Risk Assessment of Endometrial Hyperplasia or Endometrial Cancer with Simplified Ultrasound-Based Scoring Systems
Abstract
1. Introduction
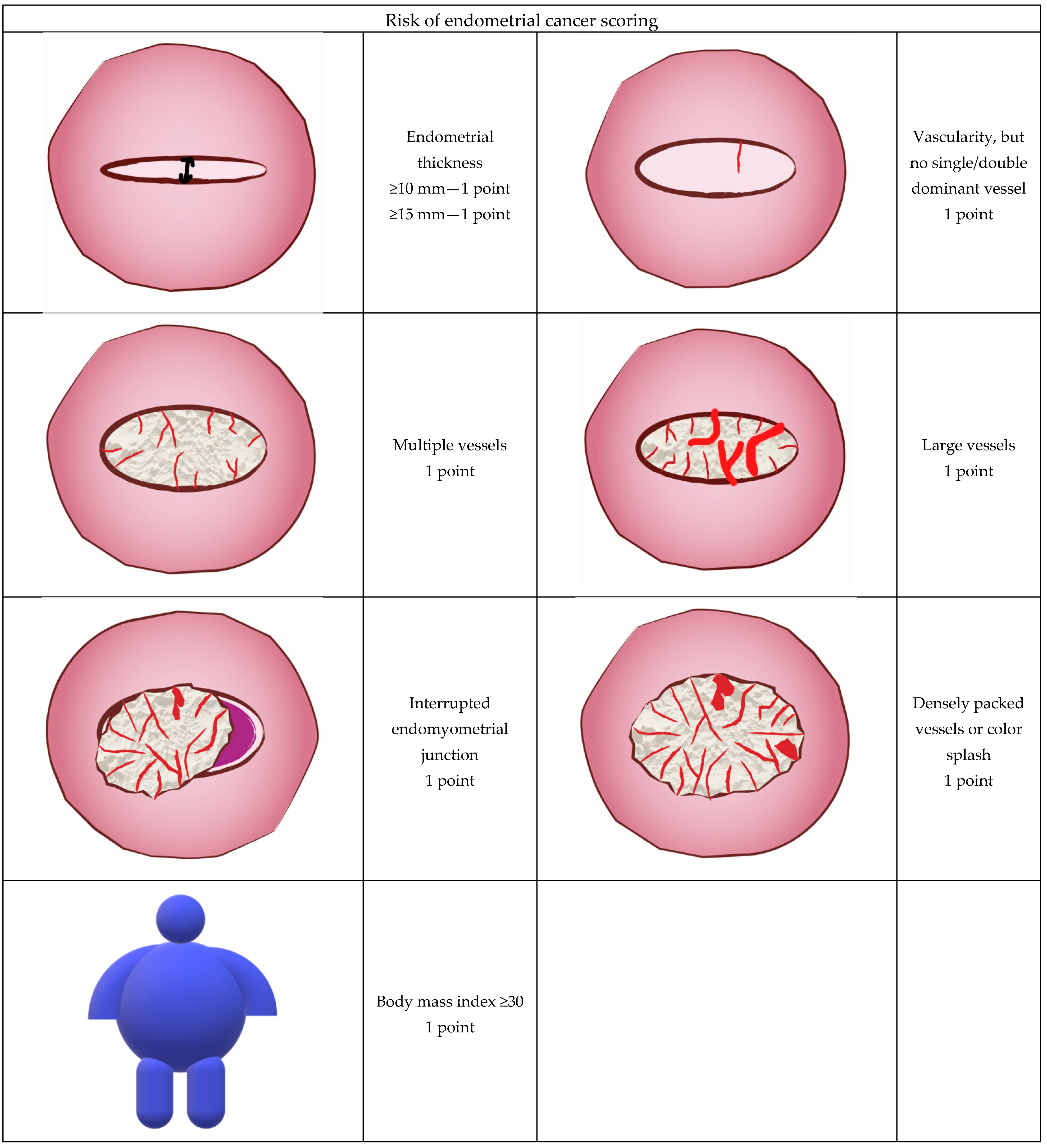
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Munro, M.G.; Critchley, H.; Fraser, I.S. Research and clinical management for women with abnormal uterine bleeding in the reproductive years: More than PALM-COEIN. BJOG 2017, 124, 185–189. [Google Scholar] [CrossRef]
- Munro, M.G.; Critchley, H.O.; Broder, M.S.; Fraser, I.S.; FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int. J. Gynaecol. Obstet. 2011, 113, 3–13. [Google Scholar] [CrossRef]
- Munro, M.G.; Southern California Permanente Medical Group’s Abnormal Uterine Bleeding Working Group. Investigation of women with postmenopausal uterine bleeding: Clinical practice recommendations. Perm. J. 2014, 18, 55–70. [Google Scholar] [CrossRef][Green Version]
- Giampaolino, P.; Della Corte, L.; Di Filippo, C.; Mercorio, A.; Vitale, S.G.; Bifulco, G. Office hysteroscopy in the management of women with postmenopausal bleeding. Climacteric 2020, 23, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Zalewski, K.; Rzepka, J.; Madry, R.; Danska-Bidzinska, A.; Bidzinski, M. Analysis of risk factors for recurrence after treatment of endometrial uterine cancer. Ginekol. Pol. 2009, 80, 687–693. [Google Scholar] [PubMed]
- Burbos, N.; Musonda, P.; Giarenis, I.; Shiner, A.M.; Giamougiannis, P.; Morris, E.P.; Nieto, J.J. Predicting the risk of endometrial cancer in postmenopausal women presenting with vaginal bleeding: The Norwich DEFAB risk assessment tool. Br. J. Cancer 2010, 102, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Alcazar, J.L.; Castillo, G.; Minguez, J.A.; Galan, M.J. Endometrial blood flow mapping using transvaginal power Doppler sonography in women with postmenopausal bleeding and thickened endometrium. Ultrasound Obstet. Gynecol. 2003, 21, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Falcone, F.; Balbi, G.; Di Martino, L.; Grauso, F.; Salzillo, M.E.; Messalli, E.M. Surgical management of early endometrial cancer: An update and proposal of a therapeutic algorithm. Med. Sci. Monit. 2014, 20, 1298–1313. [Google Scholar] [CrossRef] [PubMed]
- Du, J.; Li, Y.; Lv, S.; Wang, Q.; Sun, C.; Dong, X.; He, M.; Ulain, Q.; Yuan, Y.; Tuo, X.; et al. Endometrial sampling devices for early diagnosis of endometrial lesions. J. Cancer Res. Clin. Oncol. 2016, 142, 2515–2522. [Google Scholar] [CrossRef] [PubMed]
- Szubert, S.; Szpurek, D.; Wojtowicz, A.; Zywica, P.; Stukan, M.; Sajdak, S.; Jablonski, S.; Wicherek, L.; Moszynski, R. Performance of selected models for predicting malignancy in ovarian tumors in relation to the degree of diagnostic uncertainty by subjective assessment with ultrasound. J. Ultrasound. Med. 2020, 39, 939–947. [Google Scholar] [CrossRef]
- Gull, B.; Karlsson, B.; Milsom, I.; Granberg, S. Can ultrasound replace dilation and curettage? A longitudinal evaluation of postmenopausal bleeding and transvaginal sonographic measurement of the endometrium as predictors of endometrial cancer. Am. J. Obstet. Gynecol. 2003, 188, 401–408. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 734: The Role of Transvaginal Ultrasonography in Evaluating the Endometrium of Women with Postmenopausal Bleeding. Obstet. Gynecol. 2018, 131, e124–e129. [Google Scholar] [CrossRef]
- Wong, A.S.; Lao, T.T.; Cheung, C.W.; Yeung, S.W.; Fan, H.L.; Ng, P.S.; Yuen, P.M.; Sahota, D.S. Reappraisal of endometrial thickness for the detection of endometrial cancer in postmenopausal bleeding: A retrospective cohort study. BJOG 2016, 123, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Vetter, M.H.; Smith, B.; Benedict, J.; Hade, E.M.; Bixel, K.; Copeland, L.J.; Cohn, D.E.; Fowler, J.M.; O’Malley, D.; Salani, R.; et al. Preoperative predictors of endometrial cancer at time of hysterectomy for endometrial intraepithelial neoplasia or complex atypical hyperplasia. Am. J. Obstet. Gynecol. 2020, 222, 60.e61–60.e67. [Google Scholar] [CrossRef] [PubMed]
- Pirog, M.; Kacalska-Janssen, O.; Bereza, T.; Jach, R. The thin red line—postmenopausal abnormal uterine bleeding with endometrial thickness less than 4 mm. Contemp. Oncol. 2019, 23, 43–46. [Google Scholar] [CrossRef]
- Pennant, M.E.; Mehta, R.; Moody, P.; Hackett, G.; Prentice, A.; Sharp, S.J.; Lakshman, R. Premenopausal abnormal uterine bleeding and risk of endometrial cancer. BJOG 2017, 124, 404–411. [Google Scholar] [CrossRef]
- Dubinsky, T.J. Color Doppler imaging improves specificity of diagnosis in women with thickened endometrium on transvaginal ultrasonography. Am. J. Obstet. Gynecol. 1995, 172, 1645–1647. [Google Scholar] [CrossRef]
- Epstein, E.; Van Holsbeke, C.; Mascilini, F.; Masback, A.; Kannisto, P.; Ameye, L.; Fischerova, D.; Zannoni, G.; Vellone, V.; Timmerman, D.; et al. Gray-scale and color Doppler ultrasound characteristics of endometrial cancer in relation to stage, grade and tumor size. Ultrasound Obstet. Gynecol. 2011, 38, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Scioscia, M.; Noventa, M.; Lagana, A.S. Abnormal uterine bleeding and the risk of endometrial cancer: Can subendometrial vascular ultrasound be of help to discriminate cancer from adenomyosis? Am. J. Obstet. Gynecol. 2020, 223, 605–606. [Google Scholar] [CrossRef] [PubMed]
- Stachowicz, N.; Czekierdowski, A.; Danilos, J.; Kotarski, J. Three dimensional sonography in the endometrial volume measurement in women with perimenopausal irregular uterine bleeding. Ginekol. Pol. 2002, 73, 970–975. [Google Scholar]
- Stachowicz, N.; Czekierdowski, A.; Danilos, J.; Smolen, A.; Kotarski, J. Three-dimensional sonoangiography in diagnostic of endometrial hyperplasia and carcinoma. An assessment of vascularization indices and endometrial volume. Przegl. Lek. 2005, 62, 827–829. [Google Scholar]
- Odeh, M.; Vainerovsky, I.; Grinin, V.; Kais, M.; Ophir, E.; Bornstein, J. Three-dimensional endometrial volume and 3-dimensional power Doppler analysis in predicting endometrial carcinoma and hyperplasia. Gynecol. Oncol. 2007, 106, 348–353. [Google Scholar] [CrossRef]
- Galvan, R.; Merce, L.; Jurado, M.; Minguez, J.A.; Lopez-Garcia, G.; Alcazar, J.L. Three-dimensional power Doppler angiography in endometrial cancer: Correlation with tumor characteristics. Ultrasound Obstet. Gynecol. 2010, 35, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Green, R.W.; Valentin, L.; Alcazar, J.L.; Chiappa, V.; Erdodi, B.; Franchi, D.; Fruhauf, F.; Fruscio, R.; Guerriero, S.; Graupera, B.; et al. Endometrial cancer off-line staging using two-dimensional transvaginal ultrasound and three-dimensional volume contrast imaging: Intermethod agreement, interrater reliability and diagnostic accuracy. Gynecol. Oncol. 2018, 150, 438–445. [Google Scholar] [CrossRef]
- Leone, F.P.; Timmerman, D.; Bourne, T.; Valentin, L.; Epstein, E.; Goldstein, S.R.; Marret, H.; Parsons, A.K.; Gull, B.; Istre, O.; et al. Terms, definitions and measurements to describe the sonographic features of the endometrium and intrauterine lesions: A consensus opinion from the International Endometrial Tumor Analysis (IETA) group. Ultrasound Obstet. Gynecol. 2010, 35, 103–112. [Google Scholar] [CrossRef]
- Sladkevicius, P.; Installe, A.; Van Den Bosch, T.; Timmerman, D.; Benacerraf, B.; Jokubkiene, L.; Di Legge, A.; Votino, A.; Zannoni, L.; De Moor, B.; et al. International Endometrial Tumor Analysis (IETA) terminology in women with postmenopausal bleeding and sonographic endometrial thickness >/= 4.5 mm: Agreement and reliability study. Ultrasound Obstet. Gynecol. 2018, 51, 259–268. [Google Scholar] [CrossRef]
- Epstein, E.; Fischerova, D.; Valentin, L.; Testa, A.C.; Franchi, D.; Sladkevicius, P.; Fruhauf, F.; Lindqvist, P.G.; Mascilini, F.; Fruscio, R.; et al. Ultrasound characteristics of endometrial cancer as defined by International Endometrial Tumor Analysis (IETA) consensus nomenclature: Prospective multicenter study. Ultrasound Obstet. Gynecol. 2018, 51, 818–828. [Google Scholar] [CrossRef] [PubMed]
- Verbakel, J.Y.; Mascilini, F.; Wynants, L.; Fischerova, D.; Testa, A.C.; Franchi, D.; Fruhauf, F.; Cibula, D.; Lindqvist, P.G.; Fruscio, R.; et al. Validation of ultrasound strategies to assess tumor extension and to predict high-risk endometrial cancer in women from the prospective IETA (International Endometrial Tumor Analysis)-4 cohort. Ultrasound Obstet. Gynecol. 2020, 55, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Dueholm, M.; Moller, C.; Rydbjerg, S.; Hansen, E.S.; Ortoft, G. An ultrasound algorithm for identification of endometrial cancer. Ultrasound Obstet. Gynecol. 2014, 43, 557–568. [Google Scholar] [CrossRef]
- Dueholm, M.; Hjorth, I.M. Structured imaging technique in the gynecologic office for the diagnosis of abnormal uterine bleeding. Best Pract. Res. Clin. Obstet. Gynaecol. 2017, 40, 23–43. [Google Scholar] [CrossRef]
- Dueholm, M.; Hjorth, I.M.D.; Dahl, K.; Pedersen, L.K.; Ortoft, G. Identification of endometrial cancers and atypical hyperplasia: Development and validation of a simplified system for ultrasound scoring of endometrial pattern. Maturitas 2019, 123, 15–24. [Google Scholar] [CrossRef]
- Guralp, O.; Kushner, D.M. Iatrogenic transtubal spill of endometrial cancer: Risk or myth. Arch. Gynecol. Obstet. 2011, 284, 1209–1221. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.N.; Zhang, Y.; Wang, Y.J.; Wang, L.P.; Duan, H. Effect of hysteroscopy on the peritoneal dissemination of endometrial cancer cells: A meta-analysis. Fertil. Steril. 2011, 96, 957–961. [Google Scholar] [CrossRef]
- Opolskiene, G.; Sladkevicius, P.; Valentin, L. Ultrasound assessment of endometrial morphology and vascularity to predict endometrial malignancy in women with postmenopausal bleeding and sonographic endometrial thickness >or= 4.5 mm. Ultrasound Obstet. Gynecol. 2007, 30, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Van Hanegem, N.; Breijer, M.C.; Khan, K.S.; Clark, T.J.; Burger, M.P.; Mol, B.W.; Timmermans, A. Diagnostic evaluation of the endometrium in postmenopausal bleeding: An evidence-based approach. Maturitas 2011, 68, 155–164. [Google Scholar] [CrossRef]
- Van Hanegem, N.; Prins, M.M.; Bongers, M.Y.; Opmeer, B.C.; Sahota, D.S.; Mol, B.W.; Timmermans, A. The accuracy of endometrial sampling in women with postmenopausal bleeding: A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod Biol. 2016, 197, 147–155. [Google Scholar] [CrossRef]
- Huang, Z.; Zheng, Y.; Wen, W.; Wu, C.; Bao, P.; Wang, C.; Zhong, W.; Gao, Y.T.; Jin, F.; Xiang, Y.B.; et al. Incidence and mortality of gynaecological cancers: Secular trends in urban Shanghai, China over 40 years. Eur. J. Cancer 2016, 63, 1–10. [Google Scholar] [CrossRef]
- Akhtar-Danesh, N.; Lytwyn, A.; Elit, L. Five-year trends in mortality indices among gynecological cancer patients in Canada. Gynecol. Oncol. 2012, 127, 620–624. [Google Scholar] [CrossRef]
- Haldorsen, I.S.; Salvesen, H.B. What is the best preoperative imaging for endometrial cancer? Curr. Oncol. Rep. 2016, 18, 25. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, S.R.; Nachtigall, M.; Snyder, J.R.; Nachtigall, L. Endometrial assessment by vaginal ultrasonography before endometrial sampling in patients with postmenopausal bleeding. Am. J. Obstet. Gynecol. 1990, 163, 119–123. [Google Scholar] [CrossRef]
- Osmers, R.; Volksen, M.; Schauer, A. Vaginosonography for early detection of endometrial carcinoma? Lancet 1990, 335, 1569–1571. [Google Scholar] [CrossRef]
- Karlsson, B.; Granberg, S.; Wikland, M.; Ylostalo, P.; Torvid, K.; Marsal, K.; Valentin, L. Transvaginal ultrasonography of the endometrium in women with postmenopausal bleeding--a Nordic multicenter study. Am. J. Obstet. Gynecol. 1995, 172, 1488–1494. [Google Scholar] [CrossRef]
- Goldstein, S.R. Appropriate evaluation of postmenopausal bleeding. Menopause 2018, 25, 1476–1478. [Google Scholar] [CrossRef]
- Clarke, M.A.; Long, B.J.; Del Mar Morillo, A.; Arbyn, M.; Bakkum-Gamez, J.N.; Wentzensen, N. Association of endometrial cancer risk with postmenopausal bleeding in women: A systematic review and meta-analysis. JAMA Intern. Med. 2018, 178, 1210–1222. [Google Scholar] [CrossRef]
- Clarke, M.A.; Long, B.J.; Sherman, M.E.; Lemens, M.A.; Podratz, K.C.; Hopkins, M.R.; Ahlberg, L.J.; Mc Guire, L.J.; Laughlin-Tommaso, S.K.; Bakkum-Gamez, J.N.; et al. Risk assessment of endometrial cancer and endometrial intraepithelial neoplasia in women with abnormal bleeding and implications for clinical management algorithms. Am. J. Obstet. Gynecol. 2020. [Google Scholar] [CrossRef]
- Chiofalo, B.; Mazzon, I.; Di Angelo Antonio, S.; Amadore, D.; Vizza, E.; Lagana, A.S.; Vocaturo, G.; Calagna, G.; Favilli, A.; Palmara, V.; et al. Hysteroscopic evaluation of endometrial changes in breast cancer women with or without hormone therapies: Results from a large multicenter cohort study. J. Minim. Invasive Gynecol. 2020, 27, 832–839. [Google Scholar] [CrossRef]
- Hefler, L.; Lemach, A.; Seebacher, V.; Polterauer, S.; Tempfer, C.; Reinthaller, A. The intraoperative complication rate of nonobstetric dilation and curettage. Obstet. Gynecol. 2009, 113, 1268–1271. [Google Scholar] [CrossRef]
- Carugno, J.; Marbin, S.; Lagana, A.S.; Vitale, S.G.; Alonso, L.; Di Spiezio Sardo, A.; Haimovich, S. New development on hysteroscopy for endometrial cancer diagnosis: State of the art. Minerva Med. 2021. [Google Scholar] [CrossRef]
- Kolhe, S. Management of abnormal uterine bleeding—Focus on ambulatory hysteroscopy. Int. J. Womens Health 2018, 10, 127–136. [Google Scholar] [CrossRef]

| Age (years) | 60.3 ± 10.7 |
| BMI (kg/m2) | 30.4 ± 6.0 |
| BMI (kg/m2) ≥ 30 kg/m2 (n) | 180 [46%] |
| Menopausal status | |
| Postmenopausal (n) | 289 [73.4%] |
| Premenopausal (n) | 105 [26.6%] |
| n | % | |
|---|---|---|
| All patients | 394 | 100 |
| Hyperplasia without atypia (SH) | 103 | 26.1 |
| Atypical hyperplasia (AH) | 55 | 14 |
| Endometrial Cancer (EC) | 236 | 59.9 |
| Endometrioid EC (EEC) | 216 | 54.8 |
| Non-endometrioid EC (NEC) | 20 | 5.1 |
| Stage 1 | 152 | 38.57 |
| Stage 2 | 47 | 11.93 |
| Stage 3 | 30 | 7.61 |
| Stage 4 | 7 | 1.77 |
| ET ≥ 8 mm | 332 | 84.26 |
| EC or AH in women with ET ≥ 8 mm (% of total number of EC/AH) | 263 | 90.37 |
| n | AUC (95% CI) | Sensitivity (%) | Specificity (%) | Accuracy (%) | LR+ | LR− | |
|---|---|---|---|---|---|---|---|
| BMI | 394 | 59 (53–69) | |||||
| BMI ≥ 30 | 180 | 58 (52–64) | 52 | 65 | 57 | 1.47 | 0.75 |
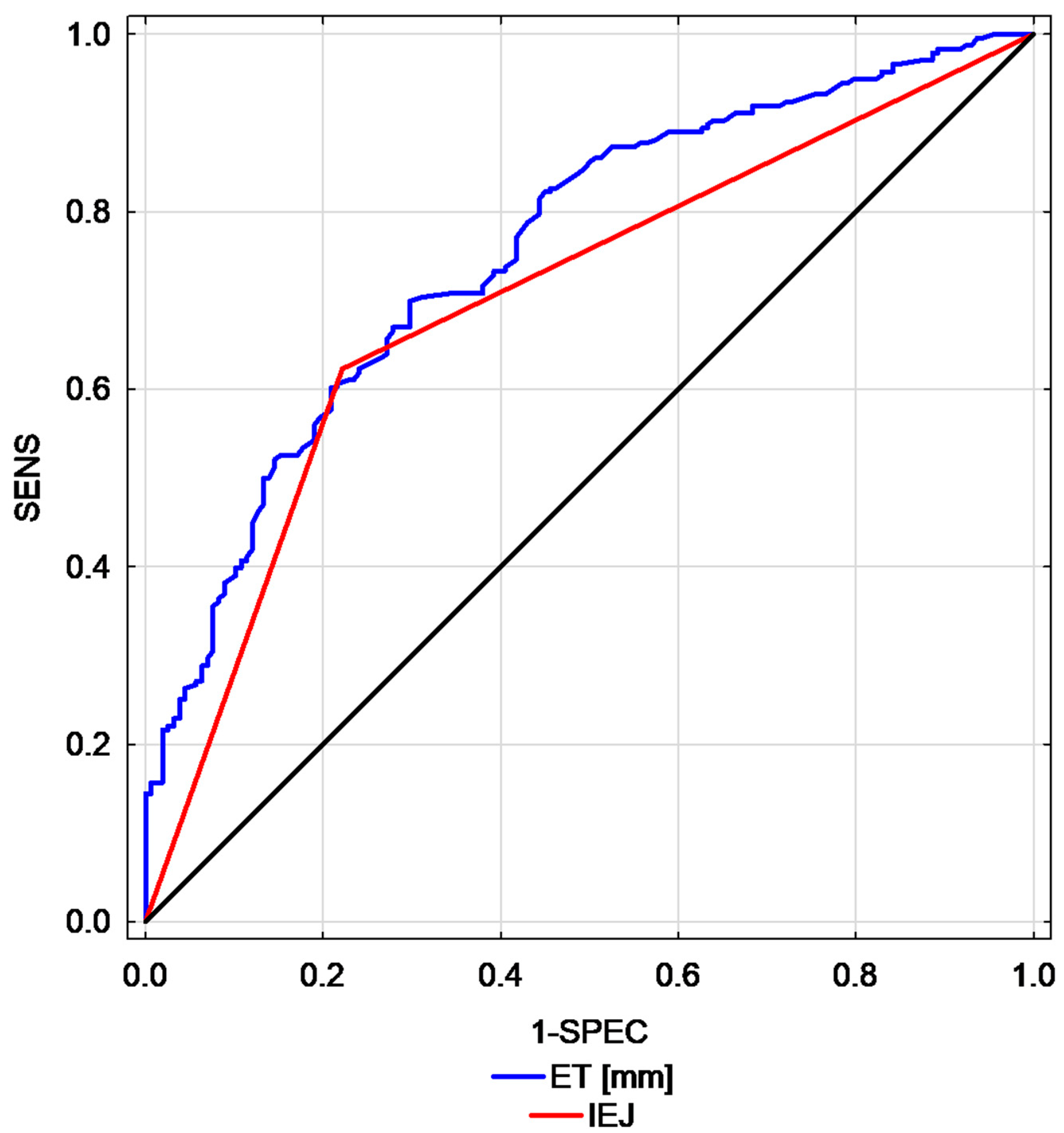
| Endometrial thickness | 394 | 76 (71–81) | |||||
| Endometrial thickness ≥8 | 332 | 60 (54–66) | 92 | 28 | 67 | 1.28 | 0.27 |
| Endometrial thickness ≥10 | 299 | 65 (60–71) | 88 | 42 | 70 | 1.53 | 0.28 |
| Endometrial thickness ≥15 | 221 | 68 (63–74) | 71 | 66 | 69 | 2.07 | 0.44 |
| Heterogenic endometrium | 350 | 54 (48–60) | 14 | 94 | 46 | 2.28 | 0.91 |
| Cystic endometrium | 67 | 55 (49–60) | 21 | 89 | 48 | 1.82 | 0.89 |
| Interrupted endomyometrial junction (IEJ) | 182 | 70 (65–75) | 62 | 78 | 69 | 2.81 | 0.48 |
| Vascularity, and more than one single or double dominant vessel (a) | 208 | 53 (48–59) | 56 | 51 | 54 | 1.14 | 0.87 |
| Multiple endometrial vessels (b) | 110 | 61 (56–67) | 37 | 85 | 56 | 2.53 | 0.74 |
| Large endometrial vessels (c) | 17 | 51 (45–57) | 5 | 97 | 42 | 1.61 | 0.98 |
| Densely packed or color splash | 25 | 54 (48–59) | 9 | 98 | 45 | 4.91 | 0.92 |
| Doppler score (a + b + c) | 394 | 58 (53–64) | |||||
| Doppler score (a + b + c) ≥ 1 | 209 | 54 (48–59) | 56 | 51 | 54 | 1.15 | 0.86 |
| Doppler score (a + b + c) ≥ 2 | 115 | 60 (55–66) | 37 | 83 | 56 | 2.18 | 0.76 |
| n = 394 | AUC (95% CI) | Sensitivity (%) | Specificity (%) | Accuracy (%) | LR+ | LR− |
|---|---|---|---|---|---|---|
| Score A | 68 (62–73) | 72 | 71 | 72 | 2.47 | 0.40 |
| REC | 75 (70–79) | 79 | 61 | 72 | 2.02 | 0.34 |
| Basic Model [29] ET, Doppler score, IEJ | 77 (73–82) | 78 | 70 | 75 | 2.58 | 0.31 |
| Model A [31] Doppler score, IEJ | 71 (66–76) | 72 | 70 | 71 | 2.36 | 0.41 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stachowicz, N.; Smoleń, A.; Ciebiera, M.; Łoziński, T.; Poziemski, P.; Borowski, D.; Czekierdowski, A. Risk Assessment of Endometrial Hyperplasia or Endometrial Cancer with Simplified Ultrasound-Based Scoring Systems. Diagnostics 2021, 11, 442. https://doi.org/10.3390/diagnostics11030442
Stachowicz N, Smoleń A, Ciebiera M, Łoziński T, Poziemski P, Borowski D, Czekierdowski A. Risk Assessment of Endometrial Hyperplasia or Endometrial Cancer with Simplified Ultrasound-Based Scoring Systems. Diagnostics. 2021; 11(3):442. https://doi.org/10.3390/diagnostics11030442
Chicago/Turabian StyleStachowicz, Norbert, Agata Smoleń, Michał Ciebiera, Tomasz Łoziński, Paweł Poziemski, Dariusz Borowski, and Artur Czekierdowski. 2021. "Risk Assessment of Endometrial Hyperplasia or Endometrial Cancer with Simplified Ultrasound-Based Scoring Systems" Diagnostics 11, no. 3: 442. https://doi.org/10.3390/diagnostics11030442
APA StyleStachowicz, N., Smoleń, A., Ciebiera, M., Łoziński, T., Poziemski, P., Borowski, D., & Czekierdowski, A. (2021). Risk Assessment of Endometrial Hyperplasia or Endometrial Cancer with Simplified Ultrasound-Based Scoring Systems. Diagnostics, 11(3), 442. https://doi.org/10.3390/diagnostics11030442






