Measurement of Nasal Contour Landmarks in Septorhinoplasties with Special Regard to the Course of Postoperative Swelling Using a Three-Dimensional Camera
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Surgical Treatment Procedure
2.3. Camera System
2.4. Data Acquisition and Measurements
2.5. Anatomic Landmarks
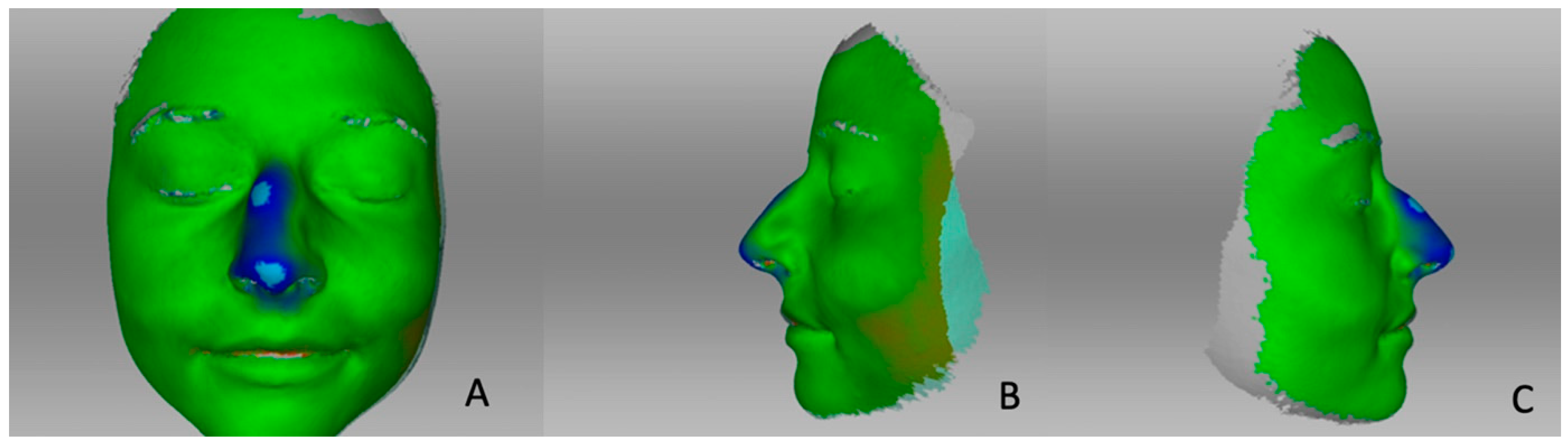
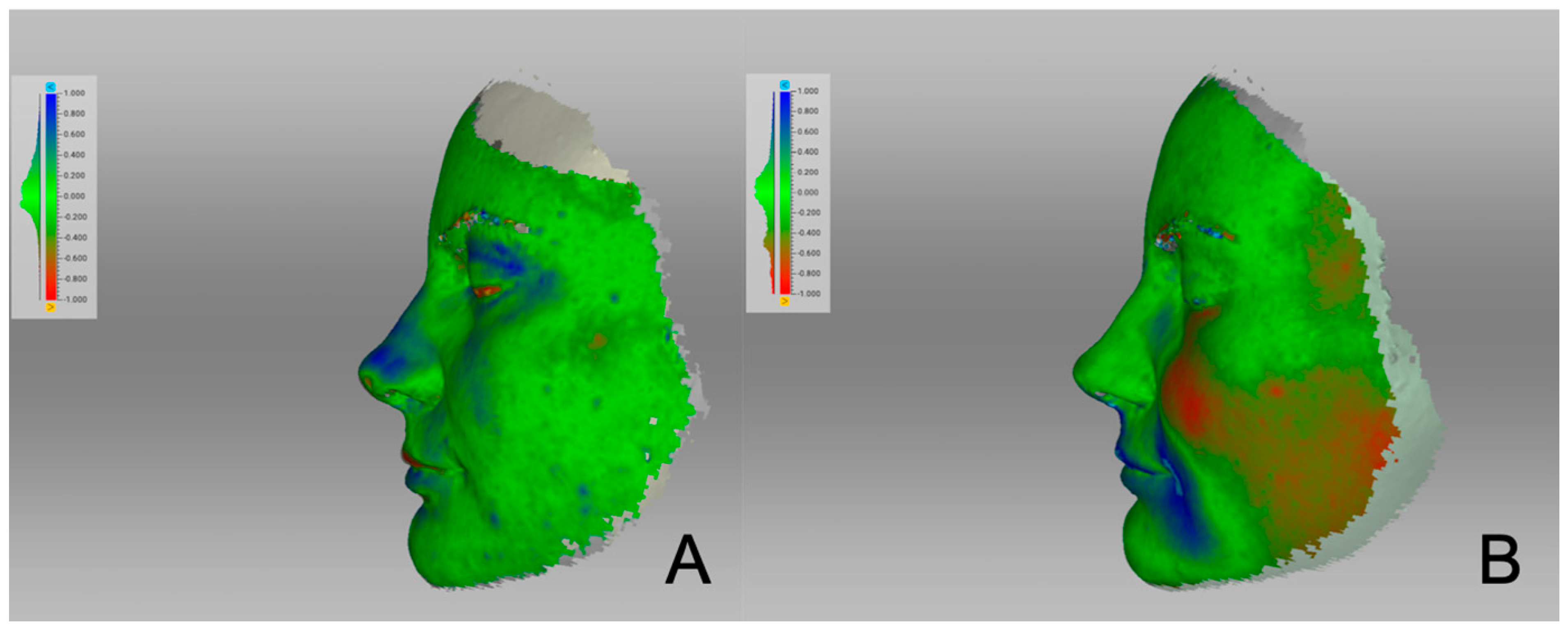
2.6. Surface Distance Maps
2.7. Statistical Analysis
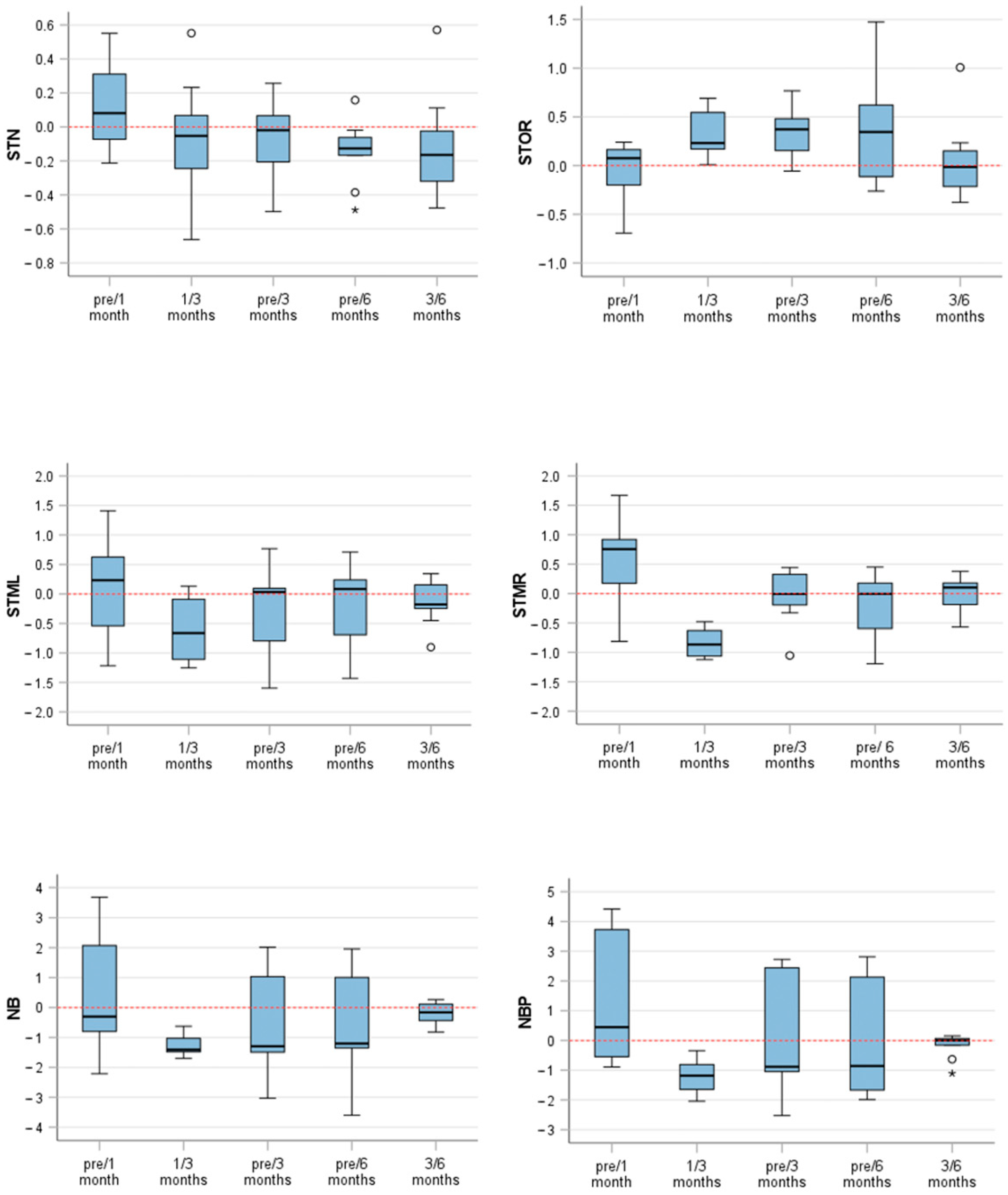
3. Results
Landmark Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Honrado, C.P.; Lee, S.; Bloomquist, D.S.; Larrabee, J.W.F. Quantitative assessment of nasal changes after maxillomandibular surgery using a 3-dimensional digital imaging system. Arch. Facial Plast. Surg. 2006, 8, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Ritschl, L.M.; Grill, F.D.; Mittermeier, F.; Lonic, D.; Wolff, K.-D.; Roth, M.; Loeffelbein, D.J. Evaluation of a portable low-budget three-dimensional stereophotogrammetry system for nasal analysis. J. Cranio-Maxillofac. Surg. 2018, 46, 2008–2016. [Google Scholar] [CrossRef] [PubMed]
- Lekakis, G.; Claes, P.; Hamilton, G.S., 3rd; Hellings, P.W. Three-dimensional surface imaging and the continuous evolution of preoperative and postoperative assessment in rhinoplasty. Facial. Plast. Surg. 2016, 32, 88–94. [Google Scholar] [PubMed]
- Hollander, M.H.J.; Kraeima, J.; Meesters, A.M.L.; Delli, K.; Vissink, A.; Jansma, J.; Schepers, R.H. Reproducibility of 3D scanning in the periorbital region. Sci. Rep. 2021, 11, 3671. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, J.E.; Marcus, E.; Tepper, O.; Layke, J. Discovering the true resolution of postoperative swelling after rhinoplasty using 3-dimensional photographic assessment. Plast. Reconstr. Surg. Glob. Open 2019, 7 (Suppl. S8), 11–12. [Google Scholar] [CrossRef]
- Ritschl, L.M.; Classen, C.; Kilbertus, P.; Eufinger, J.; Storck, K.; Fichter, A.M.; Wolff, K.-D.; Grill, F.D. Comparison of three-dimensional imaging of the nose using three different 3D-photography systems: An observational study. Head Face Med. 2024, 20, 7. [Google Scholar] [CrossRef] [PubMed]
- Hitch, J. The amazing spider scan: Artec’s hand-held 3D scanner was developed for the International Space Station, though its earthbound applications will really have you over the moon. New Equip. Digest 2016, 81, 27. [Google Scholar]
- Available online: http://cdn.artec3d.com/content-hub-filed/artec3d.-s.spider-a.8-web-de-nop.pdf (accessed on 6 November 2023).
- Göldner, D.; Karakostis, F.A.; Falcucci, A. Practical and technical aspects for the 3D scanning of lithic artefacts using micro-computed tomography techniques and laser light scanners for subsequent geometric morphometric analysis. Introducing the StyroStone protocol. PLoS ONE 2021, 17, e0267163. [Google Scholar] [CrossRef]
- Probst, J.; Dritsas, K.; Halazonetis, D.; Ren, Y.; Katsaros, C.; Gkantidis, N. Precision of a hand-held 3D surface scanner in dry and wet skeletal surfaces: An ex vivo study. Diagnostics 2022, 12, 2251. [Google Scholar] [CrossRef]
- Campanacho, V. 3D Scanning Guidelines for Skeletal Remains with Artec Studio 11 at the University of Sheffield. 2017. Available online: https://sites.google.com/site/vanessacampanacho/resources (accessed on 4 November 2023).
- Christou, T.; Kau, C.H.; Waite, P.D.; Kheir, N.A.; Mouritsen, D. Modified method of analysis for surgical correction of facial asymmetry. Ann. Maxillofac. Surg. 2013, 3, 185–191. [Google Scholar]
- Swennen, G.R.J.; Schutyser, F.A.; Hausamen, J.E. Three-Dimensional Cephalometry: A Color Atlas and Manual; Springer Science and Business Media: Berlin/Heidelberg, Germany, 2005. [Google Scholar]
- Jayaratne, Y.S.; McGrath, C.P.; Zwahlen, R.A. How accurate are the fusion of cone-beam CT and 3-D stereophotographic images? PLoS ONE 2012, 7, e49585. [Google Scholar] [CrossRef] [PubMed]
- Brito, Í.M.; Avashia, Y.; Rohrich, R.J. Evidence-based nasal analysis for rhinoplasty: The 10-7-5 method. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2632. [Google Scholar] [CrossRef] [PubMed]
- Clappier, M.; Tanna, N. Preoperative evaluation of the rhinoplasty patient. Clin. Plast. Surg. 2021, 49, 1–11. [Google Scholar] [CrossRef]
- Lekakis, G.; Claes, P.; Hamilton, G.S., 3rd; Hellings, P.W. Evolution of preoperative rhinoplasty consult by computer imaging. Facial Plast. Surg. 2016, 32, 80–87. [Google Scholar] [PubMed]
- Woodard, C.R.; Park, S.S. Nasal and facial analysis. Clin. Plast. Surg. 2010, 37, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Strub, B.; Meuli-Simmen, C.; Bessler, S. Photodocumentation in rhinoplasty surgery. Eur. J. Plast. Surg. 2013, 36, 141–148. [Google Scholar] [CrossRef]
- Seymour, R.; Meechan, J.; Blair, G. An investigation into post-operative pain after third molar surgery under local analgesia. Br. J. Oral Maxillofac. Surg. 1985, 23, 410–418. [Google Scholar] [CrossRef]
- Demir, N.; Sanli, A.; Demir, G.; Erdogan, B.A.; Yilmaz, H.B.; Paksoy, M. The Evaluation of relationship between body mass index and nasal geometry using objective and subjective methods. J. Craniofacial Surg. 2015, 26, 1861–1864. [Google Scholar] [CrossRef]
- Lee, H.S.; Yoon, H.Y.; Kim, I.H.; Hwang, S.H. The effectiveness of postoperative intervention in patients after rhinoplasty: A meta-analysis. Eur. Arch. Otorhinolaryngol. 2017, 274, 2685–2694. [Google Scholar] [CrossRef]
- Li, Z.; Giunta, R.E.; Frank, K.; Schenck, T.L.; Koban, K.C. Reproducibility of novel soft-tissue landmarks on three-dimensional human facial scan images in caucasian and asian. Aesthetic Plast. Surg. 2022, 46, 719–731. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Gašparović, B.; Morelato, L.; Lenac, K.; Mauša, G.; Zhurov, A.; Katić, V. Comparing direct measurements and three-dimensional (3D) scans for evaluating facial soft tissue. Sensors 2023, 23, 2412. [Google Scholar] [CrossRef] [PubMed]
- Chisholm, E.; Jallali, N. Rhinoplasty and septorhinoplasty outcome evaluation. Ear Nose Throat J. 2012, 91, E10–E14. [Google Scholar] [CrossRef] [PubMed]
- Modabber, A.; Rana, M.; Ghassemi, A.; Gerressen, M.; Gellrich, N.-C.; Hölzle, F.; Rana, M. Three-dimensional evaluation of postoperative swelling in treatment of zygomatic bone fractures using two different cooling therapy methods: A randomized, observer-blind, prospective study. Trials 2013, 14, 238. [Google Scholar] [CrossRef] [PubMed]
- Osborne, P.R.; Magri, L.V.; da Silva, A.M.B.R.; da Silva, M.A.M.R.; Sverzut, A.T.; Trivellato, A.E.; Sverzut, C.E. A retrospective evaluation of facial volume in patients submitted to bimaxillary orthognathic surgery using 3D stereophotogrammetry. Craniomaxillofacial Trauma Reconstr. Open 2021, 6, 2472751221990272. [Google Scholar] [CrossRef]
- van der Vlis, M.; Dentino, K.M.; Vervloet, B.; Padwa, B.L. Postoperative swelling after orthognathic surgery: A prospective volumetric analysis. J. Oral Maxillofac. Surg. 2014, 72, 2241–2247. [Google Scholar] [CrossRef] [PubMed]
- Reategui, A.B.; Phillips, S.B.; Dinis, J.B.; Junn, A.B.; Parsaei, Y.D.; Yang, J.; Lopez, J.M.; Steinbacher, D.M.D. Postoperative edema resolution post-orthognathic triple jaw surgery: A three-dimensional volumetric analysis. J. Craniofacial Surg. 2022, 33, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Kau, C.H.; Cronin, A.; Durning, P.; Zhurov, A.I.; Sandham, A.; Richmond, S. A new method for the 3D measurement of postoperative swelling following orthognathic surgery. Orthod. Craniofac. Res. 2006, 9, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Koban, K.C.; Perko, P.; Li, Z.; Xu, Y.; Giunta, R.E.; Alfertshofer, M.G.; Kohler, L.H.; Freytag, D.L.; Cotofana, S.; Frank, K. 3D anthropometric facial imaging—A comparison of different 3D scanners. Facial Plast. Surg. Clin. N. Am. 2022, 30, 149–158. [Google Scholar]
- Tsounis, M.; Papadopoulou, D.; Faris, C. Intraoperative use of a tablet computer to aid rhinoplasty. Ann. R. Coll. Surg. Engl. 2017, 99, 37–38. [Google Scholar] [CrossRef]
- Pallanch, J. Introduction to 3D imaging technologies for the facial plastic surgeon. Facial Plast. Surg. Clin. N. Am. 2011, 19, xv–xvi, vii. [Google Scholar] [CrossRef] [PubMed]
- Koban, K.C.; Leitsch, S.; Holzbach, T.; Volkmer, E.; Metz, P.M.; Giunta, R.E. 3D-imaging and analysis for plastic surgery by smartphone and tablet: An alternative to professional systems? Handchir. Mikrochir. Plast. Chir. 2014, 46, 97–104. [Google Scholar] [PubMed]



| Variable | n (%) |
|---|---|
| Female | 20 (69) |
| Male | 9 (31) |
| Age, years (mean ± SD) | 34.2 ± 14.6 |
| Diagnosis/intention | n (%) |
| Aesthetically + functional | 29 (100) |
| Paired Samples Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Paired Differences | t | df | Significance | |||||||
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval | One-Sided p | Two-Sided p | |||||
| Lower | Upper | |||||||||
| Pair 1 | STN—pre/1 month vs. STN—pre/3 months | 0.217 | 0.508 | 0.141 | −0.090 | 0.523 | 1.538 | 12 | 0.075 | 0.150 |
| Pair 2 | STN—pre/3 months–STN—pre/6 months | 0.172 | 0.384 | 0.077 | 0.013 | 0.330 | 2.231 | 24 | 0.018 | 0.035 |
| Pair 3 | STN—1/3 months–STN—3/6 months | 0.026 | 0.638 | 0.213 | −0.465 | 0.517 | 0.122 | 8 | 0.453 | 0.906 |
| Paired Samples Test | ||||||||||
| Paired Differences | t | df | Significance | |||||||
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | One-Sided p | Two-Sided p | |||||
| Lower | Upper | |||||||||
| Pair 1 | STOR—pre/1 month vs. STOR—pre/3 months | −0.312 | 0.384 | 0.107 | −0.544 | −0.080 | −2.930 | 12 | 0.006 | 0.013 |
| Pair 2 | STOR—pre/3 months vs. STOR—pre/6 months | 0.030 | 0.487 | 0.097 | −0.171 | 0.231 | 0.311 | 24 | 0.379 | 0.758 |
| Pair 3 | STOR—1/3 months vs. STOR—3/6 months | 0.277 | 0.452 | 0.151 | −0.070 | 0.624 | 1.840 | 8 | 0.052 | 0.103 |
| Pair 1 | STML—pre/1 month vs. STML—pre/3 months | 0.541 | 0.708 | 0.196 | 0.113 | 0.968 | 2.755 | 12 | 0.009 | 0.017 |
| Pair 2 | STML—pre/3 months vs. STML—pre/6 months | 0.105 | 0.404 | 0.081 | −0.061 | 0.272 | 1.304 | 24 | 0.102 | 0.205 |
| Pair 3 | STML—1/3 months vs. STML—3/6 months | −0.431 | 0.700 | 0.233 | −0.969 | 0.107 | −1.847 | 8 | 0.051 | 0.102 |
| Pair 1 | STMR—pre/1 month vs. STMR—pre/3 months | 0.621 | 0.487 | 0.135 | 0.327 | 0.916 | 4.595 | 12 | 0.000 | 0.001 |
| Pair 2 | STMR—pre/3 months vs. STMR—pre/6 months | 0.130 | 0.380 | 0.076 | −0.027 | 0.287 | 1.714 | 24 | 0.050 | 0.099 |
| Pair 3 | STMR—1/3 months vs. STMR—3/6 months | −0.809 | 0.337 | 0.112 | −1.068 | −0.550 | −7.197 | 8 | 0.000 | 0.000 |
| Pair 1 | NB—pre/1 month vs. NB—pre/3 months | 0.986 | 0.547 | 0.152 | 0.656 | 1.317 | 6.501 | 12 | 0.000 | 0.000 |
| Pair 2 | NB—pre/3 months vs. NB—pre/6 months | 0.149 | 0.382 | 0.076 | −0.009 | 0.306 | 1.946 | 24 | 0.032 | 0.063 |
| Pair 3 | NB—1/3 months vs. NB—3/6 months | −1.075 | 0.528 | 0.176 | −1.481 | −0.669 | −6.109 | 8 | 0.000 | 0.000 |
| Pair 1 | NBP—pre/1 month vs. NBP—pre/3 months | 1.296 | 0.825 | 0.229 | 0.798 | 1.795 | 5.667 | 12 | 0.000 | 0.000 |
| Pair 2 | NBP—pre/3 months vs. NBP—pre/6 months | 0.232 | 0.507 | 0.101 | 0.023 | 0.441 | 2.286 | 24 | 0.016 | 0.031 |
| Pair 3 | NBP—1/3 months vs. NBP—3/6 months | −1.035 | 0.575 | 0.192 | −1.477 | −0.594 | −5.406 | 8 | 0.000 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Storck, K.; Eufinger, J.; Kotz, S.; Classen, C.; Ritschl, L.M. Measurement of Nasal Contour Landmarks in Septorhinoplasties with Special Regard to the Course of Postoperative Swelling Using a Three-Dimensional Camera. Life 2024, 14, 813. https://doi.org/10.3390/life14070813
Storck K, Eufinger J, Kotz S, Classen C, Ritschl LM. Measurement of Nasal Contour Landmarks in Septorhinoplasties with Special Regard to the Course of Postoperative Swelling Using a Three-Dimensional Camera. Life. 2024; 14(7):813. https://doi.org/10.3390/life14070813
Chicago/Turabian StyleStorck, Katharina, Julia Eufinger, Sebastian Kotz, Carolina Classen, and Lucas M. Ritschl. 2024. "Measurement of Nasal Contour Landmarks in Septorhinoplasties with Special Regard to the Course of Postoperative Swelling Using a Three-Dimensional Camera" Life 14, no. 7: 813. https://doi.org/10.3390/life14070813
APA StyleStorck, K., Eufinger, J., Kotz, S., Classen, C., & Ritschl, L. M. (2024). Measurement of Nasal Contour Landmarks in Septorhinoplasties with Special Regard to the Course of Postoperative Swelling Using a Three-Dimensional Camera. Life, 14(7), 813. https://doi.org/10.3390/life14070813






