Reliability of Sonography Measures of the Lumbar Multifidus and Transversus Abdominis during Static and Dynamic Activities in Subjects with Non-Specific Chronic Low Back Pain
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
- Before entering to the center, shoes were disinfected by stepping on a mat soaked in hydrogen peroxide.
- Then, the patient was given a temperature measurement with a digital thermometer, and hydroalcoholic gel was applied to the hands.
- The use of surgical mask by the patient and FFP2 mask and face shield by the physiotherapist, in addition to a disposable gown, was mandatory.
- Not having symptoms or having been in contact with people suspected of being with the current disease was verbally expressed.
- During treatment, the stretcher, chair, ultrasound probe, and gloves were disinfected.
- A safe distance was always maintained except during treatment.
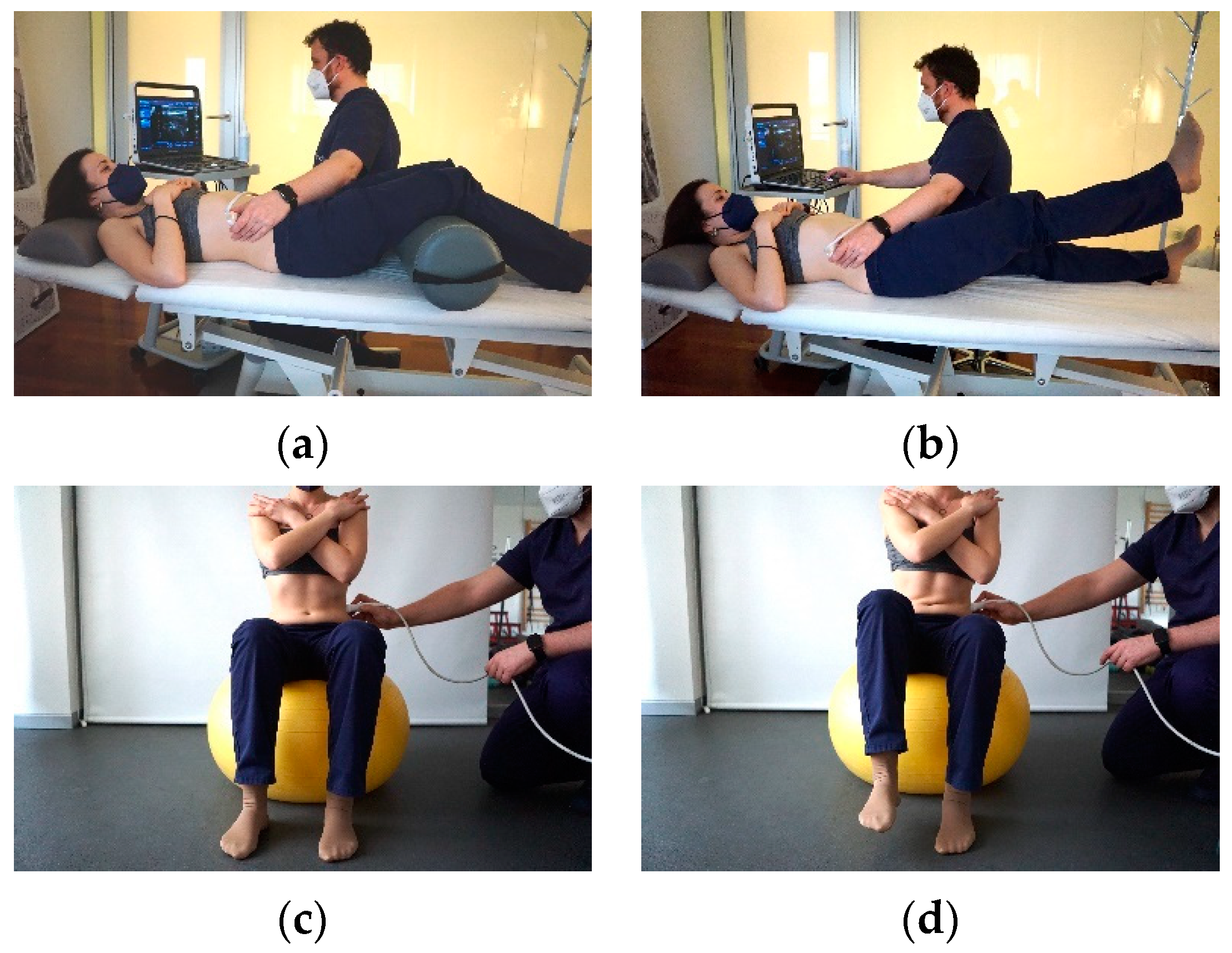
2.3. Sonographic Assessment of the LM and TA
2.4. Image Analysis
2.5. Procedure
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Data of Participants
3.2. Variation of the US and CR Parameters
3.3. Test-Retest Reliability
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Balague, F.; Mannion, A.F.; Pellise, F.; Cedraschi, C. Non-specific low back pain. Lancet 2012, 379, 482–491. [Google Scholar] [CrossRef]
- O’Sullivan, P. Diagnosis and classification of chronic low back pain disorders: Maladaptive movement and motor control impairments as underlying mechanism. Man. Ther. 2005, 10, 242–255. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Imperio, G.; Villafañe, J.H.; Negrini, F.; Zaina, F. Systematic reviews of physical and rehabilitation medicine Cochrane contents. Part 1. Disabilities due to spinal disorders and pain syndromes in adults. Eur. J. Phys. Rehabil. Med. 2013, 49, 597–609. [Google Scholar] [PubMed]
- Graven-Nielsen, T.; Arendt-Nielsen, L. Assessment of mechanisms in localized and widespread musculoskeletal pain. Nat. Rev. Rheumatol. 2010, 6, 599–606. [Google Scholar] [CrossRef]
- Pak, D.J.; Yong, R.J.; Kaye, A.D.; Urman, R.D. Chronification of Pain: Mechanisms, Current Understanding, and Clinical Implications. Curr. Pain Headache Rep. 2018, 22, 9. [Google Scholar] [CrossRef] [PubMed]
- Ji, R.R.; Nackley, A.; Huh, Y.; Terrando, N.; Maixner, W. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology 2018, 129, 343–366. [Google Scholar] [CrossRef] [PubMed]
- Villafane, J.H.; Zanetti, L.; Isgro, M.; Cleland, J.A.; Bertozzi, L.; Gobbo, M.; Negrini, S. Methods for the assessment of neuromotor capacity in non-specific low back pain: Validity and applicability in everyday clinical practice. J. Back Musculoskelet. Rehabil. 2015, 28, 201–214. [Google Scholar] [CrossRef]
- Ferreira, P.H.; Ferreira, M.L.; Hodges, P.W. Changes in recruitment of the abdominal muscles in people with low back pain: Ultrasound measurement of muscle activity. Spine 2004, 29, 2560–2566. [Google Scholar] [CrossRef]
- Pillastrini, P.; Ferrari, S.; Rattin, S.; Cupello, A.; Villafane, J.H.; Vanti, C. Exercise and tropism of the multifidus muscle in low back pain: A short review. J. Phys. Ther. Sci. 2015, 27, 943–945. [Google Scholar] [CrossRef]
- Morales, C.R.; Polo, J.A.; Sanz, D.R.; Lopez, D.L.; Gonzalez, S.V.; Buria, J.L.A.; Lobo, C.C. Ultrasonography features of abdominal perimuscular connective tissue in elite and amateur basketball players: An observational study. Rev. Assoc. Med. Bras. 2018, 64, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Kliziene, I.; Sipaviciene, S.; Klizas, S.; Imbrasiene, D. Effects of core stability exercises on multifidus muscles in healthy women and women with chronic low-back pain. J. Back Musculoskelet. Rehabil. 2015, 28, 841–847. [Google Scholar] [CrossRef] [PubMed]
- Wallwork, T.L.; Stanton, W.R.; Freke, M.; Hides, J.A. The effect of chronic low back pain on size and contraction of the lumbar multifidus muscle. Man. Ther. 2009, 14, 496–500. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P.B.; Mitchell, T.; Bulich, P.; Waller, R.; Holte, J. The relationship beween posture and back muscle endurance in industrial workers with flexion-related low back pain. Man. Ther. 2006, 11, 264–271. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P.; Dankaerts, W.; Burnett, A.; Farrell, G.; Jefford, E.; Naylor, C. The effect different ‘upright’sitting postures have on trunk muscle activation in pain-free subjects. Physiotherapy 2007, 93, S96. [Google Scholar]
- Kiesel, K.B.; Uhl, T.L.; Underwood, F.B.; Rodd, D.W.; Nitz, A.J. Measurement of lumbar multifidus muscle contraction with rehabilitative ultrasound imaging. Man. Ther. 2007, 12, 161–166. [Google Scholar] [CrossRef]
- Stokes, I.A.; Henry, S.M.; Single, R.M. Surface EMG electrodes do not accurately record from lumbar multifidus muscles. Clin. Biomech. 2003, 18, 9–13. [Google Scholar] [CrossRef]
- Sutherlin, M.A.; Gage, M.; Mangum, L.C.; Hertel, J.; Russell, S.; Saliba, S.A.; Hart, J.M. Changes in Muscle Thickness Across Positions on Ultrasound Imaging in Participants With or Without a History of Low Back Pain. J. Athl. Train. 2018, 53, 553–559. [Google Scholar] [CrossRef]
- Teyhen, D.S.; Miltenberger, C.E.; Deiters, H.M.; Del Toro, Y.M.; Pulliam, J.N.; Childs, J.D.; Boyles, R.E.; Flynn, T.W. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J. Orthop. Sports Phys. Ther. 2005, 35, 346–355. [Google Scholar] [CrossRef]
- Koppenhaver, S.L.; Hebert, J.J.; Fritz, J.M.; Parent, E.C.; Teyhen, D.S.; Magel, J.S. Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch. Phys. Med. Rehabil. 2009, 90, 87–94. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin Epidemiol. 2008, 61, 1500–1524. [Google Scholar]
- Nourbakhsh, M.R.; Arab, A.M. Relationship between mechanical factors and incidence of low back pain. J. Orthop. Sports Phys. Ther. 2002, 32, 447–460. [Google Scholar] [CrossRef] [PubMed]
- Unsgaard-Tøndel, M.; Nilsen, T.I.L.; Magnussen, J.; Vasseljen, O. Is activation of transversus abdominis and obliquus internus abdominis associated with long-term changes in chronic low back pain? A prospective study with 1-year follow-up. Br. J. Sports Med. 2012, 46, 729–734. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry disability index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef]
- Negahban, H.; Mostafaee, N.; Sohani, S.M.; Mazaheri, M.; Goharpey, S.; Salavati, M.; Zahednejad, S.; Meshkati, Z.; Montazeri, A. Reliability and validity of the Tegner and Marx activity rating scales in Iranian patients with anterior cruciate ligament injury. Disabil. Rehabil. 2011, 33, 2305–2310. [Google Scholar] [CrossRef]
- Teyhen, D.S.; Williamson, J.N.; Carlson, N.H.; Suttles, S.T.; O’Laughlin, S.J.; Whittaker, J.L.; Goffar, S.L.; Childs, J.D. Ultrasound characteristics of the deep abdominal muscles during the active straight leg raise test. Arch. Phys. Med. Rehabil. 2009, 90, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Ainscough-Potts, A.M.; Morrissey, M.C.; Critchley, D. The response of the transverse abdominis and internal oblique muscles to different postures. Man. Ther. 2006, 11, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Rankin, G.; Stokes, M.; Newham, D.J. Abdominal muscle size and symmetry in normal subjects. Muscle Nerve 2006, 34, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Stokes, M.; Rankin, G.; Newham, D. Ultrasound imaging of lumbar multifidus muscle: Normal reference ranges for measurements and practical guidance on the technique. Man. Ther. 2005, 10, 116–126. [Google Scholar] [CrossRef]
- Koppenhaver, S.L.; Parent, E.C.; Teyhen, D.S.; Hebert, J.J.; Fritz, J.M. The Effect of Averaging Multiple Trials on Measurement Error During Ultrasound Imaging of Transversus Abdominis and Lumbar Multifidus Muscles in Individuals With Low Back Pain. J. Orthop. Sports Phys. Ther. 2009, 39, 604–611. [Google Scholar] [CrossRef]
- Linek, P.; Saulicz, E.; Wolny, T.; Myśliwiec, A.; Kokosz, M. Lateral abdominal muscle size at rest and during abdominal drawing-in manoeuvre in healthy adolescents. Man. Ther. 2015, 20, 117–123. [Google Scholar] [CrossRef]
- Arab, A.M.; Rasouli, O.; Amiri, M.; Tahan, N. Reliability of ultrasound measurement of automatic activity of the abdominal muscle in participants with and without chronic low back pain. Chiropr Man Ther. 2013, 21, 37. [Google Scholar] [CrossRef]
- Gibbon, K.C.; Debuse, D.; Hibbs, A.; Caplan, N. Reliability and Precision of Sonography of the Lumbar Multifidus and Transversus Abdominis During Dynamic Activities. J. Ultrasound Med. 2017, 36, 571–581. [Google Scholar] [CrossRef]
- Abboud, J.; Nougarou, F.; Pagé, I.; Cantin, V.; Massicotte, D.; Descarreaux, M. Trunk motor variability in patients with non-specific chronic low back pain. Eur. J. Appl. Physiol. 2014, 114, 2645–2654. [Google Scholar] [CrossRef]
- Rossi, D.M.; Morcelli, M.H.; Cardozo, A.C.; Denadai, B.S.; Goncalves, M.; Navega, M.T. Rate of force development and muscle activation of trunk muscles in women with and without low back pain: A case-control study. Phys. Ther. Sport 2017, 26, 41–48. [Google Scholar] [CrossRef][Green Version]
- Yanik, B.; Keyik, B.; Conkbayir, I. Fatty degeneration of multifidus muscle in patients with chronic low back pain and in asymptomatic volunteers: Quantification with chemical shift magnetic resonance imaging. Skelet. Radiol. 2013, 42, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Beneck, G.J.; Baker, L.L.; Kulig, K. Spectral analysis of EMG using intramuscular electrodes reveals non-linear fatigability characteristics in persons with chronic low back pain. J. Electromyogr. Kinesiol. 2013, 23, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; Richardson, C.A. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch. Phys. Med. Rehabil. 1999, 80, 1005–1012. [Google Scholar] [CrossRef]
- Gruther, W.; Wick, F.; Paul, B.; Leitner, C.; Posch, M.; Matzner, M.; Crevenna, R.; Ebenbichler, G. 400 Diagnostic accuracy and reliability of muscle strength and endurance measurements 401 in patients with chronic low back pain. J. Rehabil. Med. 2009, 41, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Yahia, A.; Jribi, S.; Ghroubi, S.; Elleuch, M.; Baklouti, S. Evaluation of the posture and muscular strength of the trunk and inferior 455 members of patients with chronic lumbar pain. Jt. Bone Spine 2011, 78, 291–297. [Google Scholar] [CrossRef]
- Kiesel, K.B.; Underwood, F.B.; Mattacola, C.G.; Nitz, A.J.; Malone, T.R. A comparison of select trunk muscle thickness change between subjects with low back pain classified in the treatment-based classification system and asymptomatic controls. J. Orthop. Sports Phys. 2007, 37, 596–607. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Aagaard, P.; Blazevich, A.J.; Folland, J.; Tillin, N.; Duchateau, J. Rate of force development: Physiological and methodological 424 considerations. Eur. J. Appl. Physiol. 2016, 116, 1091–1116. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.L.; Andersen, J.L.; Suetta, C.; Kjaer, M.; Sogaard, K.; Sjogaard, G. Effect of contrasting physical exercise interventions on rapid force capacity 370 of chronically painful muscles. J. Appl. Physiol. 2009, 107, 1413–1419. [Google Scholar] [CrossRef] [PubMed]


| Variable | Experimental Group (n = 37) | Control Group (n = 25) | p-Value |
|---|---|---|---|
| Age, years | 47.2 ± 9.3 | 43.3 ± 7.8 | 0.04 |
| BMI, kg/m2 | 25.6 ± 3.4 | 24.8 ± 3.6 | 0.02 |
| VAS | 3.6 ± 1.4 | - | - |
| ODI | 22.6 ± 12.1 | - | - |
| Tegner scale | 3.4 ± 0.7 | 3.1 ± 0.4 | 0.05 |
| Position | Muscle Task | Experimental Group | Control Group | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Within-Day | Between-Days | Within-Day | Between-Days | |||||||||||||||
| SD | ICC | SEM | MDC | SD | ICC | SEM | MDC | SD | ICC | SEM | MDC | SD | ICC | SEM | MDC | |||
| Static | TA | Rest | 1.50 | 0.93 | 0.40 | 1.21 | 1.70 | 0.92 | 0.46 | 1.28 | 3.11 | 0.94 | 0.55 | 1.39 | 2.43 | 0.90 | 0.69 | 1.91 |
| Contraction | 1.81 | 0.88 | 0.54 | 1.45 | 1.81 | 0.72 | 0.94 | 2.21 | 2.63 | 0.96 | 0.46 | 1.27 | 2.52 | 0.95 | 0.52 | 1.44 | ||
| Contraction ratio | 0.4 | 0.95 | 0.08 | 0.20 | 0.40 | 0.93 | 0.11 | 0.31 | 0.29 | 0.86 | 0.13 | 0.35 | 0.42 | 0.80 | 0.16 | 0.45 | ||
| LM | Rest | 5.27 | 0.91 | 1.48 | 4.23 | 5.26 | 0.82 | 2.31 | 6.28 | 6.58 | 0.98 | 0.50 | 1.63 | 7.01 | 0.98 | 0.44 | 1.79 | |
| Contraction | 6.37 | 0.94 | 1.68 | 4.81 | 6.42 | 0.82 | 2.55 | 7.30 | 9.60 | 0.92 | 2.38 | 7.07 | 9.98 | 0.94 | 2.30 | 6.31 | ||
| Contraction ratio | 0.19 | 0.95 | 0.06 | 0.11 | 0.11 | 0.91 | 0.03 | 0.11 | 0.21 | 0.90 | 0.06 | 1.09 | 0.23 | 0.93 | 0.05 | 0.15 | ||
| Dynamic | TA | Rest | 1.26 | 0.90 | 0.40 | 0.98 | 1.46 | 0.74 | 0.69 | 2.07 | 1.55 | 0.93 | 0.40 | 1.10 | 1.38 | 0.94 | 0.31 | 0.88 |
| Contraction | 1.87 | 0.90 | 0.55 | 1.63 | 2.10 | 0.85 | 0.75 | 2.16 | 1.68 | 0.97 | 0.33 | 0.70 | 1.59 | 0.95 | 0.20 | 0.92 | ||
| Contraction ratio | 0.39 | 0.93 | 0.15 | 0.31 | 0.51 | 0.94 | 0.15 | 0.31 | 0.35 | 0.95 | 0.07 | 0.15 | 0.35 | 0.93 | 0.08 | 0.221 | ||
| LM | Rest | 7.92 | 0.96 | 1.42 | 4.05 | 7.88 | 0.93 | 2.10 | 5.95 | 9.42 | 0.95 | 1.78 | 5.08 | 9.21 | 0.97 | 1.88 | 5.19 | |
| Contraction | 8.32 | 0.90 | 2.60 | 7.10 | 8.57 | 0.85 | 3.40 | 8.91 | 11.05 | 0.93 | 2.70 | 7.48 | 10.95 | 0.93 | 2.79 | 7.79 | ||
| Contraction ratio | 0.27 | 0.97 | 0.04 | 0.16 | 0.27 | 0.96 | 0.04 | 0.14 | 0.41 | 0.93 | 0.10 | 0.23 | 0.41 | 0.93 | 0.07 | 0.25 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez Romero, E.A.; Alonso Pérez, J.L.; Muñoz Fernández, A.C.; Battaglino, A.; Castaldo, M.; Cleland, J.A.; Villafañe, J.H. Reliability of Sonography Measures of the Lumbar Multifidus and Transversus Abdominis during Static and Dynamic Activities in Subjects with Non-Specific Chronic Low Back Pain. Diagnostics 2021, 11, 632. https://doi.org/10.3390/diagnostics11040632
Sánchez Romero EA, Alonso Pérez JL, Muñoz Fernández AC, Battaglino A, Castaldo M, Cleland JA, Villafañe JH. Reliability of Sonography Measures of the Lumbar Multifidus and Transversus Abdominis during Static and Dynamic Activities in Subjects with Non-Specific Chronic Low Back Pain. Diagnostics. 2021; 11(4):632. https://doi.org/10.3390/diagnostics11040632
Chicago/Turabian StyleSánchez Romero, Eleuterio A., José Luis Alonso Pérez, Alberto Carlos Muñoz Fernández, Andrea Battaglino, Matteo Castaldo, Joshua A. Cleland, and Jorge Hugo Villafañe. 2021. "Reliability of Sonography Measures of the Lumbar Multifidus and Transversus Abdominis during Static and Dynamic Activities in Subjects with Non-Specific Chronic Low Back Pain" Diagnostics 11, no. 4: 632. https://doi.org/10.3390/diagnostics11040632
APA StyleSánchez Romero, E. A., Alonso Pérez, J. L., Muñoz Fernández, A. C., Battaglino, A., Castaldo, M., Cleland, J. A., & Villafañe, J. H. (2021). Reliability of Sonography Measures of the Lumbar Multifidus and Transversus Abdominis during Static and Dynamic Activities in Subjects with Non-Specific Chronic Low Back Pain. Diagnostics, 11(4), 632. https://doi.org/10.3390/diagnostics11040632







