Computer-Assisted System in Stress Radiography for Anterior Cruciate Ligament Injury with Correspondent Evaluation of Relevant Diagnostic Factors
Abstract
1. Introduction
2. Materials and Methods
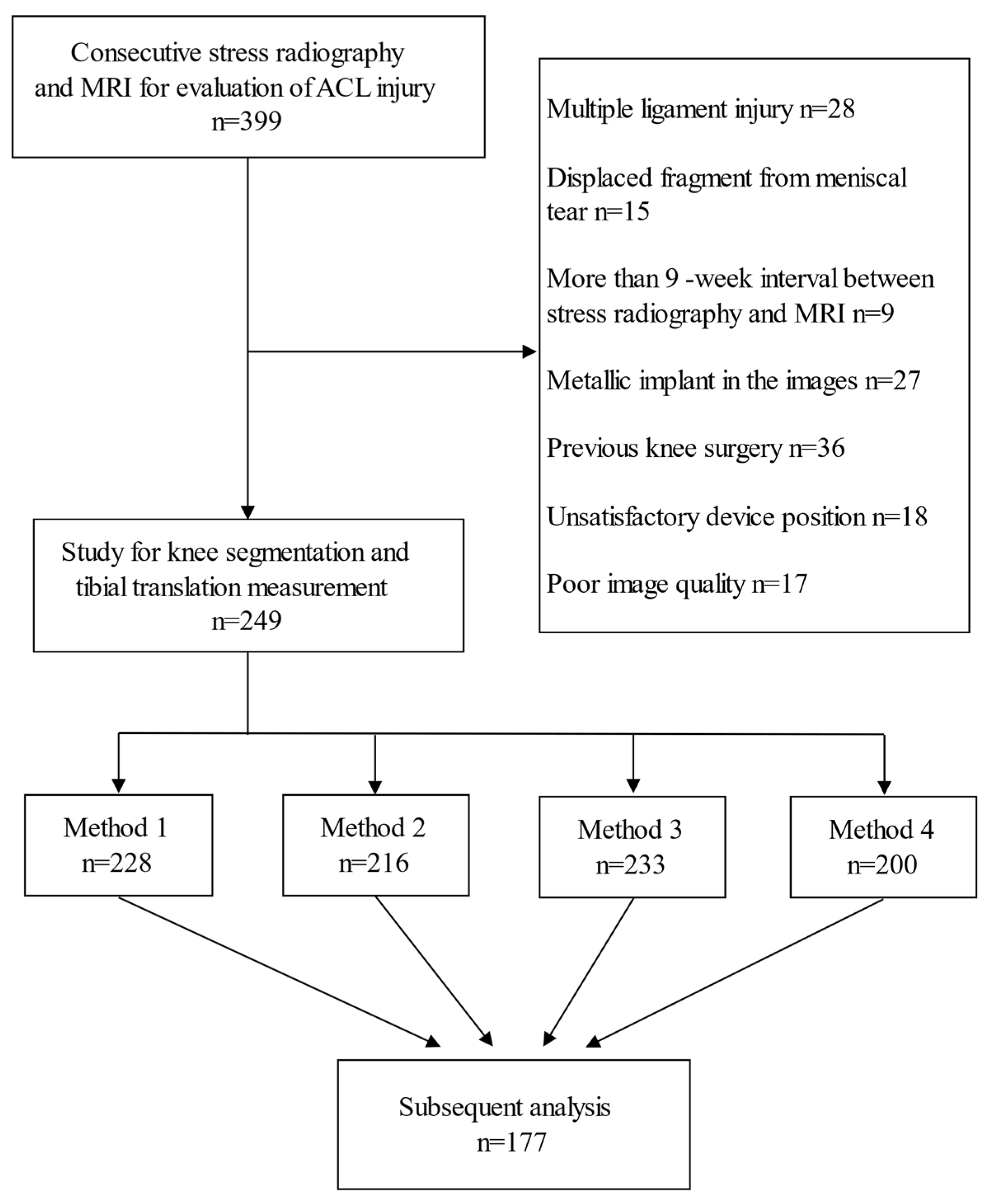
2.1. Patients
2.2. Knee Segmentation
2.3. Methods to Measure Tibial Translation
2.4. Measurements of Technical Factors
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- A Torzilli, P.; Greenberg, R.L.; Hood, R.W.; Pavlov, H.; Insall, J.N. Measurement of anterior-posterior motion of the knee in injured patients using a biomechanical stress technique. J. Bone Jt. Surg. Am. Vol. 1984, 66, 1438–1442. [Google Scholar] [CrossRef]
- Kim, H.K.; Laor, T.; Shire, N.J.; Bean, J.A.; Dardzinski, B.J. Anterior and Posterior Cruciate Ligaments at Different Patient Ages: MR Imaging Findings. Radiology 2008, 247, 826–835. [Google Scholar] [CrossRef]
- Leblanc, M.-C.; Kowalczuk, M.; Andruszkiewicz, N.; Simunovic, N.; Farrokhyar, F.; Turnbull, T.L.; Debski, R.E.; Ayeni, O.R. Diagnostic accuracy of physical examination for anterior knee instability: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2805–2813. [Google Scholar] [CrossRef] [PubMed]
- Beldame, J.; Bertiaux, S.; Roussignol, X.; Lefebvre, B.; Adam, J.-M.; Mouilhade, F.; Dujardin, F. Laxity measurements using stress radiography to assess anterior cruciate ligament tears. Orthop. Traumatol. Surg. Res. 2011, 97, 34–43. [Google Scholar] [CrossRef]
- Lerat, J.L.; Moyen, B.L.; Cladière, F.; Besse, J.L.; Abidi, H. Knee instability after injury to the anterior cruciate ligament. J. Bone Jt. Surg. Br. Vol. 2000, 82, 42–47. [Google Scholar] [CrossRef]
- Benvenuti, J.-F.; Vallotton, J.A.; Meystre, J.-L.; Leyvraz, P.F. Objective assessment of the anterior tibial translation in Lachman test position. Knee Surg. Sports Traumatol. Arthrosc. 1998, 6, 215–219. [Google Scholar] [CrossRef]
- Rijke, A.M.; Tegtmeyer, C.J.; Weiland, D.J.; McCue, F.C. Stress examination of the cruciate ligaments: A radiologic Lachman test. Radiology 1987, 165, 867–869. [Google Scholar] [CrossRef] [PubMed]
- Wirz, P.; Von Stokar, P.; Jakob, R.P. The effect of knee position on the reproducibility of measurements taken from stress films: A comparison of four measurement methods. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Park, Y.-B.; Kim, S.H. Diagnostic Value of Stress Radiography and Arthrometer Measurement for Anterior Instability in Anterior Cruciate Ligament Injured Knees at Different Knee Flexion Position. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 1721–1732. [Google Scholar] [CrossRef]
- Nakamura, K.; Koga, H.; Sekiya, I.; Watanabe, T.; Mochizuki, T.; Horie, M.; Nakamura, T.; Otabe, K.; Muneta, T. Evaluation of pivot shift phenomenon while awake and under anaesthesia by different manoeuvres using triaxial accelerometer. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2377–2383. [Google Scholar] [CrossRef]
- Lee, Y.S.; Han, S.H.; Jo, J.; Kwak, K.-S.; Nha, K.W.; Kim, J.H. Comparison of 5 Different Methods for Measuring Stress Radiographs to Improve Reproducibility During the Evaluation of Knee Instability. Am. J. Sports Med. 2011, 39, 1275–1281. [Google Scholar] [CrossRef]
- Takahashi, T.; Yamanaka, N.; Komatsu, M.; Ogawa, Y.; Yoshida, S.; Yamamoto, H. A new computer-assisted method for measuring the tibio-femoral angle in patients with osteoarthritis of the knee. Osteoarthr. Cartil. 2004, 12, 256–259. [Google Scholar] [CrossRef]
- Oka, H.; Muraki, S.; Akune, T.; Mabuchi, A.; Suzuki, T.; Yoshida, H.; Yamamoto, S.; Nakamura, K.; Yoshimura, N.; Kawaguchi, H. Fully automatic quantification of knee osteoarthritis severity on plain radiographs. Osteoarthr. Cartil. 2008, 16, 1300–1306. [Google Scholar] [CrossRef] [PubMed]
- Santosh, K.C.; Antani, S.; Guru, D.S.; Dey, N. Medical Imaging: Artificial Intelligence, Image Recognition, and Machine Learning Techniques, 1st ed.; CRC Press: Boca Raton, FL, USA, 2019. [Google Scholar]
- DeJour, D.; Ntagiopoulos, P.G.; Saggin, P.R.; Panisset, J.-C. The Diagnostic Value of Clinical Tests, Magnetic Resonance Imaging, and Instrumented Laxity in the Differentiation of Complete Versus Partial Anterior Cruciate Ligament Tears. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 491–499. [Google Scholar] [CrossRef]
- Seghers, D.; Loeckx, D.; Maes, F.; Vandermeulen, D.; Suetens, P. Minimal Shape and Intensity Cost Path Segmentation. IEEE Trans. Med. Imaging 2007, 26, 1115–1129. [Google Scholar] [CrossRef]
- Schulz, M.S.; Russe, K.; Lampakis, G.; Strobel, M.J. Reliability of Stress Radiography for Evaluation of Posterior Knee Laxity. Am. J. Sports Med. 2005, 33, 502–506. [Google Scholar] [CrossRef]
- Boks, S.S.; Vroegindeweij, D.; Koes, B.W.; Hunink, M.G.M.; Bierma-Zeinstra, S.M.A. Follow-up of Posttraumatic Ligamentous and Meniscal Knee Lesions Detected at MR Imaging: Systematic Review. Radiology 2006, 238, 863–871. [Google Scholar] [CrossRef]
- Fujimoto, E.; Sumen, Y.; Ochi, M.; Ikuta, Y. Spontaneous healing of acute anterior cruciate ligament (ACL) injuries-conservative treatment using an extension block soft brace without anterior stabilization. Arch. Orthop. Trauma Surg. 2002, 122, 212–216. [Google Scholar] [CrossRef]
- Ihara, H.; Miwa, M.; Deya, K.; Torisu, K. MRI of Anterior Cruciate Ligament Healing. J. Comput. Assist. Tomogr. 1996, 20, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Mae, T.; Shino, K.; Hiramatsu, K.; Tachibana, Y.; Nakagawa, S.; Yoshikawa, H. Anterior laxity of the knee assessed with gravity stress radiograph. Skelet. Radiol. 2018, 47, 1349–1355. [Google Scholar] [CrossRef]
- Yanagisawa, S.; Kimura, M.; Hagiwara, K.; Ogoshi, A.; Nakagawa, T.; Shiozawa, H.; Ohsawa, T. Factors affecting knee laxity following anterior cruciate ligament reconstruction using a hamstring tendon. Knee 2017, 24, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Beldame, J.; Mouchel, S.; Bertiaux, S.; Adam, J.-M.; Mouilhade, F.; Roussignol, X.; Dujardin, F. Anterior knee laxity measurement: Comparison of passive stress radiographs Telos® and “Lerat”, and GNRB® arthrometer. Orthop. Traumatol. Surg. Res. 2012, 98, 744–750. [Google Scholar] [CrossRef]
- Ahn, J.H.; Bae, T.S.; Kang, K.-S.; Kang, S.Y.; Lee, S.H. Longitudinal Tear of the Medial Meniscus Posterior Horn in the Anterior Cruciate Ligament–Deficient Knee Significantly Influences Anterior Stability. Am. J. Sports Med. 2011, 39, 2187–2193. [Google Scholar] [CrossRef]



| Parameter | Value |
|---|---|
| Mean age (y) | 28.4 ± 10.5 (16–68) |
| Male gender * | 144 (81.4) |
| Interval between stress view and MRI (d) | 20.44 ± 13.80 (0–61) |
| Flexion angle (°) on stress view | 38.47 ± 11.22 (11.88–63.86) |
| Intercondylar distance (mm) on stress view | 4.53 ± 3.61 (0–16.73) |
| Force-joint distance (mm) on stress view | 39.70 ± 11.74 (11.19–67.22) |
| Force-joint angle (°) on stress view | −10.58 ± 9.30 (−32.14–12.51) |
| Torn ACL on MRI * | 129 (72.9) |
| Sensitivity | Specificity | PPV | NPV | Accuracy | |
|---|---|---|---|---|---|
| percentage (95% confidence interval) | |||||
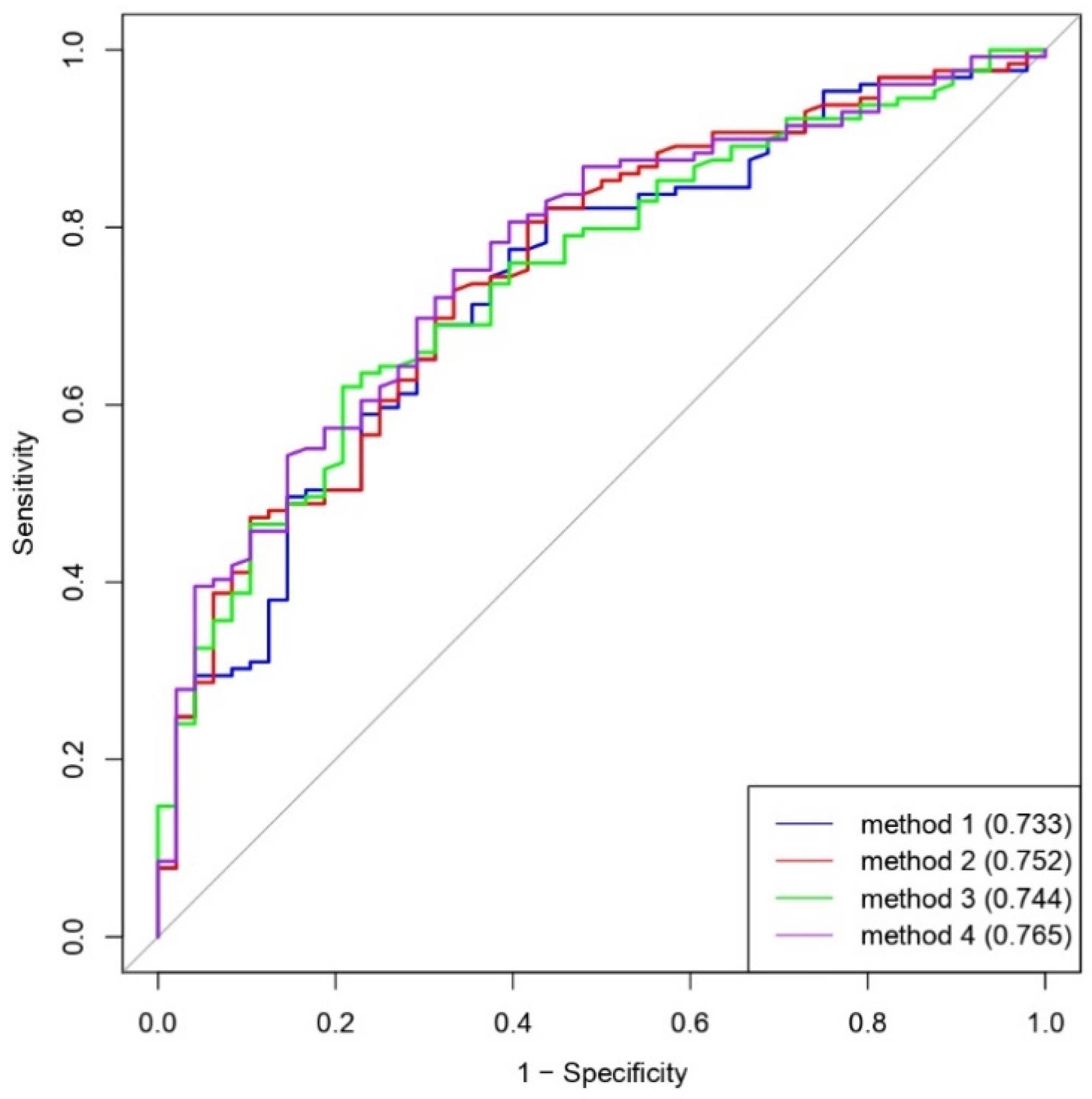
| Method 1 | 106/129, 82.2 (76.5–87.8) | 27/48, 56.3 (48.9–63.6) | 106/127, 83.5 (78.0–88.9) | 27/50, 54.0 (46.7–61.3) | 133/177, 75.1 (68.8–81.5) |
| Method 2 | 94/129, 72.9 (66.3–79.4) | 32/48, 66.7 (59.7–73.6) | 94/110, 85.5 (80.3–90.6) | 32/67, 47.8 (40.4–55.1) | 126/177, 71.2 (64.5–77.9) |
| Method 3 | 80/129, 62.0 (54.9–69.2) | 38/48, 79.2 (73.2–85.1) | 80/90, 88.9 (84.3–93.5) | 38/87, 43.7 (36.4–51.0) | 118/177, 66.7 (59.7–73.6) |
| Method 4 | 97/129, 75.2 (68.8–81.6) | 32/48, 66.7 (59.7–73.6) | 97/113, 85.8 (80.7–91.0) | 32/64, 50.0 (42.6–57.4) | 129/177, 72.9 (66.3–79.4) |
| Accurate Cases (TP + FN = 129) | Error Cases (FP + TN = 48) | Odds Ratio (95% CI) * | β Value † | p Value ‡ | |
|---|---|---|---|---|---|
| Age—y | 28.85 ± 10.68 | 27.29 ± 10.00 | 1.016 (0.983–1.054) | 0.015 | 0.380 |
| Male gender—no. (%) | 104 (80.62) | 40 (83.33) | 0.832 (0.328–1.930) | −0.184 | 0.681 |
| Interval between stress radiography and MRI—d | 19.08 ± 13.75 | 24.08 ± 13.39 | 0.975 (0.952–0.998) | −0.025 | 0.035 |
| Flexion angle on stress view—° | 37.82 ± 11.36 | 40.24 ± 10.74 | 0.980 (0.951–1.010) | −0.020 | 0.201 |
| Intercondylar distance on stress view—mm | 4.54 ± 3.68 | 4.52 ± 3.46 | 1.000 (0.915–1.101) | 0.002 | 0.971 |
| Force-joint distance on stress view—mm | 38.53 ± 11.48 | 42.84 ± 11.96 | 0.968 (0.938–0.996) | −0.033 | 0.032 |
| Force-joint angle on stress view—° | −10.31 ± 9.28 | −11.05 ± 9.50 | 1.009 (0.973–1.047) | 0.009 | 0.637 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, C.-K.; Lin, L.-C.; Sun, Y.-N.; Lai, C.-S.; Chen, C.-H.; Kao, C.-Y. Computer-Assisted System in Stress Radiography for Anterior Cruciate Ligament Injury with Correspondent Evaluation of Relevant Diagnostic Factors. Diagnostics 2021, 11, 419. https://doi.org/10.3390/diagnostics11030419
Wang C-K, Lin L-C, Sun Y-N, Lai C-S, Chen C-H, Kao C-Y. Computer-Assisted System in Stress Radiography for Anterior Cruciate Ligament Injury with Correspondent Evaluation of Relevant Diagnostic Factors. Diagnostics. 2021; 11(3):419. https://doi.org/10.3390/diagnostics11030419
Chicago/Turabian StyleWang, Chien-Kuo, Liang-Ching Lin, Yung-Nien Sun, Cheng-Shih Lai, Chia-Hui Chen, and Cheng-Yi Kao. 2021. "Computer-Assisted System in Stress Radiography for Anterior Cruciate Ligament Injury with Correspondent Evaluation of Relevant Diagnostic Factors" Diagnostics 11, no. 3: 419. https://doi.org/10.3390/diagnostics11030419
APA StyleWang, C.-K., Lin, L.-C., Sun, Y.-N., Lai, C.-S., Chen, C.-H., & Kao, C.-Y. (2021). Computer-Assisted System in Stress Radiography for Anterior Cruciate Ligament Injury with Correspondent Evaluation of Relevant Diagnostic Factors. Diagnostics, 11(3), 419. https://doi.org/10.3390/diagnostics11030419







