Ultrasound Cine Loop Standard Operating Procedure for Benign Thyroid Diseases—Evaluation of Non-Physician Application
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Ethics
2.2. Investigators and Observers
2.3. Examination Protocols and Devices
2.4. Volumetric Determinations
2.5. Data Analyses and Statistics
3. Results
3.1. Patient Data and Thyroid Volume Measurements
- Thyroid volume on conventional physician US vs. MTA US cine loop review: r(33) = 0.89, p < 0.0001.
- Thyroid volume on conventional physician US vs. mtCT: r(33) = 0.90, p < 0.0001.
- Thyroid volume on MTA US cine loop review vs. mtCT: r(33) = 0.90, p < 0.0001.
- Thyroid volume on mtCT vs. emCT: r(33) = 0.93, p < 0.0001.
3.2. Thyroid Nodules
- TN volume on conventional physicians US vs. MTA US cine loop review: r(67) = 0.96, p < 0.0001.
- largest TN diameter on conventional physician US vs. MTS US cine loop review: r(67) = 0.99, p < 0.0001.
3.3. Technical Impairments
4. Discussion
Limitations of this Study
- The number of patients included is relatively low (n = 33). This is due to the wish of the authors to compare the US volumetric determinations to a gold standard. Since only benign thyroid diseases have been investigated, surgical results are not available, and multi-contour 3D CT measurements were defined as the gold standard. Therefore, patients with I-124-PET/CT of the neck (performed within the scope of other study protocols that were not part of the present research) were chosen. The reliability of the presented data should be proven by future research containing larger patient collectives.
- Due to the limited number of surgical results (n = 5), comprehensive histopathological correlations of the TIRADS classifications are missing. There was no gold standard to define reference TIRADS classifications. However, it was not the aim of this study to verify TIRADS findings but to prove whether TIRADS classifications can be assessed concordantly by conventional physician US and MTA US cine loop review. In order to generate evidence regarding the value of cine loop review for TIRADS classifications, further studies with TIRADS focused prospective study protocols need to be conducted.
- US investigations are not part of the MTA curriculum in Germany. Therefore, one-hour training might be insufficient to allow for high-quality cine loops. The authors concede that the brevity of the conducted training session might be one of the reasons for the impairments shown in Figure 5. In addition, it is not possible to teach pathological US findings within an hour, which would be necessary for reliable static images.
- The second reading reviews of the MTA US cine loops were performed by the same three physicians that conducted and assessed the initial conventional thyroid US. To avoid remembrance biases, the review process was carried out blinded. That means the initial examiner and the reviewer of the MTA US were different persons. Furthermore, the cine loop reviews were carried out after a long interval (five years after the conventional US investigations).
- The thyroid volume of the included patients was <100 mL. Larger thyroid volumes may lead to higher variances of the results. This effect could already be seen with the larger volumes (>40 mL) of the examined collective (Figure 3).
- The evaluation of the thyroid US cine loop SOP was restricted to its reliability with regard to volumetric determinations and TIRADS classifications. The study cannot provide any information regarding auto-immune or inflammatory thyroid disorders such as Graves’ disease, Hashimoto’s disease, De Quervain’s thyroiditis, or Riedel’s thyroiditis, which are often characterized by hypoechoic parenchyma patterns or infiltrations.
- Duplex sonography and elastography have not been investigated. Applying these two methods would require more in-depth MTA training. In particular, identifying reasonable nodular lesions for elastography would be challenging for non-physician operators. The additional acquisition of Doppler-enhanced US images, on the other hand, is theoretically unproblematic and is established in our department in the meantime.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meltzer, C.J.; Irish, J.; Angelos, P.; Busaidy, N.L.; Davies, L.; Dwojak, S.; Ferris, R.L.; Haugen, B.R.; Harrell, R.M.; Haymart, M.R.; et al. American head and neck society endocrine section clinical consensus statement: North American quality statements and evidence-based multidisciplinary workflow algorithms for the evaluation and management of thyroid nodules. Head Neck 2019, 41, 843–856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dietrich, C.F.; Bojunga, J. Ultrasound of the thyroid. Laryngorhinootologie 2016, 95, 87–104. [Google Scholar] [PubMed]
- Kahaly, G.J.; Bartalena, L.; Hegedus, L.; Leenhardt, L.; Poppe, K.; Pearce, S.H. 2018 European thyroid association guideline for the management of Graves’ hyperthyroidism. Eur. Thyroid J. 2018, 7, 167–186. [Google Scholar] [CrossRef]
- Luster, M.; Pfestroff, A.; Hanscheid, H.; Verburg, F.A. Radioiodine therapy. Semin. Nucl. Med. 2017, 47, 126–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horvath, E.; Majlis, S.; Rossi, R.; Franco, C.; Niedmann, J.P.; Castro, A.; Dominguez, M. An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J. Clin. Endocrinol. Metab. 2009, 94, 1748–1751. [Google Scholar] [CrossRef]
- Tessler, F.N.; Middleton, W.D.; Grant, E.G.; Hoang, J.K.; Berland, L.L.; Teefey, S.A.; Cronan, J.J.; Beland, M.D.; Desser, T.S.; Frates, M.C.; et al. ACR thyroid imaging, reporting and data system (TI-RADS): White paper of the ACR TI-RADS committee. J. Am. Coll. Radiol. 2017, 14, 587–595. [Google Scholar] [CrossRef] [Green Version]
- Russ, G.; Bonnema, S.J.; Erdogan, M.F.; Durante, C.; Ngu, R.; Leenhardt, L. European thyroid association guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults: The EU-TIRADS. Eur. Thyroid J. 2017, 6, 225–237. [Google Scholar] [CrossRef] [Green Version]
- Verburg, F.A.; Grelle, I.; Tatschner, K.; Reiners, C.; Luster, M. Prevalence of thyroid disorders in elderly people in Germany. A screening study in a country with endemic goitre. Nuklearmedizin 2017, 56, 9–13. [Google Scholar] [CrossRef]
- Bianek-Bodzak, A.; Lewczuk, A.; Sworczak, K. [The role of doppler ultrasound studies in the diagnosis of the thyroid diseases]. Polski Merkuriusz Lekarski 2003, 15, 588–591. [Google Scholar]
- Bojunga, J.; Mondorf, A. Thyroid elastography. Laryngorhinootologie 2019, 98, 150–156. [Google Scholar]
- Klein, B.; Djaldetti, M. Side effects of ultrasound examinations. Harefuah 1980, 99, 442–443. [Google Scholar] [PubMed]
- Curriculum for fundamentals of ultrasound in clinical practice. J. Ultrasound. Med. 2019, 38, 1937–1950. [CrossRef] [PubMed] [Green Version]
- Chiu, Y.H.; Chang, K.V.; Chen, I.J.; Wu, W.T.; Ozcakar, L. Utility of sonoelastography for the evaluation of rotator cuff tendon and pertinent disorders: A systematic review and meta-analysis. Eur. Radiol. 2020, 30, 6663–6672. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.H.; Chen, Y.J.; Chang, K.V.; Wu, W.T.; Ozcakar, L. Ultrasound measurements of superficial and deep masticatory muscles in various postures: Reliability and influencers. Sci. Rep. 2020, 10, 14357. [Google Scholar] [CrossRef]
- Andermann, P.; Schlogl, S.; Mader, U.; Luster, M.; Lassmann, M.; Reiners, C. Intra- and interobserver variability of thyroid volume measurements in healthy adults by 2D versus 3D ultrasound. Nuklearmedizin 2007, 46, 1–7. [Google Scholar]
- Grani, G.; Lamartina, L.; Cantisani, V.; Maranghi, M.; Lucia, P.; Durante, C. Interobserver agreement of various thyroid imaging reporting and data systems. Endocr. Connect. 2018, 7, 1–7. [Google Scholar] [CrossRef]
- Attenhofer, C.H.; Pellikka, P.A.; Oh, J.K.; Roger, V.L.; McCully, R.B.; Shub, C.; Seward, J.B. Is review of videotape necessary after review of digitized cine-loop images in stress echocardiography? A prospective study in 306 patients. J. Am. Soc. Echocardiogr. 1997, 10, 179–184. [Google Scholar] [CrossRef]
- Scott, T.E.; Jones, J.; Rosenberg, H.; Thomson, A.; Ghandehari, H.; Rosta, N.; Jozkow, K.; Stromer, M.; Swan, H. Increasing the detection rate of congenital heart disease during routine obstetric screening using cine loop sweeps. J. Ultrasound Med. 2013, 32, 973–979. [Google Scholar] [CrossRef]
- Gaarder, M.; Seierstad, T.; Soreng, R.; Drolsum, A.; Begum, K.; Dormagen, J.B. Standardized cine-loop documentation in renal ultrasound facilitates skill-mix between radiographer and radiologist. Acta Radiol. 2015, 56, 368–373. [Google Scholar] [CrossRef]
- Dormagen, J.B.; Gaarder, M.; Drolsum, A. Standardized cine-loop documentation in abdominal ultrasound facilitates offline image interpretation. Acta Radiol. 2015, 56, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Stolz, L.A.; Muruganandan, K.M.; Bisanzo, M.C.; Sebikali, M.J.; Dreifuss, B.A.; Hammerstedt, H.S.; Nelson, S.W.; Nayabale, I.; Adhikari, S.; Shah, S.P. Point-of-care ultrasound education for non-physician clinicians in a resource-limited emergency department. Trop. Med. Int. Health 2015, 20, 1067–1072. [Google Scholar] [CrossRef] [PubMed]
- O’Dochartaigh, D.; Douma, M.; MacKenzie, M. Five-year retrospective review of physician and non-physician performed ultrasound in a Canadian critical care helicopter emergency medical service. Prehosp. Emerg. Care 2017, 21, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Barnett, M.; Pillow, M.T.; Carnell, J.; Rohra, A.; DeSandro, S.; Gardner, A.K. Informing the revolution: A needs assessment of ultrasound knowledge and skills among graduating physician assistant students. J. Physician Assist. Educ. 2018, 29, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Rizzolo, D.; Krackov, R.E. Integration of ultrasound into the physician assistant curriculum. J. Physician Assist. Educ. 2019, 30, 103–110. [Google Scholar] [CrossRef]
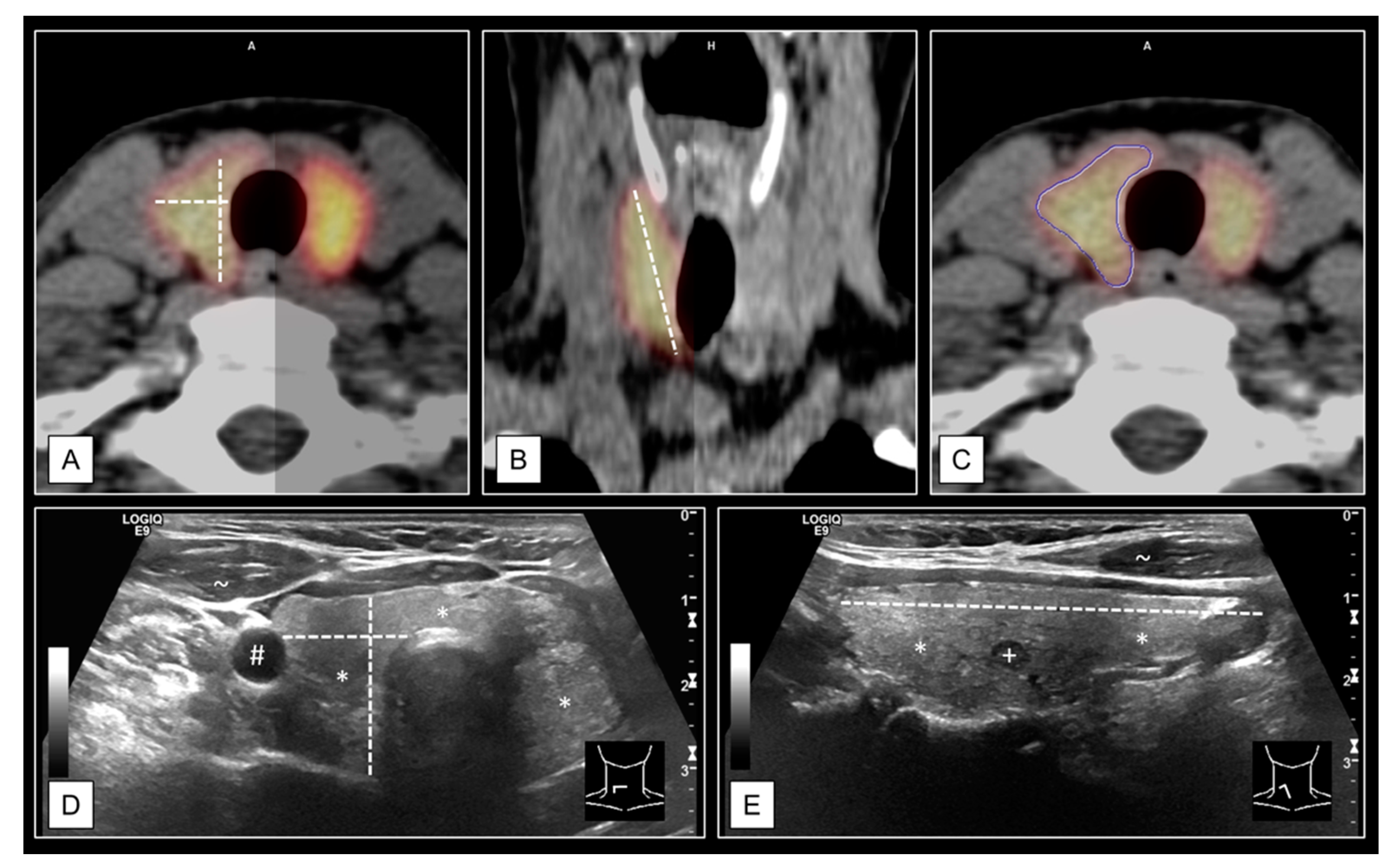
- Seifert, P.; Winkens, T.; Kuhnel, C.; Guhne, F.; Freesmeyer, M. I-124-pet/us fusion imaging in comparison to conventional diagnostics and tc-99m pertechnetate spect/us fusion imaging for the function assessment of thyroid nodules. Ultrasound Med. Biol. 2019, 45, 2298–2308. [Google Scholar] [CrossRef] [PubMed]
- Winkens, T.; Seifert, P.; Hollenbach, C.; Kuhnel, C.; Guhne, F.; Freesmeyer, M. The fusion iena study: Comparison of i-124-pet/us fusion imaging with conventional diagnostics for the functional assessment of thyroid nodules by multiple observers. Nuklearmedizin 2019, 58, 434–442. [Google Scholar] [CrossRef]
- Freesmeyer, M.; Winkens, T.; Weissenrieder, L.; Kuhnel, C.; Guhne, F.; Schenke, S.; Drescher, R.; Seifert, P. Fusion iena scholar study: Sensor-navigated i-124-pet/us fusion imaging versus conventional diagnostics for retrospective functional assessment of thyroid nodules by medical students. Sensors 2020, 20, 3409. [Google Scholar] [CrossRef]
- Kwak, J.Y.; Han, K.H.; Yoon, J.H.; Moon, H.J.; Son, E.J.; Park, S.H.; Jung, H.K.; Choi, J.S.; Kim, B.M.; Kim, E.K. Thyroid imaging reporting and data system for us features of nodules: A step in establishing better stratification of cancer risk. Radiology 2011, 260, 892–899. [Google Scholar] [CrossRef] [Green Version]
- Brunn, J.; Block, U.; Ruf, G.; Bos, I.; Kunze, W.P.; Scriba, P.C. Volumetric analysis of thyroid lobes by real-time ultrasound (author’s transl.). Deutsche Medizinische Wochenschrift 1981, 106, 1338–1340. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, S.; Midorikawa, S.; Fukushima, T.; Shimura, H.; Ohira, T.; Ohtsuru, A.; Abe, M.; Shibata, Y.; Yamashita, S.; Suzuki, S.; et al. Systematic determination of thyroid volume by ultrasound examination from infancy to adolescence in Japan: The Fukushima health management survey. Endocr. J. 2015, 62, 261–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bojunga, J. Ultrasound of thyroid nodules. Ultraschall. Med. 2018, 39, 488–511. [Google Scholar] [CrossRef] [PubMed]
- Freesmeyer, M.; Darr, A.; Schierz, J.H.; Schleussner, E.; Wiegand, S.; Opfermann, T. 3D ultrasound dicom data of the thyroid gland. First experiences in exporting, archiving, second reading and 3D processing. Nuklearmedizin 2012, 51, 73–78. [Google Scholar]
- Poole, P.S.; Chung, R.; Lacoursiere, Y.; Palmieri, C.R.; Hull, A.; Engelkemier, D.; Rochelle, M.; Trivedi, N.; Pretorius, D.H. Two-dimensional sonographic cine imaging improves confidence in the initial evaluation of the fetal heart. J. Ultrasound Med. 2013, 32, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Yoon, D.Y.; Seo, Y.L.; Kim, J.H.; Baek, S.; Lim, K.J.; Cho, Y.K.; Yun, E.J. Intraobserver and interobserver variability in ultrasound measurements of thyroid nodules. J. Ultrasound Med. 2018, 37, 173–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vulpoi, C.; Mogos, V.; Ciobanu, D.G.; Preda, C.; Ungureanu, M.C.; Cristea, C.; Leustean, L.; Zbranca, E. Thyroid ultrasonography. Interobserver and intraobserver variations. Revista Medico-Chirurgicala a Societatii de Medici si Naturalisti din Iasi 2007, 111, 864–871. [Google Scholar] [PubMed]
- Freesmeyer, M.; Knichel, L.; Kuehnel, C.; Winkens, T. Stitching of sensor-navigated 3D ultrasound datasets for the determination of large thyroid volumes—A phantom study. Med. Ultrason. 2018, 20, 480–486. [Google Scholar] [CrossRef] [Green Version]
- Seifert, P.; Winkens, T.; Knichel, L.; Kuhnel, C.; Freesmeyer, M. Stitching of 3D ultrasound datasets for the determination of large thyroid volumes—Phantom study part II: Mechanically-swept probes. Med. Ultrason. 2019, 21, 389–398. [Google Scholar] [CrossRef]
- Ruggieri, M.; Fumarola, A.; Straniero, A.; Maiuolo, A.; Coletta, I.; Veltri, A.; Di Fiore, A.; Trimboli, P.; Gargiulo, P.; Genderini, M.; et al. The estimation of the thyroid volume before surgery—An important prerequisite for minimally invasive thyroidectomy. Langenbeck’s Arch. Surg. 2008, 393, 721–724. [Google Scholar] [CrossRef]
- Seifert, P.; Gorges, R.; Zimny, M.; Kreissl, M.C.; Schenke, S. Interobserver agreement and efficacy of consensus reading in Kwak-, EU-, and ACR-thyroid imaging recording and data systems and ATA guidelines for the ultrasound risk stratification of thyroid nodules. Endocrine 2020, 67, 143–154. [Google Scholar] [CrossRef]




| Method | Lobe/Organ | Mean ± SD | Median | Range (Min, Max) | LoA |
|---|---|---|---|---|---|
| mtCT (mL) | Right | 19.0 ± 15.4 | 13.1 | 2.7, 64.3 | −11.3, 49.2 |
| (gold standard) | Left | 12.7 ± 8.4 | 10.2 | 2.4, 36.3 | −3.7, 29.2 |
| n = 33 | Thyroid | 31.7 ± 19.9 | 22.1 | 6.9, 85.3 | −7.3, 70.7 |
| emCT (mL) | Right | 17.9 ± 15.1 | 13.9 | 3.0, 72.2 | −11.8, 47.5 |
| n = 33 | Left | 13.2 ± 10.3 | 10.5 | 2.9, 48.5 | −7.0, 33.5 |
| Thyroid | 31.1 ± 19.8 | 26.2 | 5.9, 76.7 | −7.8, 70.0 | |
| physician US (mL) | Right | 16.7 ± 12.9 | 11.9 | 3.8, 65.7 | −8.7, 42.0 |
| n = 33 | Left | 12.0 ± 9.0 | 9.3 | 2.9, 46.1 | −5.7, 29.7 |
| Thyroid | 28.7 ± 17.6 | 22.6 | 6.8, 85.2 | −5.8, 63.2 | |
| MTA US (mL) | Right | 18.0 ± 18.5 | 10.8 | 4.2, 80.2 | −18.2, 54.2 |
| n = 33 | Left | 11.8 ± 7.5 | 9.1 | 2.6, 37.7 | −3.0, 26.5 |
| Thyroid | 29.8 ± 21.2 | 21.3 | 6.8, 93.8 | −11.8, 71.3 |
| Thyroid Nodules | Value | Physician US N = 72 | MTA US N = 68 |
|---|---|---|---|
| Volume | Mean ± SD | 2.9 ± 5.5 | 3.1 ± 4.4 |
| (mL) | Median | 1.3 | 1.2 |
| Range (Min, Max) | 0.1, 37.9 | 0.1, 24.7 | |
| LoA | −7.8, 13.6 | −5.7, 11.8 | |
| Largest diameter | Mean ± SD | 18 ± 9 | 19 ± 9 |
| (mm) | Median | 16 | 17 |
| Range (Min, Max) | 5, 49 | 5, 40 | |
| LoA | 0, 35 | 1, 36 | |
| Kwak-TIRADS [29] | 3 | 13/18.1 | 13/19.1 |
| (N/%) | 4A | 21/29.2 | 19/27.9 |
| 4B | 29/40.3 | 26/38.2 | |
| 4C(3) | 7/9.7 | 7/10.3 | |
| 4C(4) | 2/2.8 | 3/4.4 | |
| 5 | 0/0 | 0/0 |
| Consecutive TN Number | Largest Diameter | Physician US (Additional Feature) | MTA US (Additional Feature) |
|---|---|---|---|
| #4 | 11 mm | 4B | 4C(3) (taller-than-wide) |
| #8 | 38 mm | 4C(3) (microcalcifications) | 4B |
| #16 | 10 mm | 4B | 4C(3) (irregular margins) |
| #21 | 7 mm | N/A | 4C(4) |
| #23 | 18 mm | 4A | 4B (taller-than-wide) |
| #28 | 15 mm | 4B (microcalcifications) | 4A |
| #34 | 8 mm | 4A | N/A |
| #49 | 8 mm | 4B | N/A |
| #51 | 7 mm | 4A | N/A |
| #53 | 9 mm | 4B | N/A |
| #55 | 13 mm | 4A | 4B (taller-than-wide) |
| #58 | 7 mm | 4B | N/A |
| #60 | 17 mm | 4A | 4B (taller-than-wide) |
| #62 | 16 mm | 4B | 4C(3) (irregular margins) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seifert, P.; Maikowski, I.; Winkens, T.; Kühnel, C.; Gühne, F.; Drescher, R.; Freesmeyer, M. Ultrasound Cine Loop Standard Operating Procedure for Benign Thyroid Diseases—Evaluation of Non-Physician Application. Diagnostics 2021, 11, 67. https://doi.org/10.3390/diagnostics11010067
Seifert P, Maikowski I, Winkens T, Kühnel C, Gühne F, Drescher R, Freesmeyer M. Ultrasound Cine Loop Standard Operating Procedure for Benign Thyroid Diseases—Evaluation of Non-Physician Application. Diagnostics. 2021; 11(1):67. https://doi.org/10.3390/diagnostics11010067
Chicago/Turabian StyleSeifert, Philipp, Ivonne Maikowski, Thomas Winkens, Christian Kühnel, Falk Gühne, Robert Drescher, and Martin Freesmeyer. 2021. "Ultrasound Cine Loop Standard Operating Procedure for Benign Thyroid Diseases—Evaluation of Non-Physician Application" Diagnostics 11, no. 1: 67. https://doi.org/10.3390/diagnostics11010067
APA StyleSeifert, P., Maikowski, I., Winkens, T., Kühnel, C., Gühne, F., Drescher, R., & Freesmeyer, M. (2021). Ultrasound Cine Loop Standard Operating Procedure for Benign Thyroid Diseases—Evaluation of Non-Physician Application. Diagnostics, 11(1), 67. https://doi.org/10.3390/diagnostics11010067






