Pre- and Postoperative Ultrasound and MRI Examinations in Assessing Vocal Folds in Patients with Goiter
Abstract
:1. Introduction
2. Materials and Methods
3. Results
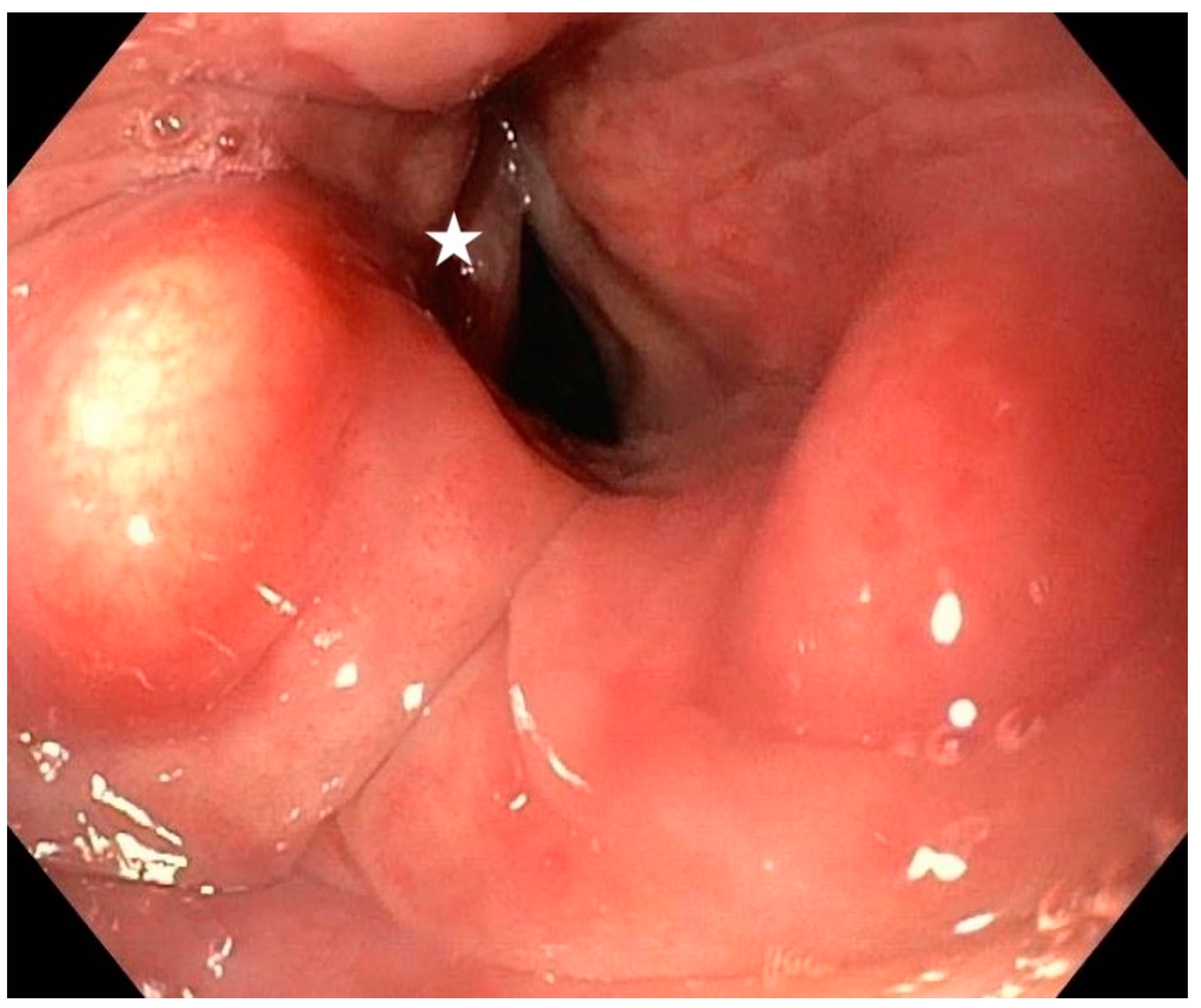
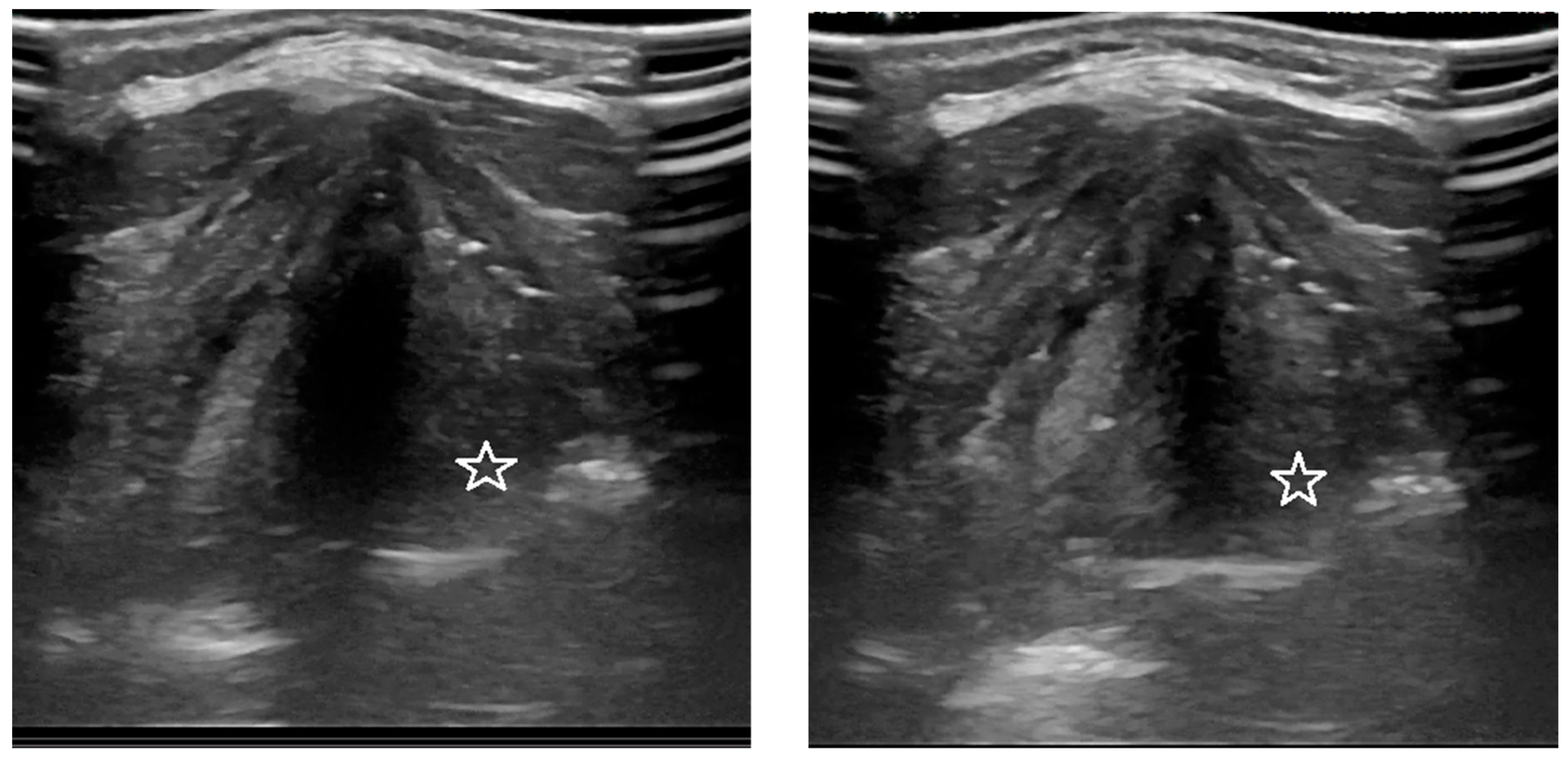
3.1. Analysis of the Qualitative Data Obtained during Ultrasound and MRI in Patients with Goiter Compared to Direct Laryngoscopy
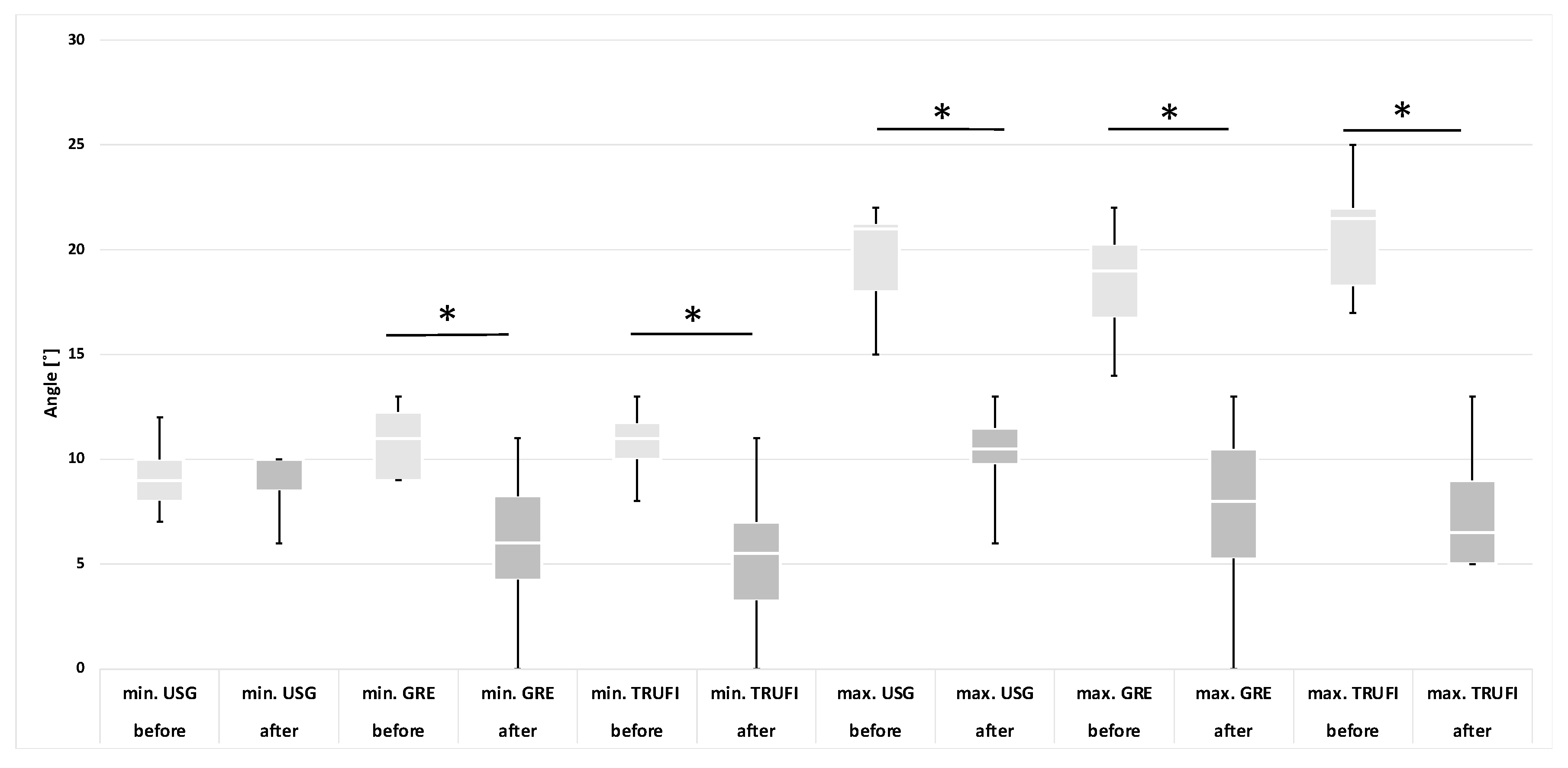
3.2. Analysis of the Quantitative Data Obtained Using Ultrasound and MRI Methods (GRE and TRUFI Sequences) before and after Thyroidectomy
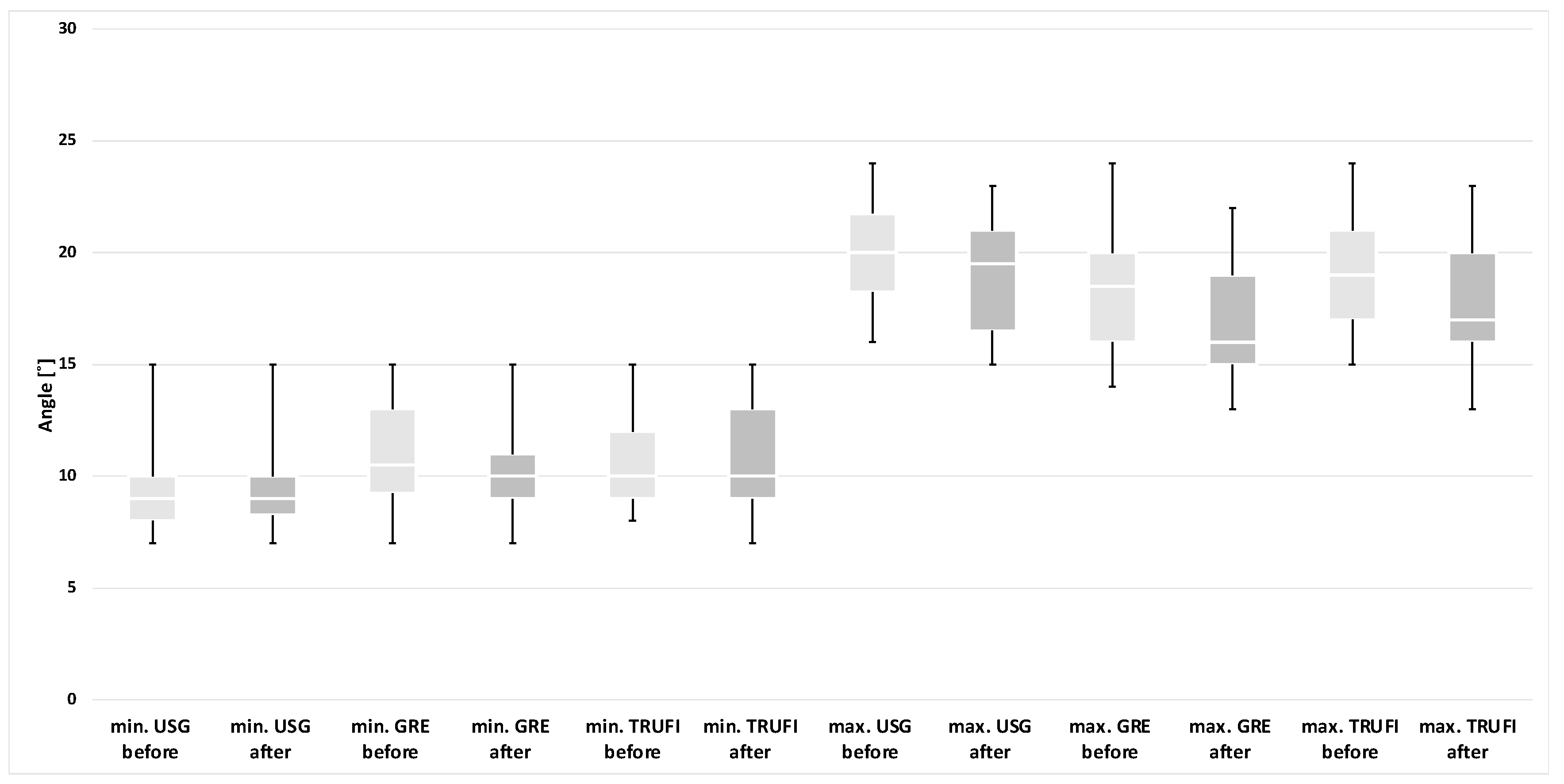
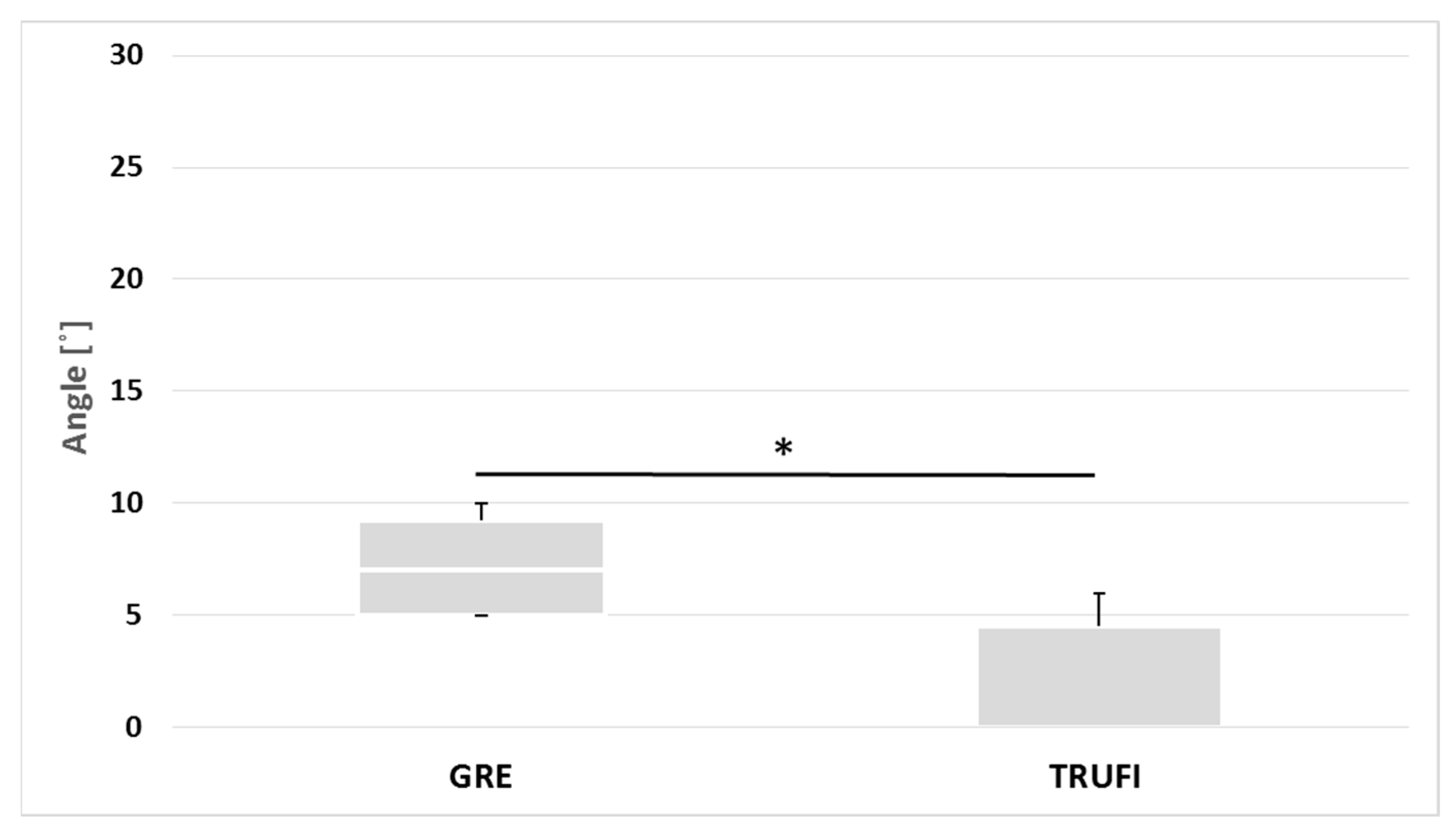
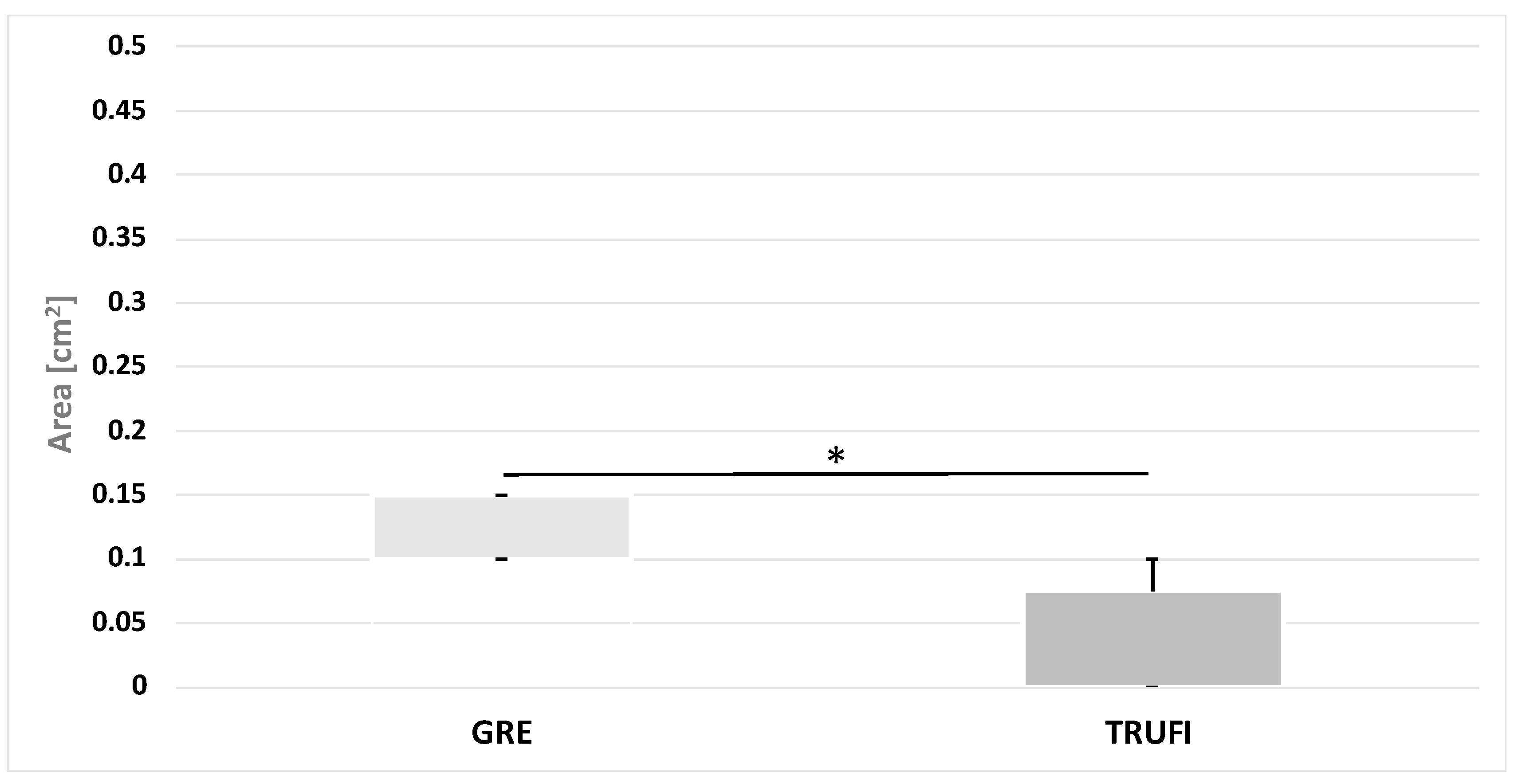
3.3. Analysis of the Quantitative Data Obtained with the Use of GRE and TRUFI Dynamic Sequences in the Group of Paralyzed Vocal Folds during Phonation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| GRE | generic gradient echo |
| MRI | magnetic resonance imaging |
| ROI | region of interest |
| TRUFI | true fast imaging with steady-state free precession |
| US | ultrasonography |
| VF | vocal fold |
References
- Vanderpump, M.P.J. The Epidemiology of Thyroid Disease. Br. Med. Bull. 2011, 99, 39–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aslan, F.; Alyanak, A. Nodule and Cancer Assessment Following Thyroid Surgery: A Cohort of 460 Patients. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9565–9570. [Google Scholar] [CrossRef] [PubMed]
- Iyomasa, R.M.; Tagliarini, J.V.; Rodrigues, S.A.; Tavares, E.L.M.; Martins, R.H.G. Laryngeal and Vocal Alterations after Thyroidectomy. Braz. J. Otorhinolaryngol. 2019, 85, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.W.; Lu, C.C.; Chao, P.Z.; Lee, F.P. Causes of Vocal Fold Paralysis. Ear. Nose Throat J. 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Gunn, A.; Oyekunle, T.; Stang, M.; Kazaure, H.; Scheri, R. Recurrent Laryngeal Nerve Injury After Thyroid Surgery: An Analysis of 11,370 Patients. J. Surg. Res. 2020, 255, 42–49. [Google Scholar] [CrossRef]
- Sinclair, C.F.; Bumpous, J.M.; Haugen, B.R.; Chala, A.; Meltzer, D.; Miller, B.S.; Tolley, N.S.; Shin, J.J.; Woodson, G.; Randolph, G.W. Laryngeal Examination in Thyroid and Parathyroid Surgery: An American Head and Neck Society Consensus Statement. Head Neck 2016, 38, 811–819. [Google Scholar] [CrossRef]
- Noel, J.E.; Orloff, L.A.; Sung, K. Laryngeal Evaluation during the COVID-19 Pandemic: Transcervical Laryngeal Ultrasonography. Otolaryngol. Head Neck Surg. 2020, 163, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Rameau, A.; Young, V.V.N.; Amin, M.R.; Sulica, L. Flexible Laryngoscopy and COVID-19. Otolaryngol. Head Neck Surg. 2020, 162, 813–815. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.P.; Au, K.P.; Lam, S.; Chang, Y.K.; Lang, B.H.H. Vocal Cord Palsies Missed by Transcutaneous Laryngeal Ultrasound (TLUSG): Do They Experience Worse Outcomes? World J. Surg. 2019, 43, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Ongkasuwan, J.; Ocampo, E.; Tran, B. Laryngeal Ultrasound and Vocal Fold Movement in the Pediatric Cardiovascular Intensive Care Unit. Laryngoscope 2017, 127, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.; Dargaud, J.; Morin, A.; Cotton, F. Dynamic MRI of Larynx and Vocal Fold Vibrations in Normal Phonation. J. Voice 2009, 23, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Baki, M.M.; Menys, A.; Atkinson, D.; Bassett, P.; Morley, S.; Beale, T.; Sandhu, G.; Naduvilethil, G.; Stevenson, N.; Birchall, M.A.; et al. Feasibility of Vocal Fold Abduction and Adduction Assessment Using Cine-MRI. Eur. Radiol. 2017, 27, 598–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gambardella, C.; Offi, C.; Maria, R.; Maurizio, R.; Roberto, D.P.; Candela, G.; Puziello, A.; Docimo, L.; Grasso, M.; Docimo, G. Transcutaneous Laryngeal Ultrasonography: A Reliable, Non—Invasive and Inexpensive Preoperative Method in the Evaluation of Vocal Cords Motility—A Prospective Multicentric Analysis on a Large Series and a Literature Review. Updates Surg. 2020, 72, 885–892. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.K.; Ghai, B.; Bhatia, N.; Verma, R.K.; Panda, N.K. ☆Comparison of Transcutaneous Laryngeal Ultrasound with Video Laryngoscope for Assessing the Vocal Cord Mobility in Patients Undergoing Thyroid Surgery. Auris Nasus Larynx 2019, 46, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Schlamann, M.; Lehnerdt, G.; Maderwald, S.; Ladd, S. Dynamic MRI of the Vocal Cords Using Phased-Array Coils: A Feasibility Study. Indian J. Radiol. Imaging 2009, 19, 127. [Google Scholar] [CrossRef] [PubMed]
- Faust, R.A.; Remley, K.B.; Rimell, F.L. Real-Time, Cine Magnetic Resonance Imaging for Evaluation of the Pediatric Airway. Laryngoscope 2001, 111, 2187–2190. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, S.E.; McRobbie, D.W. Studies of the Human Oropharyngeal Airspaces Using Magnetic Resonance Imaging. II. The Use of Three-Dimensional Gated MRI to Determine the Influence of Mouthpiece Diameter and Resistance of Inhalation Devices on the Oropharyngeal Airspace Geometry. J. Aerosol Med. Depos. Clear. Eff. Lung 2004, 17, 310–324. [Google Scholar] [CrossRef] [PubMed]
- Scheinherr, A.; Bailly, L.; Boiron, O.; Lagier, A.; Legou, T.; Pichelin, M.; Caillibotte, G.; Giovanni, A. Realistic Glottal Motion and Airflow Rate during Human Breathing. Med. Eng. Phys. 2015, 37, 829–839. [Google Scholar] [CrossRef] [PubMed]



| Parameter | Min. Angle [°] | Max. Angle [°] | ||||||
| Method | US | MRI-GRE | MRI-TRUFI | US | MRI-GRE | MRI-TRUFI | ||
| Female | 9.60 ± 2.37 (Me = 10) | 5.90 ± 3.21 (Me = 6) | 5.38 ± 3.25 (Me = 5.5) | 10.6 ± 2.37 (Me = 10.5) | 7.50 ± 3.89 (Me = 8) | 7.38 ± 2.83 (Me = 6.5) | ||
| Parameter | Min. Area [cm2] | Max. Area [cm2] | ||||||
| Method | MRI-GRE | MRI-TRUFI | MRI-GRE | MRI-TRUFI | ||||
| Female | 0.19 ± 0.13 (Me = 0.18) | 0.14 ± 0.11 (Me = 0.1) | 0.22 ± 0.15 (Me = 0.2) | 0.18 ± 0.11 (Me = 0.1) | ||||
| Parameter | Min. Angle [°] | Max. Angle [°] | ||||||
| Method | US | MRI-GRE | MRI-TRUFI | US | MRI-GRE | MRI-TRUFI | ||
| Female US/All MRI | 9.70 ± 2.056 (Me = 9) | 10.35 ± 2.25 (Me = 10) | 10.7 ± 2.39 (Me = 10) | 19.15 ± 2.50 (Me = 19.5) | 16.85 ± 2.46 (Me = 16) | 18.00 ± 2.89 (Me = 17) | ||
| Parameter | Min. Area [cm2] | Max. Area. [cm2] | ||||||
| Method | MRI-GRE | MRI-TRUFI | MRI-GRE | MRI-TRUFI | ||||
| All | 0.28 ± 0.09 (Me = 0.25) | 0.27 ± 0.07 (Me = 0.25) | 0.52 ± 0.14 (Me = 0.50) | 0.49 ± 0.11 (Me = 0.50) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Derlatka-Kochel, M.; Kumoniewski, P.; Majos, M.; Ludwisiak, K.; Pomorski, L.; Majos, A. Pre- and Postoperative Ultrasound and MRI Examinations in Assessing Vocal Folds in Patients with Goiter. Diagnostics 2022, 12, 1362. https://doi.org/10.3390/diagnostics12061362
Derlatka-Kochel M, Kumoniewski P, Majos M, Ludwisiak K, Pomorski L, Majos A. Pre- and Postoperative Ultrasound and MRI Examinations in Assessing Vocal Folds in Patients with Goiter. Diagnostics. 2022; 12(6):1362. https://doi.org/10.3390/diagnostics12061362
Chicago/Turabian StyleDerlatka-Kochel, Magdalena, Paweł Kumoniewski, Marcin Majos, Kamil Ludwisiak, Lech Pomorski, and Agata Majos. 2022. "Pre- and Postoperative Ultrasound and MRI Examinations in Assessing Vocal Folds in Patients with Goiter" Diagnostics 12, no. 6: 1362. https://doi.org/10.3390/diagnostics12061362
APA StyleDerlatka-Kochel, M., Kumoniewski, P., Majos, M., Ludwisiak, K., Pomorski, L., & Majos, A. (2022). Pre- and Postoperative Ultrasound and MRI Examinations in Assessing Vocal Folds in Patients with Goiter. Diagnostics, 12(6), 1362. https://doi.org/10.3390/diagnostics12061362






