Role of Contrast-Enhanced Ultrasound (CEUS) in Native Kidney Pathology: Limits and Fields of Action
Abstract
:1. Introduction
2. Repeatability of CEUS
3. Tolerance and Safety
4. Limitations
5. Examination Technique and Normal Renal Parenchyma
6. Clinical Indications in the Native Kidney
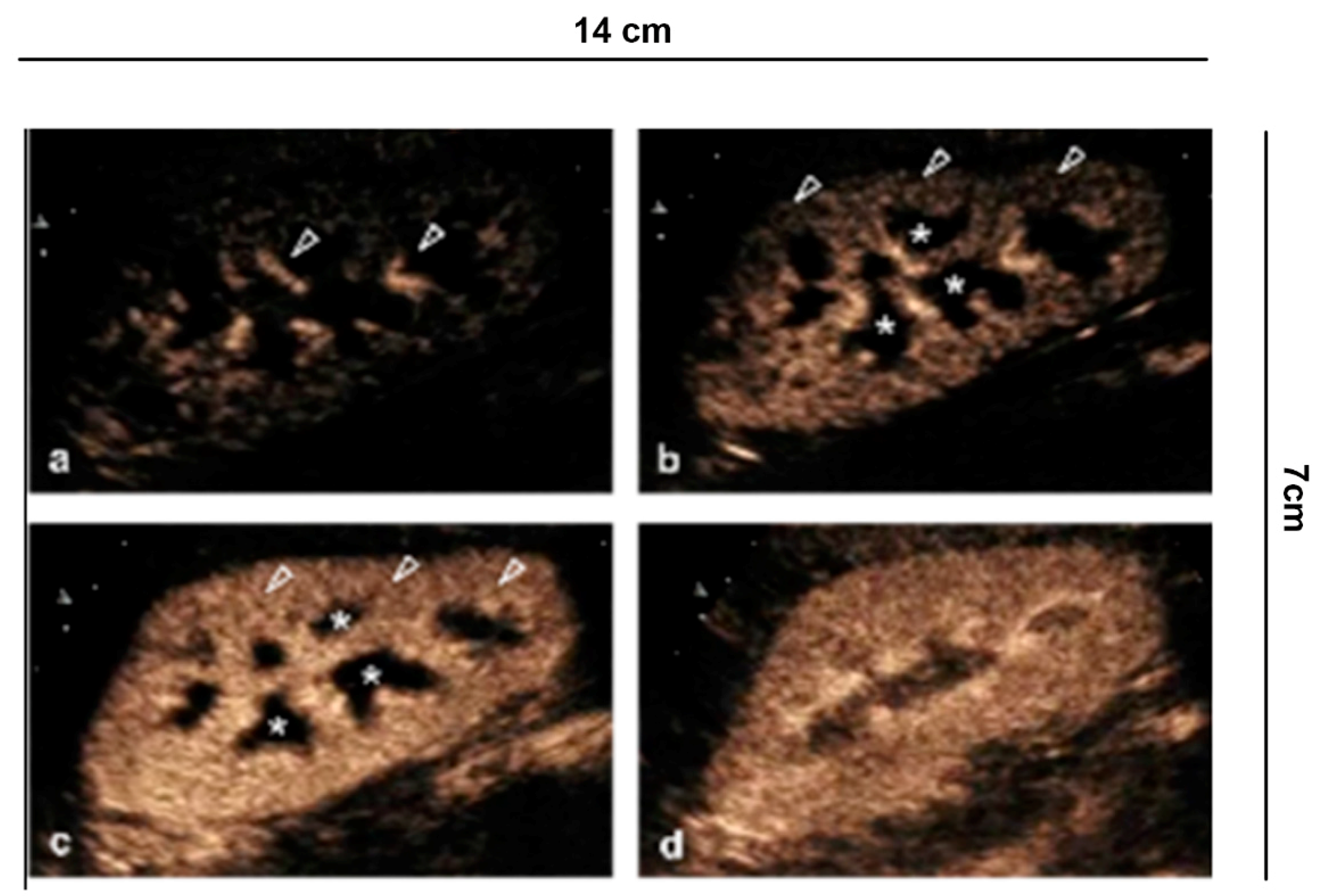
6.1. Characterization of Cystic Lesions
6.2. Characterization of Indeterminate Lesions
6.3. Characterization of Solid Renal Lesions
6.4. Differential Diagnosis between Solid Renal Masses and Pseudotumors
6.5. Follow-Up of Tumor Ablation
6.6. Complicated Pyelonephritis
6.7. Vascular Lesions
6.7.1. Renal Artery Stenosis
6.7.2. Renal Vein Thrombosis
7. Potential Future Scenarios
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AKI | acute kidney injury |
| ccRCC | clear Cell Renal Cell Carcinoma |
| CDUS | Color Doppler US |
| CECT | contrast-enhanced computed tomography |
| CEMRI | contrast-enhanced MRI |
| CEUS | contrast enhancement ultrasound |
| CKD | chronic kidney disease |
| CRF | chronic renal failure |
| CT | computed tomography |
| MRI | magnetic resonance imaging |
| pRCC | papillary Renal Cell Carcinoma |
| UCAs | ultrasound contrast agents |
| US | ultrasound |
References
- Albrecht, T.; Blomley, M.; Bolondi, L.; Claudon, M.; Correas, J.-M.; Cosgrove, D.; Greiner, L.; Jäger, K.; Jong, N.; Leen, E.; et al. Guidelines for the Use of Contrast Agents in Ultrasound—January 2004. Ultraschall Med. 2004, 25, 249–256. [Google Scholar] [CrossRef] [Green Version]
- Claudon, M.; Cosgrove, D.; Albrecht, T.; Bolondi, L.; Bosio, M.; Calliada, F.; Correas, J.-M.; Darge, K.; Dietrich, C.; D’Onofrio, M.; et al. Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS)—Update 2008. Ultraschall Med. 2008, 29, 28–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sidhu, P.; Cantisani, V.; Dietrich, C.; Gilja, O.; Saftoiu, A.; Bartels, E.; Bertolotto, M.; Calliada, F.; Clevert, D.-A.; Cosgrove, D.; et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. 2018, 39, e2–e44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sidhu, P.; Cantisani, V.; Dietrich, C.; Gilja, O.; Saftoiu, A.; Bartels, E.; Bertolotto, M.; Calliada, F.; Clevert, D.-A.; Cosgrove, D.; et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Short Version). Ultraschall Med. 2018, 39, 154–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertolotto, M.; Quaia, E.; Galli, G.; Martinoli, C.; Locatelli, M. Color Doppler Sonographic Appearance of Renal Perforating Vessels in Subjects with Normal and Impaired Renal Function. J. Clin. Ultrasound 2000, 28, 10. [Google Scholar] [CrossRef]
- Pozzi Mucelli, R.; Bertolotto, M.; Quaia, E. Imaging Techniques in Acute Renal Failure. In Contributions to Nephrology; Ronco, C., Bellomo, R., La Greca, G., Eds.; KARGER: Basel, Switzerland, 2001; Volume 132, pp. 76–91. [Google Scholar] [CrossRef]
- Quaia, E.; Bertolotto, M. Renal Parenchymal Diseases: Is Characterization Feasible with Ultrasound? Eur. Radiol. 2002, 12, 2006–2020. [Google Scholar] [CrossRef] [PubMed]
- Quaia, E.; Bertolotto, M.; Cioffi, V.; Rossi, A.; Baratella, E.; Pizzolato, R.; Cova, M.A. Comparison of Contrast-Enhanced Sonography with Unenhanced Sonography and Contrast-Enhanced CT in the Diagnosis of Malignancy in Complex Cystic Renal Masses. Am. J. Roentgenol. 2008, 191, 1239–1249. [Google Scholar] [CrossRef]
- Bertolotto, M.; Martegani, A.; Aiani, L.; Zappetti, R.; Cernic, S.; Cova, M.A. Value of Contrast-Enhanced Ultrasonography for Detecting Renal Infarcts Proven by Contrast Enhanced CT. A Feasibility Study. Eur. Radiol. 2008, 18, 376–383. [Google Scholar] [CrossRef]
- Miller, D.L.; Dou, C.; Lucchesi, B.R. Are ECG Premature Complexes Induced by Ultrasonic Cavitation Electrophysiological Responses to Irreversible Cardiomyocyte Injury? Ultrasound Med. Biol. 2011, 37, 312–320. [Google Scholar] [CrossRef] [Green Version]
- Granata, A.; Zanoli, L.; Insalaco, M.; Valentino, M.; Pavlica, P.; Di Nicolò, P.P.; Scuderi, M.; Fiorini, F.; Fatuzzo, P.; Bertolotto, M. Contrast-Enhanced Ultrasound (CEUS) in Nephrology: Has the Time Come for Its Widespread Use? Clin. Exp. Nephrol. 2015, 19, 606–615. [Google Scholar] [CrossRef]
- Bosniak, M.A. The current radiological approach to renal cysts. Radiology 1986, 158, 1–10. [Google Scholar] [CrossRef]
- Israel, G.M.; Bosniak, M.A. How I Do It: Evaluating Renal Masses. Radiology 2005, 236, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Sevcenco, S.; Spick, C.; Helbich, T.H.; Heinz, G.; Shariat, S.F.; Klingler, H.C.; Rauchenwald, M.; Baltzer, P.A. Malignancy Rates and Diagnostic Performance of the Bosniak Classification for the Diagnosis of Cystic Renal Lesions in Computed Tomography—A Systematic Review and Meta-Analysis. Eur. Radiol. 2017, 27, 2239–2247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertolotto, M.; Zappetti, R.; Cavallaro, M.; Perrone, R.; Perretti, L.; Cova, M.A. Characterization of Atypical Cystic Renal Masses With MDCT: Comparison of 5-Mm Axial Images and Thin Multiplanar Reconstructed Images. Am. J. Roentgenol. 2010, 195, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Ascenti, G.; Mazziotti, S.; Zimbaro, G.; Settineri, N.; Magno, C.; Melloni, D.; Caruso, R.; Scribano, E. Complex Cystic Renal Masses: Characterization with Contrast-Enhanced US. Radiology 2007, 243, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Bosniak, M.A. Difficulties in Classifying Cystic Lesions of the Kidney. Urol. Radiol. 1991, 13, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Cantisani, V.; Bertolotto, M.; Clevert, D.-A.; Correas, J.-M.; Drudi, F.M.; Fischer, T.; Gilja, O.H.; Granata, A.; Graumann, O.; Harvey, C.J.; et al. EFSUMB 2020 Proposal for a Contrast-Enhanced Ultrasound-Adapted Bosniak Cyst Categorization—Position Statement. Ultraschall Med. 2020, 1300–1727. [Google Scholar] [CrossRef]
- Silverman, S.G.; Pedrosa, I.; Ellis, J.H.; Hindman, N.M.; Schieda, N.; Smith, A.D.; Remer, E.M.; Shinagare, A.B.; Curci, N.E.; Raman, S.S.; et al. Bosniak Classification of Cystic Renal Masses, Version 2019: An Update Proposal and Needs Assessment. Radiology 2019, 292, 475–488. [Google Scholar] [CrossRef] [Green Version]
- Bertolotto, M.; Cicero, C.; Perrone, R.; Degrassi, F.; Cacciato, F.; Cova, M.A. Renal Masses with Equivocal Enhancement at CT: Characterization With Contrast-Enhanced Ultrasound. Am. J. Roentgenol. 2015, 204, W557–W565. [Google Scholar] [CrossRef]
- Bertolotto, M.; Derchi, L.E.; Cicero, C.; Iannelli, M. Renal Masses as Characterized by Ultrasound Contrast. Ultrasound Clin. 2013, 8, 581–592. [Google Scholar] [CrossRef]
- Bertolotto, M.; Bucci, S.; Valentino, M.; Currò, F.; Sachs, C.; Cova, M.A. Contrast-Enhanced Ultrasound for Characterizing Renal Masses. Eur. J. Radiol. 2018, 105, 41–48. [Google Scholar] [CrossRef]
- King, K.G. Use of Contrast Ultrasound for Renal Mass Evaluation. Radiol. Clin. N. Am. 2020, 58, 935–949. [Google Scholar] [CrossRef]
- Bhatt, S.; MacLennan, G.; Dogra, V. Renal Pseudotumors. Am. J. Roentgenol. 2007, 188, 1380–1387. [Google Scholar] [CrossRef]
- Ascenti, G.; Zimbaro, G.; Mazziotti, S.; Gaeta, M.; Lamberto, S.; Scribano, E. Contrast-Enhanced Power Doppler US in the Diagnosis of Renal Pseudotumors. Eur. Radiol. 2001, 11, 2496–2499. [Google Scholar] [CrossRef]
- Bertolotto, M.; Cicero, C.; Catalano, O.; Currò, F.; Derchi, L.E. Solid Renal Tumors Isoenhancing to Kidneys on Contrast-Enhanced Sonography: Differentiation from Pseudomasses: Isoenhancing Tumors and Pseudomasses on Contrast-Enhanced Sonography. J. Ultrasound Med. 2018, 37, 233–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granata, A.; Floccari, F.; Insalaco, M.; Clementi, A.; Di Lullo, L.; D’Amelio, A.; Zamboli, P.; Logias, F.; Romano, M.; Fiorini, F. Ultrasound assessment in renal infections. G. Ital. Nefrol. Organo Uff. Della Soc. Ital. Nefrol. 2012, 29 (Suppl. S57), S47–S57. [Google Scholar]
- Jungberg, B.; Albiges, L.; Bedke, J.; Bex, A.; Capitanio, U.; Giles, R.H.; Hora, M.; Klatte, T.; Lam, T.; Marconi, L.; et al. EAU Guidelines on Renal Cell Carcinoma 2021. In Proceedings of the EAU Annual Congress, Amsterdam, The Netherlands, 8–12 July 2021; European Association of Urology Guidelines Office: Arnhem, The Netherlands, 2021. [Google Scholar]
- Meloni, M.F.; Bertolotto, M.; Alberzoni, C.; Lazzaroni, S.; Filice, C.; Livraghi, T.; Ferraioli, G. Follow-Up After Percutaneous Radiofrequency Ablation of Renal Cell Carcinoma: Contrast-Enhanced Sonography Versus Contrast-Enhanced CT or MRI. Am. J. Roentgenol. 2008, 191, 1233–1238. [Google Scholar] [CrossRef] [PubMed]
- Bertolotto, M.; Siracusano, S.; Cicero, C.; Iannelli, M.; Silvestri, T.; Celia, A.; Guarise, A.; Stacul, F. Cryotherapy of Renal Lesions: Enhancement on Contrast-Enhanced Sonography on Postoperative Day 1 Does Not Imply Viable Tissue Persistence: Early Contrast-Enhanced Sonography After Renal Tumor Cryoablation. J. Ultrasound Med. 2017, 36, 301–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertolotto, M.; Campo, I.; Sachs, C.; Ciabattoni, R.; Cicero, C.; Drudi, F.M.; Derchi, L.E.; Cova, M.A. Contrast-Enhanced Ultrasound after Successful Cryoablation of Benign and Malignant Renal Tumours: How Long Does Tumour Enhancement Persist? J. Med. Imaging Radiat. Oncol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Hoeffel, C.; Pousset, M.; Timsit, M.-O.; Elie, C.; Méjean, A.; Merran, S.; Tranquart, F.; Khairoune, A.; Joly, D.; Richard, S.; et al. Radiofrequency Ablation of Renal Tumours: Diagnostic Accuracy of Contrast-Enhanced Ultrasound for Early Detection of Residual Tumour. Eur. Radiol. 2010, 20, 1812–1821. [Google Scholar] [CrossRef]
- Bonkat, G.; Bartoletti, R.; Bruyère, F.; Cai, T.; Geerlings, S.E.; Köves, B.; Schubert, S.; Wagenlehner, F.; Devlies, W.; Horváth, J.; et al. EAU Guidelines on Urological-Infections-2021. In Proceedings of the EAU Annual Congress, Amsterdam, The Netherlands, 8–12 July 2021; European Association of Urology Guidelines Office: Arnhem, The Netherlands, 2021. [Google Scholar]
- Fontanilla, T.; Minaya, J.; Cortés, C.; Hernando, C.G.; Arangüena, R.P.; Arriaga, J.; Carmona, M.S.; Alcolado, A. Acute Complicated Pyelonephritis: Contrast-Enhanced Ultrasound. Abdom. Imaging 2012, 37, 639–646. [Google Scholar] [CrossRef]
- Yusuf, G.T.; Sellars, M.E.; Huang, D.Y.; Deganello, A.; Sidhu, P.S. Cortical Necrosis Secondary to Trauma in a Child: Contrast-Enhanced Ultrasound Comparable to Magnetic Resonance Imaging. Pediatr. Radiol. 2014, 44, 484–487. [Google Scholar] [CrossRef]
- Valentino, M.; Serra, C.; Zironi, G.; De Luca, C.; Pavlica, P.; Barozzi, L. Blunt Abdominal Trauma: Emergency Contrast-Enhanced Sonography for Detection of Solid Organ Injuries. Am. J. Roentgenol. 2006, 186, 1361–1367. [Google Scholar] [CrossRef]
- Valentino, M.; Ansaloni, L.; Catena, F.; Pavlica, P.; Pinna, A.D.; Barozzi, L. Contrast-Enhanced Ultrasonography in Blunt Abdominal Trauma: Considerations after 5 Years of Experience. Radiol. Med. 2009, 114, 1080–1093. [Google Scholar] [CrossRef] [PubMed]
- Ciccone, M.M.; Cortese, F.; Fiorella, A.; Scicchitano, P.; Cito, F.; Quistelli, G.; Pertosa, G.; D’Agostino, R.; Guida, P.; Favale, S. The clinical role of contrast-enhanced ultrasound in the evaluation of renal artery stenosis and diagnostic superiority as compared to traditional echo-color-Doppler flow imaging. Int. Angiol. 2011, 30, 135–139. [Google Scholar]
- Cui, Y.; Zhang, Q.; Yan, J.; Wu, J. The Value of Contrast-Enhanced Ultrasound versus Doppler Ultrasound in Grading Renal Artery Stenosis. BioMed Res. Int. 2020, 1–10. [Google Scholar] [CrossRef]
- Spiesecke, P.; Münch, F.; Fischer, T.; Hamm, B.; Lerchbaumer, M.H. Multiparametric Ultrasound Findings in Acute Kidney Failure Due to Rare Renal Cortical Necrosis. Sci. Rep. 2021, 11, 2060. [Google Scholar] [CrossRef] [PubMed]
- Dalla Palma, L.; Bertolotto, M. Introduction to Ultrasound Contrast Agents: Physics Overview. Eur. Radiol. 1999, 9, S338–S342. [Google Scholar] [CrossRef]
- Frinking, P.; Segers, T.; Luan, Y.; Tranquart, F. Three Decades of Ultrasound Contrast Agents: A Review of the Past, Present and Future Improvements. Ultrasound Med. Biol. 2020, 46, 892–908. [Google Scholar] [CrossRef] [Green Version]
- Segers, T.; Kruizinga, P.; Kok, M.P.; Lajoinie, G.; de Jong, N.; Versluis, M. Monodisperse Versus Polydisperse Ultrasound Contrast Agents: Non-Linear Response, Sensitivity, and Deep Tissue Imaging Potential. Ultrasound Med. Biol. 2018, 44, 1482–1492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deelman, L.E.; Declèves, A.-E.; Rychak, J.J.; Sharma, K. Targeted Renal Therapies through Microbubbles and Ultrasound. Adv. Drug Deliv. Rev. 2010, 62, 1369–1377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hull, T.D.; Agarwal, A.; Hoyt, K. New Ultrasound Techniques Promise Further Advances in AKI and CKD. J. Am. Soc. Nephrol. 2017, 28, 3452–3460. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, P.; Li, X.; Dong, Y.; Wu, S.; Xu, M.; Chen, X.; Wang, S.; Zheng, C.; Zou, C. Combination CTLA-4 Immunoglobulin Treatment and Ultrasound Microbubble-Mediated Exposure Improve Renal Function in a Rat Model of Diabetic Nephropathy. Aging 2021, 13, 8524–8540. [Google Scholar] [CrossRef] [PubMed]








Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Granata, A.; Campo, I.; Lentini, P.; Pesce, F.; Gesualdo, L.; Basile, A.; Cantisani, V.; Zeiler, M.; Bertolotto, M. Role of Contrast-Enhanced Ultrasound (CEUS) in Native Kidney Pathology: Limits and Fields of Action. Diagnostics 2021, 11, 1058. https://doi.org/10.3390/diagnostics11061058
Granata A, Campo I, Lentini P, Pesce F, Gesualdo L, Basile A, Cantisani V, Zeiler M, Bertolotto M. Role of Contrast-Enhanced Ultrasound (CEUS) in Native Kidney Pathology: Limits and Fields of Action. Diagnostics. 2021; 11(6):1058. https://doi.org/10.3390/diagnostics11061058
Chicago/Turabian StyleGranata, Antonio, Irene Campo, Paolo Lentini, Francesco Pesce, Loreto Gesualdo, Antonio Basile, Vito Cantisani, Matthias Zeiler, and Michele Bertolotto. 2021. "Role of Contrast-Enhanced Ultrasound (CEUS) in Native Kidney Pathology: Limits and Fields of Action" Diagnostics 11, no. 6: 1058. https://doi.org/10.3390/diagnostics11061058
APA StyleGranata, A., Campo, I., Lentini, P., Pesce, F., Gesualdo, L., Basile, A., Cantisani, V., Zeiler, M., & Bertolotto, M. (2021). Role of Contrast-Enhanced Ultrasound (CEUS) in Native Kidney Pathology: Limits and Fields of Action. Diagnostics, 11(6), 1058. https://doi.org/10.3390/diagnostics11061058





