Association between Chronic Exposure to Ambient Air Pollutants, Demography, Vaccination Level, and the Spread of COVID-19 during 2021 Delta Variant Morbidity Wave
Abstract
:1. Introduction
2. Methods
2.1. Data Collection
2.2. Statistical Analyses
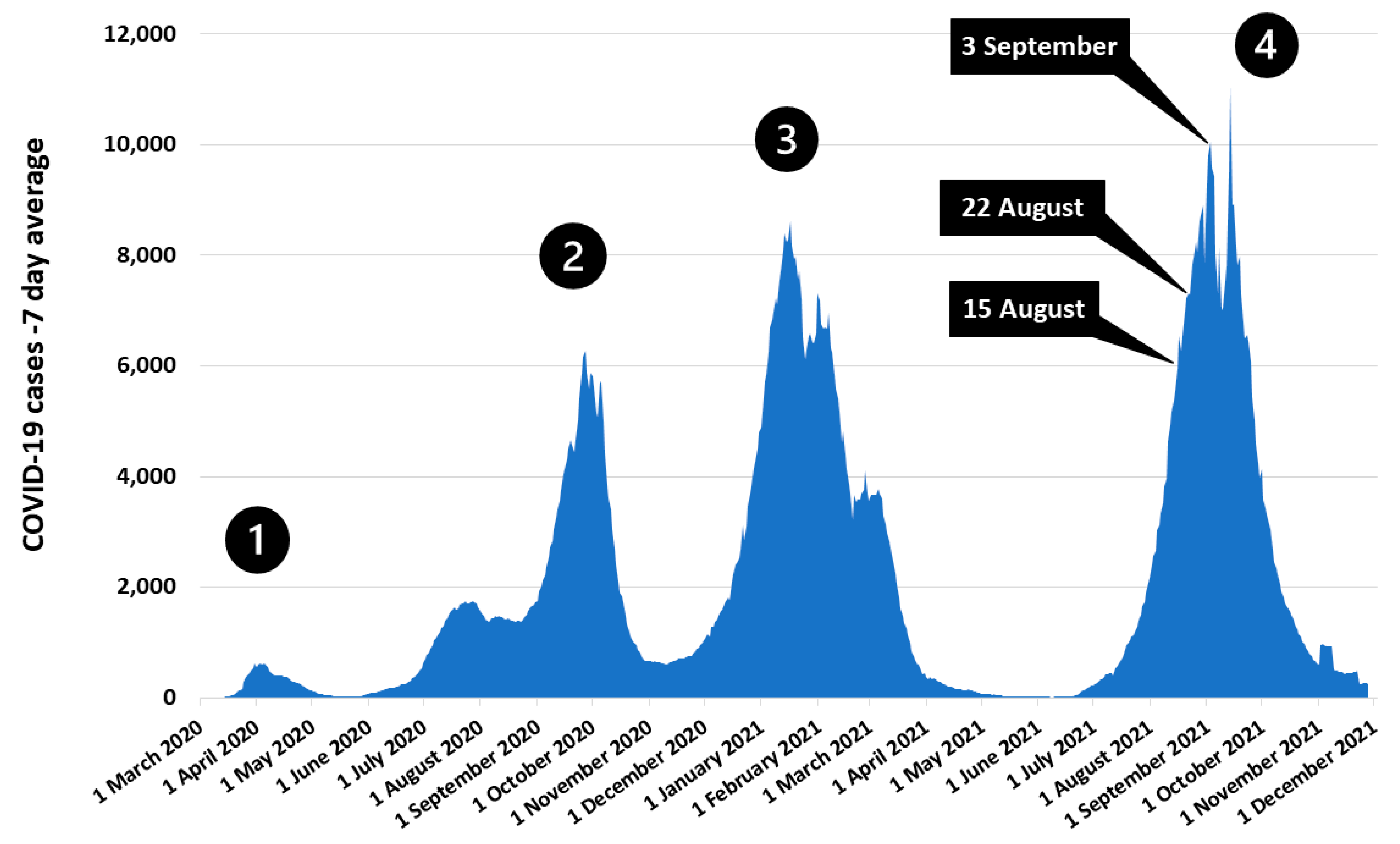
3. Results
3.1. Air Pollutant Concentrations in Israel during 2016–2020
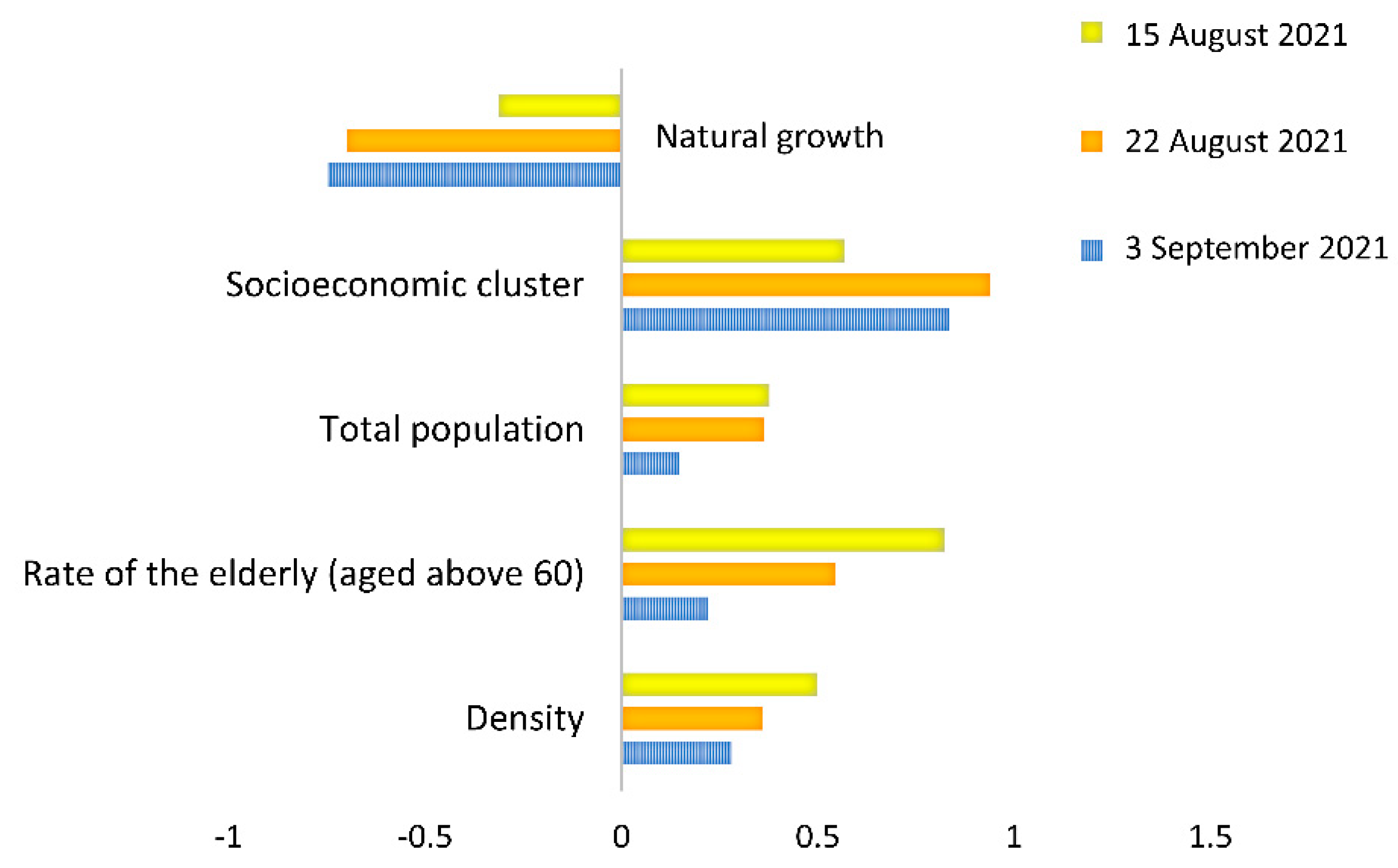
3.2. Associations between Demographic Parameters, Vaccination Level, and Rates of Positive Cases
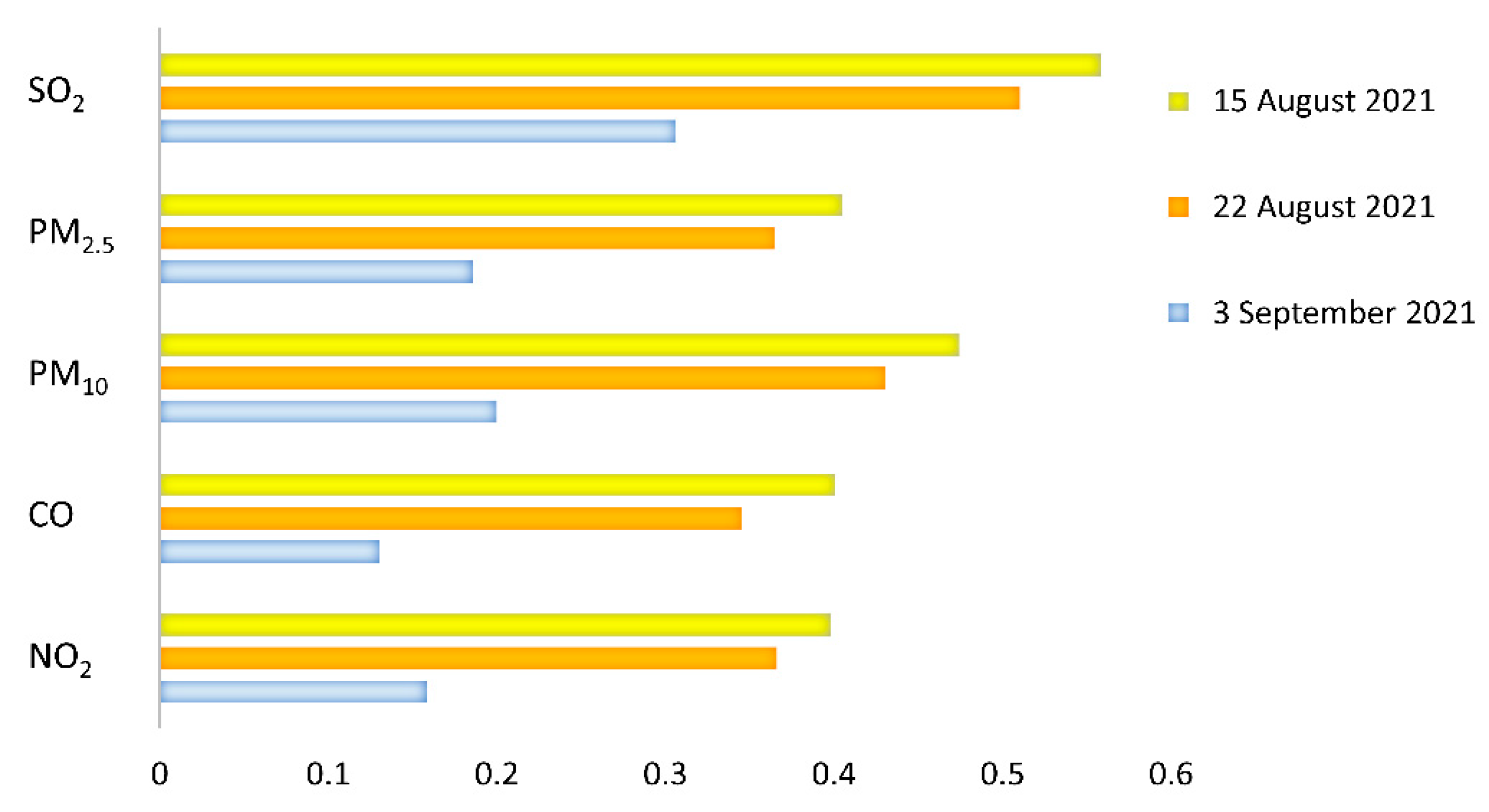
3.3. Associations between Air Pollutant Concentrations and Rates of Positive Cases
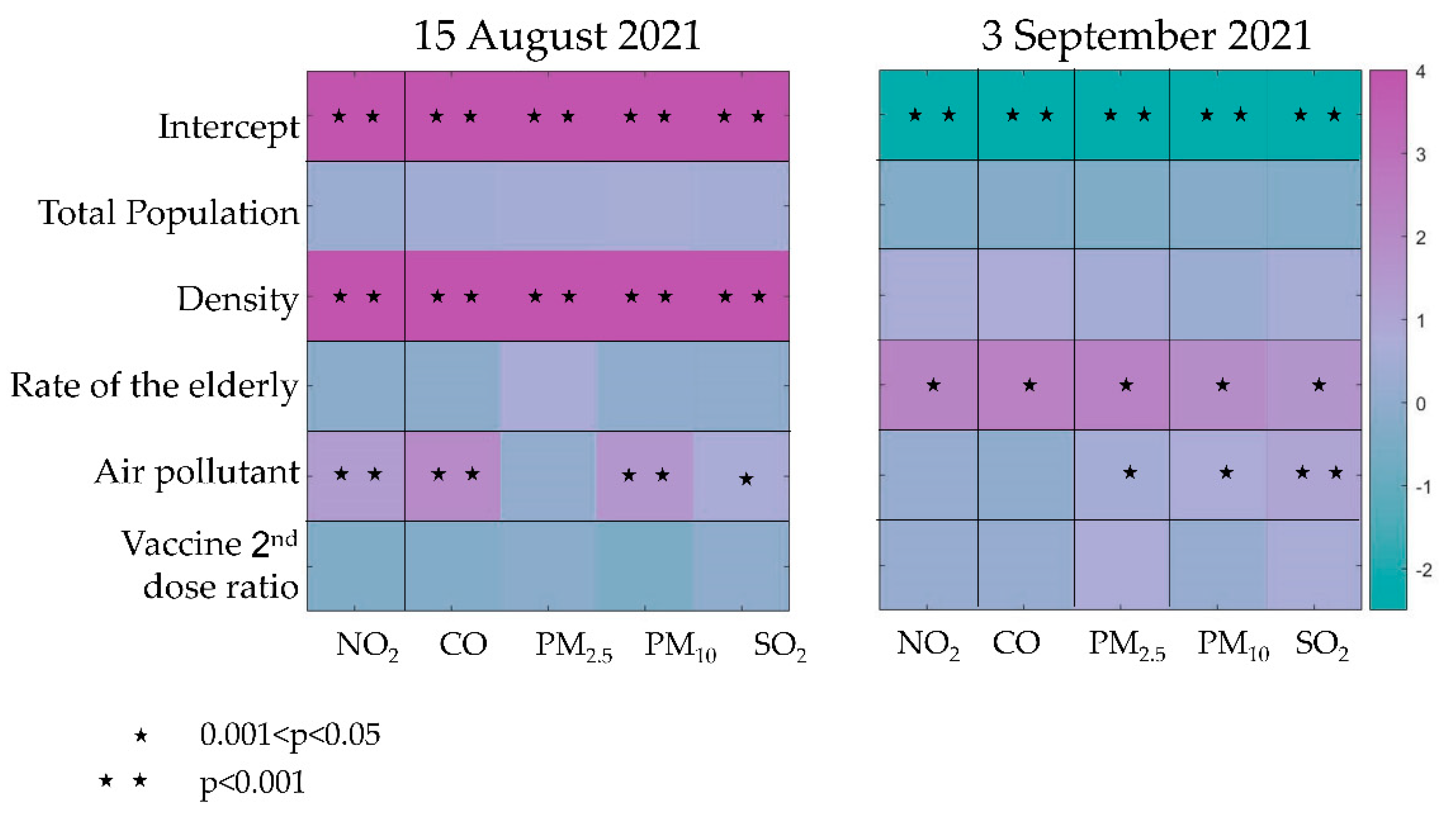
3.4. Multivariate Linear Regressions
4. Discussion
4.1. Air Pollutant Concentrations in Israel during 2016–2020
4.2. Associations between Demographic Parameters, Vaccination Level, and Rates of Positive Cases
4.3. Associations between Air Pollutant Concentrations and Rates of Positive Cases
4.4. Multivariate Linear Regressions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- World Health Organization. Ambient (outdoor) air pollution. 2021. Available online: https://www.who.int/en/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 24 August 2022).
- Loomis, D.; Grosse, Y.; Lauby-Secretan, B.; El Ghissassi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Guha, N.; Bann, R.; Straif, K. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013, 14, 1262. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Air Quality Guidelines. Particulate Matter (PM2.5 And PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; World Health Organization: Geneva, Switzerland, 2021; Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- Barnett-Itzhaki, Z.; Levi, A. Effects of chronic exposure to ambient air pollutants on COVID-19 morbidity and mortality-A lesson from OECD countries. Environ. Res. 2021, 195, 110723. [Google Scholar] [CrossRef] [PubMed]
- Fernández, D.; Giné-Vázquez, I.; Liu, I.; Yucel, R.; Ruscone, M.N.; Morena, M.; García, V.G.; Haro, J.M.; Tyrovolas, S. Are environmental pollution and biodiversity levels associated to the spread and mortality of COVID-19? A four-month global analysis. Environ. Pollut. 2021, 271, 116326. [Google Scholar] [CrossRef] [PubMed]
- Solimini, A.; Filipponi, F.; Fegatelli, D.A.; Caputo, B.; De Marco, C.M.; Spagnoli, A.; Vestri, A.R. A global association between Covid-19 cases and airborne particulate matter at regional level. Sci. Rep. 2021, 11, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Cole, M.; Ozgen, C.; Strobl, E. Air pollution exposure and COVID-19. Institute for the Study of Labor, Discussion Paper No. 13367. 2020. Available online: https://ssrn.com/abstract=3628242 (accessed on 24 August 2022).
- Conticini, E.; Frediani, B.; Caro, D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020, 261, 114465. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, E.; Renzetti, S.; Volta, M.; Donato, F.; Calza, S.; Placidi, D.; Lucchini, R.J.; Rota, M. COVID-19 incidence and mortality in Lombardy, Italy: An ecological study on the role of air pollution, meteorological factors, demographic, and socioeconomic variables. Environ. Res. 2021, 195, 110777. [Google Scholar] [CrossRef]
- Levi, A.; Barnett-Itzhaki, Z. Effects of chronic exposure to ambient air pollutants, demographic, and socioeconomic factors on COVID-19 morbidity: The Israeli case study. Environ. Res. 2021, 202, 111673. [Google Scholar] [CrossRef]
- Sasidharan, M.; Singh, A.; Torbaghan, M.E.; Parlikad, A.K. A vulnerability-based approach to human-mobility reduction for countering COVID-19 transmission in London while considering local air quality. Sci. Total Environ. 2020, 741, 140515. [Google Scholar] [CrossRef]
- Setti, L.; Passarini, F.; De Gennaro, G.; Barbieri, P.; Licen, S.; Perrone, M.G.; Piazzalunga, A.; Borelli, M.; Palmisani, J.; Di Gilio, A.; et al. Potential role of particulate matter in the spreading of COVID-19 in Northern Italy: First observational study based on initial epidemic diffusion. BMJ Open 2020, 10, e039338. [Google Scholar] [CrossRef]
- Tian, H.; Liu, Y.; Song, H.; Wu, C.H.; Li, B.; Kraemer, M.U.; Zheng, P.; Yan, X.; Jia, G.; Zheng, Y.; et al. Risk of COVID-19 is associated with long-term exposure to air pollution. medRxiv 2020. medRxiv:04.21.20073700. [Google Scholar]
- Wu, X.; Nethery, R.C.; Sabath, B.M.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. medRxiv 2020, medRxiv:04.05.20054502. arXiv:04.05.20054502. [Google Scholar]
- Zoran, M.A.; Savastru, R.S.; Savastru, D.M.; Tautan, M.N. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci. Total Environ. 2020, 738, 139825. [Google Scholar] [CrossRef] [PubMed]
- Marquès, M.; Domingo, J.L. Positive association between outdoor air pollution and the incidence and severity of COVID-19. A review of the recent scientific evidence. Environ. Res. 2022, 203, 111930. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, A.; Scher, E.; Rambaut, A. SARS-CoV-2 lineages. 2022. Available online: https://cov-lineages.org/lineage_list.html (accessed on 13 September 2022).
- Goldberg, Y.; Mandel, M.; Bar-On, Y.M.; Bodenheimer, O.; Freedman, L.; Haas, E.J.; Milo, R.; Alroy-Preis, S.; Ash, N.; Huppert, A. Waning immunity after the BNT162b2 vaccine in Israel. N. Engl. J. Med. 2021, 385, e85. [Google Scholar] [CrossRef]
- Sah, P.; Vilches, T.N.; Moghadas, S.M.; Fitzpatrick, M.C.; Singer, B.H.; Hotez, P.J.; Galvani, A.P. Accelerated vaccine rollout is imperative to mitigate highly transmissible COVID-19 variants. EClinicalMedicine 2021, 35, 100865. [Google Scholar] [CrossRef]
- CDC. SARS-CoV-2 Variant Classifications and Definitions. Updated 26 April 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html (accessed on 24 July 2022).
- Zhang, M.; Liang, Y.; Yu, D.; Du, B.; Cheng, W.; Li, L.; Yu, Z.; Luo, S.; Zhang, Y.; Wang, H.; et al. A systematic review of vaccine breakthrough infections by SARS-CoV-2 Delta variant. Int. J. Biol. Sci. 2022, 18, 889. [Google Scholar] [CrossRef]
- Cahyadi, M.N.; Handayani, H.H.; Warmadewanthi, I.D.A.A.; Rokhmana, C.A.; Sulistiawan, S.S.; Waloedjo, C.S.; Raharjo, A.B.; Endroyono; Atok, M.; Navisa, S.C.; et al. Spatiotemporal Analysis for COVID-19 Delta Variant Using GIS-Based Air Parameter and Spatial Modeling. Int. J. Environ. Res. Public Health 2022, 19, 1614. [Google Scholar] [CrossRef]
- Li, Z.; Tao, B.; Hu, Z.; Yi, Y.; Wang, J. Effects of short-term ambient particulate matter exposure on the risk of severe COVID-19. J. Infect. 2022, 84, 684–691. [Google Scholar] [CrossRef]
- Chen, Z.; Sidell, M.A.; Huang, B.Z.; Chow, T.; Martinez, M.P.; Lurmann, F.; Gilliland, F.D.; Xiang, A.H. The Independent Effect of COVID-19 Vaccinations and Air Pollution Exposure on Risk of COVID-19 Hospitalizations in Southern California. Am. J. Respir. Crit. Care Med. 2022. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Ortiz-Ospina, E.; et al. Coronavirus Pandemic (COVID-19). Published online at OurWorldInData.org. 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 20 April 2022).
- CBS-Israel Central Bureau of Statistics. Municipalities in Israel—data files for processing 1999–2019. 2019; Updated 8 March 2022. Available online: https://www.cbs.gov.il/he/publications/doclib/2019/hamakomiot1999_2017/2019.xlsx (accessed on 20 April 2022).
- DataGov. Israel’s Government COVID-19 dataset website. 2022. Available online: https://data.gov.il/dataset/covid-19/resource/8a21d39d-91e3-40db-aca1-f73f7ab1df69 (accessed on 20 April 2022).
- Monteiro, A.; Miranda, A.; Borrego, C.; Vautard, R.; Ferreira, J.; Perez, A. Long-term assessment of particulate matter using CHIMERE model. Atmos. Environ. 2007, 41, 7726–7738. [Google Scholar] [CrossRef]
- Yuval; Levy, I.; Broday, D.M. Improving modeled air pollution concentration maps by residual interpolation. Sci. Total Environ. 2017, 598, 780–788. [Google Scholar] [CrossRef] [PubMed]
- Levy, I.; Karakis, I.; Berman, T.; Amitay, M.; Barnett-Itzhaki, Z. A hybrid model for evaluating exposure of the general population in Israel to air pollutants. Environ. Monit. Assess. 2020, 192, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bdal, D.; Glas, E.; Bachar, N. Israel’s Energy Sector 2019 Report. Israeli Ministry of Energy. 2022; (in Hebrew). Available online: https://www.gov.il/he/departments/publications/reports/energy_sector_2019 (accessed on 26 October 2022).
- Noga–The Israel Independent System Operator Ltd. Summary of Electricity Production and Consumption for 2020. 2020. Available online: https://www.noga-iso.co.il/media/pywdnn5o/%D7%A1%D7%99%D7%9B%D7%95%D7%9D-%D7%A9%D7%A0%D7%AA-2020.pdf (accessed on 5 April 2022).
- Yu, X.; Wong, M.S.; Kwan, M.P.; Nichol, J.E.; Zhu, R.; Heo, J.; Chan, P.W.; Chin, D.C.W.; Kwok, C.Y.T.; Kan, Z. COVID-19 infection and mortality: Association with PM2.5 concentration and population density—An exploratory study. ISPRS Int. J. Geoinf. 2021, 10, 123. [Google Scholar] [CrossRef]
- Páez-Osuna, F.; Valencia-Castañeda, G.; Rebolledo, U.A. The link between COVID-19 mortality and PM2.5 emissions in rural and medium-size municipalities considering population density, dust events, and wind speed. Chemosphere 2022, 286, 131634. [Google Scholar] [CrossRef] [PubMed]
- Mudway, I.S.; Kelly, F.J.; Holgate, S.T. Oxidative stress in air pollution research. Free Radic. Biol. Med. 2020, 151, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Chen, M.; Dong, D.; Xie, S.; Liu, M. Environmental pollutants damage airway epithelial cell cilia: Implications for the prevention of obstructive lung diseases. Thorac. Cancer 2020, 11, 505–510. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barnett-Itzhaki, Z.; Levi, A. Association between Chronic Exposure to Ambient Air Pollutants, Demography, Vaccination Level, and the Spread of COVID-19 during 2021 Delta Variant Morbidity Wave. Atmosphere 2022, 13, 1845. https://doi.org/10.3390/atmos13111845
Barnett-Itzhaki Z, Levi A. Association between Chronic Exposure to Ambient Air Pollutants, Demography, Vaccination Level, and the Spread of COVID-19 during 2021 Delta Variant Morbidity Wave. Atmosphere. 2022; 13(11):1845. https://doi.org/10.3390/atmos13111845
Chicago/Turabian StyleBarnett-Itzhaki, Zohar, and Adi Levi. 2022. "Association between Chronic Exposure to Ambient Air Pollutants, Demography, Vaccination Level, and the Spread of COVID-19 during 2021 Delta Variant Morbidity Wave" Atmosphere 13, no. 11: 1845. https://doi.org/10.3390/atmos13111845
APA StyleBarnett-Itzhaki, Z., & Levi, A. (2022). Association between Chronic Exposure to Ambient Air Pollutants, Demography, Vaccination Level, and the Spread of COVID-19 during 2021 Delta Variant Morbidity Wave. Atmosphere, 13(11), 1845. https://doi.org/10.3390/atmos13111845






