Cerebral Perfusion Pressure-Guided Therapy in Patients with Subarachnoid Haemorrhage—A Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient and Inclusion Criteria
2.2. Exclusion Criteria
2.3. Measurements
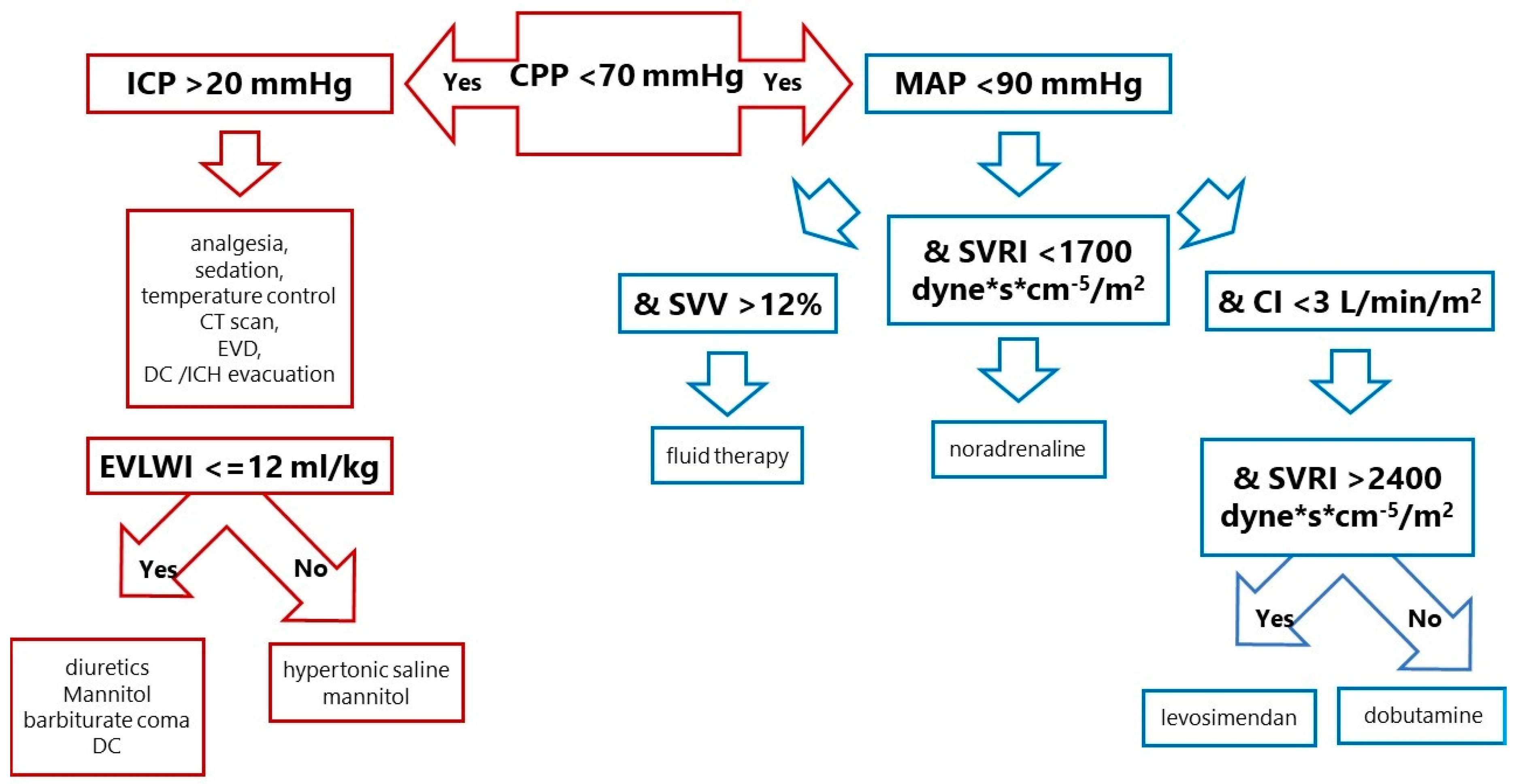
2.4. Study Flow and Treatment Protocol
2.5. Outcomes
2.6. Statistics
3. Results
- −
- ICP monitoring without haemodynamic monitoring (7 patients);
- −
- TPTD monitoring without ICP measurements (3 patients).
3.1. Haemodynamic Therapy
3.2. Neurosurgical Treatment
3.3. Mortality Rate, DCI and Functional Outcomes
4. Discussion
4.1. Epidemiology, Prognostic Scales, Mortality and Functional Outcome
4.2. Intracranial Hypertension
4.3. Haemodynamic Profile
4.4. Haemodynamic Support
4.5. Limitations of the Study
4.6. Novelty the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rinkel, G.J.; Algra, A. Long term outcomes of patients with aneurysmal subarachnoid hemorrhage. Lancet Neurol. 2011, 10, 349–356. [Google Scholar] [CrossRef]
- Priebe, H.J. Aneurysmal subarachnoid haemorrhage and the anaesthetist. Br. J. Anaesth. 2007, 99, 102–118. [Google Scholar] [CrossRef]
- Davison, D. Neurogenic pulmonary edema. Crit. Care 2012, 16, 212–220. [Google Scholar] [CrossRef]
- Kerro, A. Neurogenic stunned myocardium in subarachnoid hemorrhage. J. Crit. Care 2017, 38, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Cossu, G.; Messerer, M.; Stocchetti, N.; Levivier, M.; Daniel, R.T.; Oddo, M. Intracranial pressure and outcome in critically ill patients with aneurysmal subarachnoid hemorrhage: A systematic review. Minerv. Anest. 2016, 82, 684–694. [Google Scholar]
- Florez, W.A.; García-Ballestas, E.; Deora, H.; Agrawal, A.; Martinez-Perez, R.; Galwankar, S.; Keni, R.; Menon, G.R.; Joaquim, A.; Moscote-Salazar, L.R. Intracranial hypertension in patients with aneurysmal subarachnoid hemorrhage: A systematic review and metaanalysis. Neurosurg. Rev. 2021, 44, 203–211. [Google Scholar] [CrossRef]
- Carney, N.; Totten, A.M.; O’Reilly, C.; Ullman, J.S.; Hawryluk, G.W.; Bell, M.J.; Bratton, S.L.; Chesnut, R.; Harris, O.A.; Kissoon, N.; et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery 2017, 80, 6–15. [Google Scholar] [CrossRef]
- Monnet, X.; Teboul, J.L. Transpulmonary thermodilution: Advantages and limits. Crit. Care 2017, 21, 147–159. [Google Scholar] [CrossRef]
- Steiner, T.; Juveal, S.; Unterberg, A.; Jung, C.; Forsting, M.; Rinkel, G. European Stroke Organization guidelines for the management of intracranial aneurysms and subarachnoid hemorrhage. Cerebrovasc. Dis. 2013, 35, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Connolly, E.S.; Rabinstein, A.A.; Carhuapoma, J.R.; Derdeyn, C.P.; Dion, J.; Higashida, R.T.; Hoh, B.L.; Kirkness, C.J.; Naidech, A.M.; Ogilvy, C.S.; et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from American Heart Association/American Stroke Association. Stroke 2012, 43, 1711–1721. [Google Scholar] [CrossRef] [PubMed]
- Diringer, M.N.; Bleck, T.P.; Claude Hemphill, J., III; Menon, D.; Shutter, L.; Vespa, P.; Bruder, N.; Connolly, E.S.; Citerio, G.; Gress, D.; et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: Recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit. Care 2011, 15, 211–240. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Manoel, A.L.; Mansur, A.; Silva, G.S.; Germans, M.R.; Jaja, B.N.; Kouzmina, E.; Marotta, T.R.; Abrahamson, S.; Schweizer, T.A.; Spears, J.; et al. Functional Outcome After Poor-Grade SAH: A single Center Study and Systematic Literature Review. Neurocrit. Care 2016, 25, 338–350. [Google Scholar] [CrossRef]
- Zheng, K.; Zhong, M.; Zhao, B.; Chen, S.Y.; Tan, X.X.; Li, Z.Q.; Xiong, Y.; Duan, C.Z. Poor Grade Aneurysmal Subarachnoid Hemorrhage: Risk Factors Affecting Clinical Outcomes in Intracranial Aneurysm Patients in Multi-Center Study. Front. Neurol. 2019, 10, 123. [Google Scholar] [CrossRef]
- Phillips, T.J.; Dowling, R.J.; Yan, B.; Laidlaw, J.D.; Mitchell, P.J. Does treatment of ruptured intracranial aneurysms within 24 hours improve clinical outcome? Stroke 2011, 42, 1936–1945. [Google Scholar] [CrossRef]
- Sonig, A.; Shallwani, H.; Natarajan, S.K.; Shakir, H.J.; Hopkins, L.N.; Snyder, K.V.; Siddiqui, A.H.; Levy, E.I. Better outcomes and Reduced Hospitalization Costa re Associated with Ultra-Early treatment of Ruptured Anerusms: A US Nationwide Data Sampele Study. Neurosurgery 2018, 1, 497–505. [Google Scholar] [CrossRef]
- Heuer, G.G.; Smith, M.J.; Elliott, J.P.; Winn, H.R.; LeRoux, P.D. Relationship between intracranial pressure and other clinical variables in patients with aneurysmal subarachnoid hemorrhage. J. Neurosurg. 2004, 101, 408–416. [Google Scholar] [CrossRef]
- Mutoh, T.; Kazumata, K.; Ishikawa, T.; Terasaka, S. Performance of Bedside Transpulmonary Thermodilution Monitoring for Goal-Directed Hemodynamic Management After Subarachnoid Hemorrhage. Stroke 2009, 40, 2368–2374. [Google Scholar] [CrossRef] [PubMed]
- Vergouwen, M.D.; Vermeulen, M.; van Gijn, J.; Rinkel, G.J.; Wijdicks, E.F.; Muizelaar, J.P.; Mendelow, A.D.; Juvela, S.; Yonas, H.; Terbrugge, K.G.; et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: Proposal of multidisciplinary research group. Stroke 2010, 41, 2391–2395. [Google Scholar] [CrossRef] [PubMed]
- Vergouwen, M.D.I. Vasospasm Versus Delayed Cerebral Ischemia as an Outcome Event in Clinical Trials and Observational Studies. Neurocrit. Care 2011, 15, 308–311. [Google Scholar] [CrossRef]
- Guo, J.; Shi, Z.; Yang, K.; Tian, J.H.; Jiang, L. Endothelin receptor antagonists for subarachnoid hemorrhage. Cochrane Database Syst. Rev. 2012, 9, CD008354. [Google Scholar] [CrossRef]
- Liu, G.J.; Wang, Z.J.; Wang, Y.F.; Xu, L.L.; Wang, X.L.; Liu, Y.; Luo, G.J.; He, G.H.; Zeng, Y.J. Systematic assessment and meta-analysis of the efficacy and safety of fasudil in the treatment of cerebral vasospasm in patients with subarachnoid hemorrhage. Eur. J. Clin. Pharmacol. 2012, 68, 131–139. [Google Scholar] [CrossRef]
- Zwienenberg-Lee, M.; Hartman, J.; Rudisill, N.; Madden, L.K.; Smith, K.; Eskridge, J.; Newell, D.; Verweij, B.; Bullock, M.R.; Baker, A.; et al. Effect of prophylactic transluminal balloon angioplasty on cerebral vasospasm and outcome in patients with fisher grade III subarachnoid hemorrhage: Results of a phase II multicenter, randomized, clinical trial. Stroke 2008, 39, 1759–1765. [Google Scholar] [CrossRef] [PubMed]
- Dorhout Mees, S.; Rinkel, G.J.; Feigin, V.L.; Algra, A.; Van den Bergh, W.M.; Vermeulen, M.; Van Gijn, J.; Cochrane Stroke Group. Calcium antagonists for Aneurysmal saubarachnoid hemorrhage. Cochrane Database Syst. Rev. 2007, 3, CD000277. [Google Scholar]
- Loan, J.J.M.; Wiggins, A.N.; Brennan, P.M. Medically induced hypertension, hypervolaemia and haemodilution for the treatment and prophylaxis of vasospasm following aneurysmal subarachnoid haemorrhage: Systemic review. Br. J. Neurosurg. 2018, 2, 157–164. [Google Scholar] [CrossRef]
- Mutoh, T.; Kazamuta, K.; Ajiki, M. Goal-Directed Fluid Management by Bedside Transpulmonary Hemodynamic Monitoring After Subarachnoid Hemorrhage. Stroke 2007, 38, 3218–3224. [Google Scholar] [CrossRef]
- Anetsberger, A.; Gempt, J.; Blobner, M.; Ringel, F.; Bogdanski, R.; Heim, M.; Schneider, G.; Meyer, B.; Schmid, S.; Ryang, Y.M.; et al. Impact of Goal-Directed Therapy on Delayed Ischemia After Aneurysmal Subarachnoid Hemorrhage. Stroke 2020, 51, 2287–2296. [Google Scholar] [CrossRef] [PubMed]
- Kronvall, E.; Undren, P.; Romner, B.; Saveland, H.; Cronqvist, M.; Nilsson, O.G. Nimodipine in aneurysmal subarachnoid hemorrhage: A randomized study of intravenous or oral administration. J. Neurosurg. 2009, 110, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; de Louw, E.; Niemi, M.; Nelson, R.; Mark, R.G.; Celi, L.A.; Mukamal, K.J.; Danziger, J. Association between fluid balance and survival in critically ill patients. J. Intern. Med. 2015, 277, 468. [Google Scholar] [CrossRef]
- Vergouw, L.J.; Egal, M.; Bergmans, B.; Dippel, D.W.; Lingsma, H.F.; Vergouwen, M.D.; Willems, P.W.; Oldenbeuving, A.W.; Bakker, J.; van der Jagt, M. Highly early fluid input after aneurysmal subarachnoid hemorrhage: Combined report of association with delayed cerebral ischemia and feasibility of cardiac output-guided fluid restriction. J. Intensive Care Med. 2020, 35, 161–169. [Google Scholar] [CrossRef]
- Sakr, Y.; Dünisch, P.; Santos, C.; Matthes, L.; Zeidan, M.; Reinhart, K.; Kalff, R.; Ewald, C. Poor outcome is associated with less negative fluid balance in patients with aneurysmal subarachnoid hemorrhage treated with prophylactic vasopressor-induced hypertension. Ann. Intensive Care 2016, 6, 25–32. [Google Scholar] [CrossRef]
| Control Group n = 37 | CPP-Guided Group n = 17 | ||
|---|---|---|---|
| Variable | Median (Q1–Q3) | Median (Q1–Q3) | p Value |
| Age (years) | 63 (57−68) | 54 (48−72) | 0.48 |
| Female—number (percentage) | 23 (62%) | 11 (64%) | 1.00 |
| Body weight (kg) | 75 970−85) | 78 (65−85) | 0.92 |
| Height (cm) | 165 (164−175) | 168 (165−182) | 0.21 |
| BMI (kg/m2) | 26.5 (23.9–28.4) | 24.8 (23.9–28.3) | 0.35 |
| Troponin T (ng/mL) | 39 (24–163) | 61 (8–152) | 0.68 |
| NTproBNP (pg/mL) | 1045 (251–2077) | 314 (165–995) | 0.08 |
| Lactate (mmol/L) | 1.2 (0.8–1.8) | 1.2 (0.9–1.7) | 0.96 |
| Albumin (mg/dL) | 4.1 (3.8–4.5) | 4.3 (3.8–4.5) | 0.5 |
| CRP (mg/L) | 4.4 (1.6–15) | 3.1 (2.4–5) | 0.75 |
| Hgb (g/dL) | 13.1 (11.9–13.8) | 12.4 (12.6–14) | 0.41 |
| Na+ (mEq/L) | 143 (140–146) | 142 (138–146) | 0.69 |
| Mg++ (mg/dL) | 1.9 (1.8–2.1) | 2.1 (1.8–2.1) | 0.46 |
| SOFA (points) | 9 (7–12) | 8 (7–10) | 0.32 |
| APACHE II (points) | 19 (16–25) | 18 (14–21) | 0.24 |
| GCS (points) | 7 (6–9) | 6 (5–8) | 0.52 |
| ICH score (points) | 2 (0–3) | 2 (1–3) | 0.15 |
| Scale | Control Group n = 37 | CPP-Guided Group n = 17 | p Value |
|---|---|---|---|
| Hunt–Hess III–V | 35 (94.6%) | 17 (100%) | 1.0 |
| WFNS IV–V | 34 (91.9%) | 16 (94.1%) | 1.0 |
| Fisher IV | 30 (81.1%) | 16 (94.1%) | 0.4112 |
| Day 1 | Day 2 | Day 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Control Group n = 37 | CPP-Guided Group n = 17 | Control Group n = 37 | CPP-Guided Group n = 17 | Control Group n = 37 | CPP-Guided Group n = 17 | ||||
| Median (Q1–Q3) | Median (Q1–Q3) | p Value | Median (Q1–Q3) | Median (Q1–Q3) | p Value | Median (Q1–Q3) | Median (Q1–Q3) | p Value | |
| MAP (mmHg) | 88 (84–97) | 90 (84–97) | 0.64 | 90 (85–97) | 93 (86–96) | 0.59 | 93 (87–99) | 93 (88–99) | 0.81 |
| HR (beats per minute) | 76 (60—82) | 68 (57–88) | 0.63 | 73 (63–87) | 72 (56–87) | 0.46 | 74 (66–86) | 76 (62–85) | 0.7 |
| CVP (mmHg) | 8 (5–10) | 9 (6–10) | 0.45 | 8 (7–10) | 8 (7–11) | 0.27 | 8 (7–11) | 8 (7–10) | 0.98 |
| Day 1 | Day 2 | Day 3 | |
|---|---|---|---|
| Median (Q1–Q3) | Median (Q1–Q3) | Median (Q1–Q3) | |
| CI (L/min/m2) | 2.9 (2.6–3.2) | 2.8 (2.4–3.3) | 2.8 (2.5–3.6) |
| SVV (%) | 11 (9–16) | 10 (6–14) | 9 (6–14) |
| SVRI (dyne*s*cm−5/m2) | 2145 (1925–2572) | 2212 (1799–2371) | 2350 (1820–2660) |
| GEDVI (mL/m2) | 663 (575–808) | 730 (657–807) | 723 (623–886) |
| ITBVI (mL/m2) | 790 (767–995) | 880 (801–1019) | 890 (768–1120) |
| EVLWI (mL/kg) | 8 (7–9) | 9 (7–10) | 9 (7–10) |
| PVPI | 1.5 (1.4–1.7) | 1.5 (1.4–1.6) | 1.6 (1.4–1.8) |
| ICP (mmHg) | 18 (10–20) | 15 (10–20) | 12 (8–15) |
| CPP (mmHg) | 74 (71–80) | 78 (67–80) | 81 (70–88) |
| Control Group n = 37 | CPP-Guided Group n = 17 | ||
|---|---|---|---|
| Median (Q1–Q3) | Median (Q1–Q3) | p Value | |
| Day 1 | |||
| Crystalloids (mL/24 h) | 1500 (1000–2000) | 1500 (1000–2000) | 0.8469 |
| Fluids (mL/24 h) | 2480 (2110–3210) | 2230 (1920–3130) | 0.2759 |
| Diuresis (mL/24 h) | 2230 (1640–2940) | 2080 (1600–3430) | 0.6957 |
| Fluid balance (mL/24 h) | −160 (−950–350) | −690 (−1370–150) | 0.1267 |
| Furosemide (mg/kg/24 h) | 0.29 (0.02–0.53) | 0.27 (0.13–0.59) | 0.7360 |
| Mannitol (g/kg/24 h) | 0.43 (0–0.6) | 0.46 (0.23–0.58) | 0.7356 |
| Day 2 | |||
| Crystalloids (mL/24 h) | 1000 (500–1000) | 1000 (1000–1000) | 0.6482 |
| Fluids (mL/24 h) | 2780 (2260–3310) | 2650 (2320–3120) | 0.6482 |
| Diuresis (mL/24 h) | 2740 (2020–3290) | 2620 (2150–3650) | 0.8231 |
| Fluid balance (mL/24 h) | −920 (−20––1520) | −870 (−1380––600) | 0.5266 |
| Furosemide (mg/kg/24 h) | 0.37 (0.02–0.69) | 0.56 (0.37–0.69) | 0.5687 |
| Mannitol (g/kg/24 h) | 0.5 (0.17–0.6) | 0.53 (0.01–0.67) | 0.6461 |
| Day 3 | |||
| Crystalloids (mL/24 h) | 500 (500–1000) | 500 (500–1000) | 0.8724 |
| Fluids (mL/24 h) | 2855 (2250–3170) | 3080 (2360–3790) | 0.0993 |
| Diuresis (mL/24 h) | 3020 (2500–3440) | 3000 (2460–3780) | 0.7657 |
| Fluid balance (mL/24 h) | −810 (−1390–400) | −830 (−1400–590) | 0.7943 |
| Furosemide (mg/kg/24 h) | 0.51 (0.27–0.69) | 0.55 (0.38–0.69) | 0.8961 |
| Mannitol (g/kg/24 h) | 0.5 (0–0.6) | 0.47 (0.02–0.58) | 0.9925 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gradys, A.; Szrama, J.; Molnar, Z.; Guzik, P.; Kusza, K. Cerebral Perfusion Pressure-Guided Therapy in Patients with Subarachnoid Haemorrhage—A Retrospective Analysis. Life 2023, 13, 1597. https://doi.org/10.3390/life13071597
Gradys A, Szrama J, Molnar Z, Guzik P, Kusza K. Cerebral Perfusion Pressure-Guided Therapy in Patients with Subarachnoid Haemorrhage—A Retrospective Analysis. Life. 2023; 13(7):1597. https://doi.org/10.3390/life13071597
Chicago/Turabian StyleGradys, Agata, Jakub Szrama, Zsolt Molnar, Przemysław Guzik, and Krzysztof Kusza. 2023. "Cerebral Perfusion Pressure-Guided Therapy in Patients with Subarachnoid Haemorrhage—A Retrospective Analysis" Life 13, no. 7: 1597. https://doi.org/10.3390/life13071597
APA StyleGradys, A., Szrama, J., Molnar, Z., Guzik, P., & Kusza, K. (2023). Cerebral Perfusion Pressure-Guided Therapy in Patients with Subarachnoid Haemorrhage—A Retrospective Analysis. Life, 13(7), 1597. https://doi.org/10.3390/life13071597






