Dynamic Change of Albumin-Bilirubin Score Is Good Predictive Parameter for Prognosis in Chronic Hepatitis C-hepatocellular Carcinoma Patients Receiving Transarterial Chemoembolization
Abstract
:1. Introduction
2. Patients and Methods
2.1. Patient Selection
2.2. Treatment Procedure
2.3. Assessment of Treatment Responses Using mRECIST Guidelines
2.4. Laboratory Methods
2.5. Follow-Up Protocol
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics and Follow-Up Results
3.2. Determining the Risk Factors Affecting Mortality
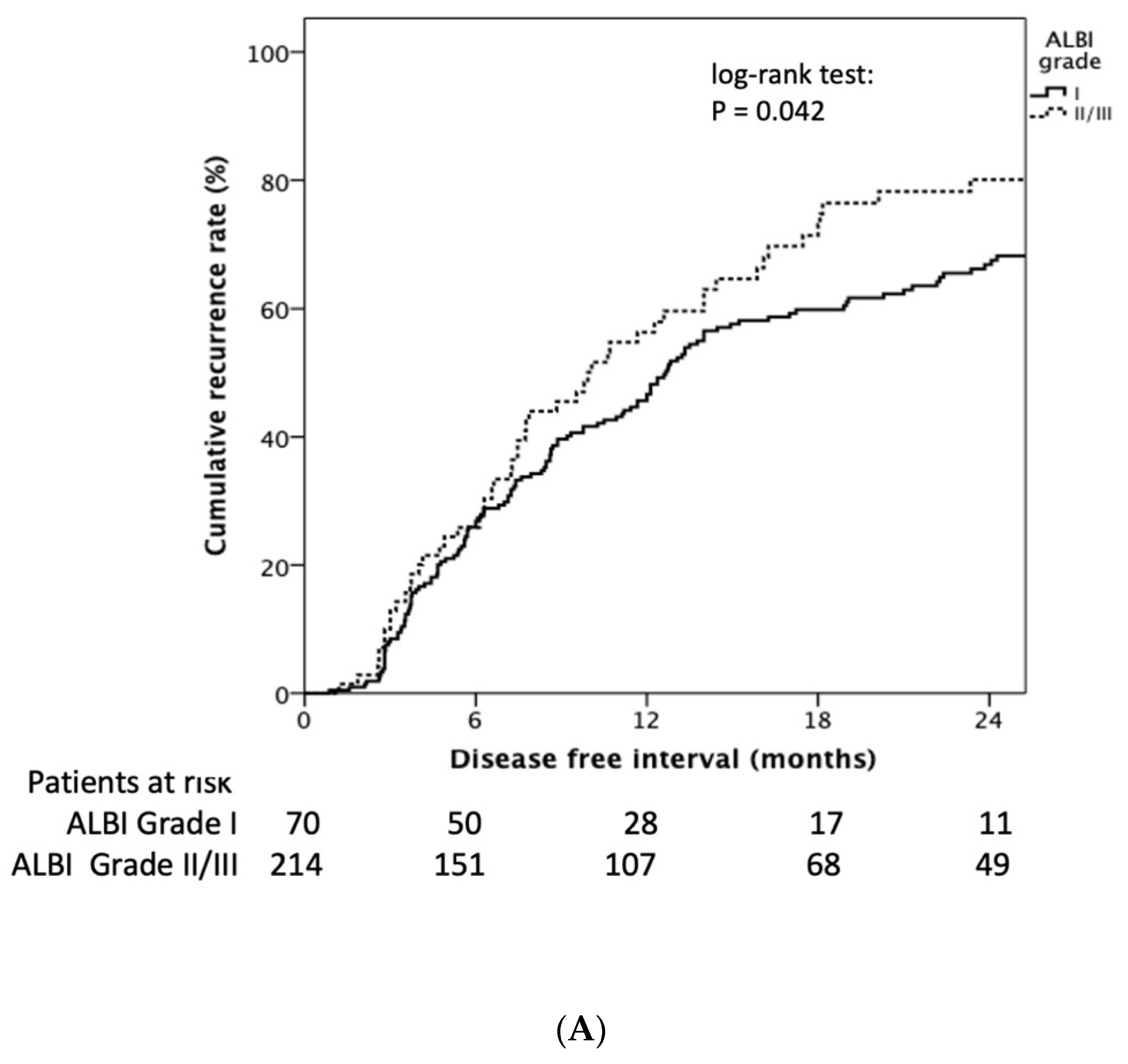
3.3. Determining the Risk Factors Affecting Tumor Recurrence
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Global Burden of Disease Cancer Collaborat; Fitzmaurice, C.; Akinyemiju, T.F.; Al Lami, F.H.; Alam, T.; Alizadeh-Navaei, R.; Allen, C.; Alsharif, U.; Alvis-Guzman, N.; Amini, E.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2016: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2018, 4, 1553–1568. [Google Scholar] [PubMed]
- Walter, S.R.; Thein, H.H.; Gidding, H.F.; Amin, J.; Law, M.G.; George, J.; Dore, G.J. Risk factors for hepatocellular carcinoma in a cohort infected with hepatitis B or C. J. Gastroenterol. Hepatol. 2011, 26, 1757–1764. [Google Scholar] [CrossRef] [PubMed]
- Durand, F.; Valla, D. Assessment of prognosis of cirrhosis. Semin. Liver Dis. 2008, 28, 110–122. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.J.; Berhane, S.; Kagebayashi, C.; Satomura, S.; Teng, M.; Reeves, H.L.; O’Beirne, J.; Fox, R.; Skowronska, A.; Palmer, D.; et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade. J. Clin. Oncol. 2015, 33, 550–558. [Google Scholar] [CrossRef]
- Pinato, D.J.; Sharma, R.; Allara, E.; Yen, C.; Arizumi, T.; Kubota, K.; Bettinger, D.; Jang, J.W.; Smirne, C.; Kim, Y.W.; et al. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma. J. Hepatol. 2017, 66, 338–346. [Google Scholar] [CrossRef] [Green Version]
- Tipaldi, M.A.; Ronconi, E.; Lucertini, E.; Krokidis, M.; Zerunian, M.; Polidori, T.; Begini, P.; Marignani, M.; Mazzuca, F.; Caruso, D.; et al. Hepatocellular Carcinoma Drug-Eluting Bead Transarterial Chemoembolization (DEB-TACE): Outcome Analysis Using a Model Based On Pre-Treatment CT Texture Features. Diagnostics 2021, 11, 956. [Google Scholar] [CrossRef]
- Shiozawa, K.; Matsui, T.; Murakami, T.; Watanabe, M.; Maetani, I. Predicting Therapeutic Efficacy of Transarterial Chemoembolization with Drug-Eluting Beads for Hepatocellular Carcinoma Using Contrast-Enhanced Ultrasound. Diagnostics 2021, 11, 291. [Google Scholar] [CrossRef]
- Llovet, J.M.; Real, M.I.; Montaña, X.; Planas, R.; Coll, S.; Aponte, J.; Ayuso, C.; Sala, M.; Muchart, J.; Solà, R.; et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: A randomised controlled trial. Lancet 2002, 359, 1734–1739. [Google Scholar] [CrossRef]
- Lo, C.-M.; Ngan, H.; Tso, W.-K.; Liu, C.-L.; Lam, C.-M.; Poon, R.T.-P.; Fan, S.-T.; Wong, J. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 2002, 35, 1164–1171. [Google Scholar] [CrossRef]
- Facciorusso, A.; Bellanti, F.; Villani, R.; Salvatore, V.; Muscatiello, N.; Piscaglia, F.; Vendemiale, G.; Serviddio, G. Transarterial chemoembolization vs bland embolization in hepatocellular carcinoma: A meta-analysis of randomized trials. United Eur. Gastroenterol. J. 2017, 5, 511–518. [Google Scholar] [CrossRef]
- Shao, Y.Y.; Wang, S.Y.; Lin, S.M.; Diagnosis, G.; Systemic Therapy, G. Management consensus guideline for hepatocellular carcinoma: 2020 update on surveillance, diagnosis, and systemic treatment by the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan. J. Formos. Med. Assoc. 2021, 120, 1051–1060. [Google Scholar] [CrossRef] [PubMed]
- Waked, I.; Berhane, S.; Toyoda, H.; Chan, S.L.; Stern, N.; Palmer, D.; Tada, T.; Yeo, W.; Mo, F.; Bettinger, D.; et al. Transarterial chemo-embolisation of hepatocellular carcinoma: Impact of liver function and vascular invasion. Br. J. Cancer 2017, 116, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.-Y.; Liu, P.-H.; Hsu, C.-Y.; Hsia, C.-Y.; Lee, Y.-H.; Lee, R.-C.; Huang, Y.-H.; Lee, F.-Y.; Hou, M.-C.; Tsai, Y.-J.; et al. Prognostic role of noninvasive liver reserve markers in patients with hepatocellular carcinoma undergoing transarterial chemoembolization. PLoS ONE 2017, 12, e0180408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, I.-C.; Hung, Y.-W.; Liu, C.-A.; Lee, R.-C.; Su, C.-W.; Huo, T.-I.; Li, C.-P.; Chao, Y.; Lin, H.-C.; Hou, M.-C.; et al. A New ALBI-based Model to Predict Survival After Transarterial Chemoembolization for BCLC Stage B Hepatocellular Carcinoma. Liver Int. 2019, 39, 1704–1712. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL Clinical Practice Guidelines: Management of alcohol-related liver disease. J. Hepatol. 2018, 69, 154–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef]
- Teng, W.; Hsieh, Y.-C.; Lui, K.-W.; Chen, W.-T.; Hung, C.-F.; Huang, C.-H.; Chen, Y.-C.; Jeng, W.-J.; Lin, C.-C.; Lin, S.-M.; et al. Eradication of hepatitis C virus profoundly prolongs survival in hepatocellular carcinoma patients receiving transarterial chemoembolization. J. Viral Hepat. 2017, 24, 1160–1167. [Google Scholar] [CrossRef]
- Peng, C.W.; Teng, W.; Lui, K.W.; Hung, C.F.; Jeng, W.J.; Huang, C.H.; Chen, W.T.; Lin, C.-C.; Lin, C.-C.; Lin, S.M.; et al. Complete response at first transarterial chemoembolization predicts favorable outcome in hepatocellular carcinoma. Am. J. Cancer Res. 2021, 11, 4956–4965. [Google Scholar]
- Lin, P.-T.; Teng, W.; Jeng, W.-J.; Hsieh, Y.-C.; Hung, C.-F.; Huang, C.-H.; Lui, K.-W.; Chen, Y.-C.; Lin, C.-C.; Lin, C.-Y.; et al. Add-on sorafenib is beneficial for hepatocellular carcinoma patients with transarterial chemoembolization refractoriness: A real-world experience. Eur. J. Gastroenterol. Hepatol. 2020, 32, 1192–1199. [Google Scholar] [CrossRef]
- Compagnone, G.; Giampalma, E.; Domenichelli, S.; Renzulli, M.; Golfieri, R. Calculation of conversion factors for effective dose for various interventional radiology procedures. Med. Phys. 2012, 39, 2491–2498. [Google Scholar] [CrossRef]
- Gillmore, R.; Stuart, S.; Kirkwood, A.; Hameeduddin, A.; Woodward, N.; Burroughs, A.K.; Meyer, T. EASL and mRECIST responses are independent prognostic factors for survival in hepatocellular cancer patients treated with transarterial embolization. J. Hepatol. 2011, 55, 1309–1316. [Google Scholar] [CrossRef]
- Tovoli, F.; Renzulli, M.; Negrini, G.; Brocchi, S.; Ferrarini, A.; Andreone, A.; Benevento, F.; Golfieri, R.; Morselli-Labate, A.M.; Mastroroberto, M.; et al. Inter-operator variability and source of errors in tumour response assessment for hepatocellular carcinoma treated with sorafenib. Eur. Radiol. 2018, 28, 3611–3620. [Google Scholar] [CrossRef]
- Mazzaferro, V.; Llovet, J.M.; Miceli, R.; Bhoori, S.; Schiavo, M.; Mariani, L.; Camerini, T.; Roayaie, S.; Schwartz, M.E.; Grazi, G.L.; et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: A retrospective, exploratory analysis. Lancet Oncol. 2009, 10, 35–43. [Google Scholar] [CrossRef]
- Jeong, S.O.; Kim, E.B.; Jeong, S.W.; Jang, J.Y.; Lee, S.H.; Kim, S.G.; Cha, S.W.; Kim, Y.S.; Cho, Y.D.; Kim, H.S.; et al. Predictive Factors for Complete Response and Recurrence after Transarterial Chemoembolization in Hepatocellular Carcinoma. Gut Liver 2017, 11, 409–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sieghart, W.; Hucke, F.; Pinter, M.; Graziadei, I.; Vogel, W.; Müller, C.; Heinzl, H.; Trauner, M.; Peck-Radosavljevic, M. The ART of decision making: Retreatment with transarterial chemoembolization in patients with hepatocellular carcinoma. Hepatology 2013, 57, 2261–2273. [Google Scholar] [CrossRef]
- Adhoute, X.; Penaranda, G.; Naude, S.; Raoul, J.L.; Perrier, H.; Bayle, O.; Monnet, O.; Beaurain, P.; Bazin, C.; Pol, B.; et al. Retreatment with TACE: The ABCR SCORE, an aid to the decision-making process. J. Hepatol. 2015, 62, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Kadalayil, L.; Benini, R.; Pallan, L.; O’Beirne, J.; Marelli, L.; Yu, D.; Hackshaw, A.; Fox, R.; Johnson, P.; Burroughs, A.K.; et al. A simple prognostic scoring system for patients receiving transarterial embolisation for hepatocellular cancer. Ann. Oncol. 2013, 24, 2565–2570. [Google Scholar] [CrossRef]
- Ogasawara, S.; Chiba, T.; Ooka, Y.; Kanogawa, N.; Motoyama, T.; Suzuki, E.; Tawada, A.; Azemoto, R.; Shinozaki, M.; Yoshikawa, M.; et al. A prognostic score for patients with intermediate-stage hepatocellular carcinoma treated with transarterial chemoembolization. PLoS ONE 2015, 10, e0125244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, B.K.; Shim, J.H.; Kim, S.U.; Park, J.Y.; Kim, D.Y.; Ahn, S.H.; Kim, K.M.; Lim, Y.-S.; Han, K.-H.; Lee, H.C. Risk prediction for patients with hepatocellular carcinoma undergoing chemoembolization: Development of a prediction model. Liver Int. 2016, 36, 92–99. [Google Scholar] [CrossRef]
- Pinato, D.J.; Yen, C.; Bettinger, D.; Ramaswami, R.; Arizumi, T.; Ward, C.; Pirisi, M.; Burlone, M.E.; Thimme, R.; Kudo, M.; et al. The albumin-bilirubin grade improves hepatic reserve estimation post-sorafenib failure: Implications for drug development. Aliment. Pharmacol. Ther. 2017, 45, 714–722. [Google Scholar] [CrossRef]
- Hiraoka, A.; Kumada, T.; Michitaka, K.; Toyoda, H.; Tada, T.; Ueki, H.; Kaneto, M.; Aibiki, T.; Okudaira, T.; Kawakami, T.; et al. Usefulness of albumin-bilirubin grade for evaluation of prognosis of 2584 Japanese patients with hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2016, 31, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, A.; Kumada, T.; Tsuji, K.; Takaguchi, K.; Itobayashi, E.; Kariyama, K.; Ochi, H.; Tajiri, K.; Hirooka, M.; Shimada, N.; et al. Validation of Modified ALBI Grade for More Detailed Assessment of Hepatic Function in Hepatocellular Carcinoma Patients: A Multicenter Analysis. Liver Cancer 2019, 8, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Oh, I.S.; Sinn, D.H.; Kang, T.W.; Lee, M.W.; Kang, W.; Gwak, G.-Y.; Paik, Y.-H.; Choi, M.S.; Lee, J.H.; Koh, K.C.; et al. Liver Function Assessment Using Albumin-Bilirubin Grade for Patients with Very Early-Stage Hepatocellular Carcinoma Treated with Radiofrequency Ablation. Dig. Dis. Sci. 2017, 62, 3235–3242. [Google Scholar] [CrossRef] [PubMed]
- Bekelis, K.; Bakhoum, S.F.; Desai, A.; Mackenzie, T.A.; Goodney, P.; Labropoulos, N. A risk factor-based predictive model of outcomes in carotid endarterectomy: The National Surgical Quality Improvement Program 2005–2010. Stroke 2013, 44, 1085–1090. [Google Scholar] [CrossRef] [Green Version]
- Saeki, I.; Yamasaki, T.; Yamashita, S.; Hanazono, T.; Urata, Y.; Furutani, T.; Yokoyama, Y.; Oishi, T.; Maeda, M.; Kimura, T.; et al. Early Predictors of Objective Response in Patients with Hepatocellular Carcinoma Undergoing Lenvatinib Treatment. Cancers 2020, 12, 779. [Google Scholar] [CrossRef] [Green Version]
- Hiraoka, A.; Kumada, T.; Kudo, M.; Hirooka, M.; Koizumi, Y.; Hiasa, Y.; Tajiri, K.; Toyoda, H.; Tada, T.; Ochi, H.; et al. Hepatic Function during Repeated TACE Procedures and Prognosis after Introducing Sorafenib in Patients with Unresectable Hepatocellular Carcinoma: Multicenter Analysis. Dig. Dis. 2017, 35, 602–610. [Google Scholar] [CrossRef]
- Nishiguchi, S.; Shiomi, S.; Nakatani, S.; Takeda, T.; Fukuda, K.; Tamori, A.; Habu, D.; Tanaka, T. Prevention of hepatocellular carcinoma in patients with chronic active hepatitis C and cirrhosis. Lancet 2001, 357, 196–197. [Google Scholar] [CrossRef]
- Manthravadi, S.; Paleti, S.; Pandya, P. Impact of sustained viral response postcurative therapy of hepatitis C-related hepatocellular carcinoma: A systematic review and meta-analysis. Int. J. Cancer 2017, 140, 1042–1049. [Google Scholar] [CrossRef]
- Reig, M.; Mariño, Z.; Perelló, C.; Iñarrairaegui, M.; Ribeiro, A.; Lens, S.; Díaz, A.; Vilana, R.; Darnell, A.; Varela, M.; et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J. Hepatol. 2016, 65, 719–726. [Google Scholar] [CrossRef] [Green Version]
- Conti, F.; Buonfiglioli, F.; Scuteri, A.; Crespi, C.; Bolondi, L.; Caraceni, P.; Foschi, F.G.; Lenzi, M.; Mazzella, G.; Verucchi, G.; et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J. Hepatol. 2016, 65, 727–733. [Google Scholar] [CrossRef]
- ANRS Collaborative Study Group on Hepatocellular Carcinoma. Lack of evidence of an effect of direct-acting antivirals on the recurrence of hepatocellular carcinoma: Data from three ANRS cohorts. J. Hepatol. 2016, 65, 734–740. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishibatake Kinoshita, M.; Minami, T.; Tateishi, R.; Wake, T.; Nakagomi, R.; Fujiwara, N.; Sato, M.; Uchino, K.; Enooku, K.; Nakagawa, H.; et al. Impact of direct-acting antivirals on early recurrence of HCV-related HCC: Comparison with interferon-based therapy. J. Hepatol. 2018, 70, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Teng, W.; Jeng, W.-J.; Yang, H.I.; Chen, W.T.; Hsieh, Y.C.; Huang, C.H.; Lin, C.C.; Lin, C.Y.; Lin, S.M.; Sheen, I.S.; et al. Interferon Is Superior to Direct Acting Antiviral Therapy in Tertiary Prevention of Early Recurrence of Hepatocellular Carcinoma. Cancers 2019, 12, 23. [Google Scholar] [CrossRef] [Green Version]
- Ebied, O.M.; Federle, M.P.; Carr, B.I.; Pealer, K.M.; Li, W.; Amesur, N.; Zajko, A. Evaluation of responses to chemoembolization in patients with unresectable hepatocellular carcinoma. Cancer 2003, 97, 1042–1050. [Google Scholar] [CrossRef]
- Vogl, T.J.; Trapp, M.; Schroeder, H.; Mack, M.; Schuster, A.; Schmitt, J.; Neuhaus, P.; Felix, R. ransarterial chemoembolization for hepatocellular carcinoma: Volumetric and morphologic CT criteria for assessment of prognosis and therapeutic success-results from a liver transplantation center. Radiology 2000, 214, 349–357. [Google Scholar] [CrossRef] [PubMed]
- European Association For The Study Of The Liver; European Organisation For Research; Treatment Of Cancer. EASL-EORTC clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2012, 56, 908–943. [Google Scholar] [CrossRef] [Green Version]
- Terzi, E.; Terenzi, L.; Venerandi, L.; Croci, L.; Renzulli, M.; Mosconi, C.; Allegretti, G.; Granito, A.; Golfieri, R.; Bolondi, L.; et al. The ART score is not effective to select patients for transarterial chemoembolization retreatment in an Italian series. Dig. Dis. 2014, 32, 711–716. [Google Scholar] [CrossRef]
- Park, H.J.; Jang, H.Y.; Kim, S.Y.; Lee, S.J.; Won, H.J.; Byun, J.H.; Choi, S.H.; Lee, S.S.; An, J.; Lim, Y.-S. Non-enhanced magnetic resonance imaging as a surveillance tool for hepatocellular carcinoma: Comparison with ultrasound. J. Hepatol. 2020, 72, 718–724. [Google Scholar] [CrossRef]
- Renzulli, M.; Golfieri, R.; Bologna Liver Oncology, G. Proposal of a new diagnostic algorithm for hepatocellular carcinoma based on the Japanese guidelines but adapted to the Western world for patients under surveillance for chronic liver disease. J. Gastroenterol. Hepatol. 2016, 31, 69–80. [Google Scholar] [CrossRef] [Green Version]



| Variables | All (n = 613) | Mortality | p-Value | |
|---|---|---|---|---|
| No. (N = 183, 29.9%) | Yes (N = 430, 70.1%) | |||
| Age (years) | 67.2 (60.4–74.1) | 66.7 (61.1–72.7) | 67.5 (60.3–74.5) | 0.5140 |
| Gender (male, %) | 368 (60.0) | 99 (54.1) | 269 (62.6) | 0.0584 |
| BCLC stage 0/A/B/C, n (%) | 28/222/240/123 (4.6/36.2/39.2/20.0) | 14/78/52/39 (7.7/42.6/28.4/21.3) | 14/144/188/84 (3.3/33.5/43.7/19.5) | 0.0009 |
| ALBI grade I/II/III, n (%) | 154/425/34 (25.1/69.3/5.6) | 57/117/9 (31.2/63.9/4.9) | 97/308/25 (22.6/71.6/5.8) | 0.0450 |
| ALBI grade increase, n (%) | 298 (48.6) | 69 (37.7) | 229 (53.3) | 0.0001 |
| Anti-viral therapy, n (%) | 120 (19.6) | 72 (39.3) | 48 (11.2) | <0.0001 |
| NLR | 1.72 (1.26–2.55) | 1.67 (1.19–2.39) | 1.74 (1.27–2.66) | 0.2643 |
| Total bilirubin (mg/dL) | 0.80 (0.60–1.20) | 0.80 (0.50–1.10) | 0.90 (0.60–1.30) | 0.0067 |
| AST (U/L) | 62 (42–98) | 62 (37–94) | 63 (43–99) | 0.1696 |
| ALT (U/L) | 56 (33–88) | 55 (30–87) | 57 (33–89) | 0.3461 |
| APRI | 1.92 (1.04–3.39) | 1.89 (0.86–3.25) | 1.92 (1.11–3.39) | 0.4968 |
| FIB-4 | 5.82 (3.78–9.45) | 5.25 (3.45–9.84) | 5.95 (3.89–9.39) | 0.3092 |
| Albumin (g/dL) | 3.55 (3.20–3.90) | 3.64 (3.30–3.97) | 3.50 (3.18–3.88) | 0.0129 |
| AFP (ng/mL) | 42 (11–297) | 40 (9–188) | 45 (11–422) | 0.1238 |
| Platelet (1000/μL) | 99 (69–146) | 102 (67–150) | 99 (70–143) | 0.9431 |
| Tumor numbers > 3, n (%) | 185 (30.2) | 33 (18.0) | 152 (35.4) | <0.0001 |
| Target lesion size (cm) | 3.3 (2.1–5.0) | 3.0 (2.0–4.5) | 3.4 (2.1–5.3) | 0.0453 |
| Within up-to-7, n (%) | 402 (65.6) | 137 (74.9) | 265 (61.6) | 0.0016 |
| Tumor extent unilobar, n (%) | 354 (57.8) | 125 (68.3) | 229 (53.3) | 0.0007 |
| Macrovascular invasion, n (%) | 59 (9.6) | 15 (8.2) | 44 (10.2) | 0.5495 |
| Final CR, n (%) | 284 (46.3) | 130 (71.0) | 154 (35.8) | <0.0001 |
| Recurrence, n (%) | 208 (73.2) | 80 (61.5) | 128 (83.1) | <0.0001 |
| Follow-up duration (months) | 31.7 (19.2–46.0) | 36.9 (27.4–49.3) | 26.9 (16.1–43.6) | <0.0001 |
| Variables | Crude HR | 95%CI | p-Value | Adjusted HR | 95%CI | p-Value | |
|---|---|---|---|---|---|---|---|
| ALBI in baseline | I | Referent | Referent | ||||
| II/III | 1.301 | 1.037–1.631 | 0.023 | 1.451 | 1.119–1.882 | 0.005 | |
| Sex | Female | Referent | |||||
| Male | 1.210 | 0.995–1.472 | 0.0764 | ||||
| Delta ALBI grade | No increase | Referent | Referent | ||||
| Increase | 1.297 | 1.013–1.661 | 0.040 | 1.436 | 1.107–1.864 | 0.006 | |
| Anti-viral therapy | No | Referent | Referent | ||||
| Yes | 0.502 | 0.370–0.681 | <0.001 | 0.580 | 0.410–0.819 | 0.002 | |
| Up-to-seven | Within | Referent | Referent | ||||
| Beyond | 1.624 | 1.338–1.970 | <0.001 | 1.214 | 0.975–1.511 | 0.083 | |
| Tumor extent | Unilobe | Referent | Referent | ||||
| Bilobe | 1.434 | 1.186–1.734 | <0.001 | 1.107 | 0.894–1.372 | 0.351 | |
| MVI | No | Referent | |||||
| Yes | 1.214 | 0.715–2.061 | 0.4726 | ||||
| CR | No | Referent | Referent | ||||
| Yes | 0.347 | 0.283–0.425 | <0.001 | 0.373 | 0.123–0.471 | <0.001 | |
| Variables | All (n = 284) | Recurrence | p-Value | |
|---|---|---|---|---|
| No (N = 76, 26.8%) | Yes (N = 208, 73.2%) | |||
| Age (years) | 66.2 (60.3–73.0) | 66.2 (61.1–75.6) | 66.2 (60.0–72.5) | 0.2601 |
| Gender (male, %) | 156 (54.9) | 41 (54.0) | 115 (55.3) | 0.8931 |
| BCLC stage 0/A/B/C, n (%) | 24/144/73/43 (8.5/50.7/25.7/15.1) | 6/41/15/14 (7.9/54.0/19.7/18.4) | 18/103/58/29 (8.7/49.5/27.9/13.9) | 0.4780 |
| ALBI grade I/II/III, n (%) | 70/201/13 (24.7/70.8/4.5) | 22/50/4 (28.9/65.8/5.3) | 48/151/9 (23.1/72.6/4.3) | 0.0453 |
| ALBI grade increase, n (%) | 140 (49.3) | 33 (43.4) | 107 (51.4) | 0.0413 |
| Anti-viral therapy, n (%) | 75 (26.4) | 27 (35.5) | 48 (23.1) | 0.0461 |
| NLR | 1.68 (1.24–2.34) | 1.85 (1.26–3.08) | 1.65 (1.22–2.21) | 0.2125 |
| Total bilirubin (mg/dL) | 0.80 (0.60–1.20) | 0.85 (0.50–1.30) | 0.80 (0.60–1.20) | 0.4805 |
| AST (U/L) | 62 (41–93) | 55 (34–88) | 62 (46–94) | 0.1517 |
| ALT (U/L) | 56 (33–90) | 40 (24–72) | 63 (37–92) | 0.0001 |
| APRI | 1.95 (1.09–3.50) | 1.71 (0.79–3.24) | 2.05 (1.32–3.51) | 0.1284 |
| FIB-4 | 5.90 (3.89–9.67) | 5.47 (3.89–10.8) | 6.36 (3.89–9.42) | 0.7924 |
| Albumin (g/dL) | 3.60 (3.26–3.89) | 3.66 (3.30–3.95) | 3.47 (3.20–3.74) | 0.0179 |
| AFP (ng/mL) | 24 (9–127) | 27 (9–205) | 23 (9–112) | 0.6332 |
| Platelet (1000/μL) | 92 (66–137) | 96 (66–151) | 90 (65–128) | 0.2305 |
| Tumor numbers > 3, n (%) | 46 (16.2) | 8 (10.5) | 38 (18.3) | 0.1458 |
| Target lesion size (cm) | 2.8 (2.0–4.0) | 3.1 (2.0–4.3) | 2.7 (2.0–3.9) | 0.1489 |
| Within up-to-7, n (%) | 236 (83.1) | 59 (77.6) | 177 (85.1) | 0.1536 |
| Tumor extent unilobar, n (%) | 209 (73.6) | 61 (80.3) | 148 (71.2) | 0.1315 |
| Macrovascular invasion, n (%) | 26 (9.2) | 10 (13.2) | 16 (7.7) | 0.1674 |
| Mortality, n (%) | 154 (54.2) | 26 (34.2) | 128 (61.5) | <0.0001 |
| Follow-up duration (months) | 37.0 (25.5–52.9) | 33.6 (19.1–43.8) | 39.6 (29.2–56.6) | 0.0003 |
| Variables | Crude HR | 95%CI | p-Value | Adjusted HR | 95%CI | p-Value | |
|---|---|---|---|---|---|---|---|
| ALBI in baseline | I | Referent | Referent | ||||
| II/III | 1.352 | 1.015–1.835 | 0.036 | 1.088 | 1.019–1.196 | 0.035 | |
| Sex | Female | Referent | |||||
| Male | 1.240 | 0.978–1.572 | 0.0756 | ||||
| Delta ALBI grade | No increase | Referent | Referent | ||||
| Increase | 1.558 | 1.071–2.268 | 0.020 | 1.456 | 1.087–2.148 | 0.029 | |
| MVI | No | Referent | |||||
| Yes | 0.898 | 0.599–1.346 | 0.6018 | ||||
| Anti-viral therapy | No | Referent | Referent | ||||
| Yes | 0.765 | 0.517–0.978 | 0.045 | 0.983 | 0.592–1.183 | 0.321 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, P.-T.; Teng, W.; Jeng, W.-J.; Chen, W.-T.; Hsieh, Y.-C.; Huang, C.-H.; Lui, K.-W.; Hung, C.-F.; Wang, C.-T.; Chai, P.-M.; et al. Dynamic Change of Albumin-Bilirubin Score Is Good Predictive Parameter for Prognosis in Chronic Hepatitis C-hepatocellular Carcinoma Patients Receiving Transarterial Chemoembolization. Diagnostics 2022, 12, 665. https://doi.org/10.3390/diagnostics12030665
Lin P-T, Teng W, Jeng W-J, Chen W-T, Hsieh Y-C, Huang C-H, Lui K-W, Hung C-F, Wang C-T, Chai P-M, et al. Dynamic Change of Albumin-Bilirubin Score Is Good Predictive Parameter for Prognosis in Chronic Hepatitis C-hepatocellular Carcinoma Patients Receiving Transarterial Chemoembolization. Diagnostics. 2022; 12(3):665. https://doi.org/10.3390/diagnostics12030665
Chicago/Turabian StyleLin, Po-Ting, Wei Teng, Wen-Juei Jeng, Wei-Ting Chen, Yi-Chung Hsieh, Chien-Hao Huang, Kar-Wai Lui, Chen-Fu Hung, Ching-Ting Wang, Pei-Mei Chai, and et al. 2022. "Dynamic Change of Albumin-Bilirubin Score Is Good Predictive Parameter for Prognosis in Chronic Hepatitis C-hepatocellular Carcinoma Patients Receiving Transarterial Chemoembolization" Diagnostics 12, no. 3: 665. https://doi.org/10.3390/diagnostics12030665







