Pacemaker Implantation in a Patient with Isolated Persistent Left Superior Vena Cava Draining into the Left Atrium: A Case Report and Brief Literature Review
Abstract
:1. Introduction
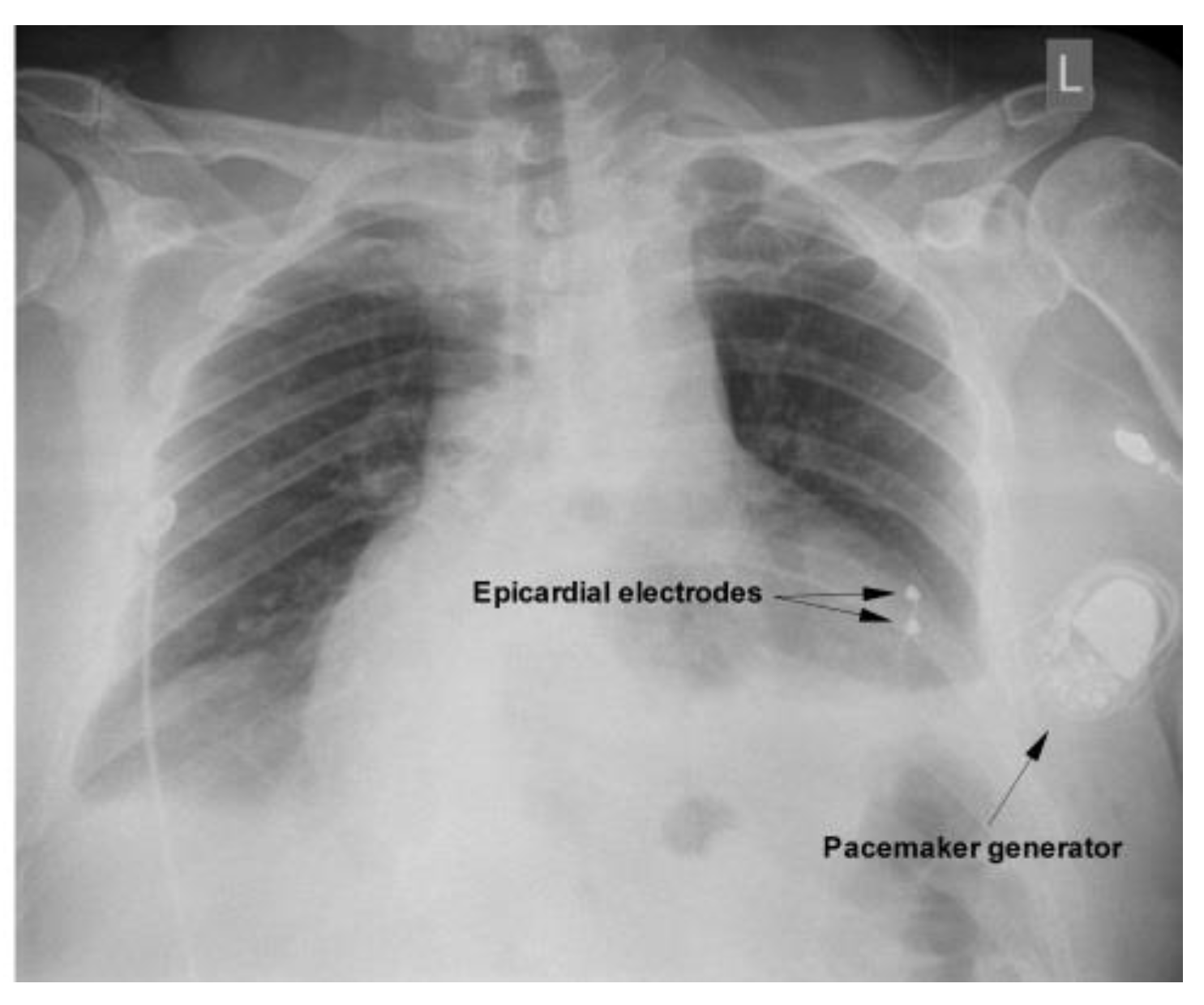
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Ratliff, H.L.; Yousufuddin, M.; Lieving, W.R.; Watson, B.E.; Malas, A.; Rosencrance, G.; McCowan, R.J. Persistent left superior vena cava: Case reports and clinical implications. Int. J. Cardiol. 2006, 10, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, A.S.; Mazhar, S. Persistent left superior vena cava with absent right superior vena cava: Review of the literature and clinical implications. Echocardiography 2014, 31, 674–679. [Google Scholar] [CrossRef] [PubMed]
- von Bismarck, A.; Weinberger, T.; Steffen, J. Images in Vascular Medicine: Vena cava syndrome mimicking caput medusae. Vasc. Med. 2021, 26, 672–673. [Google Scholar] [CrossRef] [PubMed]
- Demșa, I.; Crișu, D.; Haba, C.M.Ș.; Ursaru, A.M.; Afrăsânie, V.A.; Costache, I.I.; Petriș, A.O.; Tesloianu, D.N. Persistent Left Superior Vena Cava with Absent Right Superior Vena Cava and Discrete Subaortic Stenosis Diagnosed in a Patient with Sick Sinus Syndrome: A Case Report and Brief Review of the Literature. Diagnostics 2020, 19, 847. [Google Scholar] [CrossRef] [PubMed]
- Lendzian, T.; Vogt, J.; Krasemann, T. Are anomalies of the caval veins more common in complex congenital heart disease? Herz 2007, 32, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Bostan, A.; Astratinei, D.D.; Tăbăcaru, N.; Ailoaei, S.; Stătescu, C. Permanent pacemaker implantation in a challenging anatomy: Persistent left superior vena cava. Arch. Clin. Cases 2021, 27, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Yousaf, M.; Malak, S.F. Left Atrial Drainage of a Persistent Left Superior Vena Cava. Radiol. Case Rep. 2015, 7, 225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duymus, M.; Yesilkaya, Y.; Orman, G.; Bozkurt, A.; Yilmaz, O. Persistent left superior vena cava draining to the left atrium: A case report and review of the literature. Pol. J. Radiol. 2012, 77, 65–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Metzler, B.; Hillebrand, H.; Eulenbruch, H.P.; Dierkesmann, R.; Hust, M.H. Persistent left superior vena cava with right-left shunt into the left atrium. Dtsch. Med. Wochenschr. 2002, 18, 83–86. [Google Scholar] [CrossRef]
- Kuhn, A.; Hauser, M.; Eicken, A.; Vogt, M. Right heart failure due to an unroofed coronary sinus in an adult. Int. J. Cardiol. 2006, 10, 248–249. [Google Scholar] [CrossRef]
- Erol, I.; Cetin, I.I.; Alehan, F.; Varan, B.; Ozkan, S.; Agildere, M.; Tokel, K. Brain abscess associated with isolated left superior vena cava draining into the left atrium in the absence of coronary sinus and atrial septal defect. Cardiovasc. Interv. Radiol. 2006, 29, 454–456. [Google Scholar] [CrossRef] [PubMed]
- De Geest, B.; Vandommele, J.; Herregods, M.C.; Vanhaecke, J.; Gewillig, M.; Daenen, W.; Plets, C.; De Geest, H. Isolated left sided superior vena cava draining into the left atrium associated with recurring intracerebral abscesses. A case report. Acta Cardiol. 1994, 49, 175–182. [Google Scholar]
- Luca, C.T.; Crisan, S.; Cozma, D.; Negru, A.; Lazar, M.A.; Vacarescu, C.; Trofenciuc, M.; Rachieru, C.; Craciun, L.M.; Gaita, D.; et al. Arterial Hypertension: Individual Therapeutic Approaches-From DNA Sequencing to Gender Differentiation and New Therapeutic Targets. Pharmaceutics 2021, 13, 856. [Google Scholar] [CrossRef]
- Geva, T. Thoracic Key Home Page. Available online: https://thoracickey.com/abnormal-systemic-venousconnections (accessed on 18 August 2022).
- Recto, M.R.; Sadlo, H.; Sobczyk, W.L. Rare case of persistent left superior vena cava to left upper pulmonary vein: Pathway for paradoxical embolization and development of transient ischemic attack and subsequent occlusion with an amplatzer vascular plug. J. Invasive Cardiol. 2007, 19, E313–E316. [Google Scholar] [PubMed]
- Gupta, S.K.; Juneja, R.; Anderson, R.H.; Gulati, G.S.; Devagorou, V. Clarifying the anatomy and physiology of totally anomalous systemic venous connection. Ann. Pediatr. Cardiol. 2017, 10, 269–277. [Google Scholar] [CrossRef]
- Batouty, N.M.; Sobh, D.M.; Gadelhak, B.; Sobh, H.M.; Mahmoud, W.; Tawfik, A.M. Left superior vena cava: Cross-sectional imaging overview. Radiol. Med. 2020, 125, 237–246. [Google Scholar] [CrossRef]
- Clark, C.; MacDonald, L. Right-sided superior vena cava draining into the left atrium in a patient with persistent left-sided superior vena cava emptying into the right atrium diagnosed by echocardiography. Proc. (Bayl. Univ. Med. Cent.) 2015, 28, 365–366. [Google Scholar] [CrossRef] [Green Version]
- Ichikawa, T.; Hara, T.; Koizumi, J.; Nakamura, N.; Nagafuji, Y.; Furuya, H.; Mikami, T.; Kuroki, T.; Hashimoto, J. Persistent left superior vena cava with absent right superior vena cava in adults: CT and clinical findings. Jpn. J. Radiol. 2020, 38, 1046–1051. [Google Scholar] [CrossRef] [PubMed]
- Morgan, D.R.; Hanratty, C.G.; Dixon, L.J.; Trimble, M.; O’Keeffe, D.B. Anomalies of cardiac venous drainage associated with abnormalities of cardiac conduction system. Europace 2002, 4, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Doig, J.C.; Saito, J.; Harris, L.; Downar, E. Coronary sinus morphology in patients with atrioventricular junctional reentry tachycardia and other supraventricular tachyarrhythmias. Circulation 1995, 92, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Momma, K.; Linde, L.M. Abnormal rhythms associated with persistent left superior vena cava. Pediatr. Res. 1969, 3, 210–216. [Google Scholar] [CrossRef]
- Biffi, M.; Bertini, M.; Ziacchi, M.; Martignani, C.; Valzania, C.; Diemberger, I.; Branzi, A.; Boriani, G. Clinical implications of left superior vena cava persistence in candidates for pacemaker or cardioverter-defibrillator implantation. Heart Vessel. 2009, 24, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Rathakrishnan, S.S.; Kaliappan, T.; Gopalan, R. Beware of Venous Anomalies in Young Patients with Sick Sinus Syndrome: A Report of Two Cases of Sick Sinus Syndrome with Systemic Venous Anomalies. Heart Views 2015, 16, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Biffi, M.; Boriani, G.; Frabetti, L.; Bronzetti, G. Branzi, A. Left superior vena cava persistence in patients undergoing pacemaker or cardioverter-defibrillator implantation: A 10-year experience. Chest 2001, 120, 139–144. [Google Scholar] [CrossRef] [Green Version]
- Dąbrowski, P.; Obszański, B.; Kleinrok, A.; Kutarski, A. Long-term follow-up after pacemaker implantation via persistent left superior vena cava. Cardiol. J. 2014, 21, 413–418. [Google Scholar] [CrossRef] [Green Version]
- Li, T.; Xu, Q.; Liao, H.T.; Asvestas, D.; Letsas, K.P.; Li, Y. Transvenous dual-chamber pacemaker implantation in patients with persistent left superior vena cava. BMC Cardiovasc. Disord. 2019, 29, 100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sirugo, P.; Marchini, F.; Bertini, M.; Malagù, M. Dual chamber pacemaker implantation via both right and persistent left superior vena cava. A case report. Eur. Heart J. Case Rep. 2022, 6, ytac296. [Google Scholar] [CrossRef] [PubMed]
- Razi, M.; Madaan, A.; Goel, A.; Sinha, S.K. Troubleshooting during pacemaker implant in persistent left superior vena cava with absence of right superior vena cava (isolated persistent left superior vena cava). Avicenna J. Med. 2016, 6, 47–50. [Google Scholar] [CrossRef]
- Guenther, M.; Kolschmann, S.; Rauwolf, T.P.; Christoph, M.; Sandfort, V.; Strasser, R.H.; Wunderlich, C. Implantable cardioverter defibrillator lead implantation in patients with a persistent left superior vena cava—Feasibility, chances, and limitations: Representative cases in adults. Europace 2013, 15, 273–277. [Google Scholar] [CrossRef]
- Kahaly, O.R.; Afzal, M.R.; Okabe, T.; Houmsse, M. An Uncommon Dilemma: Cardiac Resynchronization Therapy in Patients with Persistent Left Superior Vena Cava Draining into the Coronary Sinus. J. Atr. Fibrillation 2020, 31, 2339. [Google Scholar] [CrossRef]
- Parikh, M.G.; Halleran, S.M.; Bharati, S.; Trohman, R.G. Successful percutaneous cardiac resynchronization despite an occlusive Thebesian valve. Pediatr. Cardiol. 2011, 32, 1223–1227. [Google Scholar] [CrossRef]
- Gupta, A.; Halleran, S.M.; Krishnan, K.; Trohman, R.G. Rescue permanent iliac vein pacing after epicardial lead failure: An unusual reversal of pacing fortune. Europace 2008, 10, 1236–1238. [Google Scholar] [CrossRef]
- Benz, D.C.; Krasniqi, N.; Wagnetz, U.; Stieger, R.; Tanner, F.C.; Eriksson, U. Isolated persistent left superior vena cava draining into the left atrium of an otherwise normal heart. Eur. Heart J. 2013, 34, 1505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hulten, E.A.; Pinto, G.; Weissman, G.; Fuisz, A. Anomalous vena caval return to the left atrium. Circulation 2012, 3, e525–e528. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.W.; Duan, Q.J.; Gao, Z.; Ru, W.; Ying, L.Y. Total anomalous systemic venous drainage to the left atrium. Ann. Thorac. Surg. 2009, 87, 1599–1601. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Totorean, I.-C.; Vacarescu, C.; Cozma, D.; Luca, C.-T.; Feier, H.; Lazăr, M.-A.; Deme, M.-A.; Stoica, S.; Arnautu, D.-A.; Gaiță, D. Pacemaker Implantation in a Patient with Isolated Persistent Left Superior Vena Cava Draining into the Left Atrium: A Case Report and Brief Literature Review. Diagnostics 2022, 12, 2707. https://doi.org/10.3390/diagnostics12112707
Totorean I-C, Vacarescu C, Cozma D, Luca C-T, Feier H, Lazăr M-A, Deme M-A, Stoica S, Arnautu D-A, Gaiță D. Pacemaker Implantation in a Patient with Isolated Persistent Left Superior Vena Cava Draining into the Left Atrium: A Case Report and Brief Literature Review. Diagnostics. 2022; 12(11):2707. https://doi.org/10.3390/diagnostics12112707
Chicago/Turabian StyleTotorean, Iuliana-Claudia, Cristina Vacarescu, Dragoș Cozma, Constantin-Tudor Luca, Horea Feier, Mihai-Andrei Lazăr, Maria-Anastasia Deme, Svetlana Stoica, Diana-Aurora Arnautu, and Dan Gaiță. 2022. "Pacemaker Implantation in a Patient with Isolated Persistent Left Superior Vena Cava Draining into the Left Atrium: A Case Report and Brief Literature Review" Diagnostics 12, no. 11: 2707. https://doi.org/10.3390/diagnostics12112707
APA StyleTotorean, I.-C., Vacarescu, C., Cozma, D., Luca, C.-T., Feier, H., Lazăr, M.-A., Deme, M.-A., Stoica, S., Arnautu, D.-A., & Gaiță, D. (2022). Pacemaker Implantation in a Patient with Isolated Persistent Left Superior Vena Cava Draining into the Left Atrium: A Case Report and Brief Literature Review. Diagnostics, 12(11), 2707. https://doi.org/10.3390/diagnostics12112707




