Inflammatory and Cardiac Biomarkers in Relation with Post-Acute COVID-19 and Mortality: What We Know after Successive Pandemic Waves
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting and Participants
2.2. Data Collection
2.3. Outcome Definition
2.4. Statistical Analysis
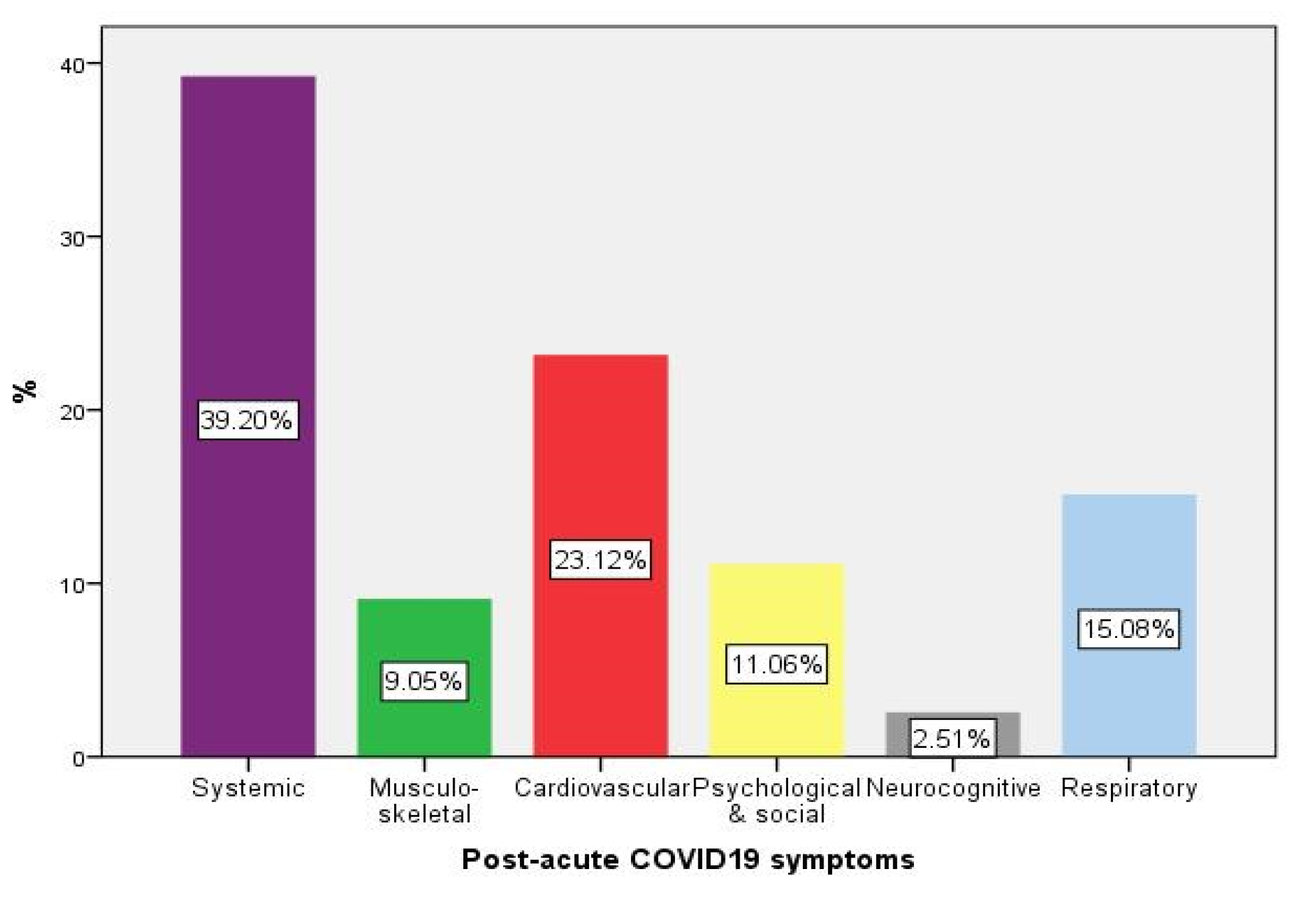
3. Results
3.1. Inflammation Biomarkers Assessment
3.2. Natriuretic Peptides Assessment
3.3. High-Sensitivity Troponin
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Butt, A.A.; Dargham, S.R.; Chemaitelly, H.; Al Khal, A.; Tang, P.; Hasan, M.R.; Coyle, P.V.; Thomas, A.G.; Borham, A.M.; Concepcion, E.G.; et al. Severity of Illness in Persons Infected With the SARS-CoV-2 Delta Variant vs Beta Variant in Qatar. JAMA Int. Med. 2022, 182, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Michelen, M.; Manoharan, L.; Elkheir, N.; Cheng, V.; Dagens, A.; Hastie, C.; O’Hara, M.; Suett, J.; Dahmash, D.; Bugaeva, P.; et al. Characterising long COVID: A living systematic review. BMJ Glob. Health 2021, 6, e005427. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Post-COVID Conditions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (accessed on 5 January 2022).
- Anka, A.U.; Tahir, M.I.; Abubakar, S.D.; Alsabbagh, M.; Zian, Z.; Hamedifar, H.; Sabzevari, A.; Azizi, G. Coronavirus disease 2019 (COVID-19): An overview of the immunopathology, serological diagnosis and management. Scand. J. Immunol. 2021, 93, e12998. [Google Scholar] [CrossRef]
- Arnold, D.T.; Attwood, M.; Barratt, S.; Morley, A.; Elvers, K.T.; McKernon, J.; Donald, C.; Oates, A.; Noel, A.; MacGowan, A.; et al. Predicting outcomes of COVID-19 from admission biomarkers: A prospective UK cohort study. Emerg. Med. J. 2021, 38, 543–548. [Google Scholar] [CrossRef]
- COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. Available online: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/ (accessed on 26 April 2022).
- O’Donnell, C.; Ashland, M.D.; Vasti, E.C.; Lu, Y.; Chang, A.Y.; Wang, P.; Daniels, L.B.; de Lemos, J.A.; Morrow, D.A.; Rodriguez, F.; et al. N-Terminal Pro-B-Type Natriuretic Peptide as a Biomarker for the Severity and Outcomes With COVID-19 in a Nationwide Hospitalized Cohort. J. Am. Heart Assoc. 2021, 10, e022913. [Google Scholar] [CrossRef]
- de Falco, R.; Vargas, M.; Palma, D.; Savoia, M.; Miscioscia, A.; Pinchera, B.; Vano, M.; Servillo, G.; Gentile, I.; Fortunato, G. B-Type Natriuretic Peptides and High-Sensitive Troponin I as COVID-19 Survival Factors: Which One Is the Best Performer? J. Clin. Med. 2021, 10, 2726. [Google Scholar] [CrossRef]
- Deng, P.; Ke, Z.; Ying, B.; Qiao, B.; Yuan, L. The diagnostic and prognostic role of myocardial injury biomarkers in hospitalized patients with COVID-19. Clin. Chim. Acta 2020, 510, 186–190. [Google Scholar] [CrossRef]
- Caro-Codón, J.; Rey, J.R.; Buño, A.; Iniesta, A.M.; Rosillo, S.O.; Castrejon-Castrejon, S.; Rodriguez-Sotelo, L.; Martinez, L.A.; Marco, I.; Merino, C.; et al. Characterization of NT-proBNP in a large cohort of COVID-19 patients. Eur. J. Heart Fail. 2021, 23, 456–464. [Google Scholar] [CrossRef]
- Baratella, E.; Ruaro, B.; Marrocchio, C.; Starvaggi, N.; Salton, F.; Giudici, F.; Quaia, E.; Confalonieri, M.; Cova, M.A. Interstitial Lung Disease at High Resolution CT after SARS-CoV-2-Related Acute Respiratory Distress Syndrome According to Pulmonary Segmental Anatomy. J. Clin. Med. 2021, 10, 3985. [Google Scholar] [CrossRef]
- Chippa, V.; Aleem, A.; Anjum, F. Post Acute Coronavirus (COVID-19) Syndrome; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK570608/ (accessed on 13 May 2022).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; Mackenzie, R.C. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chron. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- McGinley, A.; Pearse, R.M. A national early warning score for acutely ill patients. BMJ 2012, 345, e5310. [Google Scholar] [CrossRef] [PubMed]
- Mueller, C.; McDonald, K.; de Boer, R.A.; Maisel, A.; Cleland, J.G.F.; Kozhuharov, N.; Coats, A.J.S.; Metra, M.; Mebazaa, A.; Ruschitzka, F.; et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur. J. Heart Fail. 2019, 21, 715–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Centre for Disease Prevention and Control. Reinfection with SARS-CoV-2: Implementation of a Surveillance Case Definition within the EU/EEA; ECDC: Stockholm, Sweden, 2021; Available online: https://www.ecdc.europa.eu/en/publications-data/reinfection-sars-cov-2-implementation-surveillance-case-definition-within-eueea (accessed on 12 May 2022).
- Bozkurt, B.; Coats, A.J.S.; Tsutsui, H.; Abdelhamid, C.M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart Fail. 2021, 23, 352–380. [Google Scholar] [PubMed]
- Ong, S.W.X.; Chiew, C.J.; Ang, L.W.; Mak, T.M.; Cui, L.; Toh, M.P.H.S.; Lim, Y.D.; Lee, P.H.; Lee, T.H.; Chia, P.Y.; et al. Clinical and virological features of SARS-CoV-2 variants of concern: A retrospective cohort study comparing B.1.1.7 (Alpha), B.1.315 (Beta), and B.1.617.2 (Delta). Clin. Infect. Dis. 2021, ciab721. [Google Scholar] [CrossRef]
- Vafadar Moradi, E.; Teimouri, A.; Rezaee, R.; Morovatdar, N.; Foroughian, M.; Layegh, P.; Rezvani Kakhki, B.; Ahmadi Koupaei, S.R.; Ghorani, V. Increased age, neutrophil-to-lymphocyte ratio (NLR) and white blood cells count are associated with higher COVID-19 mortality. Am. J. Emerg. Med. 2021, 40, 11–14. [Google Scholar] [CrossRef]
- Carvalho-Schneider, C.; Laurent, E.; Lemaignen, A.; Beaufils, E.; Bourbao-Tournois, C.; Laribi, S.; Flament, T.; Ferreira-Maldent, N.; Bruyère, F.; Stefic, K.; et al. Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin. Microbiol. Infect. 2021, 27, 258–263. [Google Scholar] [CrossRef]
- Tabacof, L.; Tosto-Mancuso, J.; Wood, J.; Cortes, M.; Kontorovich, A.; McCarthy, D.; Rizk, D.; Rozanski, G.; Breyman, E.; Nasr, L.; et al. Post-acute COVID-19 Syndrome Negatively Impacts Physical Function, Cognitive Function, Health-Related Quality of Life, and Participation. Am. J. Phys. Med. Rehab. 2022, 101, 48–52. [Google Scholar] [CrossRef]
- Tejerina, F.; Catalan, P.; Rodriguez-Grande, C.; Adan, J.; Rodriguez-Gonzalez, C.; Muñoz, P.; Aldamiz, T.; Diez, C.; Perez, L.; Fanciulli, C.; et al. Post-COVID-19 syndrome. SARS-CoV-2 RNA detection in plasma, stool, and urine in patients with persistent symptoms after COVID-19. BMC Infect. Dis. 2022, 22, 211. [Google Scholar] [CrossRef] [PubMed]
- Han, Q.; Zheng, B.; Daines, L.; Sheikh, A. Long-Term Sequelae of COVID-19: A Systematic Review and Meta-Analysis of One-Year Follow-Up Studies on Post-COVID Symptoms. Pathogens 2022, 11, 269. [Google Scholar] [CrossRef] [PubMed]
- Smilowitz, N.R.; Kunichoff, D.; Garshick, M.; Shah, B.; Pillinger, M.; Hochman, J.S.; Berger, J.S. C-reactive protein and clinical outcomes in patients with COVID-19. Eur. Heart J. 2021, 42, 2270–2279. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.; Li, L.; Zeng, J.; Deng, Y.; Huang, H.; Chen, B.; Deng, G. Can we predict the severity of COVID-19 with a routine blood test? Pol. Arch. Int. Med. 2020, 130, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Rotty, L.; Kurube, J.; Harijanto, P.N.; Wantania, F.; Haroen, H.; Hendratta, C.; Lasut, P.; Kawengian, C.; Adiwinata, R. The Correlation between Neutrophil-to-Lymphocyte Ratio with C-reactive Protein and D-dimer Level among Indonesian COVID-19 Cases. Open Access Maced. J. Med. Sci. 2022, 10, 335–338. [Google Scholar] [CrossRef]
- Santa Cruz, A.; Mendes-Frias, A.; Oliveira, A.I.; Dias, L.; Matos, A.R.; Carvalho, A.; Capela, C.; Pedrosa, J.; Castro, A.G.; Silvestre, R. Interleukin-6 Is a Biomarker for the Development of Fatal Severe Acute Respiratory Syndrome Coronavirus 2 Pneumonia. Front. Immunol. 2021, 12, 613422. [Google Scholar] [CrossRef]
- Kappelmann, N.; Dantzer, R.; Khandaker, G.M. Interleukin-6 as potential mediator of long-term neuropsychiatric symptoms of COVID-19. Psychoneuroendocrinology 2021, 131, 105295. [Google Scholar] [CrossRef]
- Schultheiß, C.; Willscher, E.; Paschold, L.; Gottschick, C.; Klee, B.; Henkes, S.-S.; Bosurgi, L.; Dutzmann, J.; Sedding, D.; Frese, T.; et al. From online data collection to identification of disease mechanisms: The IL-1ß, IL-6 and TNF-α cytokine triad is associated with post-acute sequelae of COVID-19 in a digital research cohort. MedRxiv 2021. [Google Scholar] [CrossRef]
- Cunningham, J.W.; Claggett, B.L.; Jering, K.S.; Vaduganathan, M.; Bhatt, A.S.; Rosenthal, N.; Solomon, S.D. Prognostic Value of Natriuretic Peptides and Cardiac Troponins in COVID-19. Circulation 2021, 144, 177–179. [Google Scholar] [CrossRef]
- Task Force for the management of COVID-19 of the European Society of Cardiology. European Society of Cardiology guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: Part 1-epidemiology, pathophysiology, and diagnosis. Eur. Heart J. 2022, 43, 1033–1058. [Google Scholar] [CrossRef]
- Pranata, R.; Huang, I.; Lukito, A.A.; Raharjo, S.B. Elevated N-terminal pro-brain natriuretic peptide is associated with increased mortality in patients with COVID-19: Systematic review and meta-analysis. Postgrad. Med. J. 2020, 96, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Iorio, A.; Lombardi, C.M.; Specchia, C.; Merlo, M.; Nuzzi, V.; Ferraro, I.; Peveri, G.; Oriecuia, C.; Pozzi, A.; Inciardi, R.M.; et al. Combined Role of Troponin and Natriuretic Peptides Measurements in Patients With Covid-19 (from the Cardio-COVID-Italy Multicenter Study). Am. J. Cardiol. 2022, 167, 125–132. [Google Scholar] [CrossRef]
- Task Force for the management of COVID-19 of the European Society of Cardiology. ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: Part 2-care pathways, treatment, and follow-up. Eur. Heart J. 2022, 43, 1059–1103. [Google Scholar] [CrossRef] [PubMed]
- Sheth, A.; Modi, M.; Dawson, D.; Dominic, P. Prognostic value of cardiac biomarkers in COVID-19 infection. Sci. Rep. 2021, 11, 4930. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Rasool, S.T.; Ahmed, S.I. Role of Cardiac Biomarkers in COVID-19: What Recent Investigations Tell Us? Curr. Probl. Cardiol. 2021, 46, 100842. [Google Scholar] [CrossRef] [PubMed]
- Chehrazi, M.; Yavarpour, H.; Jalali, F.; Saravi, M.; Jafaripour, I.; Hedayati, M.T.; Amin, K.; Pourkia, R.; Abroutan, S.; Javanian, M.; et al. Optimal cut points of N-terminal of the prohormone brain natriuretic peptide (NT-proBNP) in patients with COVID-19. Egypt. Heart J. (EHJ) 2022, 74, 16. [Google Scholar] [CrossRef]



| Variable | Total Patients N = 978 | Survivors without Sequelae N = 436 (44.6%) | Post-Acute COVID-19 N = 199 (20.3%) | 30-Day Mortality N = 343 (35.1%) | p-Value * |
|---|---|---|---|---|---|
| Virus variant, N (% **) | <0.001 | ||||
| Alpha | 509 (52) | 279 (28.5) | 104 (10.6) | 126 (12.9) | |
| Beta | 120 (12.3) | 49 (5.0) | 29 (3.0) | 42 (4.3) | |
| Delta | 349 (35.7) | 108 (11.0) | 66 (6.8) | 175 (17.9) | |
| Age, median [IQR], y | 69 [59–78] | 68 [56–77] | 66 [55–73] | 72 [65–81] | <0.001 |
| Males, N (%) | 502 (51.3) | 228 (23.3) | 93 (9.5) | 181 (18.5) | 0.703 |
| Residence (rural), N (%) | 445 (45.5) | 216 (22.1) | 81 (8.3) | 148 (15.1) | 0.002 |
| CCI, median [IQR] | 4 [2–5] | 3 [2–5] | 3 [2–4] | 4 [3–6] | <0.001 |
| Onset-to-admission < 7 d, N (%) | 615 (62.9) | 294 (30.1) | 126 (12.9) | 195 (19.9) | 0.034 |
| NEWS 2, median [IQR] | 6 [4–8] | 5 [3–6] | 6 [4–7] | 8 [6–10] | <0.001 |
| SaO2 < 90%, N (%) | 341 (35.0) | 83 (8.5) | 60 (6.2) | 198 (20.3) | <0.001 |
| SBP (mmHg), median [IQR] | 130 [120–149] | 128 [115–135] | 140 [120–160] | 146 [126–164] | 0.114 |
| HR (bpm), median [IQR] | 85 [75–100] | 86 [70–92] | 82 [75–100] | 93 [81–100] | <0.001 |
| Ht (%), median [IQR] | 38.9 [34.3–42.0] | 39 [33.4–42.1] | 39.6 [35.5–41.9] | 39.8 [36.0–43.2] | 0.063 |
| RDW CV (%) | 13.8 [13.0–15.0] | 13.9 [12.9–15.4] | 14.2 [13.5–15.9] | 13.9 [12.9–14.9] | <0.001 |
| WBC (*1000/microL), median [IQR] | 8.0 [5.7–11.2] | 6.4 [5.5–10.6] | 7.4 [4.9–9.2] | 9.2 [6.1–11.8] | <0.001 |
| NLR, median [IQR] | 5.85 [3.28–10.56] | 4.59 [2.60–8.70] | 4.09 [1.93–7.38] | 7.88 [5.18–11.89] | <0.001 |
| MLR, median [IQR] | 0.54 [0.37–0.82] | 0.54 [0.34–0.69] | 0.42 [0.32–0.73] | 0.57 [0.36–0.99] | <0.001 |
| SII, median [IQR] | 1306.5 [636.9–2740.2] | 990.0 [427.0–1530.8] | 1193.4 [719.1–2156.9] | 1257.9 [805.8–2735.9] | <0.001 |
| hs-CRP (mg/dL), median [IQR] | 7.2 [2.3–15.7] | 2.0 [0.74–1.2] | 6.2 [2.8–19.8] | 9.4 [1.9–16.7] | <0.001 |
| Ferritin (ng/mL), median [IQR] | 536 [235–1285] | 475 [193–955] | 536 [235–1356] | 771 [325–1711] | <0.001 |
| Presepsin (pg/mL), median [IQR] | 356 [193–696] | 285 [188–506] | 150 [91–384] | 494 [252–1066] | <0.001 |
| Creatinine (mg/dL), median [IQR] | 0.9 [0.8–1.2] | 1.0 [0.7–1.2] | 0.9 [0.7–1.2] | 0.9 [0.8–1.2] | <0.001 |
| ALAT (U/L), median [IQR] | 33 [21–55] | 21 [13–33] | 30 [18–66] | 29 [14–48] | 0.072 |
| hs-TnI (ng/L), median [IQR] | 10.2 [2.4–44.5] | 8.5 [2.0–28.8] | 4.1 [1.5–17.7] | 18.1 [5.6–81.7] | <0.001 |
| BNP (pg/mL), median [IQR] | 204 [55.8–581] | 260 [53.2–758] | 204 [26–492] | 185 [59–592] | 0.840 |
| NT-pro BNP (pg/mL), median [IQR] | 844.5 [235.8–3207.3] | 698.0 [214.3–2256.3] | 416.5 [120.5–1380.7] | 1726.5 [555.0–4935.8] | <0.001 |
| Hospitalization (d), median [IQR] | 12 [4–16] | 14 [6–17] | 13 [4–16] | 7 [3–15] | <0.001 |
| Alpha Variant N = 509 (52%) | Parameter, Median [IQR] | Survivors without Sequelae N = 279 (28.5%) | Post-Acute COVID-19 N = 104 (10.6%) | 30-Day Mortality N = 126 (12.9%) | p Value *,a |
|---|---|---|---|---|---|
| NT-proBNP (pg/mL) | 691 [211–2256] | 398 [127–1266] | 2001 [692–4810] | <0.001 | |
| hs-TnI (ng/L) | 8.3 [2.1–31.4] | 7.5 [2.3–22.3] | 17.4 [6.7–62.2] | 0.017 | |
| hs-CRP (mg/dL) | 4.4 [1.1–10.4] | 5.0 [1.6–9.6] | 6.7 [2.3–15.8] | <0.001 | |
| RDW CV (%) | 13.8 [12.9–15.0] | 13.3 [12.7–14.1] | 14.7 [13.5–16.4] | <0.001 | |
| NLR | 3.9 [2.3–6.6] | 4.0 [2.3–6.5] | 6.4 [3.7–10.3] | <0.001 | |
| MLR | 0.5 [0.3–0.7] | 0.5 [0.3–0.7] | 0.7 [0.4–0.9] | <0.001 | |
| SII | 919 [454–1725] | 862 [459–1631] | 1219 [636–2591] | 0.010 | |
| Ferritin (ng/mL) | 353 [164–789] | 467 [223–872] | 483 [177–1261] | 0.050 | |
| Presepsin (pg/mL) | 285 [161–493] | 226 [144–421] | 560 [311–1359] | <0.001 | |
| Fibrinogen (mg/dL) | 413 [326–495] | 426 [371–487] | 411 [306–505] | 0.594 | |
| WBC (*1000/microL) | 6.92 [4.99–9.41] | 6.59 [4.91–8.71] | 10.20 [6.82–14.32] | <0.001 | |
| Age (years) | 66 [54–76] | 68 [57–73] | 73 [65–81] | <0.001 | |
| Beta Variant N = 120 (12.3%) | Parameter, Median [IQR] | Survivors without Sequelae N = 49 (5.0%) | Post-Acute COVID-19 N = 29 (3.0%) | 30-Day Mortality N = 42 (4.3%) | p Value *,a |
| NT-pro BNP (pg/mL) | 582 [105–1489] | 469 [101–2865] | 2182 [200–5028] | 0.185 | |
| hs-TnI (ng/L) | 2.8 [0.1–10.6] | 3.3 [0.1–18.1] | 16.4 [0.1–79.4] | 0.134 | |
| hs-CRP (mg/dL) | 5.2 [2.2–16.7] | 6.5 [1.6–16.8] | 10.8 [2.1–20.7] | 0.513 | |
| RDW CV (%) | 14.1 [12.8–16.2] | 13.5 [12.8–14.5] | 14.7 [13.7–16.0] | 0.061 | |
| NLR | 5.8 [2.9–12.2] | 4.9 [3.4–11.4] | 9.9 [4.8–14.8] | 0.110 | |
| MLR | 0.5 [0.3–0.8] | 0.5 [0.4–0.9] | 0.5 [0.3–0.9] | 0.856 | |
| SII | 1449 [624–3386] | 1193 [567–2372] | 1927 [846–3892] | 0.337 | |
| Ferritin (ng/mL) | 422 [147–853] | 468 [131–1629] | 856 [283–1608] | 0.086 | |
| Presepsin (pg/mL) | 307 [202–509] | 201 [147–525] | 874 [479–1105] | 0.016 | |
| Fibrinogen (mg/dL) | 444 [366–567] | 442 [342–579] | 433 [359–567] | 0.923 | |
| WBC (*1000/microL) | 7.93 [5.84–11.86] | 8.16 [5.26–11.14] | 8.73 [5.75–13.38] | 0.507 | |
| Age (years) | 70 [59–81] | 68 [59–74] | 74 [66–80] | 0.107 | |
| Delta Variant N = 349 (35.7%) | Parameter, Median [IQR] | Survivors without Sequelae N = 108 (11.0%) | Post-Acute COVID-19 N = 66 (6.8%) | 30-Day Mortality N = 175 (17.9%) | p Value *,a |
| NT-pro BNP (pg/mL) | 850 [306–3480] | 468 [92–1195] | 1394 [555–4957] | 0.003 | |
| hs-TnI (ng/L) | 13.4 [3.8–38.9] | 3.8 [0.1–12.6] | 20.7 [5.2–116.0] | 0.003 | |
| hs-CRP (mg/dL) | 11.3 [4.3–20.9] | 10.2 [5.73–19.4] | 14.9 [7.3–22.9] | 0.028 | |
| RDW CV (%) | 13.7 [13.1–14.4] | 13.6 [12.8–14.6] | 14.1 [13.3–15.1] | 0.019 | |
| NLR | 6.6 [4.7–13.5] | 6.3 [4.3–9.6] | 10.0 [5.9–17.2] | <0.001 | |
| MLR | 0.6 [0.4–0.9] | 0.5 [0.4–0.7] | 0.6 [0.5–1.0] | 0.010 | |
| SII | 1744 [930–3545] | 1754 [898–2577] | 2263 [1133–4533] | 0.009 | |
| Ferritin (ng/mL) | 711 [499–1755] | 693 [410–1.755] | 950 [500–2072] | 0.158 | |
| Presepsin (pg/mL) | 457 [264–651] | 570 [461–1174] | 735 [300–1245] | 0.228 | |
| Fibrinogen (mg/dL) | 543 [443–606] | 492 [410–573] | 514 [441–584] | 0.310 | |
| WBC (*1000/microL) | 8.31 [6.04–10.72] | 7.99 [5.70–10.53] | 9.41 [6.79–13.95] | 0.002 | |
| Age (years) | 71 [62–79] | 64 [53–73] | 72 [65–81] | <0.001 |
| Biomarker/Clinical Indicator ^ | AUC (95% CI) | Sensitivity at Youden’s Index | Specificity at Youden’s Index |
|---|---|---|---|
| NLR * (n = 555) | 0.79 (0.74–0.83) | 0.65 | 0.41 |
| MLR * (n = 556) | 0.73 (0.68–0.77) | 0.70 | 0.50 |
| Presepsin (n = 434) | 0.73 (0.68–0.78) | 0.70 | 0.36 |
| hs-CRP * (n = 532) | 0.72 (0.67–0.77) | 0.74 | 0.65 |
| hs-TnI * (n = 254) | 0.70 (0.59–0.81) | 0.63 | 0.48 |
| SII * (n = 555) | 0.69 (0.64–0.75) | 0.55 | 0.40 |
| WBC * (n = 568) | 0.68 (0.63–0.73) | 0.76 | 0.45 |
| NT-pro BNP (n = 978) | 0.66 (0.62–0.70) | 0.65 | 0.40 |
| RDW * (n = 549) | 0.64 (0.60–0.70) | 0.68 | 0.51 |
| Fibrinogen * (n = 349) | 0.55 (0.48–0.63) | 0.44 | 0.40 |
| Ferritin (n = 798) | 0.53 (0.46–0.61) | 0.73 | 0.64 |
| IL-6 (n = 39) | 0.53 (0.49–0.58) | 0.91 | 0.85 |
| NEWS 2 (n = 978) | 0.44 (0.40–0.48) | 0.31 | 0.44 |
| Age (n = 978) | 0.40 (0.36–0.44) | 0.56 | 0.68 |
| CCI (n = 978) | 0.37 (0.33–0.41) | 0.32 | 0.55 |
| Biomarker/Clinical Indicator ^ | AUC (95% CI) | Sensitivity at Youden’s Index | Specificity at Youden’s Index |
|---|---|---|---|
| Il-6 (n = 39) | 0.53 (0.49–0.58) | 0.91 | 0.85 |
| Fibrinogen * (n = 349) | 0.52 (0.44–0.59) | 0.48 | 0.53 |
| Ferritin * (n = 372) | 0.50 (0.43–0.57) | 0.48 | 0.42 |
| NT-pro BNP * (n = 638) | 0.45 (0.36–0.55) | 0.70 | 0.80 |
| WBC * (n = 568) | 0.44 (0.38–0.50) | 0.42 | 0.55 |
| NEWS 2 (n = 978) | 0.44 (0.40–0.48) | 0.31 | 0.44 |
| hs-CRP * (n = 532) | 0.41 (0.36–0.47) | 0.59 | 0.71 |
| SII * (n = 555) | 0.40 (0.35–0.46) | 0.49 | 0.64 |
| Age (n = 978) | 0.40 (0.36–0.44) | 0.56 | 0.68 |
| RDW * (n = 549) | 0.39 (0.33–0.45) | 0.55 | 0.74 |
| NLR * (n = 555) | 0.38 (0.32–0.43) | 0.84 | 0.71 |
| hs-TnI * (n = 254) | 0.38 (0.30–0.47) | 0.68 | 0.79 |
| MLR * (n = 556) | 0.37 (0.32–0.43) | 0.49 | 0.68 |
| CCI (n = 978) | 0.37 (0.33–0.41) | 0.32 | 0.55 |
| Presepsin (n = 434) | 0.36 (0.30–0.42) | 0.65 | 0.44 |
| Variable | Univariable | Multivariable | ||
|---|---|---|---|---|
| HR (95%CI) | p Value | HR (95%CI) | p Value | |
| NT-pro BNP (per log. unit) | 1.96 (1.54–2.50) | <0.001 | 1.63 (1.10–2.42) | 0.01 |
| Age (per 10 years) | 1.03 (1.02–1.04) | <0.001 | 1.03 (1.00–1.05) | 0.04 |
| Male sex | 0.82 (0.61–1.08) | 0.15 | 1.03 (0.62–1.69) | 0.92 |
| NEWS2 | 1.16 (1.11–1.21) | <0.001 | 0.95 (0.85–1.06) | 0.35 |
| Admission SaO2 < 90% | 0.46 (0.35–0.61) | <0.001 | 0.50 (0.26–0.97) | 0.04 |
| History of AD | 1.03 (0.71–1.49) | 0.89 | 0.72(0.40–1.32) | 0.29 |
| History of HT | 0.87 (0.61–1.25) | 0.44 | 0.79 (0.48–1.28) | 0.33 |
| History of DM | 1.78 (1.27–2.49) | 0.001 | 1.37 (0.32–5.81) | 0.66 |
| History of CKD | 0.39(0.24–0.64) | <0.001 | 0.51 (0.23–1.14) | 0.10 |
| History of HF | 0.72 (0.49–1.04) | 0.08 | 2.03 (0.98–4.20) | 0.05 |
| SBP (per 10 mmHg) | 0.99 (0.98–1.01) | 0.08 | 0.16 (0.01–3.45) | 0.24 |
| AHF upon admission | 0.81 (0.57–1.15) | 0.24 | 1.29 (0.58–2.90) | 0.53 |
| Mechanical ventilation | 0.84 (0.50–1.41) | 0.50 | 2.06 (0.90–4.70) | 0.08 |
| Corticotherapy | 0.63 (0.45–0.87) | 0.006 | 0.73 (0.45–1.17) | 0.19 |
| Virus variant (Delta) | 2.01 (1.66–2.43) | <0.001 | 1.68 (1.27–2.24) | <0.001 |
| CCI | 1.16 (1.08–1.23) | <0.001 | 1.06 (0.92–1.21) | 0.42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lionte, C.; Sorodoc, V.; Haliga, R.E.; Bologa, C.; Ceasovschih, A.; Petris, O.R.; Coman, A.E.; Stoica, A.; Sirbu, O.; Puha, G.; et al. Inflammatory and Cardiac Biomarkers in Relation with Post-Acute COVID-19 and Mortality: What We Know after Successive Pandemic Waves. Diagnostics 2022, 12, 1373. https://doi.org/10.3390/diagnostics12061373
Lionte C, Sorodoc V, Haliga RE, Bologa C, Ceasovschih A, Petris OR, Coman AE, Stoica A, Sirbu O, Puha G, et al. Inflammatory and Cardiac Biomarkers in Relation with Post-Acute COVID-19 and Mortality: What We Know after Successive Pandemic Waves. Diagnostics. 2022; 12(6):1373. https://doi.org/10.3390/diagnostics12061373
Chicago/Turabian StyleLionte, Catalina, Victorita Sorodoc, Raluca Ecaterina Haliga, Cristina Bologa, Alexandr Ceasovschih, Ovidiu Rusalim Petris, Adorata Elena Coman, Alexandra Stoica, Oana Sirbu, Gabriela Puha, and et al. 2022. "Inflammatory and Cardiac Biomarkers in Relation with Post-Acute COVID-19 and Mortality: What We Know after Successive Pandemic Waves" Diagnostics 12, no. 6: 1373. https://doi.org/10.3390/diagnostics12061373







