Dendrimers as Nanocarriers for the Delivery of Drugs Obtained from Natural Products
Abstract
1. Introduction
2. Alkaloids Compound
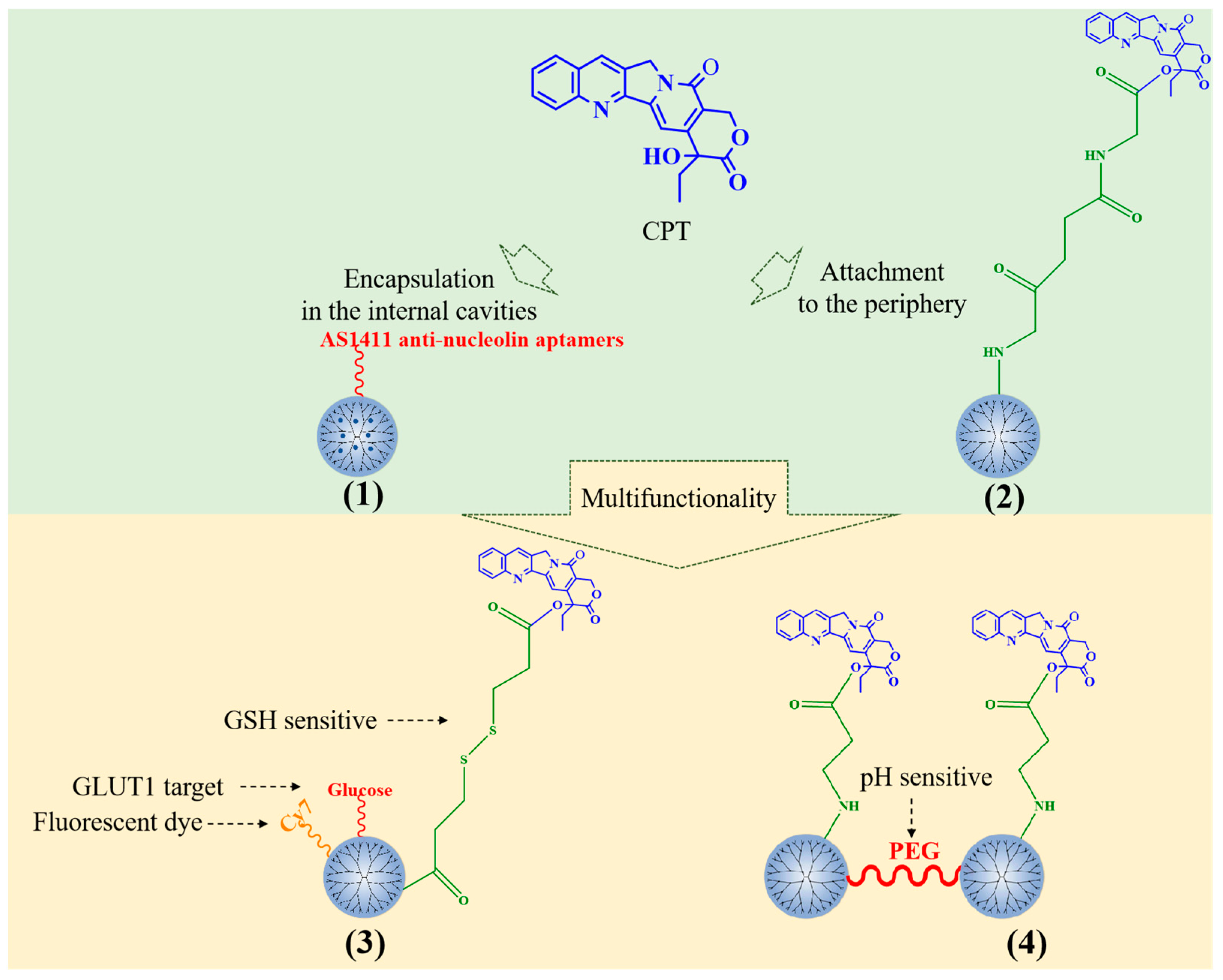
2.1. Camptothecin
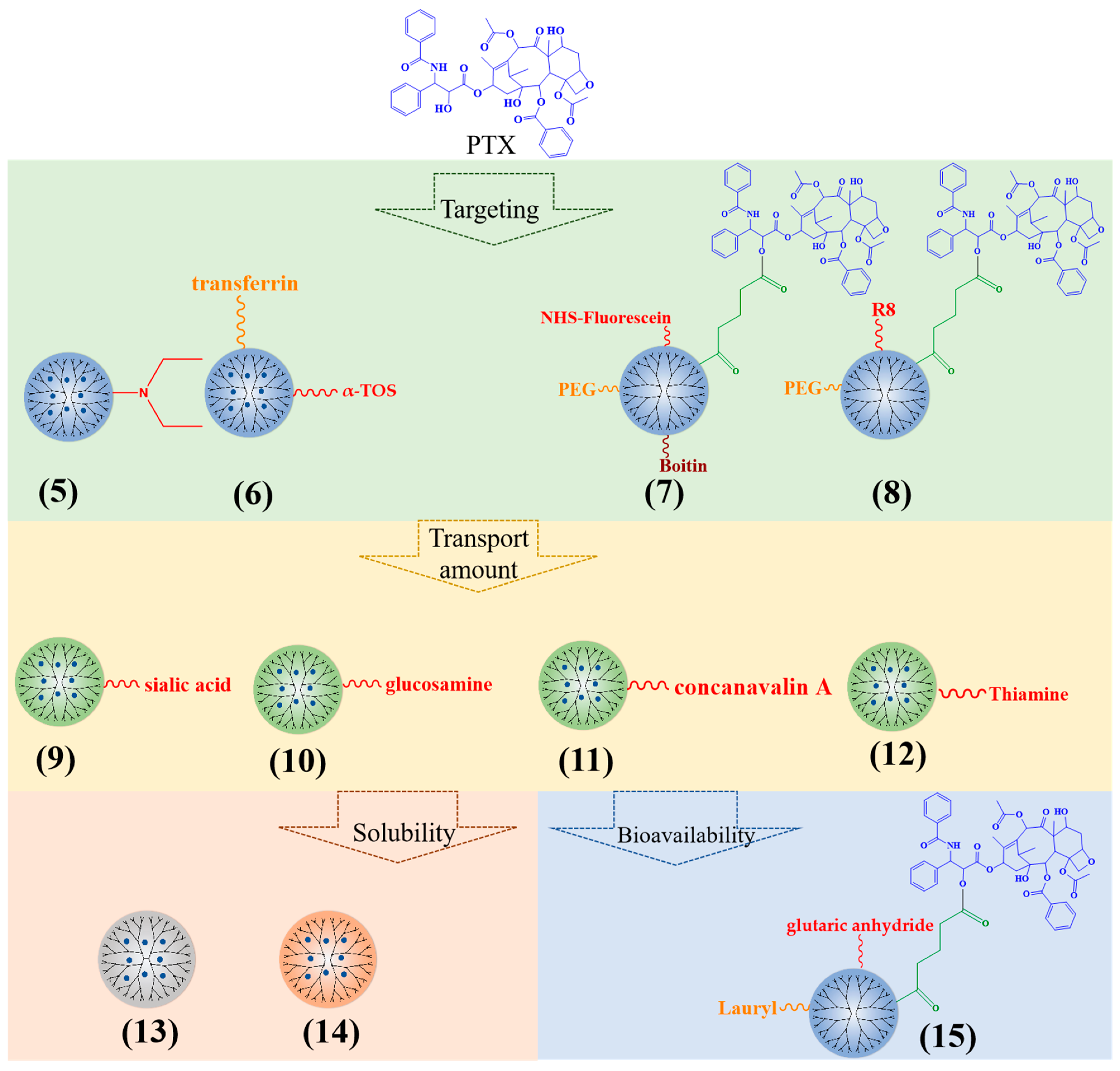
2.2. Paclitaxel
2.3. Berberine
3. Polyphenolic Compounds
3.1. Quercetin
3.2. Gallic Acid
3.3. Resveratrol
3.4. Silybin
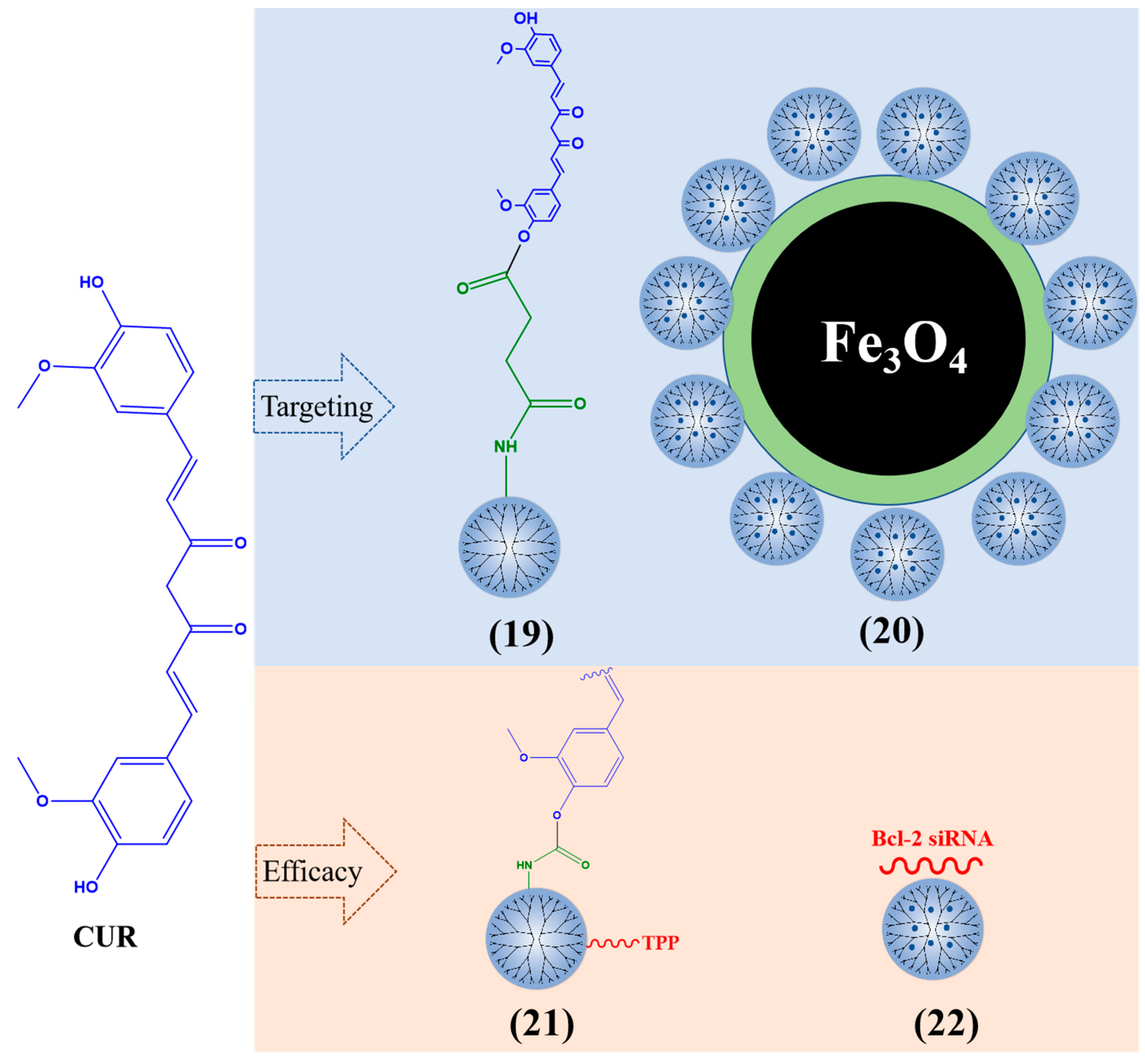
3.5. Curcumin
3.6. Puerarin
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Razavi, M.S.; Ebrahimnejad, P.; Fatahi, Y.; D’Emanuele, A.; Dinarvand, R. Recent Developments of Nanostructures for the Ocular Delivery of Natural Compounds. Front. Chem. 2022, 10, 850757. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.; Veiga, F.; Figueiras, A. Dendrimers as Pharmaceutical Excipients: Synthesis, Properties, Toxicity and Biomedical Applications. Materials 2019, 13, 65. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Alvarez, F.; Martinez-Garcia, M. Click Reaction in the Synthesis of Dendrimer Drug-delivery Systems. Curr. Med. Chem. 2022, 29, 3445–3470. [Google Scholar] [CrossRef]
- Mignani, S.; Shi, X.; Guidolin, K.; Zheng, G.; Karpus, A.; Majoral, J.P. Clinical diagonal translation of nanoparticles: Case studies in dendrimer nanomedicine. J. Control. Release 2021, 337, 356–370. [Google Scholar] [CrossRef]
- Li, H.; Zha, S.; Li, H.; Liu, H.; Wong, K.L.; All, A.H. Polymeric Dendrimers as Nanocarrier Vectors for Neurotheranostics. Small 2022, 18, e2203629. [Google Scholar] [CrossRef] [PubMed]
- Kesharwani, P.; Jain, K.; Jain, N.K. Dendrimer as nanocarrier for drug delivery. Prog. Polym. Sci. 2014, 39, 268–307. [Google Scholar] [CrossRef]
- Wang, J.; Li, B.; Qiu, L.; Qiao, X.; Yang, H. Dendrimer-based drug delivery systems: History, challenges, and latest developments. J. Biol. Eng. 2022, 16, 18. [Google Scholar] [CrossRef]
- Mignani, S.; Shi, X.; Rodrigues, J.; Tomás, H.; Majoral, J.P. Dendrimer nanoplatforms for veterinary medicine applications: A concise overview. Drug Discov. Today 2022, 27, 1251–1260. [Google Scholar] [CrossRef]
- Sathe, R.Y.; Bharatam, P.V. Drug-dendrimer complexes and conjugates: Detailed furtherance through theory and experiments. Adv. Colloid Interface Sci. 2022, 303, 102639. [Google Scholar] [CrossRef]
- Chis, A.A.; Dobrea, C.; Morgovan, C.; Arseniu, A.M.; Rus, L.L.; Butuca, A.; Juncan, A.M.; Totan, M.; Vonica-Tincu, A.L.; Cormos, G.; et al. Applications and Limitations of Dendrimers in Biomedicine. Molecules 2020, 25, 3982. [Google Scholar] [CrossRef]
- Choudhary, S.; Gupta, L.; Rani, S.; Dave, K.; Gupta, U. Impact of Dendrimers on Solubility of Hydrophobic Drug Molecules. Front. Pharmacol. 2017, 8, 261. [Google Scholar] [CrossRef] [PubMed]
- Caminade, A.M.; Turrin, C.O. Dendrimers for drug delivery. J. Mater. Chem. B 2014, 2, 4055–4066. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Wu, F.; Lin, X.; Shen, L.; Feng, Y. Developments in drug delivery of bioactive alkaloids derived from traditional Chinese medicine. Drug Deliv. 2018, 25, 398–416. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Zhang, B.; Li, M.; Zhang, J. The current scenario of naturally occurring indole alkaloids with anticancer potential. Fitoterapia 2023, 165, 105430. [Google Scholar] [CrossRef] [PubMed]
- Sindhoor, M.S.; Naveen, N.R.; Rao, G.K.; Gopan, G.; Chopra, H.; Park, M.N.; Alshahrani, M.M.; Jose, J.; Emran, T.B.; Kim, B. A spotlight on alkaloid nanoformulations for the treatment of lung cancer. Front. Oncol. 2022, 12, 994155. [Google Scholar]
- Wang, Y.; Xu, Y.; Liu, Z. A review of plant antipathogenic constituents: Source, activity and mechanism. Pestic. Biochem. Physiol. 2022, 188, 105225. [Google Scholar] [CrossRef]
- Faisal, S.; Badshah, S.L.; Kubra, B.; Emwas, A.H.; Jaremko, M. Alkaloids as potential antivirals. A comprehensive review. Nat. Prod. Bioprospect. 2023, 13, 4. [Google Scholar] [CrossRef]
- Ghanbari-Movahed, M.; Kaceli, T.; Mondal, A.; Farzaei, M.H.; Bishayee, A. Recent Advances in Improved Anticancer Efficacies of Camptothecin Nano-Formulations: A Systematic Review. Biomedicines 2021, 9, 480. [Google Scholar] [CrossRef]
- Schluep, T.; Cheng, J.; Khin, K.T.; Davis, M.E. Pharmacokinetics and biodistribution of the camptothecin-polymer conjugate IT-101 in rats and tumor-bearing mice. Cancer Chemother. Pharmacol. 2006, 57, 654–662. [Google Scholar] [CrossRef]
- Khaiwa, N.; Maarouf, N.R.; Darwish, M.H.; Alhamad, D.W.M.; Sebastian, A.; Hamad, M.; Omar, H.A.; Orive, G.; Al-Tel, T.H. Camptothecin’s journey from discovery to WHO Essential Medicine: Fifty years of promise. Eur. J. Med. Chem. 2021, 223, 113639. [Google Scholar] [CrossRef]
- Alibolandi, M.; Taghdisi, S.M.; Ramezani, P.; Hosseini Shamili, F.; Farzad, S.A.; Abnous, K.; Ramezani, M. Smart AS1411-aptamer conjugated pegylated PAMAM dendrimer for the superior delivery of camptothecin to colon adenocarcinoma in vitro and in vivo. Int. J. Pharm. 2017, 519, 352–364. [Google Scholar] [CrossRef] [PubMed]
- Pooja, D.; Srinivasa Reddy, T.; Kulhari, H.; Kadari, A.; Adams, D.J.; Bansal, V.; Sistla, R. N-acetyl-d-glucosamine-conjugated PAMAM dendrimers as dual receptor-targeting nanocarriers for anticancer drug delivery. Eur. J. Pharm. Biopharm. 2020, 154, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, G.; Ray, A.; Malugin, A.; Ghandehari, H. PAMAM-camptothecin conjugate inhibits proliferation and induces nuclear fragmentation in colorectal carcinoma cells. Pharm. Res. 2010, 27, 2307–2316. [Google Scholar] [CrossRef] [PubMed]
- Ma, P.; Sun, Y.; Chen, J.; Li, H.; Zhu, H.; Gao, X.; Bi, X.; Zhang, Y. Enhanced anti-hepatocarcinoma efficacy by GLUT1 targeting and cellular microenvironment-responsive PAMAM–camptothecin conjugate. Drug Deliv. 2017, 25, 153–165. [Google Scholar] [CrossRef]
- Wang, J.; He, H.; Cooper, R.C.; Gui, Q.; Yang, H. Drug-Conjugated Dendrimer Hydrogel Enables Sustained Drug Release via a Self-Cleaving Mechanism. Mol. Pharm. 2019, 16, 1874–1880. [Google Scholar] [CrossRef]
- Fox, M.E.; Guillaudeu, S.; Frechet, J.M.; Jerger, K.; Macaraeg, N.; Szoka, F.C. Synthesis and in vivo antitumor efficacy of PEGylated poly(l-lysine) dendrimer-camptothecin conjugates. Mol. Pharm. 2009, 6, 1562–1572. [Google Scholar] [CrossRef]
- Min, L.; Han, J.-C.; Zhang, W.; Gu, C.-C.; Zou, Y.-P.; Li, C.-C. Strategies and Lessons Learned from Total Synthesis of Taxol. Chem. Rev. 2023, 123, 4934–4971. [Google Scholar] [CrossRef] [PubMed]
- Stage, T.B.; Bergmann, T.K.; Kroetz, D.L. Clinical Pharmacokinetics of Paclitaxel Monotherapy: An Updated Literature Review. Clin. Pharmacokinet. 2018, 57, 7–19. [Google Scholar] [CrossRef]
- Niznansky, L.; Osinova, D.; Kuruc, R.; Hengerics Szabo, A.; Szoradova, A.; Masar, M.; Niznanska, Z. Natural Taxanes: From Plant Composition to Human Pharmacology and Toxicity. Int. J. Mol. Sci. 2022, 23, 15619. [Google Scholar] [CrossRef]
- Li, T.; Akinade, T.; Zhou, J.; Wang, H.; Tong, Q.; He, S.; Rinebold, E.; Valencia Salazar, L.E.; Bhansali, D.; Zhong, Y.; et al. Therapeutic Nanocarriers Inhibit Chemotherapy-Induced Breast Cancer Metastasis. Adv. Sci. 2022, 9, e2203949. [Google Scholar] [CrossRef]
- Bhatt, H.; Kiran Rompicharla, S.V.; Ghosh, B.; Torchilin, V.; Biswas, S. Transferrin/α-tocopherol modified poly(amidoamine) dendrimers for improved tumor targeting and anticancer activity of paclitaxel. Nanomedicine 2019, 14, 3159–3176. [Google Scholar] [CrossRef] [PubMed]
- Rompicharla, S.V.K.; Kumari, P.; Bhatt, H.; Ghosh, B.; Biswas, S. Biotin functionalized PEGylated poly(amidoamine) dendrimer conjugate for active targeting of paclitaxel in cancer. Int. J. Pharm. 2019, 557, 329–341. [Google Scholar] [CrossRef] [PubMed]
- Dichwalkar, T.; Patel, S.; Bapat, S.; Pancholi, P.; Jasani, N.; Desai, B.; Yellepeddi, V.K.; Sehdev, V. Omega-3 Fatty Acid Grafted PAMAM-Paclitaxel Conjugate Exhibits Enhanced Anticancer Activity in Upper Gastrointestinal Cancer Cells. Macromol. Biosci. 2017, 17, 201600457. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.; Mao, Y.; Ye, T.; Xia, S.; Wang, S.; Wang, S. Study on enhanced lymphatic exposure of polyamidoamin-alkali blue dendrimer for paclitaxel delivery and influence of the osmotic pressure on the lymphatic targeting. Drug Deliv. 2016, 23, 2617–2629. [Google Scholar] [CrossRef]
- Rompicharla, S.V.K.; Kumari, P.; Ghosh, B.; Biswas, S. Octa-arginine modified poly(amidoamine) dendrimers for improved delivery and cytotoxic effect of paclitaxel in cancer. Artif. Cells Nanomed. Biotechnol. 2018, 46, 847–859. [Google Scholar] [CrossRef]
- Bhatt, H.; Ghosh, B.; Biswas, S. Cell-Penetrating Peptide and alpha-Tocopherol-Conjugated Poly(amidoamine) Dendrimers for Improved Delivery and Anticancer Activity of Loaded Paclitaxel. ACS Appl. Bio Mater. 2020, 3, 3157–3169. [Google Scholar] [CrossRef]
- Patel, H.K.; Gajbhiye, V.; Kesharwani, P.; Jain, N.K. Ligand anchored poly(propyleneimine) dendrimers for brain targeting: Comparative in vitro and in vivo assessment. J. Colloid Interface Sci. 2016, 482, 142–150. [Google Scholar] [CrossRef]
- Patel, S.K.; Gajbhiye, V.; Jain, N.K. Synthesis, characterization and brain targeting potential of paclitaxel loaded thiamine-PPI nanoconjugates. J. Drug Target 2012, 20, 841–849. [Google Scholar] [CrossRef]
- Bansal, K.K.; Kakde, D.; Gupta, U.; Jain, N.K. Development and characterization of triazine based dendrimers for delivery of antitumor agent. J. Nanosci. Nanotechnol. 2010, 10, 8395–8404. [Google Scholar] [CrossRef]
- Ooya, T.; Lee, J.; Park, K. Hydrotropic dendrimers of generations 4 and 5: Synthesis, characterization, and hydrotropic solubilization of paclitaxel. Bioconjug. Chem. 2004, 15, 1221–1229. [Google Scholar] [CrossRef]
- Teow, H.M.; Zhou, Z.; Najlah, M.; Yusof, S.R.; Abbott, N.J.; D’Emanuele, A. Delivery of paclitaxel across cellular barriers using a dendrimer-based nanocarrier. Int. J. Pharm. 2013, 441, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Khandare, J.J.; Jayant, S.; Singh, A.; Chandna, P.; Wang, Y.; Vorsa, N.; Minko, T. Dendrimer versus linear conjugate: Influence of polymeric architecture on the delivery and anticancer effect of paclitaxel. Bioconjug. Chem. 2006, 17, 1464–1472. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Cai, H.; Jiang, L.; Hu, J.; Bains, A.; Hu, J.; Gong, Q.; Luo, K.; Gu, Z. Enzyme-Sensitive and Amphiphilic PEGylated Dendrimer-Paclitaxel Prodrug-Based Nanoparticles for Enhanced Stability and Anticancer Efficacy. ACS Appl. Mater. Interfaces 2017, 9, 6865–6877. [Google Scholar] [CrossRef] [PubMed]
- Satsangi, A.; Roy, S.S.; Satsangi, R.K.; Vadlamudi, R.K.; Ong, J.L. Design of a paclitaxel prodrug conjugate for active targeting of an enzyme upregulated in breast cancer cells. Mol. Pharm. 2014, 11, 1906–1918. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Sun, T.; Ferrari, M. Nanovector delivery of siRNA for cancer therapy. Cancer Gene Ther. 2012, 19, 367–373. [Google Scholar] [CrossRef]
- Li, Y.; Wang, H.; Wang, K.; Hu, Q.; Yao, Q.; Shen, Y.; Yu, G.; Tang, G. Targeted Co-delivery of PTX and TR3 siRNA by PTP Peptide Modified Dendrimer for the Treatment of Pancreatic Cancer. Small 2017, 13, 201602697. [Google Scholar] [CrossRef]
- Kala, S.; Mak, A.S.; Liu, X.; Posocco, P.; Pricl, S.; Peng, L.; Wong, A.S. Combination of dendrimer-nanovector-mediated small interfering RNA delivery to target Akt with the clinical anticancer drug paclitaxel for effective and potent anticancer activity in treating ovarian cancer. J. Med. Chem. 2014, 57, 2634–2642. [Google Scholar] [CrossRef]
- Xia, Q.; Wang, W.; Liu, Z.; Xiao, J.; Qiao, C.; Zhao, Y.; Li, B.; Liu, Y.; Peng, Y.; Yang, X.; et al. New insights into mechanisms of berberine in alleviating reproductive disorders of polycystic ovary syndrome: Anti-inflammatory properties. Eur. J. Pharmacol. 2023, 939, 175433. [Google Scholar] [CrossRef]
- Li, D.D.; Yu, P.; Xiao, W.; Wang, Z.Z.; Zhao, L.G. Berberine: A Promising Natural Isoquinoline Alkaloid for the Development of Hypolipidemic Drugs. Curr. Top. Med. Chem. 2020, 20, 2634–2647. [Google Scholar] [CrossRef]
- Xiong, R.-G.; Huang, S.-Y.; Wu, S.-X.; Zhou, D.-D.; Yang, Z.-J.; Saimaiti, A.; Zhao, C.-N.; Shang, A.; Zhang, Y.-J.; Gan, R.-Y.; et al. Anticancer Effects and Mechanisms of Berberine from Medicinal Herbs: An Update Review. Molecules. 2022, 27, 4523. [Google Scholar] [CrossRef]
- Goel, A. Current understanding and future prospects on Berberine for anticancer therapy. Chem. Biol. Drug Des. 2023. (Online ahead of print. early view). [Google Scholar] [CrossRef]
- Chen, W.; Miao, Y.Q.; Fan, D.J.; Yang, S.S.; Lin, X.; Meng, L.K.; Tang, X. Bioavailability study of berberine and the enhancing effects of TPGS on intestinal absorption in rats. AAPS PharmSciTech 2011, 12, 705–711. [Google Scholar] [CrossRef]
- Gupta, L.; Sharma, A.K.; Gothwal, A.; Khan, M.S.; Khinchi, M.P.; Qayum, A.; Singh, S.K.; Gupta, U. Dendrimer encapsulated and conjugated delivery of berberine: A novel approach mitigating toxicity and improving in vivo pharmacokinetics. Int. J. Pharm. 2017, 528, 88–99. [Google Scholar] [CrossRef]
- Yadav, D.; Semwal, B.C.; Dewangan, H.K. Grafting, characterization and enhancement of therapeutic activity of berberine loaded PEGylated PAMAM dendrimer for cancerous cell. J. Biomater. Sci. Polym. Ed. 2022. (Online ahead of print). [Google Scholar] [CrossRef]
- Kyriakoudi, A.; Spanidi, E.; Mourtzinos, I.; Gardikis, K. Innovative Delivery Systems Loaded with Plant Bioactive Ingredients: Formulation Approaches and Applications. Plants 2021, 10, 1238. [Google Scholar] [CrossRef]
- Albuquerque, B.R.; Heleno, S.A.; Oliveira, M.; Barros, L.; Ferreira, I. Phenolic compounds: Current industrial applications, limitations and future challenges. Food Funct. 2021, 12, 14–29. [Google Scholar] [CrossRef]
- Liu, H.M.; Cheng, M.Y.; Xun, M.H.; Zhao, Z.W.; Zhang, Y.; Tang, W.; Cheng, J.; Ni, J.; Wang, W. Possible Mechanisms of Oxidative Stress-Induced Skin Cellular Senescence, Inflammation, and Cancer and the Therapeutic Potential of Plant Polyphenols. Int. J. Mol. Sci. 2023, 24, 3755. [Google Scholar] [CrossRef]
- Dominguez-Avila, J.A.; Wall-Medrano, A.; Velderrain-Rodriguez, G.R.; Chen, C.O.; Salazar-Lopez, N.J.; Robles-Sanchez, M.; Gonzalez-Aguilar, G.A. Gastrointestinal interactions, absorption, splanchnic metabolism and pharmacokinetics of orally ingested phenolic compounds. Food Funct. 2017, 8, 15–38. [Google Scholar] [CrossRef]
- Fantini, M.; Benvenuto, M.; Masuelli, L.; Frajese, G.V.; Tresoldi, I.; Modesti, A.; Bei, R. In vitro and in vivo antitumoral effects of combinations of polyphenols, or polyphenols and anticancer drugs: Perspectives on cancer treatment. Int. J. Mol. Sci. 2015, 16, 9236–9282. [Google Scholar] [CrossRef]
- Dini, I.; Grumetto, L. Recent Advances in Natural Polyphenol Research. Molecules 2022, 27, 8777. [Google Scholar] [CrossRef]
- Brglez Mojzer, E.; Knez Hrncic, M.; Skerget, M.; Knez, Z.; Bren, U. Polyphenols: Extraction Methods, Antioxidative Action, Bioavailability and Anticarcinogenic Effects. Molecules 2016, 21, 901. [Google Scholar] [CrossRef]
- Rakotondrabe, T.F.; Fan, M.X.; Muema, F.W.; Guo, M.Q. Modulating Inflammation-Mediated Diseases via Natural Phenolic Compounds Loaded in Nanocarrier Systems. Pharmaceutics 2023, 15, 699. [Google Scholar] [CrossRef]
- Crozier, A.; Jaganath, I.B.; Clifford, M.N. Dietary phenolics: Chemistry, bioavailability and effects on health. Nat. Prod. Rep. 2009, 26, 1001–1043. [Google Scholar] [CrossRef]
- Williamson, G.; Manach, C. Bioavailability and bioefficacy of polyphenols in humans. II. Review of 93 intervention studies. Am. J. Clin. Nutr. 2005, 81, 243s–255s. [Google Scholar] [CrossRef]
- Li, Y.; Yao, J.; Han, C.; Yang, J.; Chaudhry, M.T.; Wang, S.; Liu, H.; Yin, Y. Quercetin, Inflammation and Immunity. Nutrients 2016, 8, 167. [Google Scholar] [CrossRef]
- Chen, S.; Jiang, H.; Wu, X.; Fang, J. Therapeutic Effects of Quercetin on Inflammation, Obesity, and Type 2 Diabetes. Mediat. Inflamm. 2016, 2016, 9340637. [Google Scholar] [CrossRef]
- Wang, G.; Wang, Y.; Yao, L.; Gu, W.; Zhao, S.; Shen, Z.; Lin, Z.; Liu, W.; Yan, T.; Cohen, G. Pharmacological Activity of Quercetin: An Updated Review. Evid.-Based Complement. Altern. Med. 2022, 2022, 3997190. [Google Scholar] [CrossRef]
- Azizi, E.; Fouladdel, S.; Komeili Movahhed, T.; Modaresi, F.; Barzegar, E.; Ghahremani, M.H.; Ostad, S.N.; Atashpour, S. Quercetin Effects on Cell Cycle Arrest and Apoptosis and Doxorubicin Activity in T47D Cancer Stem Cells. Asian Pac. J. Cancer Prev. 2022, 23, 4145–4154. [Google Scholar] [CrossRef]
- Sethi, G.; Rath, P.; Chauhan, A.; Ranjan, A.; Choudhary, R.; Ramniwas, S.; Sak, K.; Aggarwal, D.; Rani, I.; Tuli, H.S. Apoptotic Mechanisms of Quercetin in Liver Cancer: Recent Trends and Advancements. Pharmaceutics 2023, 15, 712. [Google Scholar] [CrossRef]
- Bhatiya, M.; Pathak, S.; Jothimani, G.; Duttaroy, A.K.; Banerjee, A. A Comprehensive Study on the Anti-cancer Effects of Quercetin and Its Epigenetic Modifications in Arresting Progression of Colon Cancer Cell Proliferation. Arch. Immunol. Ther. Exp. 2023, 71, 6. [Google Scholar] [CrossRef]
- Maugeri, A.; Calderaro, A.; Patanè, G.T.; Navarra, M.; Barreca, D.; Cirmi, S.; Felice, M.R. Targets Involved in the Anti-Cancer Activity of Quercetin in Breast, Colorectal and Liver Neoplasms. Int. J. Mol. Sci. 2023, 24, 2952. [Google Scholar] [CrossRef]
- Moghimipour, E.; Farsimadan, N.; Salimi, A. Ocular Delivery of Quercetin Using Microemulsion System: Design, Characterization, and Ex-vivo Transcorneal Permeation. Iran. J. Pharm. Res. 2022, 21, e127486. [Google Scholar] [CrossRef]
- Madaan, K.; Lather, V.; Pandita, D. Evaluation of polyamidoamine dendrimers as potential carriers for quercetin, a versatile flavonoid. Drug Deliv. 2016, 23, 254–262. [Google Scholar] [CrossRef]
- Mitri, Z.; Constantine, T.; O’Regan, R. The HER2 Receptor in Breast Cancer: Pathophysiology, Clinical Use, and New Advances in Therapy. Chemother. Res. Pract. 2012, 2012, 743193. [Google Scholar] [CrossRef]
- Khakinahad, Y.; Sohrabi, S.; Razi, S.; Narmani, A.; Khaleghi, S.; Asadiyun, M.; Jafari, H.; Mohammadnejad, J. Margetuximab conjugated-PEG-PAMAM G4 nano-complex: A smart nano-device for suppression of breast cancer. Biomed. Eng. Lett. 2022, 12, 317–329. [Google Scholar] [CrossRef]
- Rezaei, S.J.T.; Malekzadeh, A.M.; Ramazani, A.; Niknejad, H. pH-Sensitive Magnetite Nanoparticles Modified with Hyperbranched Polymers and Folic Acid for Targeted Imaging and Therapy. Curr. Drug Deliv. 2019, 16, 839–848. [Google Scholar] [CrossRef]
- Jiang, Y.; Pei, J.; Zheng, Y.; Miao, Y.J.; Duan, B.Z.; Huang, L.F. Gallic Acid: A Potential Anti-Cancer Agent. Chin. J. Integr. Med. 2022, 28, 661–671. [Google Scholar] [CrossRef]
- Tuli, H.S.; Mistry, H.; Kaur, G.; Aggarwal, D.; Garg, V.K.; Mittal, S.; Yerer, M.B.; Sak, K.; Khan, M.A. Gallic Acid: A Dietary Polyphenol that Exhibits Anti-neoplastic Activities by Modulating Multiple Oncogenic Targets. Anticancer Agents Med. Chem. 2022, 22, 499–514. [Google Scholar] [CrossRef]
- Priyadarshi, K.; Shirsath, K.; Waghela, N.B.; Sharma, A.; Kumar, A.; Pathak, C. Surface modified PAMAM dendrimers with gallic acid inhibit, cell proliferation, cell migration and inflammatory response to augment apoptotic cell death in human colon carcinoma cells. J. Biomol. Struct. Dyn. 2021, 39, 6853–6869. [Google Scholar] [CrossRef]
- Sharma, A.; Gautam, S.P.; Gupta, A.K. Surface modified dendrimers: Synthesis and characterization for cancer targeted drug delivery. Bioorg. Med. Chem. 2011, 19, 3341–3346. [Google Scholar] [CrossRef]
- Abdou, E.M.; Masoud, M.M. Gallic acid-PAMAM and gallic acid-phospholipid conjugates, physicochemical characterization and in vivo evaluation. Pharm. Dev. Technol. 2018, 23, 55–66. [Google Scholar] [CrossRef]
- Lalani, A.R.; Fakhari, F.; Radgoudarzi, S.; Rastegar-Pouyani, N.; Moloudi, K.; Khodamoradi, E.; Taeb, S.; Najafi, M. Immunoregulation by resveratrol; implications for normal tissue protection and tumour suppression. Clin. Exp. Pharmacol. Physiol. 2023, 50, 353–368. [Google Scholar] [CrossRef]
- Fernandez-Quintela, A.; Macarulla, M.T.; Gomez-Zorita, S.; Gonzalez, M.; Milton-Laskibar, I.; Portillo, M.P. Relationship between changes in microbiota induced by resveratrol and its anti-diabetic effect on type 2 diabetes. Front. Nutr. 2022, 9, 1084702. [Google Scholar] [CrossRef]
- Fan, D.; Liu, C.; Zhang, Z.; Huang, K.; Wang, T.; Chen, S.; Li, Z. Progress in the Preclinical and Clinical Study of Resveratrol for Vascular Metabolic Disease. Molecules 2022, 27, 7524. [Google Scholar] [CrossRef]
- Singh, G. Resveratrol: Nanocarrier-based delivery systems to enhance its therapeutic potential. Nanomedicine 2020, 15, 2801–2817. [Google Scholar] [CrossRef]
- Walle, T.; Hsieh, F.; DeLegge, M.H.; Oatis, J.E., Jr.; Walle, U.K. High absorption but very low bioavailability of oral resveratrol in humans. Drug Metab. Dispos. 2004, 32, 1377–1382. [Google Scholar] [CrossRef]
- Gambini, J.; López-Grueso, R.; Olaso-González, G.; Inglés, M.; Abdelazid, K.; El Alami, M.; Bonet-Costa, V.; Borrás, C.; Viña, J. [Resveratrol: Distribution, properties and perspectives]. Rev. Esp. Geriatr. Gerontol. 2013, 48, 79–88. [Google Scholar] [CrossRef]
- Pentek, T.; Newenhouse, E.; O’Brien, B.; Chauhan, A.S. Development of a Topical Resveratrol Formulation for Commercial Applications Using Dendrimer Nanotechnology. Molecules 2017, 22, 137. [Google Scholar] [CrossRef]
- Shi, Y.; Ye, F.; Lu, K.; Hui, Q.; Miao, M. Characterizations and Bioavailability of Dendrimer-like Glucan Nanoparticulate System Containing Resveratrol. J. Agric. Food. Chem. 2020, 68, 6420–6429. [Google Scholar] [CrossRef]
- Xie, Y.; Yao, Y. Octenylsuccinate hydroxypropyl phytoglycogen, a dendrimer-like biopolymer, solubilizes poorly water-soluble active pharmaceutical ingredients. Carbohydr. Polym. 2018, 180, 29–37. [Google Scholar] [CrossRef]
- Islam, A.; Mishra, A.; Siddiqui, M.A.; Siddiquie, S. Recapitulation of Evidence of Phytochemical, Pharmacokinetic and Biomedical Application of Silybin. Drug Res. 2021, 71, 489–503. [Google Scholar] [CrossRef]
- Křen, V.; Marhol, P.; Purchartová, K.; Gabrielová, E.; Modrianský, M. Biotransformation of silybin and its congeners. Curr. Drug Metab. 2013, 14, 1009–1021. [Google Scholar] [CrossRef]
- Wu, J.W.; Lin, L.C.; Hung, S.C.; Chi, C.W.; Tsai, T.H. Analysis of silibinin in rat plasma and bile for hepatobiliary excretion and oral bioavailability application. J. Pharm. Biomed. Anal. 2007, 45, 635–641. [Google Scholar] [CrossRef]
- Huang, X.; Wu, Z.; Gao, W.; Chen, Q.; Yu, B. Polyamidoamine dendrimers as potential drug carriers for enhanced aqueous solubility and oral bioavailability of silybin. Drug Dev. Ind. Pharm. 2011, 37, 419–427. [Google Scholar] [CrossRef]
- Diaz, C.; Guzman, J.; Jimenez, V.A.; Alderete, J.B. Partially PEGylated PAMAM dendrimers as solubility enhancers of Silybin. Pharm. Dev. Technol. 2018, 23, 689–696. [Google Scholar] [CrossRef]
- Shetty, P.K.; Manikkath, J.; Tupally, K.; Kokil, G.; Hegde, A.R.; Raut, S.Y.; Parekh, H.S.; Mutalik, S. Skin Delivery of EGCG and Silibinin: Potential of Peptide Dendrimers for Enhanced Skin Permeation and Deposition. AAPS PharmSciTech 2017, 18, 2346–2357. [Google Scholar] [CrossRef]
- Dehzad, M.J.; Ghalandari, H.; Nouri, M.; Askarpour, M. Antioxidant and anti-inflammatory effects of curcumin/turmeric supplementation in adults: A GRADE-assessed systematic review and dose-response meta-analysis of randomized controlled trials. Cytokine. 2023, 164, 156144. [Google Scholar] [CrossRef]
- Shakeri, A.; Ward, N.; Panahi, Y.; Sahebkar, A. Anti-Angiogenic Activity of Curcumin in Cancer Therapy: A Narrative Review. Curr. Vasc. Pharmacol. 2019, 17, 262–269. [Google Scholar] [CrossRef]
- Hussain, Y.; Alam, W.; Ullah, H.; Dacrema, M.; Daglia, M.; Khan, H.; Arciola, C.R. Antimicrobial Potential of Curcumin: Therapeutic Potential and Challenges to Clinical Applications. Antibiotics 2022, 11, 322. [Google Scholar] [CrossRef]
- PDQ Integrative, Alternative; Complementary Therapies Editorial Board. Curcumin (Curcuma, Turmeric) and Cancer (PDQ®): Health Professional Version. In PDQ Cancer Information Summaries; National Cancer Institute (US): Bethesda, MD, USA, 2002. [Google Scholar]
- Zeng, Y.; Luo, Y.; Wang, L.; Zhang, K.; Peng, J.; Fan, G. Therapeutic Effect of Curcumin on Metabolic Diseases: Evidence from Clinical Studies. Int. J. Mol. Sci. 2023, 24, 3323. [Google Scholar] [CrossRef]
- Wu, J.; Lv, M.; Zhou, Y. Efficacy and side effect of curcumin for the treatment of osteoarthritis: A meta-analysis of randomized controlled trials. Pak. J. Pharm. Sci. 2019, 32, 43–51. [Google Scholar]
- Salehi, B.; Del Prado-Audelo, M.L.; Cortes, H.; Leyva-Gomez, G.; Stojanovic-Radic, Z.; Singh, Y.D.; Patra, J.K.; Das, G.; Martins, N.; Martorell, M.; et al. Therapeutic Applications of Curcumin Nanomedicine Formulations in Cardiovascular Diseases. J. Clin. Med. 2020, 9, 746. [Google Scholar] [CrossRef]
- Cheng, A.L.; Hsu, C.H.; Lin, J.K.; Hsu, M.M.; Ho, Y.F.; Shen, T.S.; Ko, J.Y.; Lin, J.T.; Lin, B.R.; Ming-Shiang, W.; et al. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001, 21, 2895–2900. [Google Scholar]
- Soni, K.B.; Kuttan, R. Effect of oral curcumin administration on serum peroxides and cholesterol levels in human volunteers. Indian J. Physiol. Pharmacol. 1992, 36, 273–275. [Google Scholar]
- Lao, C.D.; Ruffin, M.T.t.; Normolle, D.; Heath, D.D.; Murray, S.I.; Bailey, J.M.; Boggs, M.E.; Crowell, J.; Rock, C.L.; Brenner, D.E. Dose escalation of a curcuminoid formulation. BMC Complement. Altern. Med. 2006, 6, 10. [Google Scholar] [CrossRef]
- Shoba, G.; Joy, D.; Joseph, T.; Majeed, M.; Rajendran, R.; Srinivas, P.S. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med. 1998, 64, 353–356. [Google Scholar] [CrossRef]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of curcumin: Problems and promises. Mol. Pharm. 2007, 4, 807–818. [Google Scholar] [CrossRef]
- Mollazade, M.; Nejati-Koshki, K.; Akbarzadeh, A.; Zarghami, N.; Nasiri, M.; Jahanban-Esfahlan, R.; Alibakhshi, A. PAMAM dendrimers augment inhibitory effects of curcumin on cancer cell proliferation: Possible inhibition of telomerase. Asian Pac. J. Cancer Prev. 2013, 14, 6925–6928. [Google Scholar] [CrossRef]
- Falconieri, M.C.; Adamo, M.; Monasterolo, C.; Bergonzi, M.C.; Coronnello, M.; Bilia, A.R. New Dendrimer-Based Nanoparticles Enhance Curcumin Solubility. Planta Med. 2017, 83, 420–425. [Google Scholar] [CrossRef]
- Gamage, N.H.; Jing, L.; Worsham, M.J.; Ali, M.M. Targeted Theranostic Approach for Glioma Using Dendrimer-Based Curcumin Nanoparticle. J. Nanomed. Nanotechnol. 2016, 7, 393. [Google Scholar]
- Wang, L.; Xu, X.; Zhang, Y.; Zhang, Y.; Zhu, Y.; Shi, J.; Sun, Y.; Huang, Q. Encapsulation of curcumin within poly(amidoamine) dendrimers for delivery to cancer cells. J. Mater. Sci. Mater. Med. 2013, 24, 2137–2144. [Google Scholar] [CrossRef]
- Gallien, J.; Srinageshwar, B.; Gallo, K.; Holtgrefe, G.; Koneru, S.; Otero, P.S.; Bueno, C.A.; Mosher, J.; Roh, A.; Kohtz, D.S.; et al. Curcumin Loaded Dendrimers Specifically Reduce Viability of Glioblastoma Cell Lines. Molecules 2021, 26, 6050. [Google Scholar] [CrossRef]
- Nosrati, H.; Adibtabar, M.; Sharafi, A.; Danafar, H.; Hamidreza Kheiri, M. PAMAM-modified citric acid-coated magnetic nanoparticles as pH sensitive biocompatible carrier against human breast cancer cells. Drug Dev. Ind. Pharm. 2018, 44, 1377–1384. [Google Scholar] [CrossRef]
- Wallace, D.C. Mitochondria and cancer. Nat. Rev. Cancer. 2012, 12, 685–698. [Google Scholar] [CrossRef]
- Kianamiri, S.; Dinari, A.; Sadeghizadeh, M.; Rezaei, M.; Daraei, B.; Bahsoun, N.E.; Nomani, A. Mitochondria-Targeted Polyamidoamine Dendrimer-Curcumin Construct for Hepatocellular Cancer Treatment. Mol. Pharm. 2020, 17, 4483–4498. [Google Scholar] [CrossRef]
- Ghaffari, M.; Dehghan, G.; Baradaran, B.; Zarebkohan, A.; Mansoori, B.; Soleymani, J.; Ezzati Nazhad Dolatabadi, J.; Hamblin, M.R. Co-delivery of curcumin and Bcl-2 siRNA by PAMAM dendrimers for enhancement of the therapeutic efficacy in HeLa cancer cells. Colloids Surf. B Biointerfaces 2020, 188, 110762. [Google Scholar] [CrossRef]
- Peddada, K.V.; Peddada, K.V.; Shukla, S.K.; Mishra, A.; Verma, V. Role of Curcumin in Common Musculoskeletal Disorders: A Review of Current Laboratory, Translational, and Clinical Data. Orthop. Surg. 2015, 7, 222–231. [Google Scholar] [CrossRef]
- Oh, S.; Kyung, T.W.; Choi, H.S. Curcumin inhibits osteoclastogenesis by decreasing receptor activator of nuclear factor-kappaB ligand (RANKL) in bone marrow stromal cells. Mol. Cells 2008, 26, 486–489. [Google Scholar]
- Yang, X.; Kuang, Z.; Yang, X.; Hu, X.; Luo, P.; Lai, Q.; Zhang, B.; Zhang, X.; Wei, Y. Facile synthesis of curcumin-containing poly(amidoamine) dendrimers as pH-responsive delivery system for osteoporosis treatment. Colloids Surf. B 2023, 222, 113029. [Google Scholar] [CrossRef]
- Yao, W.; Sun, K.; Mu, H.; Liang, N.; Liu, Y.; Yao, C.; Liang, R.; Wang, A. Preparation and characterization of puerarin-dendrimer complexes as an ocular drug delivery system. Drug Dev. Ind. Pharm. 2010, 36, 1027–1035. [Google Scholar] [CrossRef]
- Liu, Y.; Sun, K.; Yao, W.; Liang, N.; Mu, H.; Liang, R.; Yao, C. Corneal penetration of PAMAM dendrimers-coated puerarin liposomes. Zhongguo Zhong Yao Za Zhi 2010, 35, 30–34. [Google Scholar]
- Wang, W.Y.; Yao, C.; Shao, Y.F.; Mu, H.J.; Sun, K.X. Determination of puerarin in rabbit aqueous humor by liquid chromatography tandem mass spectrometry using microdialysis sampling after topical administration of puerarin PAMAM dendrimer complex. J. Pharm. Biomed. Anal. 2011, 56, 825–829. [Google Scholar] [CrossRef]
- Yao, W.J.; Sun, K.X.; Liu, Y.; Liang, N.; Mu, H.J.; Yao, C.; Liang, R.C.; Wang, A.P. Effect of poly(amidoamine) dendrimers on corneal penetration of puerarin. Biol. Pharm. Bull. 2010, 33, 1371–1377. [Google Scholar] [CrossRef]
- Yao, C.; Wang, W.; Zhou, X.; Qu, T.; Mu, H.; Liang, R.; Wang, A.; Sun, K. Effects of poly(amidoamine) dendrimers on ocular absorption of puerarin using microdialysis. J. Ocul. Pharmacol. Ther. 2011, 27, 565–569. [Google Scholar] [CrossRef]
- Gu, L.; Wu, Z.h.; Qi, X.; He, H.; Ma, X.; Chou, X.; Wen, X.; Zhang, M.; Jiao, F. Polyamidomine dendrimers: An excellent drug carrier for improving the solubility and bioavailability of puerarin. Pharm. Dev. Technol. 2012, 18, 1051–1057. [Google Scholar] [CrossRef]
- Wang, G.; Zhou, Z.; Zhao, Z.; Li, Q.; Wu, Y.; Yan, S.; Shen, Y.; Huang, P. Enzyme-Triggered Transcytosis of Dendrimer–Drug Conjugate for Deep Penetration into Pancreatic Tumors. ACS Nano 2020, 14, 4890–4904. [Google Scholar] [CrossRef]
- Bhatt, H.; Kiran Rompicharla, S.V.; Ghosh, B.; Biswas, S. Alpha-Tocopherol Succinate-Anchored PEGylated Poly(amidoamine) Dendrimer for the Delivery of Paclitaxel: Assessment of In Vitro and In Vivo Therapeutic Efficacy. Mol. Pharm. 2019, 16, 1541–1554. [Google Scholar] [CrossRef]
- Liu, J.; Li, J.; Liu, N.; Guo, N.; Gao, C.; Hao, Y.; Chen, L.; Zhang, X. In vitro studies of phospholipid-modified PAMAM-siMDR1 complexes for the reversal of multidrug resistance in human breast cancer cells. Int. J. Pharm. 2017, 530, 291–299. [Google Scholar] [CrossRef]
- Mei, M.; Ren, Y.; Zhou, X.; Yuan, X.B.; Han, L.; Wang, G.X.; Jia, Z.; Pu, P.Y.; Kang, C.S.; Yao, Z. Downregulation of miR-21 enhances chemotherapeutic effect of taxol in breast carcinoma cells. Technol. Cancer Res. Treat. 2010, 9, 77–86. [Google Scholar] [CrossRef]
- Sharma, R.; Kambhampati, S.P.; Zhang, Z.; Sharma, A.; Chen, S.; Duh, E.I.; Kannan, S.; Tso, M.O.M.; Kannan, R.M. Dendrimer mediated targeted delivery of sinomenine for the treatment of acute neuroinflammation in traumatic brain injury. J. Control. Release 2020, 323, 361–375. [Google Scholar] [CrossRef]
- Tripathi, P.K.; Gupta, S.; Rai, S.; Shrivatava, A.; Tripathi, S.; Singh, S.; Khopade, A.J.; Kesharwani, P. Curcumin loaded poly (amidoamine) dendrimer-plamitic acid core-shell nanoparticles as anti-stress therapeutics. Drug Dev. Ind. Pharm. 2020, 46, 412–426. [Google Scholar] [CrossRef]
- Lv, T.; Yu, T.; Fang, Y.; Zhang, S.; Jiang, M.; Zhang, H.; Zhang, Y.; Li, Z.; Chen, H.; Gao, Y. Role of generation on folic acid-modified poly(amidoamine) dendrimers for targeted delivery of baicalin to cancer cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 75, 182–190. [Google Scholar] [CrossRef]
- Zhao, C.; Wang, Y.; Su, Y.; Zhang, H.; Ding, L.; Yan, X.; Zhao, D.; Shao, N.; Ye, X.; Cheng, Y. Inclusion complexes of isoflavones with two commercially available dendrimers: Solubility, stability, structures, release behaviors, cytotoxicity, and anti-oxidant activities. Int. J. Pharm. 2011, 421, 301–309. [Google Scholar] [CrossRef]
- Yesil-Celiktas, O.; Pala, C.; Cetin-Uyanikgil, E.O.; Sevimli-Gur, C. Synthesis of silica-PAMAM dendrimer nanoparticles as promising carriers in Neuro blastoma cells. Anal. Biochem. 2017, 519, 1–7. [Google Scholar] [CrossRef]


| No. | Type of Compounds | Compounds | Type of Dendrimers | Characteristic | Application | Mode of Administration | Refs. |
|---|---|---|---|---|---|---|---|
| 1 | alkaloid | CPT | PEGylated PAMAM G5 dendrimers–AS1411 antinucleolin aptamers (Encapsulation efficiency (EE) = 93.67%, loading content% (LC) = 8.1%) | specific targeting | BALB/c female mice bearing C26 tumors | intravenous injection (200 mL) | [21] |
| 2 | alkaloid | CPT | N-acetyl-D-glucosamine-labelled–PAMAM G3.5 dendrimers (EE = 66.26 ± 2.72%) | specific targeting | mice with B16F10 lung metastasis | intravenous injection | [22] |
| 3 | alkaloid | CPT | amine-terminated PAMAM G4 dendrimers–succinic acid-glycine linker | absence of small molecular weight impurities, size and drug content | colorectal cancer cells HCT-116 | in vitro experiments | [23] |
| 4 | alkaloid | CPT | Glucose–PEG–PAMAM–S–CPT–Cy7 | specific targeting, cellular microenvironment responsive | monolayer (2D) and multilayer tumor spheroid (3D) HepG2 cancer cell models GLUT | in vitro experiments | [24] |
| 5 | alkaloid | CPT | PAMAM G3 dendrimers–CPT with acrylate end groups | self-cleaving mechanism | HN12 head and neck tumor-bearing mouse | injection (0.16 mg of CPT in 50 μL/mouse) | [25] |
| 6 | alkaloid | CPT | PEGylated PLL dendrimers–glycine linker | improved the bioavailability, solubility, and efficacy of CPT | mouse (C26) and human colon cancer cells HT-29 | intravenous injection (single dose of CPT 10 mg/kg) | [26] |
| 7 | alkaloid | CPT | PAMAM dendrimers–ROS–cleavable thioketal linker–CPT–surface modification with GGT | enzyme-triggered transcytosis | mice inoculated with BxPC-3 orthotopic pancreatic ductal adenocarcinoma | intravenous injection (equivalent to CPT 10 mg/kg) | [127] |
| 8 | alkaloid | PTX | dodecyl groups and diethylethanolamine surface-modified cationic PAMAM dendrimers | its high DNA binding ability and TLR inhibition activity, low toxicity, and smaller nanoparticle (NP) size. | a murine breast cancer metastasis model | intraperitoneal injection (15 mg/kg) | [30] |
| 9 | alkaloid | PTX | PAMAM G4 dendrimers–α-TOS–PEGylated Transferrin (EE = 71.18 ± 2.38%) | specific targeting | human cervical epithelial cells HeLa | in vitro experiments | [31] |
| 10 | alkaloid | PTX | PEGylated PAMAM G4 dendrimers–α-TOS | specific targeting | murine melanoma cancer cells (B16F10) xenografted C57Bl6/J mice | intratumoral injections (10 mg/kg/day) | [128] |
| 11 | alkaloid | PTX | PEGylated PAMAM G4 dendrimers–Biotin | specific targeting | human non-small cell lung cancer A549 cell line | in vitro experiments | [32] |
| 12 | alkaloid | PTX | PAMAMG4.0-NH2 dendrimers–omega-3 fatty acid docosahexaenoic acid | specific targeting | upper gastrointestinal cancers cells AGS and FLO-1 | in vitro experiments | [33] |
| 13 | alkaloid | PTX | PAMAM-alkali blue dendrimers | the intralymphatic targeting | tumor-bearing mice | subcutaneous administration (1 mg/kg) | [34] |
| 14 | alkaloid | PTX | PEGylated PAMAM G4 dendrimer–PEG–R8 | intracellular targetability | human cervical cancer cell line HeLa | in vitro experiments | [35] |
| 15 | alkaloid | PTX | PEGylated PAMAM G4 dendrimers–R8–vitamin-E succinate | cell penetration and improved PTX-mediated cytotoxicity | B16F10 tumor-bearing mice | intraperitoneal injection (10 mg/kg) | [36] |
| 16 | alkaloid | PTX | Sialic acid/glucosamine/concanavalin A/thiamine–PPI G5.0 dendrimers | specific targeting | human astrocytoma cells U373MG/human neuroblastoma cells IMR-32 | in vitro experiments | [37,38] |
| 17 | alkaloid | PTX | triazine dendrimers | no adverse toxicity, increases its water solubility | BALB/c mice | intraperitoneal injection (40/60/100/200/500 mg/kg) | [39] |
| 18 | alkaloid | PTX | PG dendrimers | solubilization | different solvents | in vitro experiments | [40] |
| 19 | alkaloid | PTX | lauryl chains-modified PAMAM G3 dendrimers–glutaric anhydride linker | high permeability | human colon adenocarcinoma cell line Caco-2, primary cultured porcine brain endothelial cells | in vitro experiments | [41] |
| 20 | alkaloid | PTX | PAMAM G4 dendrimers–succinic acid linker | cytoplasmic and nuclear delivery, enhanced anticancer activity of PTX | human ovarian carcinoma cells A2780 | in vitro experiments | [42] |
| 21 | alkaloid | PTX | Janus PEGylated peptide dendrimers–GFLG | enzyme-responsive feature | murine breast cancer cells 4T1 (tumor-bearing mice) | intravenous injection (5 mg/kg body weight each day for 10 days) | [43] |
| 22 | alkaloid | PTX | PAMAM G4 dendrimers–GFLG | specific targeting | breast cancer cell (MDA MB-231) mouse | intraperitoneal injection (40 mg/kg) | [44] |
| 23 | alkaloid | PTX | dendrimers–plectin-1 targeted peptide –nuclear receptor siRNA | tumor-targeted, redox-sensitive | panc-1 xenograft-bearing mice | intravenous injection | [46] |
| 24 | alkaloid | PTX | a triethanolamine-core PAMAM G6 dendrimers–Akt siRNA | initiating Akt target gene silencing both in vitro and in vivo, while being minimally toxic | mice containing human ovarian cancer cells SKOV-3 | intraperitoneal injection (2 mg/kg/week) | [47] |
| 25 | alkaloid | PTX | phospholipid-modified PAMAM dendrimers–siMDR1 | siRNA encapsulation ability, high gene delivery efficiency, and great cellular uptake | human breast cancer cells MCF-7/ADR | in vitro experiments | [129] |
| 26 | alkaloid | PTX | PAMAM G5 dendrimers–miR-21 inhibitor | improved the cytotoxicity of PTX increased the level of apoptosis of MCF-7 cells, decreased the invasiveness of the tumor cells | human breast adenocarcinoma cells MCF-7 | in vitro experiments | [130] |
| 27 | alkaloid | BBR | PEGylated PAMAM G4 dendrimers (EE = 69.56 ± 23%) | controlled the release of drug, enhanced its bioavailability | human breast cancer cells MCF-7 | in vitro experiments | [54] |
| 28 | alkaloid | sinomenine | hydroxy PAMAM G4 dendrimers with ethylenediamine nucleus (64 hydroxyl terminal groups) | increasing the therapeutic window in the treatment of early inflammation and for improving the efficacy of the drug in TBI | rabbit model of pediatric traumatic brain injury | intravenous injection (55 mg/kg, 200 μL) | [131] |
| 29 | polyphenol | quercetin | PAMAM G3 dendrimers | enhancing longer biological half-life | rats using a carrageenan-induced paw edema model | oral administration (20 mg/kg body weight) | [73] |
| 30 | polyphenol | quercetin | PEGylated PAMAM G4 dendrimer–Margetuximab | specific targeting | human breast cancer cells MDA-MB-231 | in vitro experiments | [75] |
| 31 | polyphenol | quercetin | PAMAM-b-PEG-folic acid-modified Fe3O4 nanoparticles | pH-responsiveness, specific targeting | HeLa human cervical cancer cells, human breast cancer cells MDA-MB-231 | in vitro experiments | [76] |
| 32 | polyphenol | GA | PAMAM G4 dendrimers | specific targeting, improved the bioavailability | human colon carcinoma cells HCT-116, human breast cancer MCF-7 | in vitro experiments | [79,80] |
| 33 | polyphenol | GA | PAMAM-G4-NH2 dendrimers | improved the bioavailability, increased hepatoprotective effect | CCl4-induced oxidative damage in rat liver | oral administration (50 mg/kg/day, 7 days) | [81] |
| 34 | polyphenol | RSV | PAMAM G4 dendrimers | enhanced solubility, stability and transdermal permeation | simulated gastric and simulated intestinal fluid, rat skin | in vitro experiments | [88] |
| 35 | polyphenol | RSV | SMDG | improved bioavailability | human intestinal cells Caco-2 | in vitro experiments | [89] |
| 36 | polyphenol | RSV | OHPP dendrimers | solubilization | solvents included ethanol, methanol, isopropanol, chloroform, acetonitrile, butanol, dimethyl sulfoxide (DMSO), pyridine, simulated gastric fluid, McIlvaine buffers | in vitro experiments | [90] |
| 37 | polyphenol | SIL | PAMAM G2 dendrimers | improved bioavailability | rats | oral administration (12 mg/kg) | [94] |
| 38 | polyphenol | SIL | PEGylated PAMAM G4 dendrimers | solubilization | DMSO | in vitro experiments | [95] |
| 39 | polyphenol | SIL | peptide dendrimers | enhanced skin permeation and deposition | rat skin | in vitro experiments | [96] |
| 40 | polyphenol | CUR | PAMAM G0.5 dendrimers/CUR (1:1/1:0.5) | improved solubility | mixture of distilled water and EtOH | in vitro experiments | [110] |
| 41 | polyphenol | CUR | PAMAM G3 dendrimers | full solubility, specific targeting, minimizing systemic toxic effect | breast cancer cells MDA-MB-231, human malignant glioma U-251, squamous head and neck cancer cells HNSCC, breast cancer cell line T47D | in vitro experiments | [109,111] |
| 42 | polyphenol | CUR | PAMAM G5 dendrimers with acetyl terminal groups | improved solubility and bioavailability | human lung adenocarcinoma cells A549 | in vitro experiments | [112] |
| 43 | polyphenol | CUR | PAMAM dendrimers (10% amine and 90% hydroxyl-G4 90/10-Cys) | safe, only toxic to cancer cells | glioblastoma cell lines: mouse-GL261, rat-F98, and human-U87 | in vitro experiments | [113] |
| 44 | polyphenol | CUR | PAMAM G5 dendrimers–modified citric acid coated Fe3O4 (EE = 45.58 ± 0.41%, LC = 12 ± 0.03%) | pH-responsiveness | human breast cancer cell line MCF7 | in vitro experiments | [114] |
| 45 | polyphenol | CUR | PAMAM G4 dendrimers–TPP | mitochondrial targeting | HuH-7, Jurkat T cell, Hepa1-6, and human and mouse fibroblasts | in vitro experiments | [116] |
| 46 | polyphenol | CUR | PAMAM G4 dendrimers–Bcl-2 siRNA (LC = 82 wt%) | improved solubility and bioavailability, induced the most apoptosis in HeLa cancer cells | HeLa cells | in vitro experiments | [117] |
| 47 | polyphenol | CUR | PAMAM dendrimers–HCCP linker | pH-responsiveness | bone marrow macrophage cells BMMs | in vitro experiments | [120] |
| 48 | polyphenol | CUR | PAMAM G4 dendrimers–palmitic acid core–shell nanoparticle (EE = 80.87%) | potentially active against acute stress | adult male albino mice | intravenous injection (25 mg/kg) | [132] |
| 49 | polyphenol | PUE | PAMAM G3.5/G4/G4.5/G5 dendrimers | improved the corneal permeation | corneas of each male New Zealand albino rabbit | drip into the cornea (50 μL) | [121] |
| 50 | polyphenol | PUE | PAMAM G3/G4/G5 dendrimers | improved the corneal permeation | rabbit aqueous humor | instillation (0.5 mg, 1% PUE solutions) | [123,124,125] |
| 51 | polyphenol | PUE | PAMAM G2 dendrimers | improved solubility and bioavailability | rats | oral administration (130 mg/kg PUE) | [126] |
| 52 | polyphenol | baicalin | PAMAM dendrimers–folic acid | specific targeting | HeLa human epithelial carcinoma cell line, human lung carcinoma cell line A549 | in vitro experiments | [133] |
| 53 | polyphenol | daidzein | PAMAM G3 dendrimers, PPI G4 dendrimers | improved solubility, prolonged the delivery, and maintained the antioxidant activity | human breast cancer MCF-7, human lung carcinoma cells A549 | in vitro experiments | [134] |
| 54 | polyphenol | anthocyanin | PAMAM dendrimers–silica | inhibiting the proliferative effects of Neuro 2A cancer cells, non-toxicity to the cells | Neuro 2A cancer cells | in vitro experiments | [135] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
An, H.; Deng, X.; Wang, F.; Xu, P.; Wang, N. Dendrimers as Nanocarriers for the Delivery of Drugs Obtained from Natural Products. Polymers 2023, 15, 2292. https://doi.org/10.3390/polym15102292
An H, Deng X, Wang F, Xu P, Wang N. Dendrimers as Nanocarriers for the Delivery of Drugs Obtained from Natural Products. Polymers. 2023; 15(10):2292. https://doi.org/10.3390/polym15102292
Chicago/Turabian StyleAn, Huan, Xuehui Deng, Fang Wang, Pingcui Xu, and Nani Wang. 2023. "Dendrimers as Nanocarriers for the Delivery of Drugs Obtained from Natural Products" Polymers 15, no. 10: 2292. https://doi.org/10.3390/polym15102292
APA StyleAn, H., Deng, X., Wang, F., Xu, P., & Wang, N. (2023). Dendrimers as Nanocarriers for the Delivery of Drugs Obtained from Natural Products. Polymers, 15(10), 2292. https://doi.org/10.3390/polym15102292





