Exploring the Prevalence of Antimicrobial Resistance in Salmonella and commensal Escherichia coli from Non-Traditional Companion Animals: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Epidemiological Data Collection
2.3. Sample Collection
2.4. Salmonella Isolation
2.5. E. coli Isolation
2.6. Antimicrobial Susceptibility Testing
2.7. Statistical Analysis
3. Results
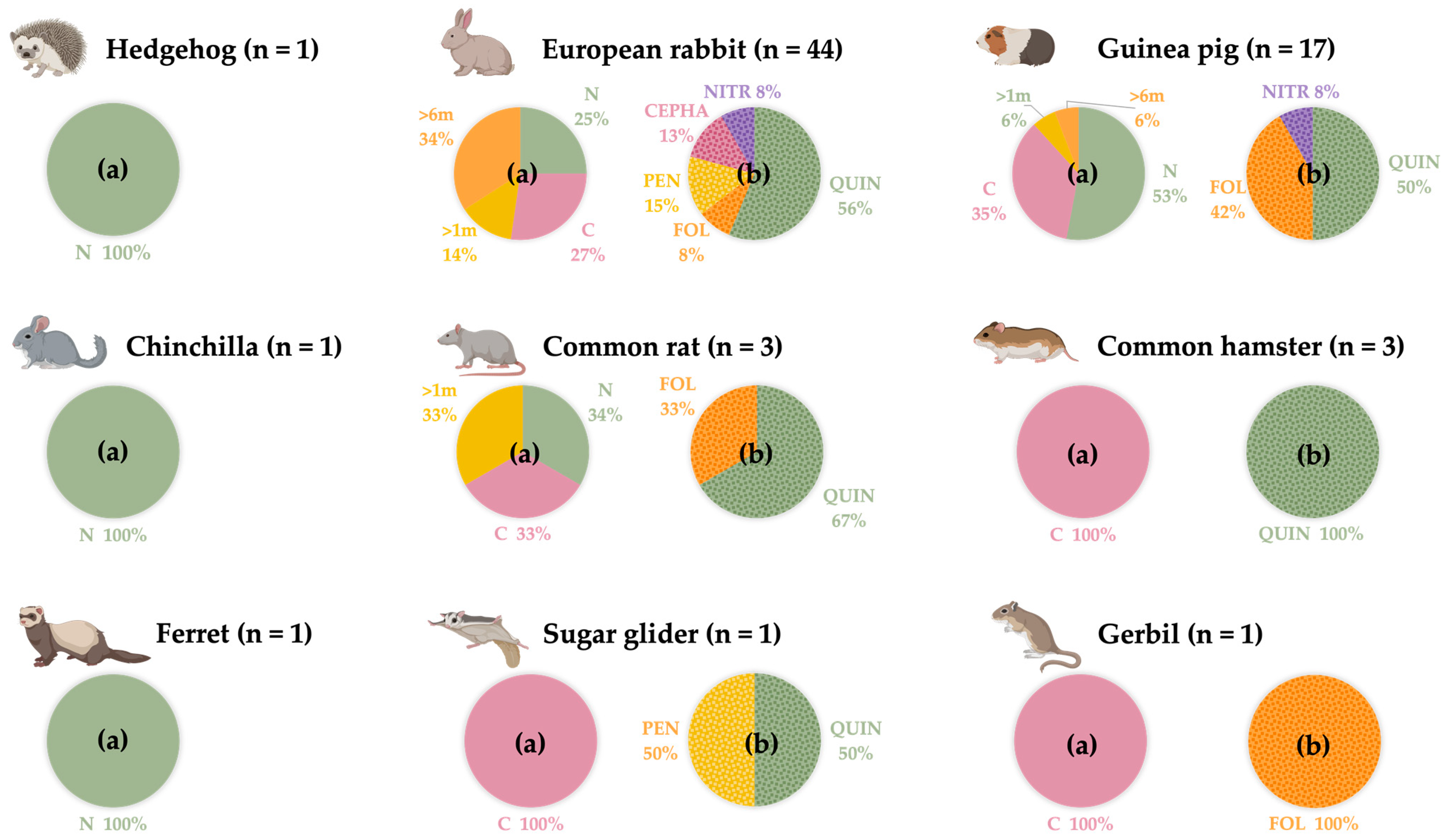
3.1. Epidemiological Results
3.2. Salmonella and E. coli Prevalence
3.3. Antimicrobial Susceptibility from E. coli and Salmonella Strains
4. Discussion
5. Conclusion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Overgaauw, P.A.M.; Vinke, C.M.; van Hagen, M.A.E.; Lipman, L.J.A. A One Health Perspective on the Human-Companion Animal Relationship with Emphasis on Zoonotic Aspects. Int. J. Environ. Res. Public Health 2020, 17, 3789. [Google Scholar] [CrossRef]
- FEDIAF. The European Pet and Food Industry. Annual Report 2023. Available online: https://europeanpetfood.org/about/annual-report/ (accessed on 7 July 2023).
- FEDIAF. The European Pet and Food Industry. Annual Report 2010. Available online: http://www.stray-afp.org/nl/wp-content/uploads/sites/2/2012/08/facts_and_figures_2010.pdf (accessed on 25 September 2023).
- García-San Román, E.; Hernández, A.; Suárez, D.; Veterinary, A.; Espinosa García-San Román, J.; Quesada-Canales, Ó.; Arbelo Hernández, M.; Déniz Suárez, S.; Castro-Alonso, A. Veterinary Education and Training on Non-Traditional Companion Animals, Exotic, Zoo, and Wild Animals: Concepts Review and Challenging Perspective on Zoological Medicine. Vet. Sci. 2023, 10, 357. [Google Scholar] [CrossRef] [PubMed]
- Marin, C.; Lorenzo-Rebenaque, L.; Laso, O.; Villora-Gonzalez, J.; Vega, S. Pet Reptiles: A Potential Source of Transmission of Multidrug-Resistant Salmonella. Front. Vet. Sci. 2021, 7, 1157. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, A.M.; Sandvik, L.M.; Skarstein, M.M.; Svendal, L.; Debenham, J.J. Prevalence of Salmonella Serovars Isolated from Reptiles in Norwegian Zoos. Acta Vet. Scand. 2020, 62, 1–9. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. List of Bacteria for Which New Antibiotics Are Urgently Needed. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 10 December 2023).
- Santana-Hernández, K.M.; Rodríguez-Ponce, E.; Medina, I.R.; Acosta-Hernández, B.; Priestnall, S.L.; Vega, S.; Marin, C.; Cerdà-Cuéllar, M.; Marco-Fuertes, A.; Ayats, T.; et al. One Health Approach: Invasive California Kingsnake (Lampropeltis Californiae) as an Important Source of Antimicrobial Drug-Resistant Salmonella Clones on Gran Canaria Island. Animals 2023, 13, 1790. [Google Scholar] [CrossRef]
- Marco-Fuertes, A.; Marin, C.; Lorenzo-Rebenaque, L.; Vega, S.; Montoro-Dasi, L. Antimicrobial Resistance in Companion Animals: A New Challenge for the One Health Approach in the European Union. Vet. Sci. 2022, 9, 208. [Google Scholar] [CrossRef]
- European Food and Safety Authority. The European Union Summary Report on Antimicrobial Resistance in Zoonotic and Indicator Bacteria from Humans, Animals and Food in 2020/2021. EFSA J. 2023, 21, e07867. [Google Scholar] [CrossRef]
- European Food and Safety Authority. The European Union One Health 2022 Zoonoses Report. EFSA J. 2023, 21, e8442. [Google Scholar] [CrossRef]
- Mader, R.; Demay, C.; Jouvin-Marche, E.; Ploy, M.C.; Barraud, O.; Bernard, S.; Lacotte, Y.; Pulcini, C.; Weinbach, J.; Berling, C.; et al. Defining the Scope of the European Antimicrobial Resistance Surveillance Network in Veterinary Medicine (EARS-Vet): A Bottom-up and One Health Approach. J. Antimicrob. Chemother. 2022, 77, 816–826. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control European Antimicrobial Resistance Surveillance Network (EARS-Net). Available online: https://www.ecdc.europa.eu/en/about-us/networks/disease-networks-and-laboratory-networks/ears-net-data (accessed on 19 July 2023).
- Muñoz-Ibarra, E.; Molina-López, R.A.; Durán, I.; Garcias, B.; Martín, M.; Darwich, L. Antimicrobial Resistance in Bacteria Isolated from Exotic Pets: The Situation in the Iberian Peninsula. Animals 2022, 12, 1912. [Google Scholar] [CrossRef]
- Fernández, M.; Garcias, B.; Duran, I.; Molina-López, R.A.; Darwich, L. Current Situation of Bacterial Infections and Antimicrobial Resistance Profiles in Pet Rabbits in Spain. Vet. Sci. 2023, 10, 352. [Google Scholar] [CrossRef] [PubMed]
- Grimont, P.A.D.; Weill, F.-X. Antigenic Formulae of the Salmonella Serovars, 9th ed.; WHO Collaborating Centre for Reference and Research on Salmonella: Paris, France, 2007. [Google Scholar]
- European Commission. Commission Implementing Decision (EU) 2020/1729 of 17 November 2020 on the Monitoring and Reporting of Antimicrobial Resistance in Zoonotic and Commensal Bacteria; European Commission: Geneva, Switzerland, 2020. [Google Scholar]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 14.0, 2024. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_14.0_Breakpoint_Tables.pdf (accessed on 5 January 2024).
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-Resistant, Extensively Drug-Resistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Searle, S.R.; Speed, F.M.; Milliken, G.A. Population Marginal Means in the Linear Model: An Alternative to Least Squares Means. Am. Stat. 1980, 34, 216–221. [Google Scholar] [CrossRef]
- Fox, J.; Weisberg, S. An R Companion to Applied Regression, 3rd. ed.; Sage: Thousand Oaks, CA, USA, 2019. [Google Scholar]
- Graves, S.; Piepho, H.; Selzer, L.; Dorai-Raj, S. MultcompView: Visualizations of Paired Comparisons. R Package Version 0.1-9. Available online: https://cran.r-project.org/web/packages/multcompView/index.html (accessed on 27 July 2023).
- Kiebler, C.A.; Bottichio, L.; Simmons, L.; Basler, C.; Klos, R.; Gurfield, N.; Roberts, E.; Kimura, A.; Lewis, L.S.; Bird, K.; et al. Outbreak of Human Infections with Uncommon Salmonella Serotypes Linked to Pet Bearded Dragons, 2012–2014. Zoonoses Public Health 2020, 67, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Marin, C.; Vega, S.; Marco-Jiménez, F. Tiny Turtles Purchased at Pet Stores Are a Potential High Risk for Salmonella Human Infection in the Valencian Region, Eastern Spain. Vector Borne Zoonotic Dis. 2016, 16, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Nakadai, A.; Kuroki, T.; Kato, Y.; Suzuki, R.; Yamai, S.; Yaginuma, C.; Shiotani, R.; Yamanouchi, A.; Hayashidani, H. Prevalence of Salmonella Spp. in Pet Reptiles in Japan. J. Vet. Med. Sci. 2005, 67, 97–101. [Google Scholar] [CrossRef]
- Schröter, M.; Roggentin, P.; Hofmann, J.; Speicher, A.; Laufs, R.; Mack, D. Pet Snakes as a Reservoir for Salmonella Enterica Subsp. Diarizonae (Serogroup IIIb): A Prospective Study. Appl. Environ. Microbiol. 2004, 70, 613–615. [Google Scholar] [CrossRef]
- Kylie, J.; McEwen, S.A.; Boerlin, P.; Reid-Smith, R.J.; Weese, J.S.; Turner, P.V. Prevalence of Antimicrobial Resistance in Fecal Escherichia coli and Salmonella Enterica in Canadian Commercial Meat, Companion, Laboratory, and Shelter Rabbits (Oryctolagus cuniculus) and Its Association with Routine Antimicrobial Use in Commercial Meat Rabbits. Prev. Vet. Med. 2017, 147, 53–57. [Google Scholar] [CrossRef]
- Ju LIM, J.; Hyeok KIM, D.; Ju LEE, J.; Geun KIM, D.; Hun KIM, S.; Min, W.; Hee CHANG, H.; Hee RHEE, M.; Kim, S. Prevalence of Lawsonia Intracellularis, Salmonella Spp. and Eimeria Spp. in Healthy and Diarrheic Pet Rabbits. J. Vet. Med. Sci. 2012, 74, 263–265. [Google Scholar] [CrossRef]
- Bartholomew, M.L.; Heffernan, R.T.; Wright, J.G.; Klos, R.F.; Monson, T.; Khan, S.; Trees, E.; Sabol, A.; Willems, R.A.; Flynn, R.; et al. Multistate Outbreak of Salmonella Enterica Serotype Enteritidis Infection Associated with Pet Guinea Pigs. Vector Borne Zoonotic Dis. 2014, 14, 414–421. [Google Scholar] [CrossRef]
- Pignon, C.; Mayer, J. Zoonoses of Ferrets, Hedgehogs, and Sugar Gliders. Vet. Clin. N. Am. Exot. Anim. Pract. 2011, 14, 533–549. [Google Scholar] [CrossRef] [PubMed]
- Keeble, E.; Koterwas, B. Salmonellosis in Hedgehogs. Vet. Clin. N. Am. Exot. Anim. Pract. 2020, 23, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Willis, C.; Wilson, T.; Greenwood, M.; Ward, L. Pet Reptiles Associated with a Case of Salmonellosis in an Infant Were Carrying Multiple Strains of Salmonella. J. Clin. Microbiol. 2002, 40, 4802–4803. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). National Salmonella Surveillance Annual Report, 2016. Atlanta, Georgia: US Department of Health and Human Services, CDC, 2018. Available online: https://www.cdc.gov/nationalsurveillance/pdfs/2016-Salmonella-report-508.pdf (accessed on 12 September 2023).
- Koutsoumanis, K.; Allende, A.; Alvarez-Ordóñez, A.; Bolton, D.; Bover-Cid, S.; Chemaly, M.; De Cesare, A.; Herman, L.; Hilbert, F.; Lindqvist, R.; et al. Salmonella Control in Poultry Flocks and Its Public Health Impact. EFSA J. 2019, 17, e05596. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.F.; Nambiar, R.B.; Xu, X.B.; Weng, S.T.; Pan, H.; Zheng, K.C.; Yue, M. Global Genomic Characterization of Salmonella Enterica Serovar Telelkebir. Front. Microbiol. 2021, 12, 704152. [Google Scholar] [CrossRef] [PubMed]
- Belas, A.; Menezes, J.; Gama, L.T.; Pomba, C. Sharing of Clinically Important Antimicrobial Resistance Genes by Companion Animals and Their Human Household Members. Microb. Drug Resist. 2020, 26, 1174–1185. [Google Scholar] [CrossRef] [PubMed]
- Prandi, I.; Bellato, A.; Nebbia, P.; Stella, M.C.; Ala, U.; von Degerfeld, M.M.; Quaranta, G.; Robino, P. Antibiotic Resistant Escherichia coli in Wild Birds Hospitalised in a Wildlife Rescue Centre. Comp. Immunol. Microbiol. Infect. Dis. 2023, 93, 101945. [Google Scholar] [CrossRef]
- Marco-Fuertes, A.; Jordá, J.; Marin, C.; Lorenzo-Rebenaque, L.; Montoro-Dasi, L.; Vega, S. Multidrug-Resistant Escherichia coli Strains to Last Resort Human Antibiotics Isolated from Healthy Companion Animals in Valencia Region. Antibiotics 2023, 12, 1638. [Google Scholar] [CrossRef]
- Fabian, N.J.; Mannion, A.J.; Feng, Y.; Madden, C.M.; Fox, J.G. Intestinal Colonization of Genotoxic Escherichia coli Strains Encoding Colibactin and Cytotoxic Necrotizing Factor in Small Mammal Pets. Vet. Microbiol. 2020, 240, 108506. [Google Scholar] [CrossRef]
- WHO. WHO Medically Important List. A Risk Management Tool. for Mitigating Antimicrobial Resistance Due to Non-Human. Use. 7 Th Revision 2023; WHO: Geneva, Switzerland, 2023. [Google Scholar]
- Dwomoh, F.P.; Kotey, F.C.N.; Dayie, N.T.K.D.; Osei, M.M.; Amoa-Owusu, F.; Bannah, V.; Alzahrani, F.M.; Halawani, I.F.; Alzahrani, K.J.; Egyir, B.; et al. Phenotypic and Genotypic Detection of Carbapenemase-Producing Escherichia coli and Klebsiella Pneumoniae in Accra, Ghana. PLoS ONE 2022, 17, e0279715. [Google Scholar] [CrossRef]
- Armin, S.; Fallah, F.; Karimi, A.; Karbasiyan, F.; Alebouyeh, M.; Rafiei Tabatabaei, S.; Rajabnejad, M.; Mansour Ghanaie, R.; Fahimzad, S.A.; Abdollahi, N.; et al. Antibiotic Susceptibility Patterns for Carbapenem-Resistant Enterobacteriaceae. Int. J. Microbiol. 2023, 2023, 8920977. [Google Scholar] [CrossRef] [PubMed]
- Tocalli, L.; Boselli, A.; Rimoldi, S.G.; Gismondo, M.R. EPIDEMIOLOGICAL OBSERVATORY: Spreading of ESBL and Carbapenemase Positive Strains in the Period between January 2007–June 2012, at the Hospital—University Campus—Hospital “Luigi Sacco” in Milan. Microbiol. Medica 2012, 27, 143–147. [Google Scholar] [CrossRef]
- Murugan, M.S.; Sinha, D.K.; Vinodh Kumar, O.R.; Yadav, A.K.; Pruthvishree, B.S.; Vadhana, P.; Nirupama, K.R.; Bhardwaj, M.; Singh, B.R. Epidemiology of Carbapenem-Resistant Escherichia coli and First Report of BlaVIM Carbapenemases Gene in Calves from India. Epidemiol. Infect. 2019, 147, e159. [Google Scholar] [CrossRef] [PubMed]
- Caneschi, A.; Bardhi, A.; Barbarossa, A.; Zaghini, A. The Use of Antibiotics and Antimicrobial Resistance in Veterinary Medicine, a Complex Phenomenon: A Narrative Review. Antibiotics 2023, 12, 487. [Google Scholar] [CrossRef] [PubMed]
- del Solar Bravo, R.E.; Sharman, M.J.; Raj, J.; Scudder, C. Antibiotic Therapy in Dogs and Cats in General Practice in the United Kingdom before Referral. J. Small Anim. Pract. 2023, 64, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Beaudoin, A.L.; Bollig, E.R.; Burgess, B.A.; Cohn, L.A.; Cole, S.D.; Dear, J.D.; Fellman, C.L.; Frey, E.; Goggs, R.; Johnston, A.; et al. Prevalence of Antibiotic Use for Dogs and Cats in United States Veterinary Teaching Hospitals, August 2020. J. Vet. Intern. Med. 2023, 37, 1864–1875. [Google Scholar] [CrossRef]
- Oglesbee, B.L.; Lord, B. Gastrointestinal Diseases of Rabbits. In Ferrets, Rabbits and Rodents, 4th ed.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 174–187. ISBN 9780323484350. [Google Scholar] [CrossRef]
- De Cubellis, J. Common Emergencies in Rabbits, Guinea Pigs, and Chinchillas. Vet. Clin. N. Am.—Exot. Anim. Pract. 2016, 19, 411–429. [Google Scholar] [CrossRef]
- Krause, K.M.; Serio, A.W.; Kane, T.R.; Connolly, L.E. Aminoglycosides: An Overview. Cold Spring Harb. Perspect. Med. 2016, 6, a027029. [Google Scholar] [CrossRef]
- Fletcher, S. Understanding the Contribution of Environmental Factors in the Spread of Antimicrobial Resistance. Environ. Health Prev. Med. 2015, 20, 243. [Google Scholar] [CrossRef]
- Aminov, R. Acquisition and Spread of Antimicrobial Resistance: A Tet(X) Case Study. Int. J. Mol. Sci. 2021, 22, 3905. [Google Scholar] [CrossRef]
- Sweileh, W.M. Global Research Activity on Antimicrobial Resistance in Food-Producing Animals. Arch. Public Health 2021, 79, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Plan Nacional de Resistencias a los Antibióticos ¿Quiénes Somos? Available online: https://www.resistenciaantibioticos.es/es/quienes-somos (accessed on 7 July 2023).
- Plan Nacional de Resistencias a los Antibióticos Programa REDUCE Porcino. Available online: https://www.resistenciaantibioticos.es/es/lineas-de-accion/control/programas-de-reduccion-en-sanidad-animal/programa-reduce-porcino (accessed on 7 July 2023).
- Talat, A.; Miranda, C.; Poeta, P.; Khan, A.U. Farm to Table: Colistin Resistance Hitchhiking through Food. Arch. Microbiol. 2023, 205, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Obando, P.; Suárez-Arrabal, M.C.; Esparza, M.J.; Guía-ABE. Descripcion General de Los Principales Grupos de Fármacos Antimicrobianos. Antibioticos 2020. Available online: https://www.guia-abe.es/generalidades-descripcion-general-de-los-principales-grupos-de-farmacos-antimicrobianos-antibioticos- (accessed on 27 July 2023).
| Antibiotic Group | Antibiotic | Abbreviation | WHO | Concentration |
|---|---|---|---|---|
| Aminoglycosides | Amikacin | AMI | CIA | 2–32 μg/mL |
| Gentamicin | GEN | CIA | 0.5–8 μg/mL | |
| Tobramycin | TOB | CIA | 0.5–8 μg/mL | |
| Carbapenemases | Ertapenem | ERT | NA | 0.12–2 μg/mL |
| Meropenem | MER | NA | 0.12–16 μg/mL | |
| Cephalosporins | Cefepime | CEP | HPCIA | 0.5–8 μg/mL |
| Cefixime | CIX | HPCIA | 0.5–2 μg/mL | |
| Cefotaxime | CTA | HIA | 0.5–4 μg/mL | |
| Cefoxitin | CXI | HIA | 2–16 μg/mL | |
| Cefuroxime | CUR | HIA | 2–16 μg/mL | |
| Cefalexin | CLE | HPCIA | 8–32 μg/mL | |
| Ceftazidime | CTZ | HPCIA | 0.5–8 μg/mL | |
| Nitrofurans | Nitrofurantoin | NIT | NA | 32–64 μg/mL |
| Penicillins | Ampicillin | AMP | HIA | 2–16 μg/mL |
| Amoxicillin/ Clavulanic acid | AMC | HIA | 2/2–32/2 μg/mL | |
| Piperacillin/ Tazobactam | PIT | NA | 2/4–32/4 μg/mL | |
| Ticarcillin | TIC | HIA | 4–32 μg/mL | |
| Quinolones | Ciprofloxacin (FQ) | CIP | HPCIA | 0.12–1 μg/mL |
| Levofloxacin (FQ) | LEVO | HPCIA | 0.25–2 μg/mL | |
| Nalidixic acid (Q) | NAL | HPCIA | 16 μg/mL | |
| Folate inhibitor pathway | Sulfamethoxazole/ Trimethoprim | TRS | HIA | 1/19–8/152 μg/mL |
| Glycylcycline | Tigecycline | TIG | NA | 0.5–4 μg/mL |
| Antibiotic Group | Antibiotic | Abbreviation | WHO | Concentration |
|---|---|---|---|---|
| Aminoglycosides | Amikacin | AMI | CIA | 2–32 μg/mL |
| Gentamicin | GEN | CIA | 0.5–8 μg/mL | |
| Amphenicols | Chloramphenicol | CHL | HIA | 8–64 μg/mL |
| Carbapenemases | Meropenem | MER | NA | 0.12–2 μg/mL |
| Cephalosporins | Cefotaxime | CTA | HPCIA | 0.5–8 μg/mL |
| Ceftazidime | CTZ | HPCIA | 0.5–8 μg/mL | |
| Folate inhibitorpathway | Sulfamethoxazole | SME | HIA | 1/19–8/152 μg/mL |
| Trimethoprim | TRI | HIA | 0.5–16 μg/mL | |
| Glycylcycline | Tigecycline | TIG | NA | 0.5–4 μg/mL |
| Macrolides | Azithromycin | AZI | CIA | 2–64 μg/mL |
| Penicillins | Ampicillin | AMP | HIA | 2–16 μg/mL |
| Polymyxins | Colistin | COL | HPCIA | 1–16 μg/mL |
| Quinolones | Ciprofloxacin (FQ) | CIP | HPCIA | 0.12–1 μg/mL |
| Nalidixic acid (Q) | NAL | HPCIA | 16 μg/mL | |
| Tetracyclines | Tetracycline | TET | HIA | 2–32 μg/mL |
| Species | NT | N and (%) of E. coli/Animal Species |
|---|---|---|
| Oryctolagus cuniculus (European rabbit) | 44 | 10/44 (22.7) |
| Cavia porcellus (Guinea pig) | 17 | 5/17 (29.4) |
| Rattus norvegicus (Common rat) | 3 | 2/3 (66.7) |
| Cricetinae (Common hamster) | 3 | 0/3 (0) |
| Chinchilla laniguera (Chinchilla) | 1 | 0/3 (0) |
| Erinaceinae (Hedgehog) | 1 | 1/1 (100) |
| Gerbillinae (Gerbil) | 1 | 0/1 (0) |
| Mustela putorius furo (Ferret) | 1 | 1/1 (100) |
| Petaurus breviceps (Sugar gliders) | 1 | 1/1 (100) |
| Total | 72 | 20/72 (27.8) |
| Antibiotic Group | % AMR of E. coli Isolated/Group | Antibiotic | % AMR of E. coli Isolated/Antibiotic |
|---|---|---|---|
| Aminoglycosides | 36.7 a,b ± 6.2 | Amikacin | 25 a,b,c ± 9.7 |
| Gentamicin | 45 c,e ± 11.1 | ||
| Tobramycin | 40 a,c,e ± 11 | ||
| Carbapenemases | 15 c ± 5.6 | Ertapenem | 30 a,c ± 10.2 |
| Meropenem | 0 g ± 0 | ||
| Cephalosporins | 34.3 a,b ± 4 | Cefepime | 30 a,c ± 10.2 |
| Cefixime | 45 c,e ± 11.1 | ||
| Cefotaxime | 30 a,c ± 10.2 | ||
| Cefoxitin | 30 a,c ± 10.2 | ||
| Cefuroxime | 40 a,c,e ± 11 | ||
| Cefalexin | 25 a,b,c ± 9.7 | ||
| Ceftazidime | 40 a,c,e ± 11 | ||
| Nitrofurans | 0 d ± 0 | Nitrofurantoin | 0 g ± 0 |
| Penicillins | 38.8 a,b ± 5.4 | Ampicillin | 60 d,e,f ± 11 |
| Amoxicillin/ Clavulanic acid | 25 a,b,c ± 9.7 | ||
| Piperacillin/ Tazobactam | 5 b,g ± 4.9 | ||
| Ticarcillin | 65 d,e,f ± 10.7 | ||
| Quinolones | 80 e ± 5.2 | Ciprofloxacin (FQ) | 80 d ± 9 |
| Levofloxacin (FQ) | 75 d,f ± 9.7 | ||
| Nalidixic acid (Q) | 85 d ± 8 | ||
| Folate inhibitor pathway | 48.3 b ± 6.5 | Sulfamethoxazole | 60 d,e,f ± 11 |
| Trimethoprim | 40 a,c,e ± 11 | ||
| Sulfamethoxazole/ Trimethoprim | 45 c,e ± 11.1 | ||
| Glycylcycline | 0 d ± 0 | Tigecycline | 0 g ± 0 |
| Polymyxins | 25 a,c ± 9.7 | Colistin | 25 a,b,c ± 9.7 |
| Tetracyclines | 50 a,b ± 11.2 | Tetracycline | 50 c,e,f ± 11.2 |
| Amphenicols | 25 a,c ± 9.7 | Chloramphenicol | 25 a,b,c ± 9.7 |
| Macrolides | 15 c,d ± 8 | Azithromycin | 15 a,b,g ± 8 |
| N of AB Groups | N of Isolates (%) | AMR Patterns |
|---|---|---|
| 0 | 3 | - |
| 1 | 2 | QUIN |
| 2 | 0 | - |
| 3 | 1 | QUIN-FOL-PEN |
| 1 | QUIN-CEPHA-AMI | |
| 1 | QUIN-TET-POLIM | |
| 4 | 2 | QUIN-FOL-AMI-PEN |
| 1 | QUIN-FOL-PEN-TET | |
| 5 | 0 | - |
| 6 | 1 | QUIN-FOL-AMI-PEN-TET-AMPH |
| 1 | QUIN-FOL-AMI-PEN-CEPHA-TET | |
| 1 | QUIN-FOL-PEN-CEPHA-TET-AMPH | |
| 7 | 1 | QUIN-FOL-AMI-PEN-CEPHA-POLIM-CARB |
| 8 | 1 | QUIN-FOL-AMI-PEN-CEPHA-TET-AMPH-CARB |
| 1 | QUIN-FOL-AMI-PEN-CEPHA-TET-POLIM-CARB | |
| 1 | QUIN-FOL-CEPHA-TET-AMPH-POLIM-MACR-CARB | |
| 9 | 1 | QUIN-FOL-AMI-PEN-CEPHA-TET-AMPH-MACR-CARB |
| 1 | QUIN-FOL-AMI-PEN-CEPHA-TET-POLIM-MACR-CARB | |
| TOTAL | 20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marco-Fuertes, A.; Vega, S.; Villora-Gonzalez, J.; Marin, C.; Montoro-Dasi, L. Exploring the Prevalence of Antimicrobial Resistance in Salmonella and commensal Escherichia coli from Non-Traditional Companion Animals: A Pilot Study. Life 2024, 14, 170. https://doi.org/10.3390/life14020170
Marco-Fuertes A, Vega S, Villora-Gonzalez J, Marin C, Montoro-Dasi L. Exploring the Prevalence of Antimicrobial Resistance in Salmonella and commensal Escherichia coli from Non-Traditional Companion Animals: A Pilot Study. Life. 2024; 14(2):170. https://doi.org/10.3390/life14020170
Chicago/Turabian StyleMarco-Fuertes, Ana, Santiago Vega, José Villora-Gonzalez, Clara Marin, and Laura Montoro-Dasi. 2024. "Exploring the Prevalence of Antimicrobial Resistance in Salmonella and commensal Escherichia coli from Non-Traditional Companion Animals: A Pilot Study" Life 14, no. 2: 170. https://doi.org/10.3390/life14020170





