Surgical Interventions for Late Aortic Valve Regurgitation Associated with Continuous Flow-Left Ventricular Assist Device Therapy: Experience Gained and Lessons Learned
Abstract
:1. Introduction
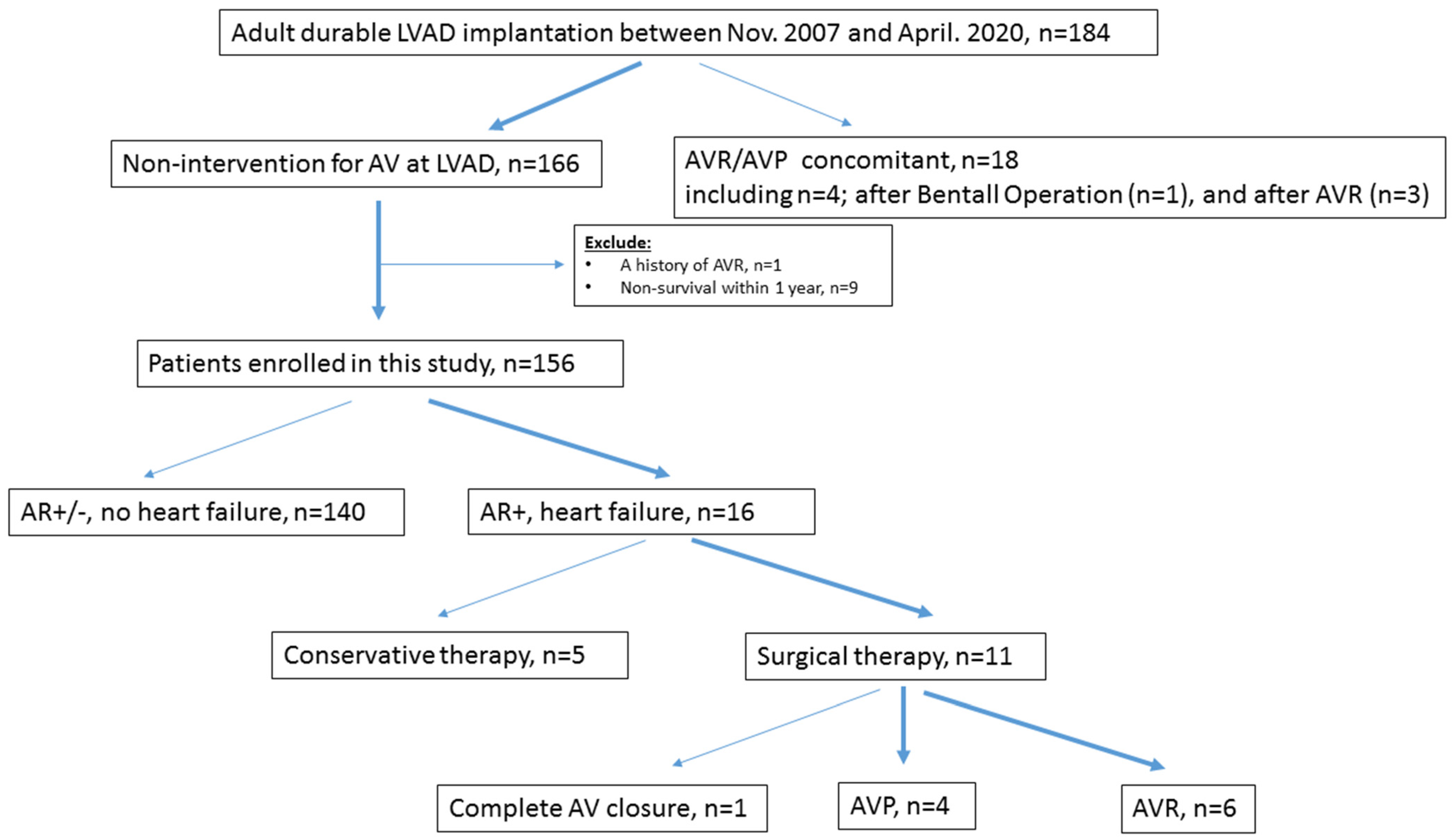
2. Materials and Methods
2.1. Study Design and Follow-Up
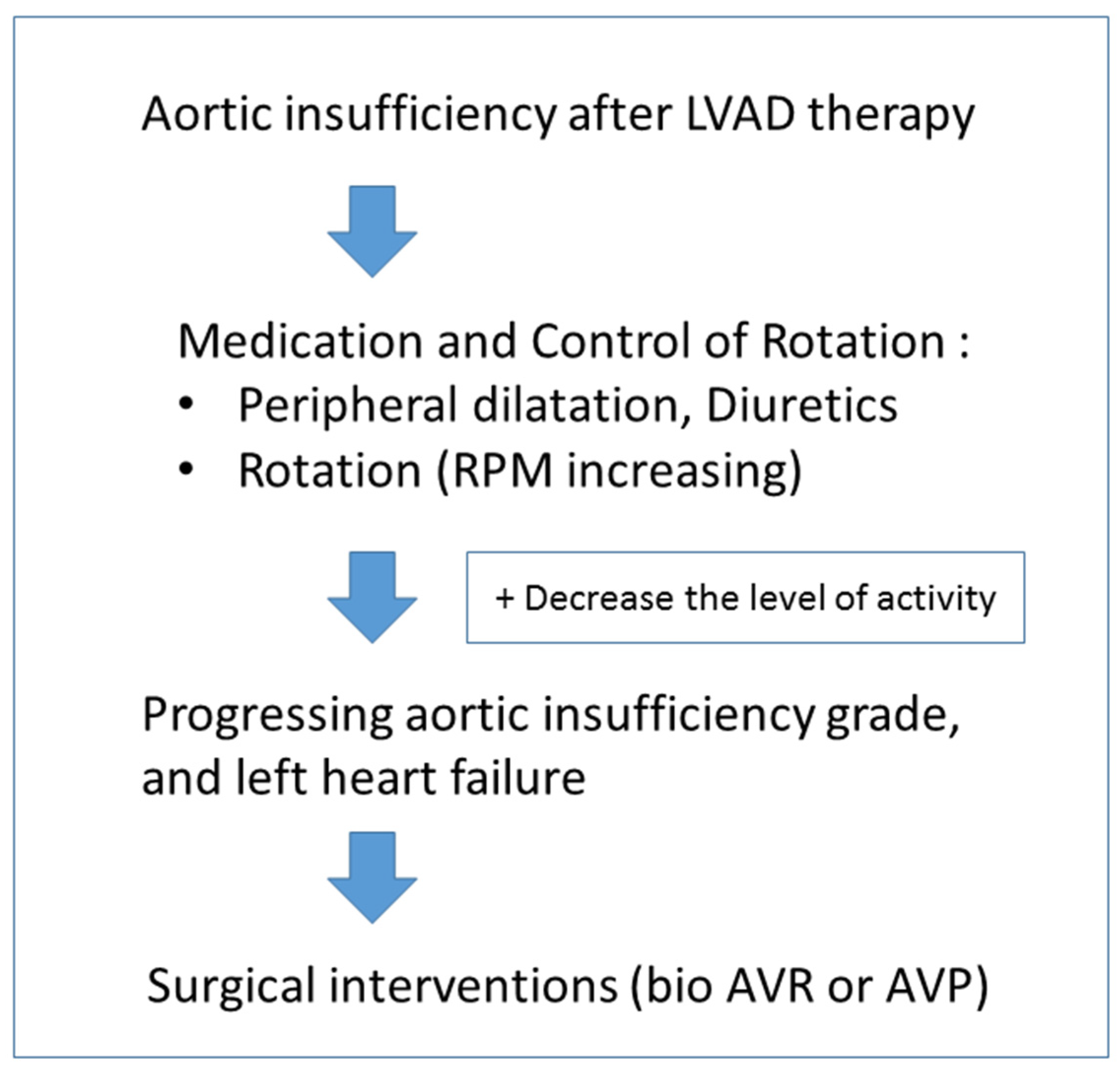
2.2. Treatment Strategies for Aortic Regurgitation (Figure 2)
2.3. Surgical Procedures
2.4. Statistical Analysis
3. Results
3.1. Preoperative Characteristics
3.2. Echocardiographic and Hemodynamic Information
3.3. Intra- and Postoperative Outcomes
3.4. Impact of Aortic Valve Interventions on Long-Term Survival
3.5. Intraoperative Pathological Findings Associated with Aortic Regurgitation
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schramm, R.; Morshuis, M.; Schoenbrodt, M.; Boergermann, J.; Hakim-Meibodi, K.; Hata, M.; Gummert, J.F. Current perspectives on mechanical circulatory support. Eur. J. Cardiothorac. Surg. 2019, 55, i31–i37. [Google Scholar] [CrossRef] [PubMed]
- Schramm, R.; Zittermann, A.; Morshuis, M.; Schoenbrodt, M.; von Roessing, E.; von Dossow, V.; Koster, A.; Fox, H.; Hakim-Meibodi, K.; Gummert, J.F. Comparing short-term outcome after implantation of the HeartWare® HVAD® and the Abbott® HeartMate 3®. ESC Heart Fail. 2020, 7, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Jorde, U.P.; Uriel, N.; Nahumi, N.; Bejar, D.; Gonzalez-Costello, J.; Thomas, S.S.; Han, J.; Morrison, K.A.; Jones, S.; Kodali, S.; et al. Prevalence, significance, and management of aortic insufficiency in continuous flow left ventricular assist device recipients. Circ. Heart Fail. 2014, 7, 310–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouabdallaoui, N.; El-Hamamsy, I.; Pham, M.; Giraldeau, G.; Parent, M.C.; Carrier, M.; Rouleau, J.L.; Ducharme, A. Aortic regurgitation in patients with a left ventricular assist device: A contemporary review. J. Heart Lung Transplant. 2018, 37, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Holtz, J.; Teuteberg, J. Management of aortic insufficiency in the continuous flow left ventricular assist device population. Curr. Heart Fail. Rep. 2014, 11, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, M.L.; Bobba, C.M.; Mokadam, N.A.; Whitson, B.A.; Essandoh, M.; Hasan, A.; Ganapathi, A.M. Continuous-flow left ventricular assist devices and the aortic valve: Interactions, issues, and surgical therapy. Curr. Heart Fail. Rep. 2020, 17, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Yamaguchi, O.; Ohtani, T.; Kinugawa, K.; Saiki, Y.; Sawa, Y.; Shiose, A.; Tsutsui, H.; Fukushima, N.; Matsumiya, G.; et al. JCS/JSCVS/JATS/JSVS 2021 Guideline on implantable left ventricular assist device for patients with advanced heart failure. Circ. J. 2022, 86, 1024–1058. [Google Scholar] [CrossRef] [PubMed]
- Gyoten, T.; Morshuis, M.; Fox, H.; Deutsch, M.A.; Hakim-Meibodi, K.; Schramm, R.; Gummert, J.F.; Rojas, S.V. Secondary aortic valve replacement in continuous flow left ventricular assist device therapy. Artif. Organs 2021, 45, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Liao, K.K.; Segurola, R.; Madhu, K.P.; Miller, L.W. Management of aortic insufficiency in patients with left ventricular assist devices: A simple coaptation stitch method (Park’s stitch). J. Thorac. Cardiovasc. Surg. 2004, 127, 264–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rojas, S.V.; Hanke, J.S.; Haverich, A.; Schmitto, J.D. Chronic ventricular assist device support: Surgical innovation. Curr. Opin. Cardiol. 2016, 31, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Gyoten, T.; Rojas, S.V.; Fox, H.; Deutsch, M.A.; Ruiz-Cano, M.; Hakim-Meibodi, K.; Gummert, J.F.; Morshuis, M.; Schramm, R. The HeartWare ventricular assist device (HVAD): A single institutional 10-year experience. Thorac. Cardiovasc. Surg. 2022, 70, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Potapov, E.V.; Antonides, C.; Crespo-Leiro, M.G.; Combes, A.; Färber, G.; Hannan, M.M.; Kukucka, M.; de Jonge, N.; Loforte, A.; Lund, L.H.; et al. 2019 EACTS Expert Consensus on long-term mechanical circulatory support. Eur. J. Cardiothorac. Surg. 2019, 56, 230–270. [Google Scholar] [CrossRef]
- Immohr, M.B.; Boeken, U.; Mueller, F.; Prashovikj, E.; Morshuis, M.; Böttger, C.; Aubin, H.; Gummert, J.; Akhyari, P.; Lichtenberg, A.; et al. Complications of left ventricular assist devices causing high urgency status on waiting list: Impact on outcome after heart transplantation. ESC Heart Fail. 2021, 8, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Yehya, A.; Rajagopal, V.; Meduri, C.; Kauten, J.; Brown, M.; Dean, L.; Webster, J.; Krishnamoorthy, A.; Hrobowski, T.; Dean, D. Short-term results with transcatheter aortic valve replacement for treatment of left ventricular assist device patients with symptomatic aortic insufficiency. J. Heart Lung Transplant. 2019, 38, 920–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kar, B.; Prathipati, P.; Jumean, M.; Nathan, S.S.; Gregoric, I.D. Management of aortic insufficiency using transcatheter aortic valve replacement in patients with left ventricular assist device support. ASAIO J. 2020, 66, e82–e86. [Google Scholar] [CrossRef] [PubMed]
- Fried, J.A.; Nazif, T.M.; Colombo, P.C. A new frontier for TAVR: Aortic insufficiency in CF-LVAD patients. J. Heart Lung Transplant. 2019, 38, 927–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKellar, S.H.; Deo, S.; Daly, R.C.; Durham, L.A., 3rd; Joyce, L.D.; Stulak, J.M.; Park, S.J. Durability of central aortic valve closure in patients with continuous flow left ventricular assist devices. J. Thorac. Cardiovasc. Surg. 2014, 147, 344–348. [Google Scholar] [CrossRef] [PubMed]



| Total n = 10 | AVP n = 4 | AVR n = 6 | p-Value | |
|---|---|---|---|---|
| Age at LVAD implantation, years | 32 (22–38) | 23 (21–26) | 37 (32–40) | 0.13 |
| Age at aortic valve intervention, years | 34 (25–41) | 26 (25–28) | 40 (34–44) | 0.11 |
| Male | 6 | 2 | 4 | 1 |
| Body mass index, kg/m2 | 19 (18–20) | 18 (17–19) | 20 (19–20) | 0.35 |
| Body surface area, m2 | 1.6 (1.5–1.8) | 1.5 (1.4–1.6) | 1.6 (1.5–1.8) | 0.35 |
| Pathology | 0.77 | |||
| Dilated cardiomyopathy | 5 | 1 | 4 | |
| Dilated phase of hypertrophic cardiomyopathy | 3 | 2 | 1 | |
| Arrhythmogenic right ventricular cardiomyopathy | 1 | 1 | 0 | |
| Transposition of the great arteries | 1 | 0 | 1 | |
| INTERMACS level at cf-LVAD implantation | 3 (3–3) | 3 (2–3) | 3 (3–3) | 0.087 |
| A history of mechanical circuratory support | ||||
| Impella | 0 | 0 | 0 | 1 |
| IABP | 1 | 1 | 0 | 0.33 |
| PCPS | 0 | 0 | 0 | 1 |
| Nipro para-corporeal pulsatile LVAD | 3 | 0 | 3 | 0.2 |
| Implanted LVAD device types | 1 | |||
| DuraHeart | 1 | 1 | 0 | |
| EVAHEART | 1 | 0 | 1 | |
| HeartMate II | 5 | 2 | 3 | |
| HeartMate 3 | 0 | 0 | 0 | |
| HVAD | 0 | 0 | 0 | |
| Jarvik 2000 | 3 | 1 | 2 | |
| Concomitant TV surgery at LVAD implantation | 3 | 1 | 2 | 1 |
| VAD duration to aortic valve intervention, month | 34 (24–44) | 37 (27–44) | 34 (25–42) | 1 |
| Laboratory | ||||
| Brain natriuretic hormone, pg/mL | 579 (369–1039) | 554 (399–799) | 579 (397–1230) | 0.76 |
| Echocardiography | ||||
| Aortic regurgitation, grade | 3 (2–4) | 4 (3–4) | 2 (2–3) | 0.071 |
| Aortic valve-opening | 2 | 0 | 2 | 0.47 |
| Mitral regurgitation, grade | 2 (1–2) | 1 (1–2) | 2 (2–2) | 0.3 |
| Tricuspid regurgitation, grade | 2 (2–4) | 4 (3–4) | 2 (2–2) | 0.1 |
| Tricuspid annular plane systolic excursion, mm | 8 (7–10) | 7 (7–8) | 10 (8–12) | 0.12 |
| Annulus, mm | 21 (18–22) | 20 (18–21) | 22 (19–24) | 0.33 |
| Valsalva, mm | 27 (25–30) | 26 (25–27) | 30 (25–31) | 0.45 |
| Sinotubular junction, mm | 23 (19–25) | 21 (19–22) | 24 (21–26) | 0.28 |
| Ascending aorta, mm | 27 (25–29) | 26 (25–28) | 27 (26–29) | 0.45 |
| Right heart catheter after increased RPM | ||||
| Mean right atrial pressure, mmHg | 12 (9–18) | 11 (10–15) | 14 (10–19) | 0.7 |
| Right ventricular end-diastolic pressure, mmHg | 13 (9–16) | 12 (10–13) | 15 (9–18) | 0.57 |
| Mean pulmonary artery pressure, mmHg | 18 (16–23) | 16 (14–18) | 21 (18–31) | 0.19 |
| Mean pulmonary capillary wedge pressure, mmHg | 12 (12–18) | 8 (8–10) | 17 (13–23) | 0.049 |
| Cardiac output, L/min | 3.2 (2.7–3.4) | 3.2 (3.2–3.4) | 2.9 (2.5–3.4) | 0.55 |
| Cardiac index, L/min/m2 | 1.8 (1.6–2.3) | 2.3 (2.0–2.4) | 1.6 (1.6–1.9) | 0.26 |
| Total n = 10 | AVP n = 4 | AVR n = 6 | p-Value | |
|---|---|---|---|---|
| Cardiopulmonary bypass time, min | 172 (152–191) | 172 (160–179) | 173 (152–205) | 0.91 |
| Ascending aorta clamp time, min | 81 (66–94) | 61 (58–70) | 88 (80–117) | 0.067 |
| Concomitant procedures | ||||
| TAP | 1 | 0 | 1 | |
| TVR | 2 | 2 | 0 | |
| Main reason of AR | ||||
| Prolapse | 2 | 1 | 1 | |
| Degenerative change | 5 | 1 | 4 | |
| Dilatation of annulus | 1 | 0 | 1 | |
| Unknown | 2 | 2 | 0 | |
| Outcomes | ||||
| Recurrent severe AR | 1 | 1 | 0 | |
| AR grade at 1 month after surgery | 0.5 (0–1) | 1 (1–1) | 0 (0–0) | 0.018 |
| AV-opening during follow up period | No | No | No | |
| Death | 1 | 0 | 1, liver failure | |
| Explant | 0 | 0 | 0 | |
| On-going LVAD support | 3 | 0 | 3 | |
| Heart transplantation | 6 | 4 | 2 | |
| Waiting time for HTx after AV surgery, month | 7 (4–13) | 6 (4–8) | 4 and 43 | |
| On the waiting list, month | - | - | 9, 13, and 15 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gyoten, T.; Amiya, E.; Ono, M. Surgical Interventions for Late Aortic Valve Regurgitation Associated with Continuous Flow-Left Ventricular Assist Device Therapy: Experience Gained and Lessons Learned. Life 2023, 13, 94. https://doi.org/10.3390/life13010094
Gyoten T, Amiya E, Ono M. Surgical Interventions for Late Aortic Valve Regurgitation Associated with Continuous Flow-Left Ventricular Assist Device Therapy: Experience Gained and Lessons Learned. Life. 2023; 13(1):94. https://doi.org/10.3390/life13010094
Chicago/Turabian StyleGyoten, Takayuki, Eisuke Amiya, and Minoru Ono. 2023. "Surgical Interventions for Late Aortic Valve Regurgitation Associated with Continuous Flow-Left Ventricular Assist Device Therapy: Experience Gained and Lessons Learned" Life 13, no. 1: 94. https://doi.org/10.3390/life13010094
APA StyleGyoten, T., Amiya, E., & Ono, M. (2023). Surgical Interventions for Late Aortic Valve Regurgitation Associated with Continuous Flow-Left Ventricular Assist Device Therapy: Experience Gained and Lessons Learned. Life, 13(1), 94. https://doi.org/10.3390/life13010094







