Expert Consensus Document: Diagnosis for Chronic Constipation with Faecal Retention in the Rectum Using Ultrasonography
Abstract
:1. Introduction
2. Methods
3. Protocol for the Observation of Rectal Faecal Impaction Using US
3.1. Subjects
3.2. Timing of the Observation
3.3. Observation Procedure
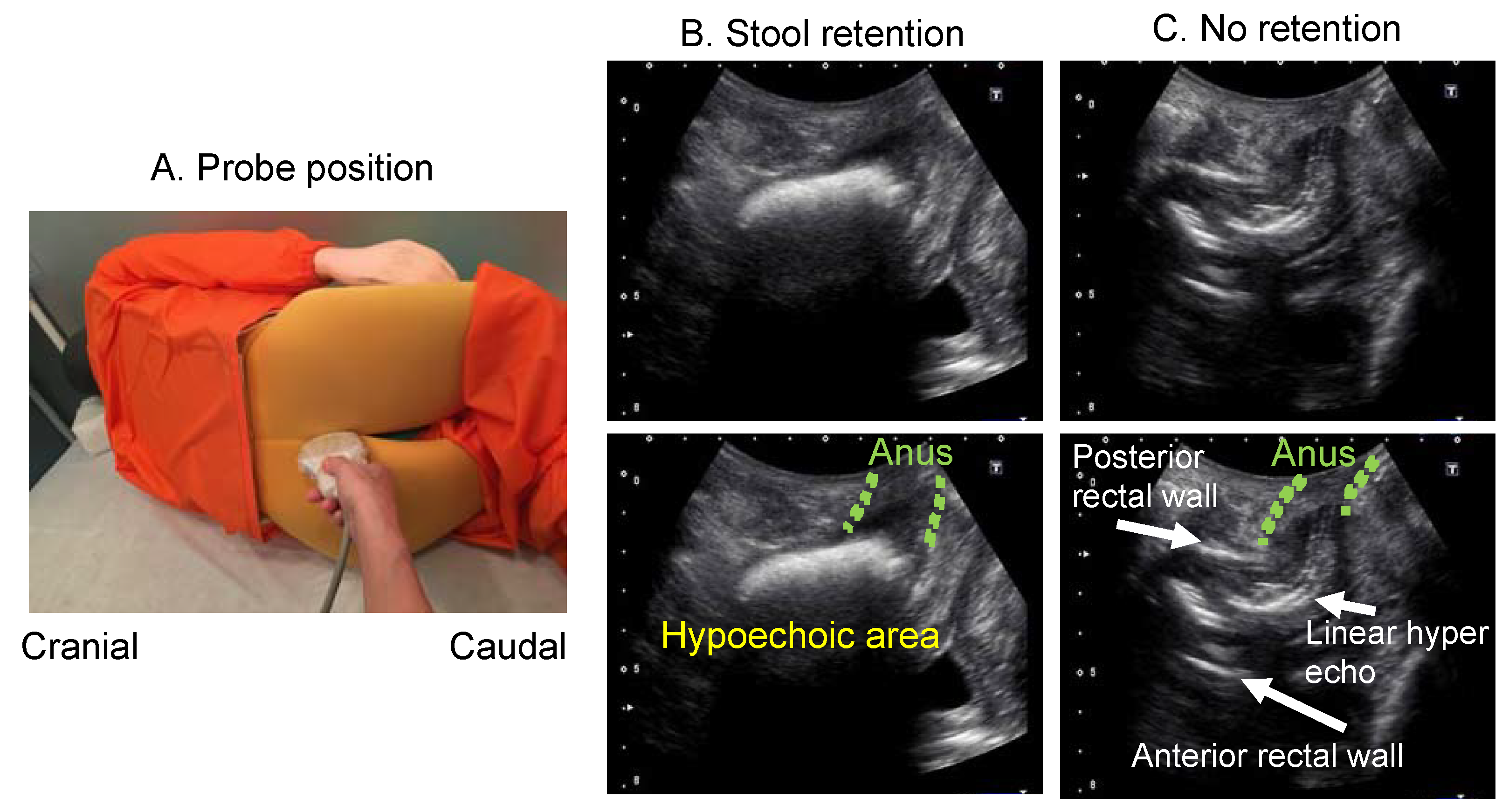
3.3.1. Position/Posture
3.3.2. US Devices
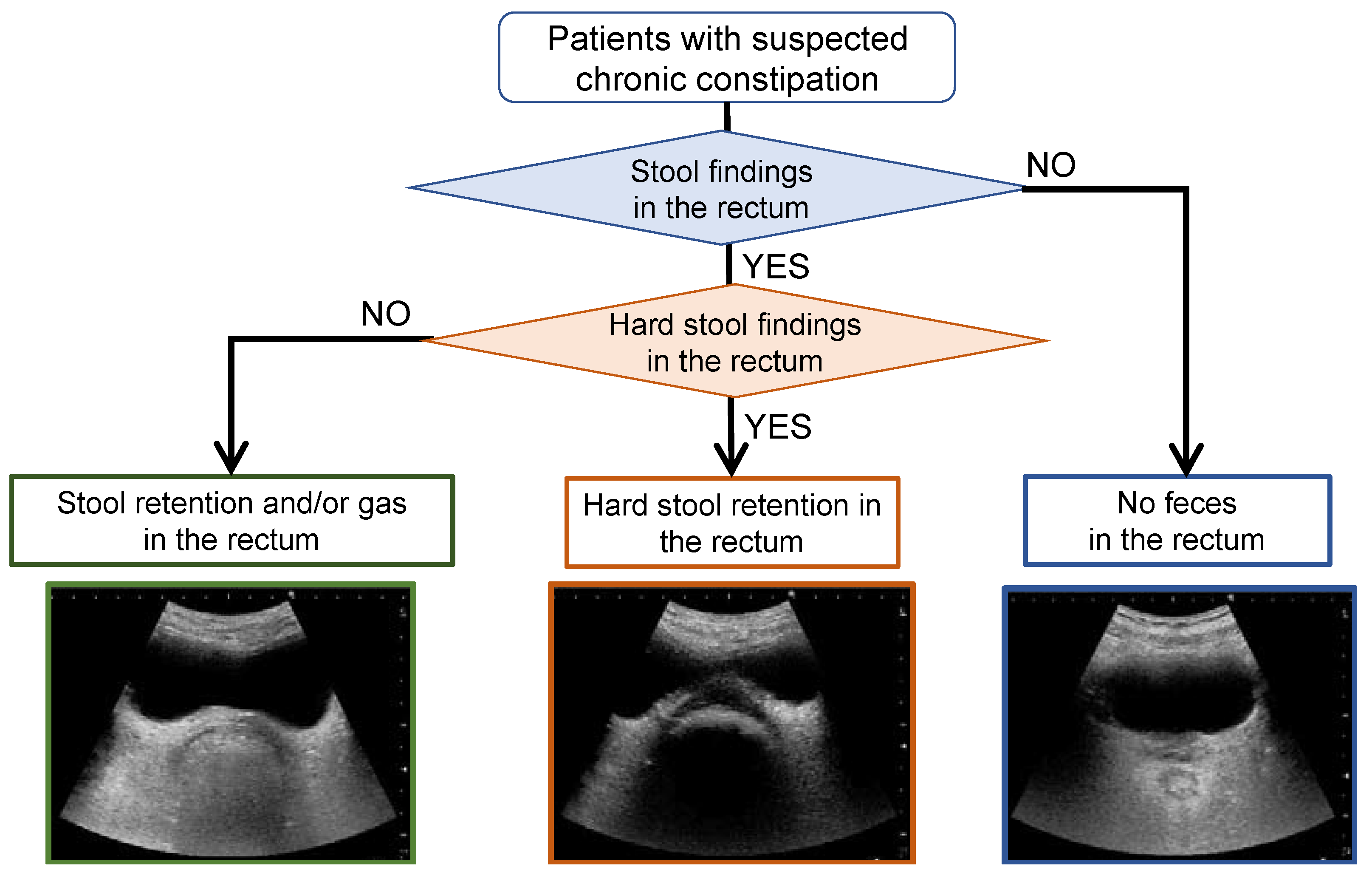
3.3.3. Flowchart of the Rectal US Observation
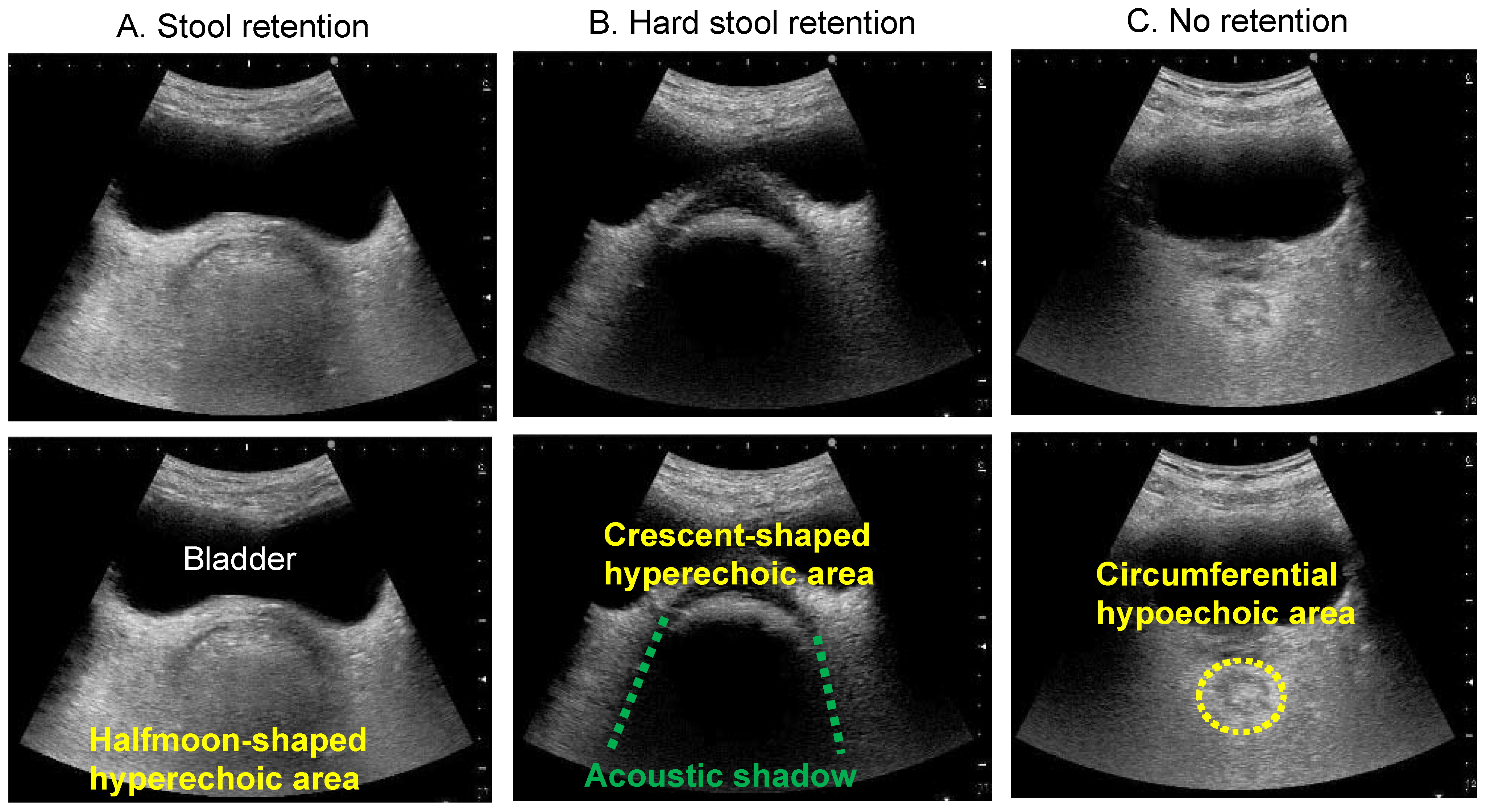
3.3.4. Probe Scanning and Typical Images
3.4. Findings That Need to Be Differentiated: Paradoxical Diarrhoea
3.5. Cases That Are Difficult to Observe
4. Future Challenges
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Bharucha, A.E.; Pemberton, J.H.; Locke, G.R., 3rd. American Gastroenterological Association technical review on constipation. Gastroenterology 2013, 144, 218–238. [Google Scholar] [CrossRef] [Green Version]
- Bouras, E.P.; Tangalos, E.G. Chronic constipation in the elderly. Gastroenterol. Clin. N. Am. 2009, 38, 463–480. [Google Scholar] [CrossRef]
- Camilleri, M.; Ford, A.C.; Mawe, G.M.; Dinning, P.G.; Rao, S.S.; Chey, W.D. Chronic constipation. Nat. Rev. Dis. Primers 2017, 3, 17095. [Google Scholar] [CrossRef]
- Suares, N.C.; Ford, A.C. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: Systematic review and meta-analysis. Am. J. Gastroenterol. 2011, 106, 1582–1591. [Google Scholar] [CrossRef]
- Sumida, K.; Molnar, M.Z.; Potukuchi, P.K.; Thomas, F.; Lu, J.L.; Yamagata, K. Constipation and risk of death and cardiovascular events. Atherosclerosis 2019, 281, 114–120. [Google Scholar] [CrossRef]
- Honkura, K.; Tomata, Y.; Sugiyama, K.; Kaiho, Y.; Watanabe, T.; Zhang, S. Defecation frequency and cardiovascular disease mortality in Japan: The Ohsaki cohort study. Atherosclerosis 2016, 246, 251–256. [Google Scholar] [CrossRef]
- Aziz, I.; Whitehead, W.E.; Palsson, O.S.; Törnblom, H.; Simrén, M. An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 39–46. [Google Scholar] [CrossRef] [Green Version]
- Seltzer, R. Evaluation and diagnosis of constipation. Gastroenterol. Nurs. 2012, 35, 343–348. [Google Scholar] [CrossRef]
- Remes-Troche, J.M.; Rao, S.S. Diagnostic testing in patients with chronic constipation. Curr. Gastroenterol. Rep. 2006, 8, 416–424. [Google Scholar] [CrossRef]
- Rao, S.S.; Ozturk, R.; Laine, L. Clinical utility of diagnostic tests for constipation in adults: A systematic review. Am. J. Gastroenterol. 2005, 100, 1605–1615. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.Y.; Tabbers, M.M.; Kurver, M.J.; Boluyt, N.; Benninga, M.A. Value of abdominal radiography, colonic transit time, and rectal ultrasound scanning in the diagnosis of idiopathic constipation in children: A systematic review. J. Pediatr. 2012, 161, e1–e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perniola, G.; Shek, C.; Chong, C.C.; Chew, S.; Cartmill, J.; Dietz, H.P. Defecation proctography and translabial ultrasound in the investigation of defecatory disorders. Ultrasound Obs. Gynecol. 2008, 31, 567–571. [Google Scholar] [CrossRef] [PubMed]
- Manabe, N.; Kamada, T.; Hata, J.; Haruma, K. New ultrasonographic evaluation of stool and/or gas distribution for treatment of chronic constipation. Int. J. Colorectal Dis. 2018, 33, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Manabe, N.; Kamada, T.; Kusunoki, H.; Hata, J.; Haruma, K. Usefulness of ultrasonographic evaluation of stool and/or gas distribution for the treatment strategy of chronic constipation. JGH Open 2019, 3, 310–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, S.; Yabunaka, K.; Matsumoto, M.; Tamai, N.; Noguchi, H.; Yoshida, M. Fecal Distribution Changes Using Colorectal Ultrasonography in Older People with Physical and Cognitive Impairment Living in Long-Term Care Facilities: A Longitudinal Observational Study. Healthcare 2018, 6, 55. [Google Scholar] [CrossRef] [Green Version]
- Matsumoto, M.; Yoshida, M.; Miura, Y.; Sato, N.; Okawa, Y.; Yamada, M. Feasibility of the constipation point-of-care ultrasound educational program in observing fecal retention in the colorectum: A descriptive study. Jpn. J. Nurs. Sci. 2021, 18, e12385. [Google Scholar] [CrossRef]
- Matsumoto, M.; Yoshida, M.; Yabunaka, K.; Nakagami, G.; Miura, Y.; Fujimaki, S. Safety and efficacy of a defecation care algorithm based on ultrasonographic bowel observation in Japanese home-care settings: A single-case, multiple-baseline study. Geriatr. Gerontol. Int. 2020, 20, 187–194. [Google Scholar] [CrossRef]
- Di Pace, M.R.; Catalano, P.; Caruso, A.M.; Bommarito, D.; Casuccio, A.; Cimador, M. Is rectal disimpact always necessary in children with chronic constipation? Evaluation with pelvic ultrasound. Pediatr. Surg. Int. 2010, 26, 601–606. [Google Scholar] [CrossRef]
- Karaman, A.; Ramadan, S.U.; Karaman, I.; Gokharman, D.; Erdogan, D.; Kacar, M. Diagnosis and follow-up in constipated children: Should we use ultrasound? J. Pediatr. Surg. 2010, 45, 1849–1855. [Google Scholar] [CrossRef]
- Hatori, R.; Tomomasa, T.; Ishige, T.; Tatsuki, M.; Arakawa, H. Fecal retention in childhood: Evaluation on ultrasonography. Pediatr. Int. 2017, 59, 462–466. [Google Scholar] [CrossRef]
- Chumpitazi, B.P.; Self, M.M.; Czyzewski, D.I.; Cejka, S.; Swank, P.R.; Shulman, R.J. Bristol Stool Form Scale reliability and agreement decreases when determining Rome III stool form designations. Neurogastroenterol. Motil. 2016, 28, 443–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yabunaka, K.; Matsumoto, M.; Yoshida, M.; Tanaka, S.; Miura, Y.; Tsutaoka, T. Assessment of rectal feces storage condition by a point-of-care pocket-size ultrasound device for healthy adult subjects: A preliminary study. Drug Discov. 2018, 12, 42–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, R.A.; Pops, M.A. Paradoxical diarrhea with opiates. JAMA 1968, 205, 802–803. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.; Gundry, C.H. Paradoxical diarrhoea in childhood. Can. Med. Assoc. J. 1955, 72, 362–368. [Google Scholar]
- Serrano Falcón, B.; Barceló López, M.; Mateos Muñoz, B.; Álvarez Sánchez, A.; Rey, E. Fecal impaction: A systematic review of its medical complications. BMC Geriatr. 2016, 16, 4. [Google Scholar] [CrossRef] [Green Version]
- Rao, S.S. Pathophysiology of adult fecal incontinence. Gastroenterology 2004, 126 (Suppl. 1), S14–S22. [Google Scholar] [CrossRef]
- Müller-Lissner, S. General geriatrics and gastroenterology: Constipation and faecal incontinence. Best Pr. Res Clin. Gastroenterol. 2002, 16, 115–133. [Google Scholar] [CrossRef]
- Dahl, J.J.; Sheth, N.M. Reverberation clutter from subcutaneous tissue layers: Simulation and in vivo demonstrations. Ultrasound Med. Biol. 2014, 40, 714–726. [Google Scholar] [CrossRef] [Green Version]
- Perez, F.; Accarino, A.; Azpiroz, F.; Quiroga, S.; Malagelada, J.R. Gas distribution within the human gut: Effect of meals. Am. J. Gastroenterol. 2007, 102, 842–849. [Google Scholar] [CrossRef]
- Sano, Y.; Muto, M.; Urata, K.; Akiyama, K. The study of feces property assessment with the ultrasonography: Usefulness of lower rectum assessment by intergluteal cleft approach scanning method. Jpn. J. Med. Ultrasound Technol. 2020, 45, 168–174. [Google Scholar]
- Matsumoto, M.; Tsutaoka, T.; Nakagami, G.; Tanaka, S.; Yoshida, M.; Miura, Y. Deep learning-based classification of rectal fecal retention and analysis of fecal properties using ultrasound images in older adult patients. Jpn. J. Nurs. Sci. 2020, 17, e12340. [Google Scholar] [CrossRef] [PubMed]
- Grossi, U.; Horrocks, E.J.; Mason, J.; Knowles, C.H.; Williams, A.B.; NIHR CapaCiTY Working Group; Pelvic Floor Society. Surgery for constipation: Systematic review and practice recommendations: Results IV: Recto-vaginal reinforcement procedures. Colorectal. Dis. 2017, 3, 73–91. [Google Scholar] [CrossRef] [PubMed]
- Knowles, C.H.; Grossi, U.; Chapman, M.; Mason, J.; NIHR CapaCiTY Working Group; Pelvic Floor Society. Surgery for constipation: Systematic review and practice recommendations: Results I: Colonic resection. Colorectal. Dis. 2017, 3, 17–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Picciariello, A.; O’Connell, P.R.; Hahnloser, D.; Gallo, G.; Munoz-Duyos, A.; Schwandner, O. Obstructed defaecation syndrome: European consensus guidelines on the surgical management. Br. J. Surg. 2021, 108, 1149–1153. [Google Scholar] [CrossRef]
- Corsetti, M.; Brown, S.; Chiarioni, G.; Dimidi, E.; Dudding, T.; Emmanuel, A. Chronic constipation in adults: Contemporary perspectives and clinical challenges. 2: Conservative, behavioural, medical and surgical treatment. Neurogastroenterol. Motil. 2021, 33, e14070. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsumoto, M.; Misawa, N.; Tsuda, M.; Manabe, N.; Kessoku, T.; Tamai, N.; Kawamoto, A.; Sugama, J.; Tanaka, H.; Kato, M.; et al. Expert Consensus Document: Diagnosis for Chronic Constipation with Faecal Retention in the Rectum Using Ultrasonography. Diagnostics 2022, 12, 300. https://doi.org/10.3390/diagnostics12020300
Matsumoto M, Misawa N, Tsuda M, Manabe N, Kessoku T, Tamai N, Kawamoto A, Sugama J, Tanaka H, Kato M, et al. Expert Consensus Document: Diagnosis for Chronic Constipation with Faecal Retention in the Rectum Using Ultrasonography. Diagnostics. 2022; 12(2):300. https://doi.org/10.3390/diagnostics12020300
Chicago/Turabian StyleMatsumoto, Masaru, Noboru Misawa, Momoko Tsuda, Noriaki Manabe, Takaomi Kessoku, Nao Tamai, Atsuo Kawamoto, Junko Sugama, Hideko Tanaka, Mototsugu Kato, and et al. 2022. "Expert Consensus Document: Diagnosis for Chronic Constipation with Faecal Retention in the Rectum Using Ultrasonography" Diagnostics 12, no. 2: 300. https://doi.org/10.3390/diagnostics12020300
APA StyleMatsumoto, M., Misawa, N., Tsuda, M., Manabe, N., Kessoku, T., Tamai, N., Kawamoto, A., Sugama, J., Tanaka, H., Kato, M., Haruma, K., Sanada, H., & Nakajima, A. (2022). Expert Consensus Document: Diagnosis for Chronic Constipation with Faecal Retention in the Rectum Using Ultrasonography. Diagnostics, 12(2), 300. https://doi.org/10.3390/diagnostics12020300






