Evaluation of the Diagnostic Accuracy of Nasal Cavity and Nasopharyngeal Swab Specimens for SARS-CoV-2 Detection via Rapid Antigen Test According to Specimen Collection Timing and Viral Load
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Sample Collection
2.3. The Rapid Antigen Test (RAT)
2.4. Real-Time Reverse-Transcription Polymerase Chain Reaction (RT-PCR)
2.5. Statistical Analysis
3. Results
3.1. Sensitivity of the Q Ag Test Using Nasopharyngeal Samples
3.2. Sensitivity of the Q Ag Test Using Nasal Cavity Samples
3.3. Agreement between Tests with the Nasal Cavity and Nasopharyngeal Swabs
3.4. Sensitivity Analysis according to DSO
3.5. Sensitivity Analysis according to Ct Value
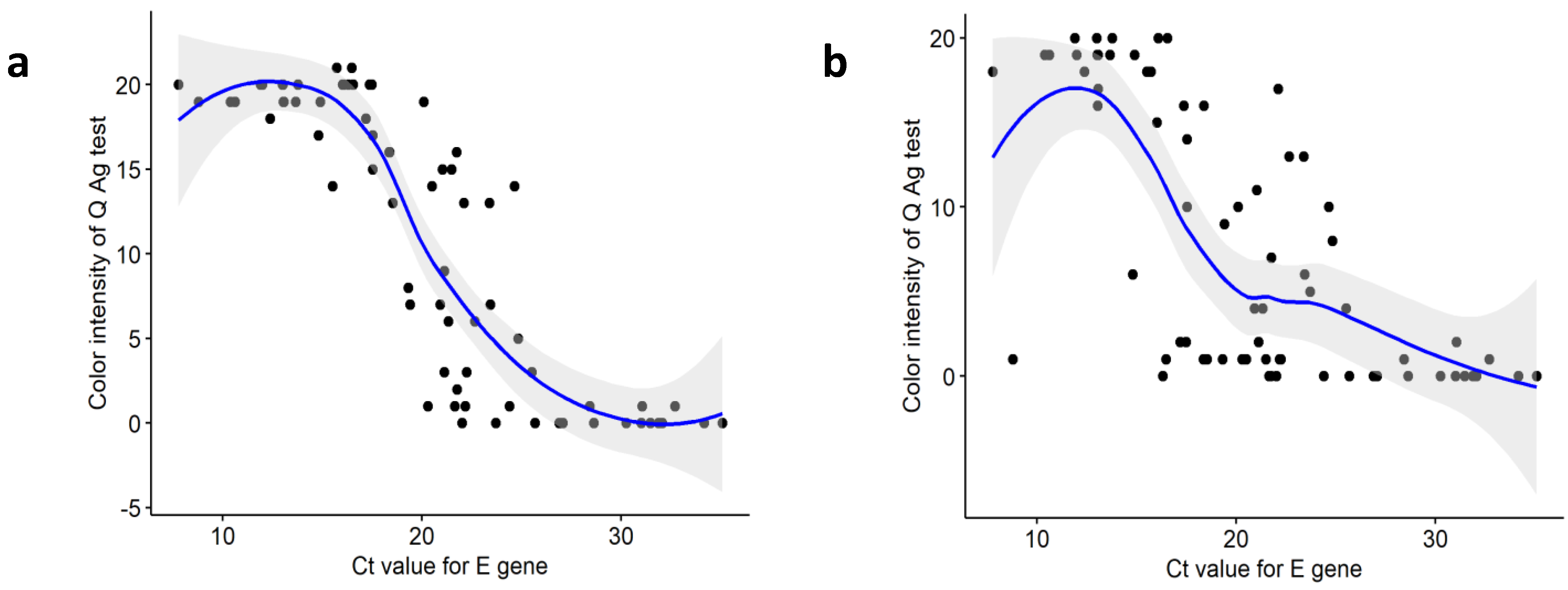
3.6. Comparison of Ct Values between Positive and Negative Samples Based on Q Ag Test
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cheng, M.P.; Papenburg, J.; Desjardins, M.; Kanjilal, S.; Quach, C.; Libman, M.; Dittrich, S.; Yansouni, C.P. Diagnostic testing for severe acute respiratory syndrome–related coronavirus 2: A narrative review. Ann. Intern. Med. 2020, 172, 726–734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Younes, N.; Al-Sadeq, D.W.; Al-Jighefee, H.; Younes, S.; Al-Jamal, O.; Daas, H.I.; Yassine, H.; Nasrallah, G.K. Challenges in laboratory diagnosis of the novel coronavirus SARS-CoV-2. Viruses 2020, 12, 582. [Google Scholar] [CrossRef] [PubMed]
- Cerutti, F.; Burdino, E.; Milia, M.G.; Allice, T.; Gregori, G.; Bruzzone, B.; Ghisetti, V. Urgent need of rapid tests for SARS CoV-2 antigen detection: Evaluation of the SD-Biosensor antigen test for SARS-CoV-2. J. Clin. Virol. 2020, 132, 104654. [Google Scholar] [CrossRef] [PubMed]
- May, L.; Tran, N.; Ledeboer, N.A. Point-of-care COVID-19 testing in the emergency department: Current status and future prospects. Expert Rev. Mol. Diagn. 2021, 21, 1333–1340. [Google Scholar] [CrossRef]
- Dinnes, J.; Deeks, J.J.; Berhane, S.; Taylor, M.; Adriano, A.; Davenport, C.; Dittrich, S.; Emperador, D.; Takwoingi, Y.; Cunningham, J. Rapid, point-of-care antigen and molecular-based tests for diagnosis of SARS-CoV-2 infection. Cochrane Database Sys. Rev. 2021. [Google Scholar]
- Mak, G.C.; Cheng, P.K.; Lau, S.S.; Wong, K.K.; Lau, C.; Lam, E.T.; Chan, R.C.; Tsang, D.N. Evaluation of rapid antigen test for detection of SARS-CoV-2 virus. J. Clin. Virol. 2020, 129, 104500. [Google Scholar] [CrossRef]
- Peeling, R.W.; Olliaro, P.L.; Boeras, D.I.; Fongwen, N. Scaling up COVID-19 rapid antigen tests: Promises and challenges. Lancet Infect. Dis. 2021, 21, e290–e295. [Google Scholar] [CrossRef]
- Abusrewil, Z.; Alhudiri, I.M.; Kaal, H.H.; El Meshri, S.E.; Ebrahim, F.O.; Dalyoum, T.; Efrefer, A.A.; Ibrahim, K.; Elfghi, M.B.; Abusrewil, S. Time scale performance of rapid antigen testing for SARS-CoV-2: Evaluation of 10 rapid antigen assays. J. Med. Virol. 2021, 93, 6512–6518. [Google Scholar] [CrossRef]
- Vasoo, S.; Stevens, J.; Singh, K. Rapid antigen tests for diagnosis of pandemic (Swine) influenza A/H1N1. Clin. Infect. Dis. 2009, 49, 1090–1093. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Advice on the Use of Point-of-Care Immunodiagnostic Tests for COVID-19. Available online: https://www.who.int/news-room/commentaries/detail/advice-on-the-use-of-point-of-care-immunodiagnostic-tests-for-covid-19 (accessed on 3 February 2022).
- World Health Organization. Antigen-Detection in the Diagnosis of SARS-CoV-2 Infection Using Rapid Immunoassays: Interim Guidance. Available online: https://apps.who.int/iris/handle/10665/334253 (accessed on 3 February 2022).
- Iezzi, R.; Valente, I.; Cina, A.; Posa, A.; Contegiacomo, A.; Alexandre, A.; D’Argento, F.; Lozupone, E.; Barone, M.; Giubbolini, F. Longitudinal study of interventional radiology activity in a large metropolitan Italian tertiary care hospital: How the COVID-19 pandemic emergency has changed our activity. Eur. Radiol. 2020, 30, 6940–6949. [Google Scholar] [CrossRef]
- Papi, C.; Spagni, G.; Alexandre, A.; Calabresi, P.; Della Marca, G.; Broccolini, A. Unprotected stroke management in an undiagnosed case of Severe Acute Respiratory Syndrome Coronavirus 2 infection. J. Stroke Cerebrovasc. Dis. 2020, 29, 104981. [Google Scholar] [CrossRef] [PubMed]
- Kevadiya, B.D.; Machhi, J.; Herskovitz, J.; Oleynikov, M.D.; Blomberg, W.R.; Bajwa, N.; Soni, D.; Das, S.; Hasan, M.; Patel, M. Diagnostics for SARS-CoV-2 infections. Nat. Mater. 2021, 20, 593–605. [Google Scholar] [CrossRef]
- Lee, R.A.; Herigon, J.C.; Benedetti, A.; Pollock, N.R.; Denkinger, C.M. Performance of saliva, oropharyngeal swabs, and nasal swabs for SARS-CoV-2 molecular detection: A systematic review and meta-analysis. J. Clin. Microbiol. 2021, 59, e02881-20. [Google Scholar] [CrossRef] [PubMed]
- Heikkinen, T.; Marttila, J.; Salmi, A.A.; Ruuskanen, O. Nasal swab versus nasopharyngeal aspirate for isolation of respiratory viruses. J. Clin. Microbiol. 2002, 40, 4337–4339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- See, A.; Toh, S.T. Respiratory sampling for severe acute respiratory syndrome coronavirus 2: An Overview. Head Neck 2020, 42, 1652–1656. [Google Scholar] [CrossRef]
- LeBlanc, J.J.; Heinstein, C.; MacDonald, J.; Pettipas, J.; Hatchette, T.F.; Patriquin, G. A combined oropharyngeal/nares swab is a suitable alternative to nasopharyngeal swabs for the detection of SARS-CoV-2. J. Clin. Virol. 2020, 128, 104442. [Google Scholar] [CrossRef] [PubMed]
- Ipp, M.; Carson, S.; Petric, M.; Parkin, P. Rapid painless diagnosis of viral respiratory infection. Arch. Dis. Child. 2002, 86, 372–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heikkinen, T.; Salmi, A.A.; Ruuskanen, O. Comparative study of nasopharyngeal aspirate and nasal swab specimens for detection of influenza. Br. Med. J. 2001, 322, 138. [Google Scholar] [CrossRef] [Green Version]
- Nodell, B. NEJM Paper Is Compendium on Rapid Tests for COVID-19. Available online: https://newsroom.uw.edu/news/nejm-paper-compendium-rapid-tests-covid-19 (accessed on 21 February 2022).
- Lee, J.; Kim, S.Y.; Huh, H.J.; Kim, N.; Sung, H.; Lee, H.; Roh, K.H.; Kim, T.S.; Hong, K.H. Clinical performance of the standard Q COVID-19 rapid antigen test and simulation of its real-world application in Korea. Ann. Lab. Med. 2021, 41, 588–592. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.-M.; Jeong, H.; Chang, E.; Choe, P.G.; Kang, C.K.; Park, W.B.; Kim, T.S.; Kwon, W.Y.; Oh, M.-D.; Kim, N.J. Clinical application of the standard Q COVID-19 Ag Test for the detection of SARS-CoV-2 infection. J. Korean Med. Sci. 2021, 36, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz Gulec, E.; Cesur, N.P.; Yesilyurt Fazlioğlu, G.; Kazezoğlu, C. Effect of different storage conditions on COVID-19 RT-PCR results. J. Med. Virol. 2021, 93, 6575–6581. [Google Scholar] [CrossRef] [PubMed]
- Skalina, K.A.; Goldstein, D.; Sulail, J.; Hahm, E.; Narlieva, M.; Szymczak, W.; Fox, A.S. Extended storage of SARS-CoV-2 nasopharyngeal swabs does not negatively impact results of molecular-based testing across three clinical platforms. J. Clin. Pathol. 2022, 75, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Parvu, V.; Gary, D.S.; Mann, J.; Lin, Y.-C.; Mills, D.; Cooper, L.; Andrews, J.C.; Manabe, Y.C.; Pekosz, A.; Cooper, C.K. Factors That Influence the Reported Sensitivity of Rapid Antigen Testing for SARS-CoV-2. Front. Microbiol. 2021, 12, 2611. [Google Scholar] [CrossRef] [PubMed]
- Iglὁi, Z.; Velzing, J.; Van Beek, J.; Van de Vijver, D.; Aron, G.; Ensing, R.; Benschop, K.; Han, W.; Boelsums, T.; Koopmans, M. Clinical evaluation of Roche SD Biosensor rapid antigen test for SARS-CoV-2 in municipal health service testing site, the Netherlands. Emerg. Infect. Dis. 2021, 27, 1323. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.W.; Park, M.; Lee, J.H. Clinical Evaluation of the Rapid STANDARD Q COVID-19 Ag Test for the Screening of Severe Acute Respiratory Syndrome Coronavirus 2. Ann. Lab. Med. 2022, 42, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Porte, L.; Legarraga, P.; Vollrath, V.; Aguilera, X.; Munita, J.M.; Araos, R.; Pizarro, G.; Vial, P.; Iruretagoyena, M.; Dittrich, S. Evaluation of a novel antigen-based rapid detection test for the diagnosis of SARS-CoV-2 in respiratory samples. Int. J. Infect. Dis. 2020, 99, 328–333. [Google Scholar] [CrossRef]
- Jones, T.C.; Biele, G.; Mühlemann, B.; Veith, T.; Schneider, J.; Beheim-Schwarzbach, J.; Bleicker, T.; Tesch, J.; Schmidt, M.L.; Sander, L.E. Estimating infectiousness throughout SARS-CoV-2 infection course. Science 2021, 373, eabi5273. [Google Scholar] [CrossRef]
- Aykac, K.; Cura Yayla, B.C.; Ozsurekci, Y.; Evren, K.; Oygar, P.D.; Gurlevik, S.L.; Coskun, T.; Tasci, O.; Demirel Kaya, F.; Fidanci, I. The association of viral load and disease severity in children with COVID-19. J. Med. Virol. 2021, 93, 3077–3083. [Google Scholar] [CrossRef]
- Mawaddah, A.; Genden, H.S.; Lum, S.G.; Marina, M.B. Upper respiratory tract sampling in COVID-19. Malays. J. Pathol. 2020, 42, 23–35. [Google Scholar]
- Hong, K.H.; Lee, S.W.; Kim, T.S.; Huh, H.J.; Lee, J.; Kim, S.Y.; Park, J.-S.; Kim, G.J.; Sung, H.; Roh, K.H. Guidelines for laboratory diagnosis of coronavirus disease 2019 (COVID-19) in Korea. Ann. Lab. Med. 2020, 40, 351–360. [Google Scholar] [CrossRef]
- Hanson, K.E.; Caliendo, A.M.; Arias, C.A.; Englund, J.A.; Lee, M.J.; Loeb, M.; Patel, R.; El Alayli, A.; Kalot, M.A.; Falck-Ytter, Y. Infectious Diseases Society of America guidelines on the diagnosis of coronavirus disease 2019. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, Y.; Akashi, Y.; Kato, D.; Kuwahara, M.; Muramatsu, S.; Ueda, A.; Notake, S.; Nakamura, K.; Ishikawa, H.; Suzuki, H. Diagnostic performance and characteristics of anterior nasal collection for the SARS-CoV-2 antigen test: A prospective study. Sci. Rep. 2021, 11, 10519. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Taylor, S.N.; Cammarata, C.L.; Varnado, K.G.; Roger-Dalbert, C.; Montano, A.; Griego-Fullbright, C.; Burgard, C.; Fernandez, C.; Eckert, K. Clinical evaluation of BD Veritor SARS-CoV-2 point-of-care test performance compared to PCR-based testing and versus the Sofia 2 SARS Antigen point-of-care test. J. Clin. Microbiol. 2020, 59, e02338-20. [Google Scholar] [CrossRef] [PubMed]
- Bekliz, M.; Adea, K.; Essaidi-Laziosi, M.; Sacks, J.A.; Escadafal, C.; Kaiser, L.; Eckerle, I. SARS-CoV-2 antigen-detecting rapid tests for the delta variant. Lancet Microbe 2022, 3, e90. [Google Scholar] [CrossRef]

| Diagnostic Performance | Nasopharyngeal Specimen | Nasal Cavity Specimen | ||
|---|---|---|---|---|
| Value | 95% CI | Value | 95% CI | |
| Sensitivity (%) | 81.7 | 72.7–90.7 | 77.5 | 67.8–87.2 |
| Specificity (%) | 100.0 | 100.0–100.0 | 100.0 | 100.0–100.0 |
| Positive predicted value (%) | 100.0 | 100.0–100.0 | 100.0 | 100.0–100.0 |
| Negative predicted value (%) | 88.9 | 83.2–94.6 | 86.7 | 80.6–92.8 |
| False positive value (%) | 0.0 | 0.0–0.0 | 0.0 | 0.0–0.0 |
| False negative value (%) | 18.3 | 9.3–27.3 | 22.5 | 12.8–32.3 |
| Accuracy (%) | 92.6 | 88.7–96.5 | 90.9 | 86.6–95.1 |
| Nasal Cavity Specimen | Nasopharyngeal Specimen | ||
|---|---|---|---|
| Positive | Negative | Total | |
| Positive | 54 | 1 | 55 |
| Negative | 4 | 12 | 16 |
| Total | 58 | 13 | 71 |
| Nasopharyngeal Specimen | Nasal Cavity Specimen | |||||||
|---|---|---|---|---|---|---|---|---|
| DSO | N | Sensitivity, % | 95% CI | p * | N | Sensitivity, % | 95% CI | p * |
| Overall | 58 | 81.7 | 72.7–90.7 | 55 | 77.5 | 67.8–87.2 | 0.82 | |
| 1–4 days | 27 | 96.4 | 89.6–100.0 | 25 | 89.3 | 77.8–100.0 | ||
| 5–7 days | 24 | 77.4 | 62.7–92.1 | 0.11 | 23 | 74.2 | 58.8–89.6 | 0.12 |
| ≥8 days | 7 | 58.3 | 30.4–86.2 | <0.01 | 7 | 58.3 | 30.4–86.2 | <0.01 |
| Nasopharyngeal Specimen | Nasal Cavity Specimen | |||||||
|---|---|---|---|---|---|---|---|---|
| Ct Value | N | Sensitivity, % | 95% CI | p * | N | Sensitivity, % | 95% CI | p * |
| Overall | 58 | 81.7 | 72.7–90.7 | 55 | 77.5 | 67.8–87.2 | 0.82 | |
| E | ||||||||
| Ct < 15 | 16 | 100.0 | 100.0–100.0 | 16 | 100.0 | 100.0–100.0 | ||
| 15 ≤ Ct < 25 | 38 | 95.0 | 88.3–100.0 | <0.01 | 35 | 87.5 | 77.3–97.8 | 0.01 |
| 25 ≤ Ct ≤ 35 | 4 | 26.7 | 4.3–49.1 | <0.01 | 4 | 26.7 | 4.3–49.1 | <0.01 |
| RdRp | ||||||||
| Ct < 15 | 22 | 100.0 | 100.0–100.0 | 21 | 95.5 | 86.8–100.0 | ||
| 15 ≤ Ct < 25 | 33 | 91.7 | 82.6–100.0 | 0.06 | 31 | 86.1 | 74.8–97.4 | 0.07 |
| 25 ≤ Ct ≤ 35 | 3 | 23.1 | 0.2–46.0 | <0.01 | 3 | 23.1 | 0.2–46.0 | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Widyasari, K.; Yang, H.-R.; Jang, J.; Kang, T.; Kim, S. Evaluation of the Diagnostic Accuracy of Nasal Cavity and Nasopharyngeal Swab Specimens for SARS-CoV-2 Detection via Rapid Antigen Test According to Specimen Collection Timing and Viral Load. Diagnostics 2022, 12, 710. https://doi.org/10.3390/diagnostics12030710
Lee S, Widyasari K, Yang H-R, Jang J, Kang T, Kim S. Evaluation of the Diagnostic Accuracy of Nasal Cavity and Nasopharyngeal Swab Specimens for SARS-CoV-2 Detection via Rapid Antigen Test According to Specimen Collection Timing and Viral Load. Diagnostics. 2022; 12(3):710. https://doi.org/10.3390/diagnostics12030710
Chicago/Turabian StyleLee, Seungjun, Kristin Widyasari, Hye-Ryun Yang, Jieun Jang, Taejoon Kang, and Sunjoo Kim. 2022. "Evaluation of the Diagnostic Accuracy of Nasal Cavity and Nasopharyngeal Swab Specimens for SARS-CoV-2 Detection via Rapid Antigen Test According to Specimen Collection Timing and Viral Load" Diagnostics 12, no. 3: 710. https://doi.org/10.3390/diagnostics12030710
APA StyleLee, S., Widyasari, K., Yang, H. -R., Jang, J., Kang, T., & Kim, S. (2022). Evaluation of the Diagnostic Accuracy of Nasal Cavity and Nasopharyngeal Swab Specimens for SARS-CoV-2 Detection via Rapid Antigen Test According to Specimen Collection Timing and Viral Load. Diagnostics, 12(3), 710. https://doi.org/10.3390/diagnostics12030710






