The Role of Cytology in the Diagnosis of Subcentimeter Thyroid Lesions
Abstract
:1. Introduction
2. Materials and Methods
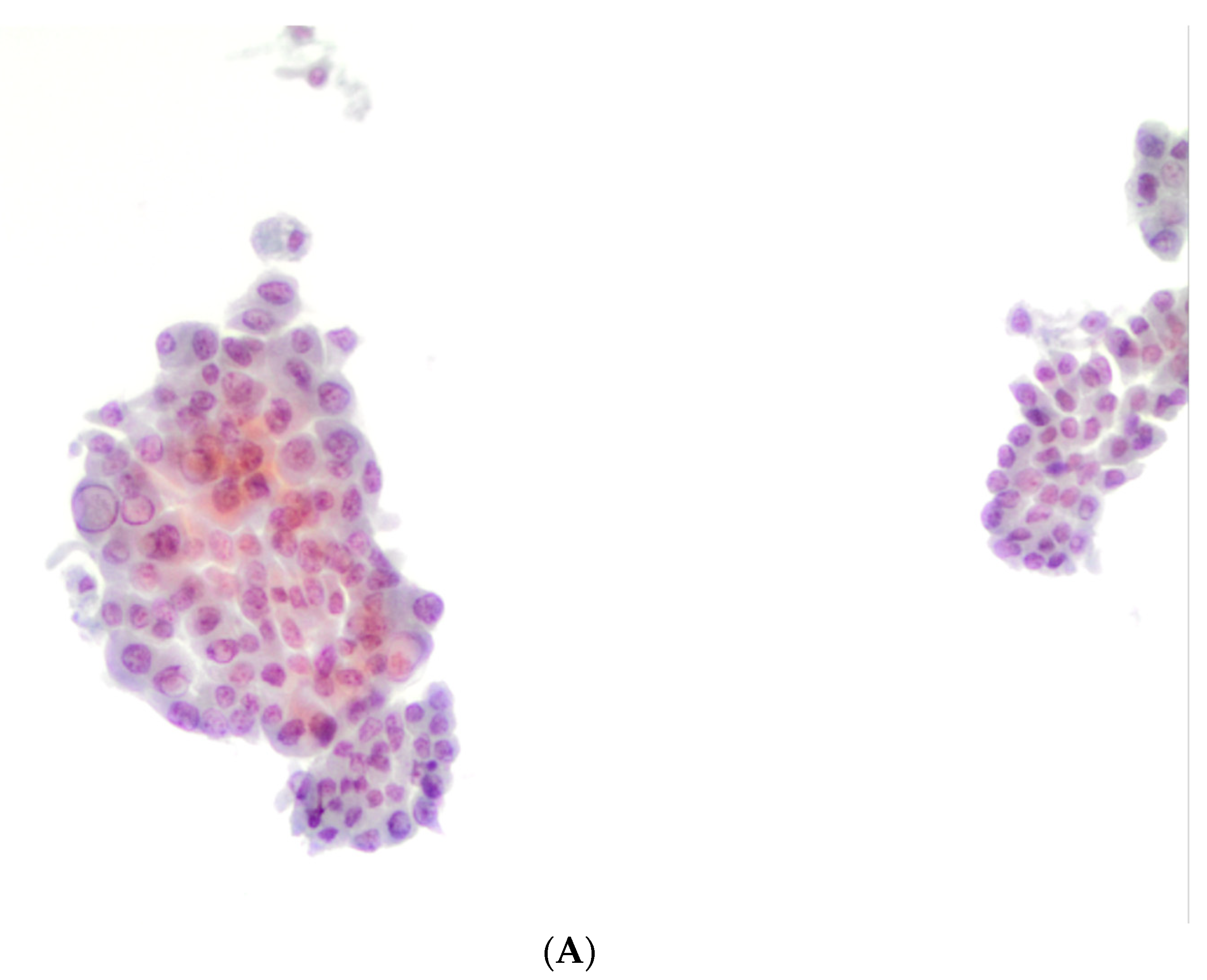
2.1. Thyroid FNAC Specimens
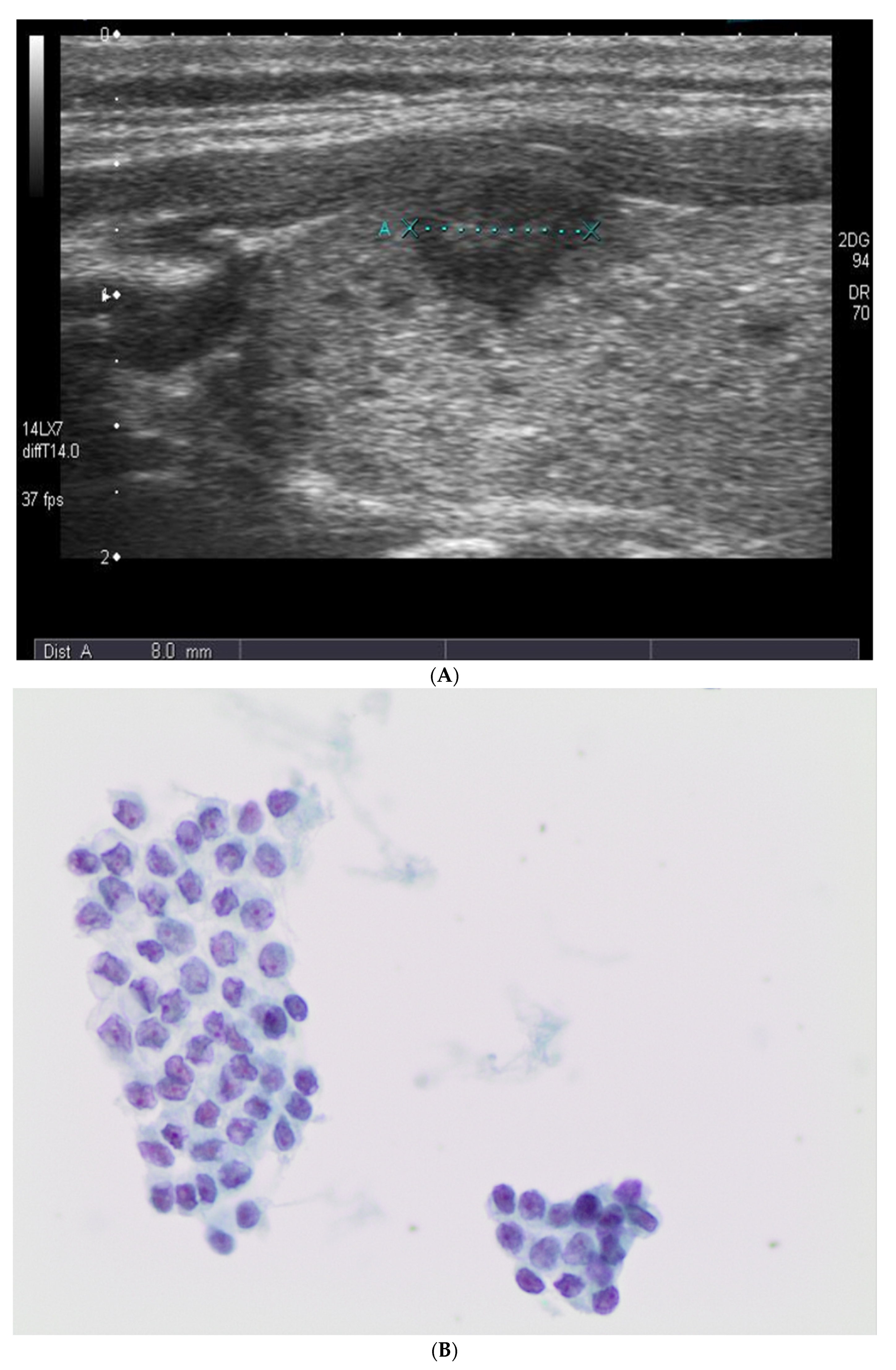
2.2. Ultrasound Evaluation
2.3. Immunocytochemistry (ICC) Analysis
2.4. Histology Specimens
2.5. Molecular Analysis for BRAF and TERT Mutation
2.6. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Partyka, K.L.; Wu, H.H. Fine-needle aspirates of thyroid microcarcinoma. J. Am. Soc. Cytopathol. 2017, 6, 236–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiss, V.L.; Andreotti, R.F.; Ely, K.A. Use of the thyroid imaging, reporting, and data system (TI-RADS) scoring system for the evaluation of subcentimeter thyroid nodules. Cancer Cytopathol. 2018, 126, 518–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.G.; Moon, H.-J.; Kwak, J.Y.; Kim, E.-K. Diagnostic Accuracy of the Ultrasonographic Features for Subcentimeter Thyroid Nodules Suggested by the Revised American Thyroid Association Guidelines. Thyroid 2013, 23, 1583–1589. [Google Scholar] [CrossRef]
- Gao, L.; Ma, B.; Zhou, L.; Wang, Y.; Yang, S.; Qu, N.; Gao, Y.; Ji, Q. The impact of presence of Hashimoto’s thyroiditis on diagnostic accuracy of ultrasound-guided fine-needle aspiration biopsy in subcentimeter thyroid nodules: A retrospective study from FUSCC. Cancer Med. 2017, 6, 1014–1022. [Google Scholar] [CrossRef]
- Zhang, M.; Zhang, Y.; Fu, S.; Lv, F.; Tang, J. Development of a Logistic Regression Formula for Evaluation of Subcentimeter Thyroid Nodules. J. Ultrasound Med. 2014, 33, 1023–1030. [Google Scholar] [CrossRef]
- Gweon, H.M.; Son, E.J.; Kim, J.-A.; Youk, J.H. Predictive Factors for Active Surveillance of Subcentimeter Thyroid Nodules with Highly Suspicious US Features. Ann. Surg. Oncol. 2017, 24, 1540–1545. [Google Scholar] [CrossRef]
- Marrero, A.P.; Gracia, A.; Méndez, W. The Sonographic Subcentimeter Malignant Thyroid Nodule: What Does It Stand For? Am. Surg. 2018, 84, 137–139. [Google Scholar] [CrossRef]
- Berker, D.; Isik, S.; Ozuguz, U.; Tutuncu, Y.A.; Kucukler, K.; Akbaba, G.; Aydin, Y.; Güler, S. Prevalence of incidental thyroid cancer and its ultrasonographic features in subcentimeter thyroid nodules of patients with hyperthyroidism. Endocrine 2010, 39, 13–20. [Google Scholar] [CrossRef]
- Berker, D.; Aydin, Y.; Ustun, I.; Gul, K.; Tutuncu, Y.; Işik, S.; Delibasi, T.; Guler, S. The value of fine-needle aspiration biopsy in sub-centimeter thyroid nodules. Thyroid 2008, 18, 603–608. [Google Scholar] [CrossRef]
- Mazzaferri, E.L.; Sipos, J. Should All Patients with Subcentimeter Thyroid Nodules Undergo Fine-Needle Aspiration Biopsy and Preoperative Neck Ultrasonography to Define the Extent of Tumor Invasion? Thyroid 2008, 18, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Chen, E.D.; Zheng, H.M.; He, Q.X.; Li, Q. Ultrasound score to select subcentimeter-sized thyroid nodules requiring ul-trasound-guided fine needle aspiration biopsy in eastern China. Asian Pac. J. Cancer Prev. 2013, 14, 4689–4692. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Yu, J.H.; Du, P.J.; Xie, Y.; Das, S.K.; Li, B.; Zhang, C. High-Score US-Suspicious Subcentimeter Thyroid Nodules: What Factors Affect Adequate Sampling of US-Guided Fine-Needle Aspiration Biopsy? Int. J. Endocrinol. 2020, 84, 646–663. [Google Scholar] [CrossRef] [Green Version]
- Mendes, G.F.; Garcia, M.R.; Falsarella, P.M.; Rahal, A.; Cavalcante, F.A., Jr.; Nery, D.R.; Garcia, R.G. Fine needle aspiration biopsy of thyroid nodule smaller than 1.0 cm: Accuracy of TIRADS classification system in more than 1000 nodules. Br. J. Radiol. 2018, 91, 20170642. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, A.; Johnson, D.N.; White, M.G.; Siddiqui, S.; Antic, T.; Mathew, M.; Grogan, R.H.; Angelos, P.; Kaplan, E.L.; Cipriani, N.A. Thyroid Nodule Size at Ultrasound as a Predictor of Malignancy and Final Pathologic Size. Thyroid 2017, 27, 641–650. [Google Scholar] [CrossRef] [PubMed]
- Lansford, C.D.; Teknos, T.N.; Lansford, C.D. Evaluation of the thyroid nodule. Cancer Control 2006, 13, 89–98. [Google Scholar] [CrossRef] [Green Version]
- Genere, N.; Hurtado, M.D.; Cortes, T.; Athimulam, S.; Al Ward, R.; Callstrom, M.R.; Stan, M.N.; Morris, J.C.; Brito, J.P. Drivers of the Decision to Biopsy and Follow-Up of Small Suspicious Thyroid Nodules. Endocr. Pract. 2020, 26, 857–868. [Google Scholar] [CrossRef]
- Papaioannou, C.; Lamnisos, D.; Kyriacou, K.; Lyssiotis, T.; Constantinides, V.; Frangos, S.; Economides, A.; Economides, P.A. Lymph Node Metastasis and Extrathyroidal Extension in Papillary Thyroid Microcarcinoma in Cyprus: Suspicious Subcentimeter Nodules Should Undergo FNA When Multifocality is Suspected. J. Thyroid. Res. 2020, 2020, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Kwak, J.Y.; Kim, E.-K.; Kim, M.J.; Son, E.J. Significance of sonographic characterization for managing subcentimeter thyroid nodules. Acta Radiol. 2009, 50, 917–923. [Google Scholar] [CrossRef] [PubMed]
- Poller, D.N.; Baloch, Z.W.; Fadda, G.; Johnson, S.J.; Bongiovanni, M.; Pontecorvi, A.; Cochand-Priollet, B. Thyroid FNA: New classifi-cations and new interpretations. Cancer Cytopathol. 2016, 124, 457–466. [Google Scholar] [CrossRef]
- Fadda, G.; Rossi, E.D. Liquid-Based Cytology in Fine-Needle Aspiration Biopsies of the Thyroid Gland. Acta Cytol. 2011, 55, 389–400. [Google Scholar] [CrossRef] [Green Version]
- Rossi, E.D.; Pusztaszeri, M.; Schmitt, F.; Bongiovanni, M.; Chandra, A.; Faquin, W.C. Thyroid FNA: International perspectives from the European Congress of Cytopathology: Can we cross the bridge of classifications? Cancer Cytopathol. 2015, 123, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Chng, C.-L.; Beale, T.; Kurzawinski, T.R. Value of sonographic features in predicting malignancy in thyroid nodules diagnosed as follicular neoplasm on cytology. Clin. Endocrinol. 2014, 83, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [Green Version]
- Cooper, D.S.; Doherty, G.M.; Haugen, B.R.; Kloos, R.T.; Lee, S.L.; Mandel, S.J.; Mazzaferri, E.L.; McIver, B.; Sherman, S.I.; Tuttle, R.M. Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2006, 16, 116–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooper, D.S.; Doherty, G.M.; Haugen, B.R.; Kloos, R.T.; Lee, S.L.; Mandel, S.J.; Mazzaferri, E.L.; McIver, B.; Pacini, F.; Schlumberger, M.; et al. American Thyroid Association (ATA) guidelines taskforce on thyroid nodules and differentiated thyroid cancer. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009, 19, 1167–1214. [Google Scholar] [CrossRef] [Green Version]
- Maia, F.F.; Matos, P.S.; Pavin, E.J.; Pallone, A.T.; Pavin, E.J.; Vassallo, J.; Zantut-Wittmann, D.E. Value of ultrasound and cytological classification system to predict the malignancy of thyroid nodules with indeterminate cytology. Endocr. Pathol. 2011, 22, 66–73. [Google Scholar] [CrossRef]
- Ding, J.; Jiang, L.; Fang, J.; Jiang, Y.; Zhu, Y.; Hua, T.; Yuan, Y.; Wu, W. Predictors for malignancy risk in subcentimeter thyroid nodules categorized as atypia/follicular lesion of undetrmined significance by fine neeldle aspiration. Sci. Rep. 2019, 9, 14973. [Google Scholar] [CrossRef]
- Koo, D.H.; Song, K.; Kwon, H.; Bae, D.S.; Kim, J.H.; Min, H.S.; Lee, K.E.; Youn, Y.K. Does tumor size influence the diagnostic accuracy of ultrasound-guided fine needle aspiration cytology for thyroid nodules? Int. J. Endocrinol. 2016, 12, 380–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aydogan, B.I.; Sahin, M.; Ceyhan, K.; Deniz, O.; Demir, Ö.; Emral, R.; Tonyukuk Gedik, V.; Uysal, A.R.; Çorapçıoğlu, D. The influence of thyroid nodule size on the diagnostic efficacy and accuracy of ultrasound guided fine-needle aspiration cytology. Diagn. Cytopathol. 2019, 42, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.J.; Son, E.; Kim, E.K.; Yoon, J.H.; Kwak, J.Y. The diagnostic value of ultrasound and ultrasound-guided fine needle aspiration in subcentimeter. Ann. Surg. Oncol. 2012, 19, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Gabriel, H.; Nemcek, A.; Nayar, R.; Du, H.; Nikolaidis, P. Subcentimeter thyroid nodules: Utility of sonographic char-acterization and ultrasound-guided needle biopsy. AJR 2011, 197, W1123–W1128. [Google Scholar] [CrossRef]
- Nam-Goong, I.S.; Kim, H.Y.; Gong, G.; Lee, H.K.; Hong, S.J.; Kim, W.B.; Shong, Y.K. Ultrasonography-guided fine-needle aspiration of thyroid incidentaloma: Correlation with pathological findings. Clin. Endocrinol. 2004, 60, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Leenhardt, L.; Hejblum, G.; Franc, B.; Fediaevsky, L.D.; Delbot, T.; Le Guillouzic, D.; Ménégaux, F.; Guillausseau, C.; Hoang, C.; Turpin, G.; et al. Indications and limits of ultrasound-guided cytology in the management of nonpalpable thyroid nodules. Clin. Endocrinol. Metab. 1999, 84, 24–28. [Google Scholar] [CrossRef]
- Siddiqui, M.A.; Griffith, K.A.; Michael, C.W.; Pu, R.T. Nodule heterogeneity as shown by size differences between the targeted nodule and the tumor in thyroidectomy specimen. Cancer 2007, 114, 27–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Bethesda System for Reporting Thyroid Cytopathology, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2018.
- Nardi, F.; Basolo, F.; Crescenzi, A.; Fadda, G.; Frasoldati, A.; Orlandi, F.; Palombini, L.; Papini, E.; Zini, M.; Pontecorvi, A.; et al. Italian consensus for the classification and reporting of thyroid cytology. J. Endocrinol. Investig. 2014, 37, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Grant, E.G.; Tessler, F.N.; Hoang, J.K.; Langer, J.E.; Beland, M.D.; Berland, L.L.; Cronan, J.J.; Desser, T.S.; Frates, M.C.; Hamper, U.M.; et al. Thyroid Ultrasound Reporting Lexicon: White Paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. J. Am. Coll. Radiol. 2015, 12, 1272–1279. [Google Scholar] [CrossRef] [PubMed]
- Fadda, G.; Rossi, E.D.; Raffaelli, M.; Pontecorvi, A.; Sioletic, S.; Morassi, F.; Lombardi, C.P.; Zannoni, G.F.; Rindi, G. Follicular thyroid neoplasms can be classified as low- and high-risk according to HBME-1 and Galectin-3 expression on liquid-based fine-needle cytology. Eur. J. Endocrinol. 2011, 165, 447–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi, E.D.; Martini, M.; Capodimonti, S.; Cenci, T.; Bilotta, M.; Pierconti, F.; Pontecorvi, A.; Lombardi, C.P.; Fadda, G.; LaRocca, L.M. Morphology combined with ancillary techniques: An algorithm approach for thyroid nodules. Cytopathology 2018, 29, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Rosai, J.; Albores Saavedra, J.; Asioli, S. Papillary thyroid carcnoma. In WHO Classification of Tumours of Endocrine Organs, 4th ed.; Lloyd, R.V., Osamura, R.Y., Klöppel, G., Rosai, J., Eds.; International Agency for Research on Cancer: Lyon, France, 2017; pp. 81–91. [Google Scholar]
- American Joint Commission on Cancer (AJCC). Cancer Staging Atlas, 8th ed.; Springer: New York, NY, USA, 2017; p. 873. [Google Scholar]
- Nikiforov, Y.E.; Seethala, R.R.; Tallini, G.; Baloch, Z.W.; Basolo, F.; Thompson, L.D.; Barletta, J.A.; Wenig, B.M.; Al Ghuzlan, A.; Kakudo, K.; et al. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: A paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2016, 2, 1023–1029. [Google Scholar] [CrossRef] [Green Version]
- Rossi, E.D.; Martini, M.; Capodimonti, S.; Lombardi, C.P.; Pontecorvi, A.; Vellone, V.G.; Zannoni, G.F.; Larocca, L.M.; Fadda, G. BRAF (v600e) mutation analysis on LBC-processed aspiration biopsies predicts bilaterality and nodal involvement in papillary thyroid microcarcinoma. Cancer Cytopathol. 2013, 121, 291–297. [Google Scholar] [CrossRef]
- Bo, Y.H.; Ahn, H.Y.; Lee, Y.H.; Lee, Y.J.; Kim, J.H.; Ohn, J.H.; Hong, E.S.; Kim, K.W.; Jeong, I.K.; Choi, S.H.; et al. Malignancy Rate in Sonographically Suspicious Thyroid Nodules of Less than a Centimeter in Size Does Not Decrease with Decreasing Size. J. Korean Med. Sci. 2011, 26, 237–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brito, J.P.; Ito, Y.; Miyauchi, A.; Tuttle, R.M. A Clinical Framework to Facilitate Risk Stratification When Considering an Active Surveillance Alternative to Immediate Biopsy and Surgery in Papillary Microcarcinoma. Thyroid 2016, 26, 144–149. [Google Scholar] [CrossRef] [Green Version]
- Schenke, S.; Klett, R.; Seifert, P.; Kreissl, M.C.; Görges, R.; Zimny, M. Diagnostic Performance of Different Thyroid Imaging Reporting and Data Systems (Kwak-TIRADS, EU-TIRADS and ACR TI-RADS) for Risk Stratification of Small Thyroid Nodules (≤10 mm). J. Clin. Med. 2020, 9, 236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.E.; Hwang, T.S.; Choi, Y.-L.; Han, H.S.; Kim, W.S.; Jang, M.H.; Kim, S.K.; Yang, J.H. Prognostic Significance of TERT Promoter Mutations in Papillary Thyroid Carcinomas in a BRAFV600E Mutation–Prevalent Population. Thyroid 2016, 26, 901–910. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.; Song, Y.S.; Kim, Y.A.; Lim, J.A.; Cho, S.W.; Moon, J.H.; Hahn, S.; Park, D.J.; Park, Y.J. Effects of coexistent BRAF V600E and TERT promoter mutations on poor clinical outcomes in papillary thyroid cancer: A meta-analysis. Thryoid 2017, 27, 651–660. [Google Scholar] [CrossRef]
- Chakraborty, A.; Narkar, A.; Mukhopadhyaya, R.; Kane, S.; D’Cruz, A.; Rajan, M.G. BRAFV600E mutation in papillary thyroid carcinoma: Significant association with node metastases and extra thyroidal invasion. Endocr. Pathol. 2012, 23, 83–93. [Google Scholar] [CrossRef] [PubMed]


| Number of Cases | <1 cm | ≥1 cm |
|---|---|---|
| 475 * | 606 | |
| Gender | ||
| Male | 146 | 239 |
| Female | 329 | 367 |
| Age—mean (range), years | 44.38 (16–81) | 42.21 (15–79) |
| Size—mean (range), mm | 4.4 (0.3–10) | 4 (1–6) |
| Cytological Diagnostic Categories | ||
| Non-diagnostic | 35 | 29 |
| Benign | 144 | 226 |
| AUS/FLUS | 12 | 54 |
| FN/SFN | 12 | 142 |
| SFM | 124 | 48 |
| M | 148 | 107 |
| Follow-Up | ||
| Surgical follow-up | 307 | 386 |
| Histopathological Diagnoses | ||
| Benign goiter | 6 | 157 |
| Hashimoto thyroiditis | 2 | 5 |
| Follicular adenoma | 8 | 97 |
| PTC and its variants | 287 | 114 |
| MTC | 4 | 6 |
| FC/OFC | 0 | 1–4 |
| NIFTP | 0 | 2 |
| Lymph node metastases * | 15 | 46 |
| Bethesda | Hyperechoic (<1 cm/≥1 cm) | Isoechoic (<1 cm/≥1 cm) | Hypoechoic (<1 cm/≥1 cm) | Taller-Than-Wide (<1 cm/≥1 cm) |
|---|---|---|---|---|
| I (35 cases/29 cases) | 5 (14.3%)/1(%) | 7 (20%)/8 | 23 (65.7%)/20 | 0/0 |
| II (144 cases/226 cases) | 5 (3.4%)/0 | 6 (4.1%)/64 | 133 (92.3%)/162 | 0/0 |
| III (12 cases/54 cases) | 2 (16.6%)/1 | 0/8 | 10 (83.3%)/45 | 0/0 |
| IV (12 cases/142 cases) | 2 (16.6%)/7 (5%) | 1 (8.3%)/57 | 9 (75%)/78 | 0/0 |
| V (124 cases/48 cases) | 3 (2.4%)/1 (%) | 9 (7.2%)/1 | 112 (90.3%)/46 | 0/0 |
| VI (148 cases/107 cases) | 6 (4%)/0 | 4 (2.7%)/26 | 138 (93.2%)/79 | 20 (13.5%)/2 |
| Diagnosis | Goiter | HT | FA | MTC | PTC | FVPTC | TCV PTC | Warthin PTC | Hobnail PTC | CCV PTC | Solid PTC |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ND (2 cases) | 1 | 1 | |||||||||
| B (10 cases) | 5 | 2 | 3 | ||||||||
| AUS/FLUS (11 cases) | 2 | 3 | 2 | 4 | |||||||
| FN/SFN (12 cases) | 2 | 4 | 4 | 2 | |||||||
| SFM (124 cases) | 1 | 105 | 10 | 6 | 2 | ||||||
| M (148 cases) | 4 | 119 | 10 | 5 | 3 | 2 | 5 |
| Diagnosis | Goiter | HT | FA | NIFTP | MTC | FC | PTC | FVPTC | TCV PTC | Warthin PTC | Hobnail PTC | CCV PTC | Solid PTC | OFC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ND (4 cases) | 3 | 0 | 1 | |||||||||||
| B (182 cases) | 145 | 3 | 31 | 0 | 1 | 1 | 1 | |||||||
| AUS/FLUS (37 cases) | 4 | 1 | 32 | 0 | ||||||||||
| FN/SFN (46 cases) | 5 | 1 | 33 | 2 | 3 | 1 | 1 | |||||||
| SFM (15 cases) | 1 | 0 | 12 | 1 | 1 | |||||||||
| M (102 cases) | 0 | 6 | 89 | 3 | 1 | 2 | 1 |
| TBRTC Category | Discordant Cases * |
|---|---|
| Bethesda I (2 cases) | 1/2 (50%) |
| Bethesda II (10 cases) | 3/10 (30%) |
| Bethesda III (11 cases) | 6/11 (54.5%) |
| Bethesda IV (12 cases) | 10/12 (83.3%) |
| Bethesda V (124 cases) | 1/124 (0.8%) |
| Bethesda VI (148 cases) | 0/148 |
| TBRTC Category | Discordant Cases * |
|---|---|
| Bethesda I (4 cases) | 1/4 (25%) |
| Bethesda II (182 cases) | 3/182 (1.6%) |
| Bethesda III (37 cases) | 0/37 |
| Bethesda IV (46 cases) | 7 */46 (10.8%) |
| Bethesda V (15 cases) | 1/15 (6.6%) |
| Bethesda VI (102 cases) | 0/102 |
| Bethesda Category | H+/G+ | Discordant | H−/G− | Calcitonin |
|---|---|---|---|---|
| I (35 cases) | 0 | 0 | 0 | 0 |
| II (144 cases) | 0 | 0 | 39 (27%) | 0 |
| III (12 cases) | 4 (33.3%) | 5 (41.6%) | 3 (25%) | 0 |
| IV (12 cases) | 4 (33.3%) | 6 (50%) | 2 (16.6%) | 0 |
| V (124 cases) | 42 (33.8%) | 3 (2.4%) | 0 | 0 |
| VI (148 cases) | 10 (6.7%) | 0 | 0 | 4 (2.7%) |
| Bethesda Category | H+/G+ | Discordant | H−/G− | Calcitonin |
|---|---|---|---|---|
| I (4 cases) | 0 | 0 | 0 | 0 |
| II (182 cases) | 0 | 0 | 5 (2.7%) | 0 |
| III (37 cases) | 3 (8.1%) | 8 (21.6%) | 26 (70.2%) | 0 |
| IV (46 cases) | 5 (10.8%) | 16 (34.7%) | 25 (54.3%) | 0 |
| V (15 cases) | 12 (80%) | 2 (13.3%) | 1 (6.6%) | 0 |
| VI (102 cases) | 15 (14.7%) | 0 | 0 | 4 (3.9%) |
| Bethesda Category | BRAF+ | BRAF− | TERT Mutated |
|---|---|---|---|
| I (35 cases) | 0 | 0 | 0 |
| II (144 cases) | 0 | 0 | 0 |
| III (12 cases) | 0 | 12 (100%) | 0 |
| IV (12 cases) | 1 (8.3%) | 11 (91.6%) | 0 |
| V (124 cases) | 9 (7.2%) | 10 (8%) | 0 |
| VI (148 cases) | 5 (3.3%) | 10 (6.7%) | 0 |
| Bethesda Category | BRAF+ | BRAF− | TERT Mutated |
|---|---|---|---|
| I (4 cases) | 0 | 0 | 0 |
| II (182 cases) | 0 | 0 | 0 |
| III (37 cases) | 0 | 37 (100%) | 0 |
| IV (46 cases) | 1 (2.1%) | 13 (28.2%) | 0 |
| V (15 cases) | 6 (40%) | 9 (60%) | 0 |
| VI (102 cases) | 2 (1.9%) | 28 (27.4%) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fiorentino, V.; Dell’ Aquila, M.; Musarra, T.; Martini, M.; Capodimonti, S.; Fadda, G.; Curatolo, M.; Traini, E.; Raffaelli, M.; Lombardi, C.P.; et al. The Role of Cytology in the Diagnosis of Subcentimeter Thyroid Lesions. Diagnostics 2021, 11, 1043. https://doi.org/10.3390/diagnostics11061043
Fiorentino V, Dell’ Aquila M, Musarra T, Martini M, Capodimonti S, Fadda G, Curatolo M, Traini E, Raffaelli M, Lombardi CP, et al. The Role of Cytology in the Diagnosis of Subcentimeter Thyroid Lesions. Diagnostics. 2021; 11(6):1043. https://doi.org/10.3390/diagnostics11061043
Chicago/Turabian StyleFiorentino, Vincenzo, Marco Dell’ Aquila, Teresa Musarra, Maurizio Martini, Sara Capodimonti, Guido Fadda, Mariangela Curatolo, Emanuela Traini, Marco Raffaelli, Celestino Pio Lombardi, and et al. 2021. "The Role of Cytology in the Diagnosis of Subcentimeter Thyroid Lesions" Diagnostics 11, no. 6: 1043. https://doi.org/10.3390/diagnostics11061043
APA StyleFiorentino, V., Dell’ Aquila, M., Musarra, T., Martini, M., Capodimonti, S., Fadda, G., Curatolo, M., Traini, E., Raffaelli, M., Lombardi, C. P., Pontecorvi, A., Larocca, L. M., Pantanowitz, L., & Rossi, E. D. (2021). The Role of Cytology in the Diagnosis of Subcentimeter Thyroid Lesions. Diagnostics, 11(6), 1043. https://doi.org/10.3390/diagnostics11061043










