ≥98 | ≥98 |
| Differential pressure (Pa·cm−2) | <40 | <40 | <60 |
| Splash resistance pressure (kPa) | NR * | NR | ≥16.0 |
| Microbial cleanliness (cfu. g−1) | ≤30 | ≤30 | ≤30 |
| Factors | Remarks |
|---|---|
| Thermal Rebound | Definition: Based on critical velocity and kinetic energy, which depends on particle diameter, yield pressure, particle density, etc. |
| Effects: Negatively affect filtration efficiency in nanoscale particles, which depends on high temperature behavior of nanoparticles that is difficult to define the exact critical diameter of the boundary condition. | |
| Face Velocity | Definition: Has an impact on diffusion, interception and electrostatic attraction of the fibrous filtration, which contributes to particle shape and velocity range. |
| Effects: Generally, in high velocities (e.g., 20 cm.s−1), it causes an outweighing interception mechanism to become a diffusion mechanism, which reduces the filtration efficiency. | |
| Airflow Rate | Definition: Used for filtration efficiency evaluation of respiratory and fibrous filtration. |
| Effects: This factor directly increases the penetration of the particles by increasing airflow rate. The suggestion for the test is 85 and 350 l.min−1 for similarity with real situation. | |
| Relative Humidity (RH) | Definition: In large scale particles, elevation in capillary force, which consequently improves the adherence of particles to the fibers in charged filters, takes a part with ions and electrons. |
| Effects: Depending on the filtration mechanism, it has negative and positive impacts on the filtration process, which, in mechanical and electrets filtration, shows an increase and decrease in the process, respectively. Generally, it was reported that the type of effect is completely related to the fabrication of the masks and filters. | |
| Particle Charge States | Definition: This considers charged/uncharged particles with mechanical and electrets filtration in the view of coulomb and image force interaction with mask medium and particles. |
| Effects: The best performance of filtration was observed in incidence of neutralized particles to the electrets filtration. |
| Components | Role |
|---|---|
| Vacuum pump | simulates inhalation process |
| Compression pump | simulates exhalation process |
| Mass flow controller | monitors airflow rate with respect to certain breathing frequency |
| Virtual instrument | controls microelectronics system, mass flow controller and obtains the dynamic altering of airflow rate from mass flow controller and breathing resistance signals from microelectronics system |
| Microelectronic system | manages solenoid valve for changing the direction of air flow for the aim of exhalation and inhalation simulation |
| Pressure sensors | records dynamic changes of breathing resistance with regard to time |
| Indices | Unit | Diagram | Remarks |
|---|---|---|---|
| Maximum exhalation resistance (MER) | Pa | 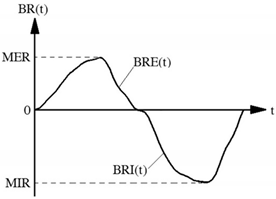 | MER is defined as: in which BRE(t) shows breathing resistance with respect to time for exhalation process. |
| Maximum inhalation resistance (MIR) | Pa | MIR is defined as: in which BRI(t) shows breathing resistance with respect to time for inhalation process. | |
| Average change rate of exhalation resistance (ACE) | Pa·S−1 | 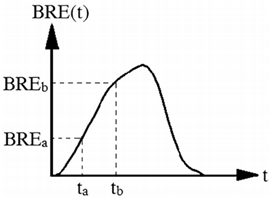 | The slope of the exhalation resistance curve that is center 60% with regard to breathing resistance: a and b refer to limits of the center 60% of the exhalation resistance curve according to BREa and BREb, respectively. |
| Average change rate of inhalation resistance (ACI) | Pa·S−1 | 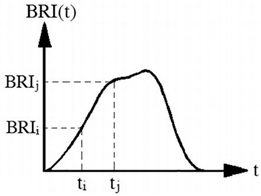 | It is defined as center 60% of the slope of the inhalation resistance curve: i and j refer to limits of the center 60% of the inhalation resistance curve according to BRIi and BRIj, respectively. |
| Maximum change rate of exhalation resistance (MCE) | Pa·S−1 | 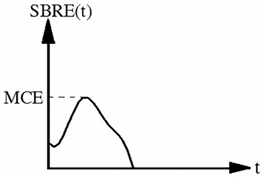 | It is defined as the maximum slope of the exhalation resistance curve: SBRE(t) is the slope of exhalation resistance with regard to time. |
| Maximum change rate of inhalation resistance (MCI) | Pa·S−1 | 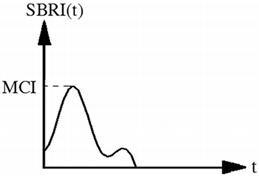 | It is defined as the maximum slope of the inhalation resistance curve: SBRI(t) is the slope of inhalation resistance with regard to time. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farzaneh, S.; Shirinbayan, M. Processing and Quality Control of Masks: A Review. Polymers 2022, 14, 291. https://doi.org/10.3390/polym14020291
Farzaneh S, Shirinbayan M. Processing and Quality Control of Masks: A Review. Polymers. 2022; 14(2):291. https://doi.org/10.3390/polym14020291
Chicago/Turabian StyleFarzaneh, Sedigheh, and Mohammadali Shirinbayan. 2022. "Processing and Quality Control of Masks: A Review" Polymers 14, no. 2: 291. https://doi.org/10.3390/polym14020291
APA StyleFarzaneh, S., & Shirinbayan, M. (2022). Processing and Quality Control of Masks: A Review. Polymers, 14(2), 291. https://doi.org/10.3390/polym14020291







