Minimally Invasive Chevron Akin (MICA) Osteotomy Corrects Radiographic Parameters but Not Central Metatarsal Loading in Moderate to Severe Hallux Valgus without Metatarsalgia
Abstract
1. Introduction
2. Material and Methods
2.1. Patient Enrollment
2.2. Surgical Techniques and Postoperative Protocols
2.3. Radiographs Analysis
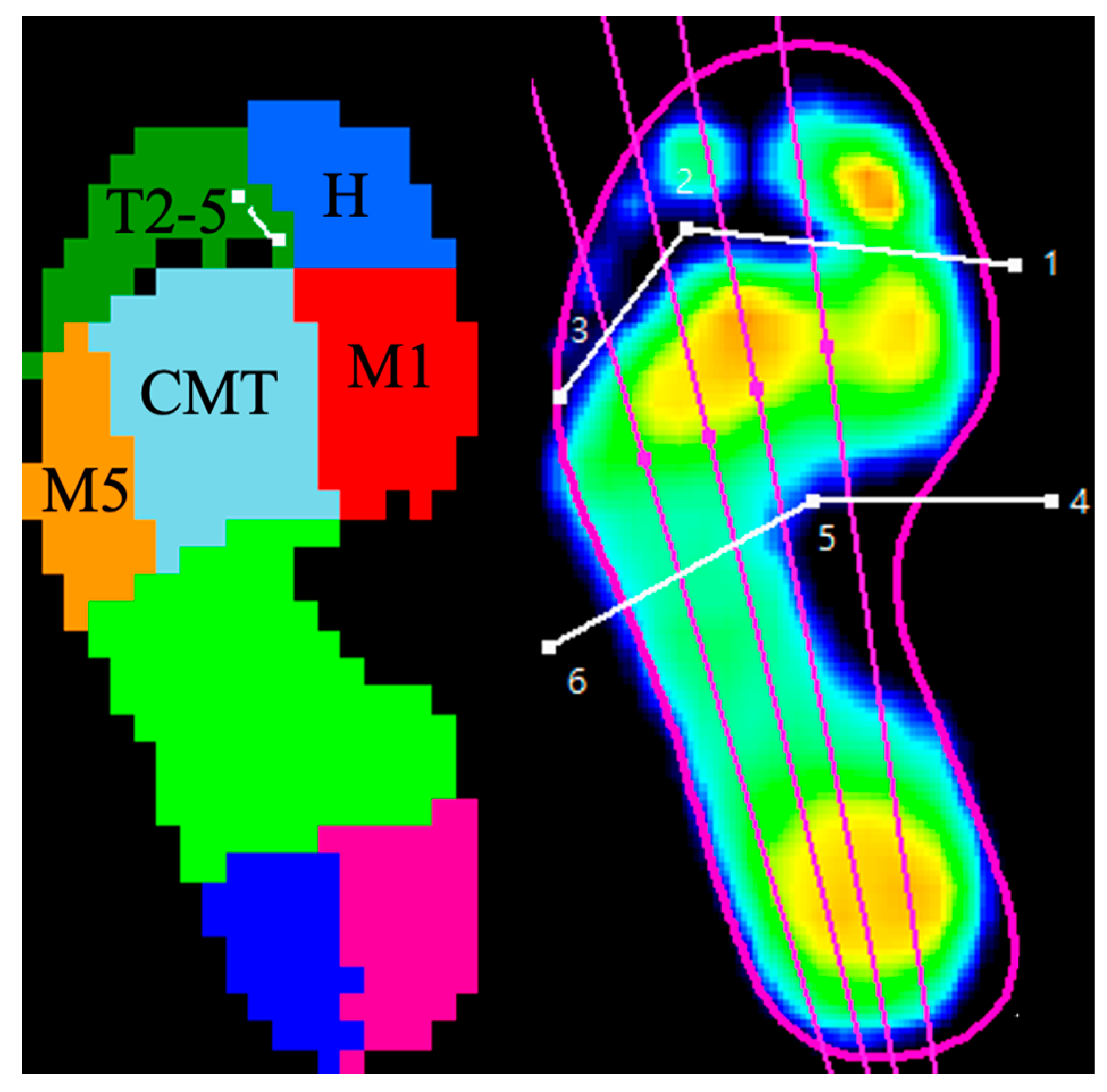
2.4. Pedographs Analysis
2.5. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Radiographic Outcomes
3.3. Pedographic Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shi, G.G.; Whalen, J.L.; Turner, N.S., 3rd; Kitaoka, H.B. Operative Approach to Adult Hallux Valgus Deformity: Principles and Techniques. J. Am. Acad. Orthop. Surg. 2020, 28, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Lopez, V.; Slullitel, G. Metatarsalgia: Assessment Algorithm and Decision Making. Foot Ankle Clin. 2019, 24, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Nunes, G.A.; de Carvalho, K.A.M.; Ferreira, G.F.; Filho, M.V.P.; Baptista, A.D.; Zambelli, R.; Vega, J. Minimally invasive Chevron Akin (MICA) osteotomy for severe hallux valgus. Arch. Orthop. Trauma Surg. 2023, 143, 5507–5514. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.L.; Ray, R.; Miller, G.; Gordon, D.J. Third-Generation Minimally Invasive Chevron and Akin Osteotomies (MICA) in Hallux Valgus Surgery: Two-Year Follow-up of 292 Cases. J. Bone Jt. Surg. Am. 2021, 103, 1203–1211. [Google Scholar] [CrossRef] [PubMed]
- Razak, A.H.; Zayegh, A.; Begg, R.K.; Wahab, Y. Foot plantar pressure measurement system: A review. Sensors 2012, 12, 9884–9912. [Google Scholar] [CrossRef] [PubMed]
- Wafai, L.; Zayegh, A.; Woulfe, J.; Aziz, S.M.; Begg, R. Identification of Foot Pathologies Based on Plantar Pressure Asymmetry. Sensors 2015, 15, 20392–20408. [Google Scholar] [CrossRef] [PubMed]
- Deepashini, H.; Omar, B.; Paungmali, A.; Amaramalar, N.; Ohnmar, H.; Leonard, J. An insight into the plantar pressure distribution of the foot in clinical practice: Narrative review. Pol. Ann. Med. 2014, 21, 51–56. [Google Scholar] [CrossRef]
- Bryant, A.R.; Tinley, P.; Cole, J.H. Plantar pressure and radiographic changes to the forefoot after the Austin bunionectomy. J. Am. Podiatr. Med. Assoc. 2005, 95, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Hida, T.; Okuda, R.; Yasuda, T.; Jotoku, T.; Shima, H.; Neo, M. Comparison of plantar pressure distribution in patients with hallux valgus and healthy matched controls. J. Orthop. Sci. 2017, 22, 1054–1059. [Google Scholar] [CrossRef]
- Hofmann, U.K.; Götze, M.; Wiesenreiter, K.; Müller, O.; Wünschel, M.; Mittag, F. Transfer of plantar pressure from the medial to the central forefoot in patients with hallux valgus. BMC Musculoskelet. Disord. 2019, 20, 149. [Google Scholar] [CrossRef]
- Verdu-Roman, C.; Sanz-Reig, J.; Martinez-Gimenez, E.; Carratala-Munuera, C.; Lopez-Pineda, A.; Quesada, J.A.; Gil-Guillen, V.F.; Orozco-Beltran, D. Plantar pressure improvement in moderate hallux valgus with modified chevron osteotomy: Clinical and radiographic outcomes. Foot Ankle Surg. 2020, 26, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Kernozek, T.W.; Sterriker, S.A. Chevron (Austin) distal metatarsal osteotomy for hallux valgus: Comparison of pre- and post-surgical characteristics. Foot Ankle Int. 2002, 23, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Costa, J.; Avila, A.; Kleinowski, D.; Kroth, L.; Contreras, M. Modified Chevron osteotomy: Preliminary analysis of baropodometric behavior. Acta Ortop. Bras. 2009, 18, 191–196. [Google Scholar] [CrossRef]
- Resch, S.; Stenström, A. Evaluation of hallux valgus surgery with dynamic foot pressure registration with the Fscan system. Foot 1995, 5, 115–121. [Google Scholar] [CrossRef]
- Mazzotti, A.; Arceri, A.; Artioli, E.; Langone, L.; Zielli, S.O.; Martini, B.; Traina, F.; Faldini, C.; Brognara, L. Hallux Valgus Plantar Pressure Distribution before and after a Distal Metatarsal Osteotomy. J. Clin. Med. 2024, 13. [Google Scholar] [CrossRef] [PubMed]
- King, C.M.; Hamilton, G.A.; Ford, L.A. Effects of the lapidus arthrodesis and chevron bunionectomy on plantar forefoot pressures. J. Foot Ankle Surg. 2014, 53, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Cancilleri, F.; Marinozzi, A.; Martinelli, N.; Ippolito, M.; Spiezia, F.; Ronconi, P.; Denaro, V. Comparison of plantar pressure, clinical, and radiographic changes of the forefoot after biplanar Austin osteotomy and triplanar Boc osteotomy in patients with mild hallux valgus. Foot Ankle Int. 2008, 29, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Waldecker, U. Metatarsalgia in hallux valgus deformity: A pedographic analysis. J. Foot Ankle Surg. 2002, 41, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.L.; Lau, B.; Alkhalfan, Y.; Trowbridge, S.; Gordon, D.; Vernois, J.; Lam, P.; Ray, R. Fourth-Generation Minimally Invasive Hallux Valgus Surgery With Metaphyseal Extra-Articular Transverse and Akin Osteotomy (META): 12 Month Clinical and Radiologic Results. Foot Ankle Int. 2023, 44, 178–191. [Google Scholar] [CrossRef]
- de Carvalho, K.A.M.; Baptista, A.D.; de Cesar Netto, C.; Johnson, A.H.; Dalmau-Pastor, M. Minimally Invasive Chevron-Akin for Correction of Moderate and Severe Hallux Valgus Deformities: Clinical and Radiologic Outcomes With a Minimum 2-Year Follow-up. Foot Ankle Int. 2022, 43, 1317–1330. [Google Scholar] [CrossRef]
- Tay, A.Y.W.; Goh, G.S.; Koo, K.; Yeo, N.E.M. Third-Generation Minimally Invasive Chevron-Akin Osteotomy for Hallux Valgus Produces Similar Clinical and Radiological Outcomes as Scarf-Akin Osteotomy at 2 Years: A Matched Cohort Study. Foot Ankle Int. 2022, 43, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Holme, T.J.; Sivaloganathan, S.S.; Patel, B.; Kunasingam, K. Third-Generation Minimally Invasive Chevron Akin Osteotomy for Hallux Valgus. Foot Ankle Int. 2020, 41, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, M.J.; Jones, C.P. Hallux valgus: Demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007, 28, 759–777. [Google Scholar] [CrossRef]
- Redfern, D.; Vernois, J. Minimally Invasive Chevron Akin (MICA) for Correction of Hallux Valgus. Tech. Foot Ankle Surg. 2016, 15, 3–11. [Google Scholar] [CrossRef]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Kitano, N.; Shima, H. The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J. Bone Jt. Surg. Am. 2007, 89, 2163–2172. [Google Scholar] [CrossRef] [PubMed]
- Wagner, P.; Wagner, E. Role of Coronal Plane Malalignment in Hallux Valgus Correction. Foot Ankle Clin. 2020, 25, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, Y.; Desai, A.; Mehta, J. Lateral sesamoid position in hallux valgus: Correlation with the conventional radiological assessment. Foot Ankle Surg. 2011, 17, 308–311. [Google Scholar] [CrossRef]
- Togei, K.; Shima, H.; Yasuda, T.; Tsujinaka, S.; Nakamura, G.; Neo, M. Plantar pressure distribution in hallux valgus feet after a first metatarsal proximal crescentic osteotomy with a lesser metatarsal proximal shortening osteotomy. Foot Ankle Surg. 2021, 27, 665–672. [Google Scholar] [CrossRef]
- Bryant, A.; Singer, K.; Tinley, P. Comparison of the reliability of plantar pressure measurements using the two-step and midgait methods of data collection. Foot Ankle Int. 1999, 20, 646–650. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.C.; Rikhraj, I.S.; Woo, Y.L.; Yeo, W.; Ng, Y.C.S.; Koo, K. Clinical and Radiological Outcomes Comparing Percutaneous Chevron-Akin Osteotomies vs Open Scarf-Akin Osteotomies for Hallux Valgus. Foot Ankle Int. 2018, 39, 311–317. [Google Scholar] [CrossRef]
- Wong, D.W.; Cheung, J.C.; Zhao, J.G.; Ni, M.; Yang, Z.Y. Forefoot Function after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis on Plantar Load Measurement. J. Clin. Med. 2023, 12, 1384. [Google Scholar] [CrossRef] [PubMed]
- Geng, X.; Shi, J.; Chen, W.; Ma, X.; Wang, X.; Zhang, C.; Chen, L. Impact of first metatarsal shortening on forefoot loading pattern: A finite element model study. BMC Musculoskelet. Disord. 2019, 20, 625. [Google Scholar] [CrossRef] [PubMed]
| Demographics | Average ± Standard Deviation |
|---|---|
| Age (years old) | 50.83 ± 12.38 |
| Height (cm) | 156.84 ± 3.07 |
| Weight (kg) | 53.38 ± 9.21 |
| BMI (kg/cm2) | 21.69 ± 3.40 |
| Pre-Op | Post-Op 3M | Change | p Value | Effect Size | |
|---|---|---|---|---|---|
| HVA | 31.90 ± 6.30 (21.27–46.59) | 7.97871 ± 6.11 (0.48–17.46) | −23.92 ± 6.52 | <0.001 * | 3.85 |
| IMA | 14.2016 ± 2.61 (12.25–18.65) | 5.94871 ± 3.20 (1.23–10.04) | −8.25 ± 2.74 | <0.001 * | 2.83 |
| DMAA | 30.9923 ± 9.91 | 9.40323 ± 7.91 | −21.59 ± 7.68 | <0.001 * | 2.41 |
| MT1L | 65.49 ± 4.79 | 62.33 ± 5.63 | |||
| MT2L | 77.79 ± 5.83 | 76.91 ± 6.81 | |||
| MT1CL | 65.49 ± 4.79 | 63.06 ± 4.99 | −2.43 ± 2.54 | <0.001 * | 0.50 |
| MT2PD | 11.41 ± 2.58 | 11.17 ± 2.43 | −0.25 ± 1.68 | 0.422 | 0.10 |
| MT1LHS | Round: 14 (45%) Intermediate: 7 (23%) Angular: 10 (32%) | Round: 6 (19%) Intermediate: 11 (35%) Angular: 14 (45%) | <0.001 # | ||
| LSG | Normal: 0 (0%) Mild: 5 (16%) Moderate: 15 (48%) Severe: 11 (35%) | Normal: 3 (10%) Mild: 16 (52%) Moderate: 9 (29%) Severe: 3 (10%) | <0.001 # | ||
| LMA | 7.397 ± 7.46 | 6.58 ± 6.59 | −0.81 ± 5.83 | 0.443 * | 0.12 |
| CPA | 19.55 ± 5.22 | 19.58 ± 4.45 | 0.035 ± 2.73 | 0.942 * | 0.01 |
| Pre-Op | Post-Op 3M | Change | p Value | Effect Size | |
|---|---|---|---|---|---|
| Hallux | 44.59 ± 21.61 | 23.56 ± 12.79 | −21.04 ± 24.43 | <0.001 * | 1.18 |
| Toe 2–5 | 26.12 ± 15.78 | 27.85 ± 12.98 | +1.72 ± 14.92 | 0.525 | 0.12 |
| M1 | 69.06 ± 29.97 | 52.73 ± 13.90 | −16.34 ± 28.14 | 0.003 * | 0.70 |
| M2–4 | 251.98 ± 58.18 | 251.08 ± 51.55 | −0.90 ± 59.50 | 0.934 | 0.02 |
| M5 | 40.49 ± 15.66 | 43.99 ± 19.02 | +3.50 ± 16.95 | 0.260 | 0.20 |
| Pre-Op | Post-Op 3M | Change | p Value | Effect Size | |
|---|---|---|---|---|---|
| Hallux | 33.30 ± 14.70 | 20.00 ± 11.23 | −13.30 ± 17.46 | <0.001 * | 1.02 |
| Toe 2–5 | 16.62 ± 11.77 | 15.44 ± 7.92 | −1.18 ± 10.60 | 0.539 | 0.12 |
| M1 | 43.12 ± 17.84 | 35.32 ± 9.89 | −7.80 ± 18.78 | 0.028 * | 0.54 |
| M2–4 | 81.18 ± 18.64 | 81.03 ± 17.28 | −0.15 ± 22.10 | 0.970 | 0.01 |
| M5 | 33.98 ± 11.69 | 37.72 ± 14.81 | +3.74 ± 14.81 | 0.170 | 0.28 |
| Pre-Op | Post-Op 3M | Change | p Value | Effect Size | |
|---|---|---|---|---|---|
| Hallux | 14.84 ± 7.32 | 5.21 ± 3.38 | −9.63 ± 7.42 | <0.001 * | 1.69 |
| Toe 2–5 | 7.71 ± 4.22 | 8.14 ± 4.04 | +0.43 ± 4.39 | 0.584 | 0.10 |
| M1 | 28.85 ± 10.84 | 20.66 ± 5.80 | −8.19 ± 9.24 | 0.008 * | 0.94 |
| M2–4 | 115.55 ± 35.71 | 106.78 ± 30.54 | −8.77 ± 23.28 | 0.129 | 0.26 |
| M5 | 17.95 ± 8.01 | 17.41 ± 7.53 | −0.55 ± 6.93 | 0.676 | 0.07 |
| Pre-Op | Post-Op 3M | Change | p Value | Effect Size | |
|---|---|---|---|---|---|
| Hallux | 10.82 ± 5.36 | 4.29 ± 2.92 | −6.53 ± 5.59 | <0.001 * | 1.51 |
| Toe 2–5 | 4.82 ± 3.23 | 4.32± 2.21 | −0.49 ± 3.01 | 0.360 | 0.18 |
| M1 | 17.99 ± 5.06 | 13.63 ± 3.70 | −4.35 ± 5.16 | 0.038 * | 0.98 |
| M2–4 | 37.41 ± 11.08 | 34.25 ± 8.29 | −3.16 ± 9.37 | 0.150 | 0.32 |
| M5 | 15.13 ± 5.66 | 14.72 ± 5.13 | −0.41 ± 5.68 | 0.712 | 0.08 |
| Year | Authors | Patients Population | Intervention | Follow-Up | Pedographic Outcomes |
|---|---|---|---|---|---|
| 2024 | Mazzotti et al. [15] | Mild-to-moderate HV Excluded patients with metatarsalgia and longer 2–3 metatarsals | Distal metatarsal SERI osteotomy | 12 months | Increased loading on 1st and central metatarsals |
| 2020 | Verdu-Roman et al. [11] | Moderate HV Not mentioned if metatarsalgia or not | Modified Chevron osteotomy | 12 months | Increased loading on hallux and all metatarsals |
| 2014 | King et al. [16] | No mention of HV severity (Chevron group: average HVA 24.38, IMA 13.59) Not mentioned if metatarsalgia occurred or not | Chevron osteotomy vs. Lapidus procedure (both may include associated procedures) | 6 months | Chevron osteotomy: decreased loading on hallux |
| 2010 | Costa et al. [13] | Mild-to-moderate HV Included patients both with and without metatarsalgia. | Mod. Chevron osteotomy (No metatarsalgia) vs. Cheveron with Weil osteotomy (Metatarsalgia) | 3 months | Chevron: decreased loading on hallux and 1st metatarsal, increased loading on lesser metatarsals Chevron with Weil osteotomy: decreased loading on hallux |
| 2008 | Cancilleri et al. [17] | Mild HV with metatarsalgia | Austin osteotomy vs. Boc osteotomy | Austin group: 43.4 months Boc group: 31.6 months | Austin osteotomy: decreased loading on hallux and 1st metatarsal Boc osteotomy: decreased loading on hallux, 1st to 3rd metatarsals |
| 2005 | Bryant et al. [8] | HVA > 20 Not mentioned if metatarsalgia occurred or not | Modified Austin bunionectomy | 24 months | Decreased loading on hallux, 1st and 2nd metatarsal |
| 2002 | Kernozek et al. [12] | Mild to moderate Not mentioned if metatarsalgia or not | Austin osteotomy | 12 months | Increased central metatarsal loading, decreased medial toe loading |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, W.-K.; Tie, T.-H.A.; Hsu, W.-L.; Chen, Y.-Y. Minimally Invasive Chevron Akin (MICA) Osteotomy Corrects Radiographic Parameters but Not Central Metatarsal Loading in Moderate to Severe Hallux Valgus without Metatarsalgia. Life 2024, 14, 734. https://doi.org/10.3390/life14060734
Hsu W-K, Tie T-HA, Hsu W-L, Chen Y-Y. Minimally Invasive Chevron Akin (MICA) Osteotomy Corrects Radiographic Parameters but Not Central Metatarsal Loading in Moderate to Severe Hallux Valgus without Metatarsalgia. Life. 2024; 14(6):734. https://doi.org/10.3390/life14060734
Chicago/Turabian StyleHsu, Wei-Kuo, Tung-Hee Albert Tie, Wei-Li Hsu, and Yan-Yu Chen. 2024. "Minimally Invasive Chevron Akin (MICA) Osteotomy Corrects Radiographic Parameters but Not Central Metatarsal Loading in Moderate to Severe Hallux Valgus without Metatarsalgia" Life 14, no. 6: 734. https://doi.org/10.3390/life14060734
APA StyleHsu, W.-K., Tie, T.-H. A., Hsu, W.-L., & Chen, Y.-Y. (2024). Minimally Invasive Chevron Akin (MICA) Osteotomy Corrects Radiographic Parameters but Not Central Metatarsal Loading in Moderate to Severe Hallux Valgus without Metatarsalgia. Life, 14(6), 734. https://doi.org/10.3390/life14060734






