Climate Change, Obesity, and COVID-19—Global Crises with Catastrophic Consequences. Is This the Future?
Abstract
:1. Introduction
2. Materials and Methods
3. Results and Discussion
3.1. High Temperatures and Obesity
3.2. Low Temperatures and Obesity
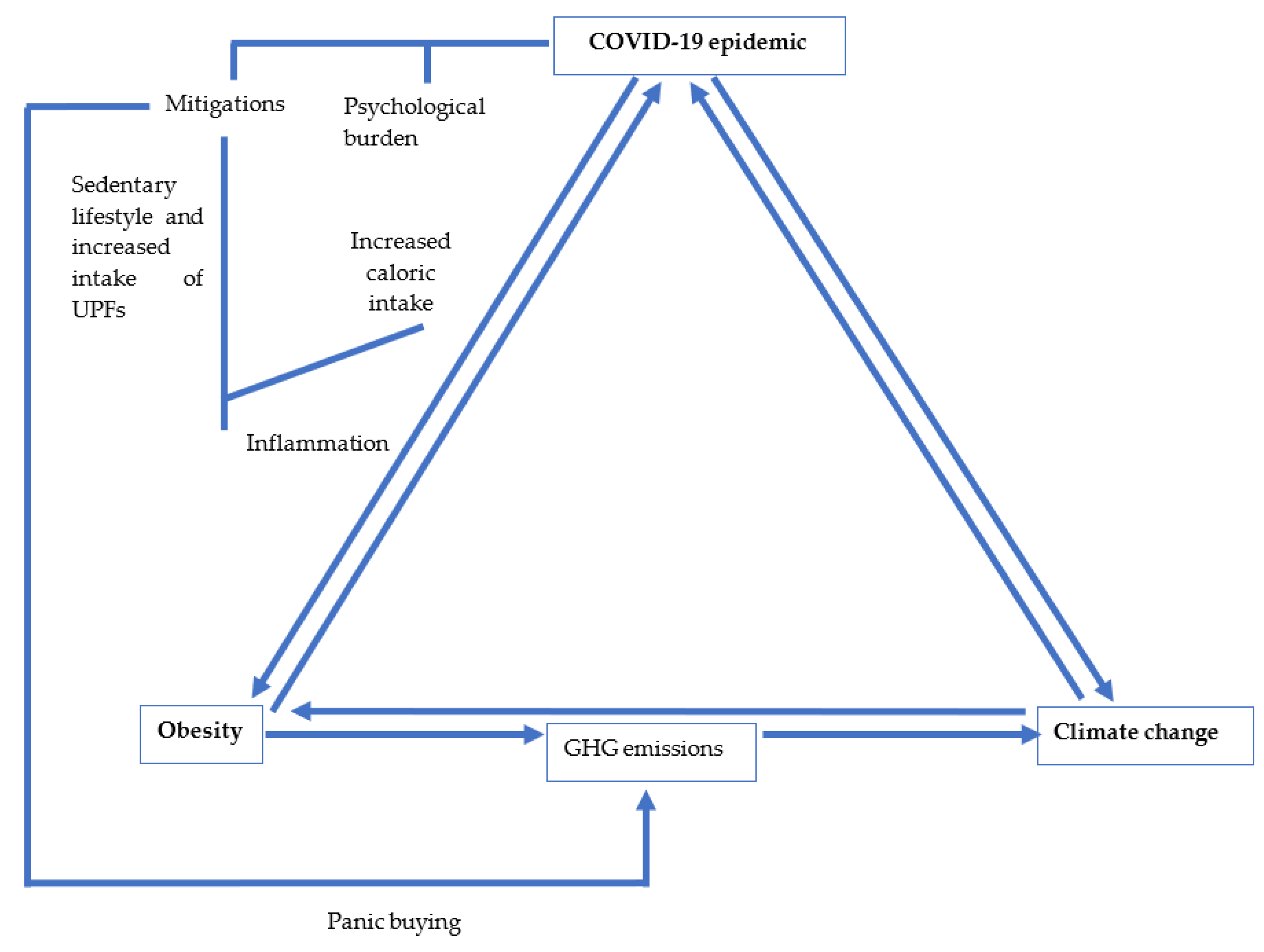
3.3. COVID-19, Obesity, and Climate Change
3.3.1. Indirect Effects of COVID-19 on Obesity and Climate Change
3.3.2. Direct Effects of COVID-19 on Obesity and Climate Change
3.4. Implications for Policy
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The global syndemic of obesity, undernutrition, and climate change: The lancet commission report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Last, J.M. A Dictionary of Epidemiology, 4th ed.; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Houghton, J.T.; Ding, Y.; Griggs, D.J.; Noguer, M.; van der Linden, P.J.; Dai, X.; Maskell, K.; Johnson, C.A. Climate Change 2001: The Scientific Basis Contribution of Working Group I to the Third Assessment Report of the Intergovernmental Panel on Climate Change Published for the Intergovernmental Panel on Climate Change. 2001. Available online: http://www.cambridge.org (accessed on 20 March 2020).
- Rockström, J.; Steffen, W.; Noone, K.; Persson, Å.; Stuart Chapin, F., III; Lambin, E.F.; Lenton, T.M.; Scheffer, M.; Folke, C.; Schellnhuber, H.J.; et al. A safe operating space for humanity. Nature 2009, 461, 472–475. [Google Scholar] [CrossRef] [PubMed]
- Olivier, J.; Janssens-Maenhout, G.; Muntean, M.; Peters, J. Trends in global CO2 Emissions: 2013 Report (PBL Netherlands Environ-Mental Assessment Agency). 2013. Available online: https://www.pbl.nl/en/publications/long-term-trend-in-global-co2-emissions-2011-report (accessed on 20 March 2020).
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Jaacks, L.M.; Vandevijvere, S.; Pan, A.; McGowan, C.; Wallace, C.; Imamura, F.; Mozaffarian, D.; Swinburn, B.; Ezzati, M. The obesity transition: Stages of the global epidemic. Lancet Diabetes Endocrinol. 2019, 7, 231–240. [Google Scholar] [CrossRef]
- Burki, T. European Commission classifies obesity as a chronic disease. Lancet Diabetes Endocrinol. 2021, 9, 418. [Google Scholar] [CrossRef]
- Lobstein, T.; Brinsden, H. Obesity: Missing the 2025 Global Targets. 2020. Available online: www.worldobesity.org (accessed on 19 August 2021).
- Magkos, F.; Tetens, I.; Bügel, S.G.; Felby, C.; Schacht, S.R.; Hill, J.O.; Ravussin, E.; Astrup, A. The environmental foodprint of obesity. Obesity 2019, 28, 73–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swinburn, B. The obesity and climate change nexus. Obesity 2019, 28, 8. [Google Scholar] [CrossRef] [PubMed]
- Webb, G.J.; Egger, G. Obesity and climate change. Am. J. Lifestyle Med. 2013, 8, 200–204. [Google Scholar] [CrossRef]
- Minos, D.; Butzlaff, I.; Demmler, K.M.; Rischke, R. Economic growth, climate change, and obesity. Curr. Obes. Rep. 2016, 5, 441–448. [Google Scholar] [CrossRef] [Green Version]
- Tabari, P.; Amini, M.; Moghadami, M.; Moosavi, M. International public health responses to COVID-19 outbreak: A rapid review. Iran. J. Med. Sci. 2020, 45, 157–169. [Google Scholar]
- Du, J.; Rakha, H.A.; Filali, F.; Eldardiry, H. COVID-19 pandemic impacts on traffic system delay, fuel consumption and emissions. Int. J. Transp. Sci. Technol. 2021, 10, 184–196. [Google Scholar] [CrossRef]
- Janssen, M.; Chang, B.P.I.; Hristov, H.; Pravst, I.; Profeta, A.; Millard, J. Changes in food consumption during the COVID-19 Pandemic: Analysis of consumer survey data from the first lockdown period in Denmark, Germany, and Slovenia. Front. Nutr. 2021, 8, 635859. [Google Scholar] [CrossRef]
- Amini, H.; Habibi, S.; Islamoglu, A.H.; Isanejad, E.; Uz, C.; Daniyari, H. COVID-19 pandemic-induced physical inactivity: The necessity of updating the Global Action Plan on Physical Activity 2018–2030. Environ. Health Prev. Med. 2021, 26, 1–3. [Google Scholar] [CrossRef]
- National Geographic Society. Climate Change. Natl. Geogr. Soc. 2019. Available online: https://www.nationalgeographic.org/encyclopedia/climate-change/ (accessed on 20 September 2021).
- An, R.; Ji, M.; Zhang, S. Global warming and obesity: A systematic review. Obes. Rev. 2017, 19, 150–163. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Hawk, T.; Aggarwal, A.; Drewnowski, A. Characterizing ultra-processed foods by energy density, nutrient density, and cost. Front. Nutr. 2019, 6, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moubarac, J.-C.; Batal, M.; Louzada, M.L.; Martinez Steele, E.; Monteiro, C.A. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite 2017, 108, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Louzada, M.L.d.C.; Martins, A.P.B.; Canella, D.S.; Baraldi, L.G.; Levy, R.B.; Claro, R.M.; Moubarac, J.-C.; Cannon, G.; Monteiro, C.A. Ultra-processed foods and the nutritional dietary profile in Brazil. Rev. Saude Publica 2015, 49. [Google Scholar] [CrossRef]
- Poti, J.M.; Mendez, M.A.; Ng, S.W.; Popkin, B.M. Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households? Am. J. Clin. Nutr. 2015, 101, 1251–1262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martínez Steele, E.; Baraldi, L.G.; da Costa Louzada, M.L.; Moubarac, J.-C.; Mozaffarian, D.; Monteiro, C.A. Ultra-processed foods and added sugars in the US diet: Evidence from a nationally representative cross-sectional study. BMJ Open 2016, 6, e009892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Costa Louzada, M.L.; Baraldi, L.G.; Steele, E.M.; Martins, A.P.B.; Canella, D.S.; Moubarac, J.-C.; Levy, R.B.; Cannon, G.; Afshin, A.; Imamura, F.; et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev. Med. 2015, 81, 9–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, C.A.; Moubarac, J.-C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system: Ultra-processed products: Global dominance. Obes. Rev. 2013, 14, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Galdamez, D.H.; González-Block, M.Á.; Romo-Dueñas, D.K.; Lima-Morales, R.; Hernández-Vicente, I.A.; Lumbreras-Guzmán, M.; Méndez-Hernández, P. Increased risk of hospitalization and death in patients with COVID-19 and pre-existing noncommunicable diseases and modifiable risk factors in Mexico. Arch. Med. Res. 2020, 51, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Muka, T.; Imo, D.; Jaspers, L.; Colpani, V.; Chaker, L.; van der Lee, S.; Mendis, S.; Chowdhury, R.; Bramer, W.; Falla, A.; et al. The global impact of non-communicable diseases on healthcare spending and national income: A systematic review. Eur. J. Epidemiology 2015, 30, 251–277. [Google Scholar] [CrossRef] [PubMed]
- Tomson, C. Reducing the carbon footprint of hospital-based care. Futur. Hosp. J. 2015, 2, 57–62. [Google Scholar] [CrossRef]
- Salas, R.N.; Maibach, E.; Pencheon, D.; Watts, N.; Frumkin, H. A pathway to net zero emissions for healthcare. BMJ 2020, 371, m3785. [Google Scholar] [CrossRef] [PubMed]
- Budd, K. Hospitals Race to Save Patients—And the Planet. AAMC. 2019. Available online: https://www.aamc.org/news-insights/hospitals-race-save-patients-and-planet (accessed on 23 September 2021).
- Walpole, S.C.; Prieto-Merino, D.; Edwards, P.; Cleland, J.; Stevens, G.; Roberts, I. The weight of nations: An estimation of adult human biomass. BMC Public Health 2012, 12, 439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pradhan, P.; Reusser, D.E.; Kropp, J. Embodied greenhouse gas emissions in diets. PLoS ONE 2013, 8, e62228. [Google Scholar] [CrossRef] [Green Version]
- Prentice, A.M.; Black, A.E.; Coward, W.A.; Cole, T.J. Energy expenditure in overweight and obese adults in affluent societies: An analysis of 319 doubly-labelled water measurements. Eur. J. Clin. Nutr. 1996, 50, 93–97. [Google Scholar]
- Hiç, C.; Pradhan, P.; Rybski, D.; Kropp, J. Food surplus and its climate burdens. Environ. Sci. Technol. 2016, 50, 4269–4277. [Google Scholar] [CrossRef] [Green Version]
- IPCC. Global Warming of 1.5 °C. Available online: https://www.ipcc.ch/sr15/ (accessed on 19 August 2021).
- Edwards, P.; Roberts, I. Population adiposity and climate change. Int. J. Epidemiology 2009, 38, 1137–1140. [Google Scholar] [CrossRef]
- Kim, J.-S.; Kug, J.-S.; Jeong, S.-J.; Huntzinger, D.N.; Michalak, A.M.; Schwalm, C.; Wei, Y.; Schaefer, K. Reduced North American terrestrial primary productivity linked to anomalous Arctic warming. Nat. Geosci. 2017, 10, 572–576. [Google Scholar] [CrossRef]
- Cohen, J.; Pfeiffer, K.; Francis, J.A. Warm Arctic episodes linked with increased frequency of extreme winter weather in the United States. Nat. Commun. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Habibzadeh, N. Why Physiologically cold weather can increase obesity rates? Int. Physiol. J. 2018, 2, 11–13. [Google Scholar] [CrossRef]
- Wagner, A.L.; Keusch, F.; Yan, T.; Clarke, P.J. The impact of weather on summer and winter exercise behaviors. J. Sport Health Sci. 2019, 8, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M. The relationship between obesity and seasonal variation in body weight among elementary school children in Tokyo. Econ. Hum. Biol. 2006, 4, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Von Hippel, P.; Benson, R. Obesity and the natural environment across US counties. Am. J. Public Health 2014, 104, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, K.M.; Pereira, M.A.; Jacobs, D.R.; Sidney, S.; Odegaard, A.O. sedentary behavior, physical activity, and abdominal adipose tissue deposition. Med. Sci. Sports Exerc. 2017, 49, 450–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutherland, K.; Chessman, J.; Zhao, J.; Sara, G.; Went, A.; Dyson, S.; Levesque, J.-F. Impact of COVID-19 on healthcare activity in NSW, Australia. Public Health Res. Pr. 2020, 30. [Google Scholar] [CrossRef]
- Mercier, G.; Arquizan, C.; Roubille, F. Understanding the effects of COVID-19 on health care and systems. Lancet Public Health 2020, 5, e524. [Google Scholar] [CrossRef]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef]
- Jia, P.; Zhang, L.; Yu, W.; Yu, B.; Liu, M.; Zhang, D.; Yang, S. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: The COVID-19 impact on lifestyle change survey (COINLICS). Int. J. Obes. 2021, 45, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Mulugeta, W.; Desalegn, H.; Solomon, S. Impact of the COVID-19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin. Obes. 2021, 11, e12453. [Google Scholar] [CrossRef] [PubMed]
- Le Quéré, C.; Jackson, R.B.; Jones, M.W.; Smith, A.; Abernethy, S.; Andrew, R.M.; De-Gol, A.J.; Willis, D.R.; Shan, Y.; Canadell, J.G.; et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat. Clim. Chang. 2020, 10, 647–653. [Google Scholar] [CrossRef]
- Tollefson, J. COVID curbed carbon emissions in 2020—But not by much. Nat. Cell Biol. 2021, 589, 343. [Google Scholar] [CrossRef]
- Carbon Dioxide Levels Continue at Record Levels, Despite COVID-19 Lockdown; The World Meteorological Organization: Geneva, Switzerland, 2020.
- Maalouf, A.; Maalouf, H. Impact of COVID-19 pandemic on medical waste management in Lebanon. Waste Manag. Res. 2021, 39, 45–55. [Google Scholar] [CrossRef]
- Galanakis, C.M. The food systems in the era of the Coronavirus (COVID-19) pandemic crisis. Foods 2020, 9, 523. [Google Scholar] [CrossRef]
- Fanelli, R. Changes in the food-related behaviour of Italian consumers during the COVID-19 pandemic. Foods 2021, 10, 169. [Google Scholar] [CrossRef]
- Public Health England. Impact of COVID-19 Pandemic on Grocery Shopping Behaviours. London: 2020. Available online: www.facebook.com/PublicHealthEngland (accessed on 20 September 2021).
- Posel, D.; Oyenubi, A.; Kollamparambil, U. Job loss and mental health during the COVID-19 lockdown: Evidence from South Africa. PLoS ONE 2021, 16, e0249352. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Coronavirus and Redundancies in the UK Labour Market. Off. Natl. Stat. 2020. Available online: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/articles/labourmarketeconomicanalysisquarterly/december2020 (accessed on 20 September 2021).
- Vandevijvere, S.; Pedroni, C.; De Ridder, K.; Castetbon, K. The cost of diets according to their caloric share of ultraprocessed and minimally processed foods in Belgium. Nutrition 2020, 12, 2787. [Google Scholar] [CrossRef]
- Allabadi, H.; Dabis, J.; Aghabekian, V.; Khader, A.; Khammash, U. Impact of COVID-19 lockdown on dietary and lifestyle behaviours among adolescents in Palestine. Dynam. Hum. Health 2020, 7, 2170. [Google Scholar] [CrossRef]
- Clemmensen, C.; Petersen, M.B.; Sørensen, T.I.A. Will the COVID-19 pandemic worsen the obesity epidemic? Nat. Rev. Endocrinol. 2020, 16, 469–470. [Google Scholar] [CrossRef]
- Ulrich-Lai, Y.; Ryan, K.K. Neuroendocrine circuits governing energy balance and stress regulation: Functional overlap and therapeutic implications. Cell Metab. 2014, 19, 910–925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marazziti, D.; Cianconi, P.; Mucci, F.; Foresi, L.; Chiarantini, I.; Della Vecchia, A. Climate change, environment pollution, COVID-19 pandemic and mental health. Sci. Total Environ. 2021, 773, 145182. [Google Scholar] [CrossRef] [PubMed]
- Palinkas, L.A.; Wong, M. Global climate change and mental health. Curr. Opin. Psychol. 2020, 32, 12–16. [Google Scholar] [CrossRef]
- Hills, A.P.; King, N.A.; Armstrong, T.P. The contribution of physical activity and sedentary behaviours to the growth and development of children and adolescents: Implications for overweight and obesity. Sports Med. 2007, 37, 533–545. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Public Health. Childhood obesity beyond COVID-19. Lancet Public Health 2021, 6, e534. [Google Scholar] [CrossRef]
- Scully, M.; Dixon, H.; Wakefield, M. Association between commercial television exposure and fast-food consumption among adults. Public Health Nutr. 2009, 12, 105–110. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, L.; et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020, 88, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Zakka, K.; Chidambaram, S.; Mansour, S.; Mahawar, K.; Salminen, P.; Almino, R.; Schauer, P.; Kinross, J.; Purkayastha, S.; on behalf of the PanSurg Collaborative; Chidambaram, S. SARS-CoV-2 and obesity: “CoVesity”—A pandemic within a pandemic. Obes. Surg. 2021, 31, 1–10. [Google Scholar] [CrossRef]
- Klemeš, J.J.; Van Fan, Y.; Jiang, P. The energy and environmental footprints of COVID-19 fighting measures—PPE, disinfection, supply chains. Energy 2020, 211, 118701. [Google Scholar] [CrossRef] [PubMed]
- Gillingham, K.T.; Knittel, C.R.; Li, J.; Ovaere, M.; Reguant, M. The Short-run and Long-run Effects of Covid-19 on Energy and the Environment. Joule 2020, 4, 1337–1341. [Google Scholar] [CrossRef] [PubMed]
- Laverty, A.A.; Millett, C.; Majeed, A.; Vamos, E.P. COVID-19 presents opportunities and threats to transport and health. J. R. Soc. Med. 2020, 113, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.; Shen, Q.; Fan, L.C.; Wang, Y.; Zhang, L. Greenhouse gas emissions in building construction: A case study of One Peking in Hong Kong. Build. Environ. 2010, 45, 949–955. [Google Scholar] [CrossRef] [Green Version]
- Hu, Y.; Barbour, W.; Samaranayake, S.; Work, D. Impacts of Covid-19 mode shift on road traffic. arXiv 2020, arXiv:2005.01610. [Google Scholar]
- Galanti, T.; Guidetti, G.; Mazzei, E.; Zappalà, S.; Toscano, F. Work from home during the COVID-19 outbreak. J. Occup. Environ. Med. 2021, 63, e426–e432. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- McLaughlin, T.; Ackerman, S.E.; Shen, L.; Engleman, E. Role of innate and adaptive immunity in obesity-associated metabolic disease. J. Clin. Investig. 2017, 127, 5–13. [Google Scholar] [CrossRef] [Green Version]
- Cuschieri, S.; Grech, S. Obesity population at risk of COVID-19 complications. Glob. Health Epidemiol. Genom. 2020, 5. [Google Scholar] [CrossRef]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A.; Labreuche, J.; Mathieu, D.; Pattou, F.; Jourdain, M.; et al. High prevalence of obesity in severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity 2020, 28, 1195–1199. [Google Scholar] [CrossRef]
- Senthilingam, M. Covid-19 has made the obesity epidemic worse, but failed to ignite enough action. BMJ 2021, 372, n411. [Google Scholar] [CrossRef] [PubMed]
- Landier, J.; Paireau, J.; Rebaudet, S.; Legendre, E.; Lehot, L.; Fontanet, A.; Cauchemez, S.; Gaudart, J. Cold and dry winter conditions are associated with greater SARS-CoV-2 transmission at regional level in western countries during the first epidemic wave. Sci. Rep. 2021, 11, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.B. Epidemics on the move: Climate change and infectious disease. PLoS Biol. 2020, 18, e3001013. [Google Scholar] [CrossRef] [PubMed]
- Usman, M.; Husnain, M.; Riaz, A.; Riaz, A.; Ali, Y. Climate change during the COVID-19 outbreak: Scoping future perspectives. Environ. Sci. Pollut. Res. 2021, 28, 49302–49313. [Google Scholar] [CrossRef] [PubMed]
- Mckeever, A. Why climate change is still the greatest threat to human health. National Geographic Magazine, 19 August 2021. [Google Scholar]
- Tong, S.; Ebi, K.; Olsen, J. Infectious disease, the climate, and the future. Environ. Epidemiol. 2021, 5, e133. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuschieri, S.; Grech, E.; Cuschieri, A. Climate Change, Obesity, and COVID-19—Global Crises with Catastrophic Consequences. Is This the Future? Atmosphere 2021, 12, 1292. https://doi.org/10.3390/atmos12101292
Cuschieri S, Grech E, Cuschieri A. Climate Change, Obesity, and COVID-19—Global Crises with Catastrophic Consequences. Is This the Future? Atmosphere. 2021; 12(10):1292. https://doi.org/10.3390/atmos12101292
Chicago/Turabian StyleCuschieri, Sarah, Elizabeth Grech, and Andrea Cuschieri. 2021. "Climate Change, Obesity, and COVID-19—Global Crises with Catastrophic Consequences. Is This the Future?" Atmosphere 12, no. 10: 1292. https://doi.org/10.3390/atmos12101292
APA StyleCuschieri, S., Grech, E., & Cuschieri, A. (2021). Climate Change, Obesity, and COVID-19—Global Crises with Catastrophic Consequences. Is This the Future? Atmosphere, 12(10), 1292. https://doi.org/10.3390/atmos12101292






