Deformation of the Titanium Plate Stabilizing the Lateral Ankle Fracture Due to Its Overloading in Case of the Young, Obese Patient: Case Report Including the Biomechanical Analysis
Abstract
:1. Introduction
2. Materials and Methods
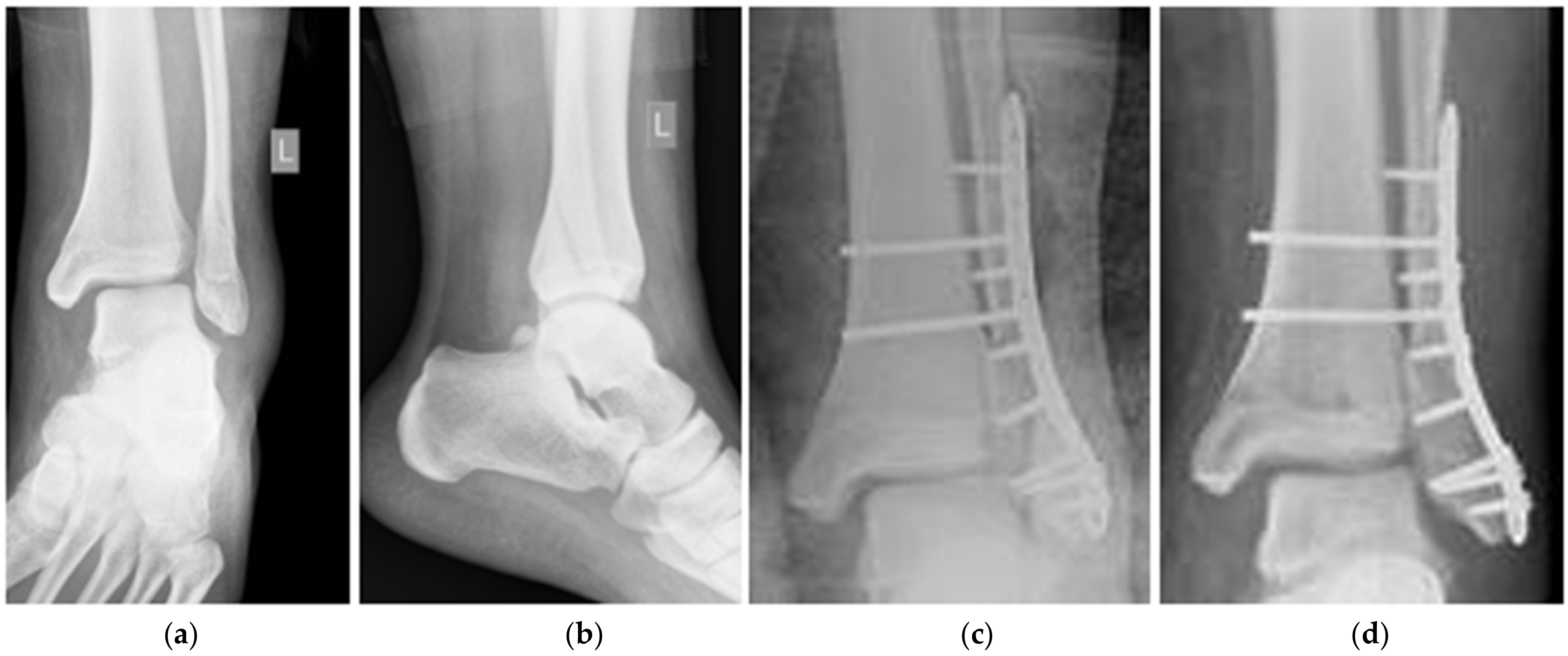
2.1. Patient and the History of Treatment
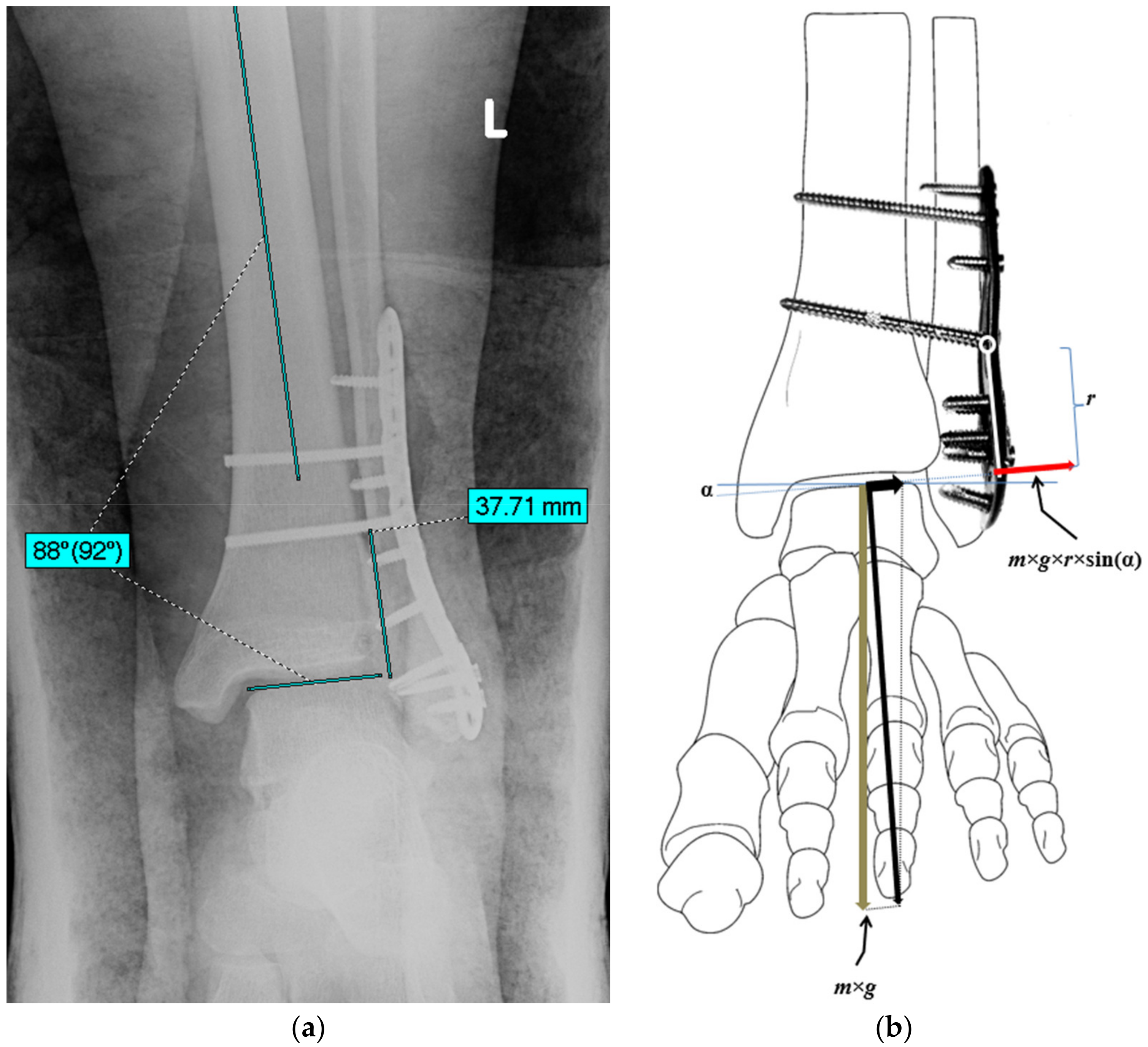
2.2. An Estimation of the Bending Moment Acting on the Plate
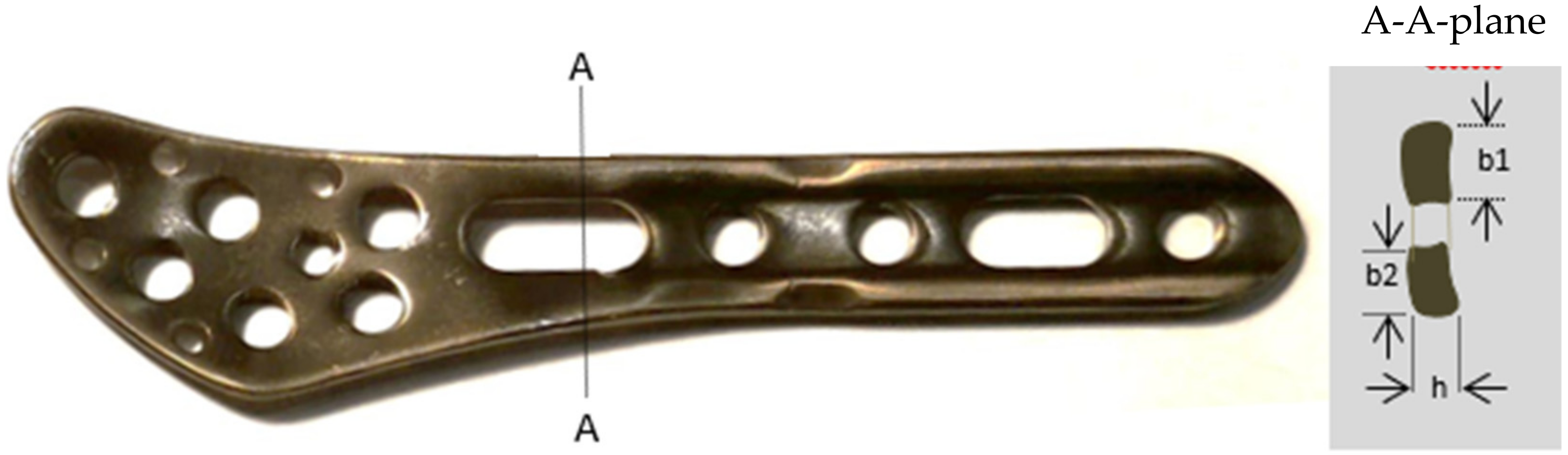
2.3. Strength Assessment of the Plate
2.4. An Analysis of Constitutive Parameters of Patients Treated in the Department of Orthopedic Surgery and Traumatology
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kopec, M.; Brodecki, A.; Szczęsny, G.; Kowalewski, Z.L. Microstructural analysis of fractured orthopedic implants. Materials 2021, 14, 2209. [Google Scholar] [CrossRef] [PubMed]
- Mónico, J.L.; Silva, F.; Marques, J.P.; Cardoso, J.; Mónico, L.; Fonseca, F. Study on Overload Injuries during Periods of Intense Physical Activity Complemented by Isokinetic Dynamometry Evaluation. Rev. Bras. Ortop. 2020, 55, 681–686. [Google Scholar] [CrossRef]
- Nourisa, J.; Rouhi, G. Biomechanical evaluation of intramedullary nail and bone plate for the fixation of distal metaphyseal fractures. J. Mech. Behav. Biomed. Mater. 2016, 56, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Kearney, J. Food consumption trends and drivers. Philos. Trans. Royal Soc. B Biol. Sci. 2010, 365, 2793–2807. [Google Scholar] [CrossRef]
- Pechey, R.; Monsivais, P. Socioeconomic inequalities in the healthiness of food choices: Exploring the contributions of food expenditures. Prev. Med. 2016, 88, 203–209. [Google Scholar] [CrossRef] [Green Version]
- Kopczyński, M. [Height and BMI in cities and country in XIX and XX centuries: Warsaw]. Wysokość ciała i BMI w miastach i na terenach wiejskich na przełomie XIX i XX wieku: Przypadek Warszawy. In Budowa Fizyczna Człowieka na Ziemiach Polskich Wczoraj i Dziś [Physical Posture of People Living in Lands of Poland Nowadays and in the Past]; Kopczyński, M., Siniarska, A., Eds.; Muzeum Historii Polski: Warszawa, Poland, 2017; pp. 89–109. [Google Scholar]
- Kopczyński, M. Between the Great War and the Great Depression: Preliminary observations on the ‘missing link’ in the history of human stature in Poland. Econ. Hum. Biol. 2019, 34, 162–168. [Google Scholar] [CrossRef]
- Kopczyński, M. The physical stature of Jewish men in Poland in the second half of the 19th century. Econ. Hum. Biol. 2011, 9, 203–210. [Google Scholar] [CrossRef]
- Kołodziej, H.; Łopuszańska, M.; Lipowicz, A.; Szklarska, A.; Bielicki, T. Secular trends in body height and body mass in 19-year-old Polish men based on six national surveys from 1965 to 2010. Am. J. Hum. Biol. 2015, 27, 704–709. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Freedman, D.S.; CDC. Obesity—United States, 1988–2008. MMWR Suppl. 2011, 60, 73–77. [Google Scholar]
- Craik, J.D.; Bircher, M.D.; Rickman, M. Hip and knee arthroplasty implants contraindicated in obesity. Ann. R. Coll. Surg. Engl. 2016, 98, 295–299. [Google Scholar] [CrossRef]
- Murphy, D.F.; Connolly, D.A.J.; Beynnon, B.D. Risk factors for lower extremity injury: A review of the literature. Br. J. Sports Med. 2003, 37, 13–29. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Hu, H.; Zeng, M.; Chu, H.; Gan, Z.; Duan, J.; Rong, M. The survival rates and risk factors of implants in the early stage: A retrospective study. BMC Oral Health 2021, 21, 293. [Google Scholar] [CrossRef]
- Han, S.M.; Wu, T.H.; Wen, J.X.; Wang, Y.; Cao, L.; Wu, W.J.; Gao, B.L. Radiographic analysis of adult ankle fractures using combined Danis-Weber and Lauge-Hansen classification systems. Sci. Rep. 2020, 10, 7655. [Google Scholar] [CrossRef]
- Berend, K.R.; Lombardi, A.V., Jr.; Mallory, T.H.; Adams, J.B.; Groseth, K.L. Early failure of minimally invasive unicompartmental knee arthroplasty is associated with obesity. Clin. Orthop. Relat. Res. 2005, 440, 60–66. [Google Scholar] [CrossRef]
- Corbeil, P.; Simoneau, M.; Rancourt, D.; Tremblay, A.; Teasdale, N. Increased risk for falling associated with obesity: Mathematical modeling of postural control. IEEE Trans. Neural. Syst. Rehabil. Eng. 2001, 9, 126–136. [Google Scholar] [CrossRef]
- Kessler, J.; Koebnick, C.; Smith, N.; Adams, A. Childhood obesity is associated with increased risk of most lower extremity fractures. Clin. Orthop. Relat. Res. 2013, 471, 1199–1207. [Google Scholar] [CrossRef] [Green Version]
- Wang, T.; He, C. Pro-inflammatory cytokines: The link between obesity and osteoarthritis. Cytokine Growth Factor Rev. 2018, 44, 38–50. [Google Scholar] [CrossRef]
- Jeschke, E.; Citak, M.; Günster, C.; Halder, A.M.; Heller, K.D.; Malzahn, J.; Niethard, F.U.; Schräder, P.; Zacher, J.; Gehrke, T. Obesity Increases the Risk of Postoperative Complications and Revision Rates Following Primary Total Hip Arthroplasty: An Analysis of 131,576 Total Hip Arthroplasty Cases. J. Arthroplast. 2018, 33, 2287–2292.e1. [Google Scholar] [CrossRef]
- Ricci, W.M.; Streubel, P.N.; Morshed, S.; Collinge, C.A.; Nork, S.E.; Gardner, M.J. Risk factors for failure of locked plate fixation of distal femur fractures: An analysis of 335 cases. J. Orthop. Trauma 2014, 28, 83–89. [Google Scholar] [CrossRef]
- Burrus, T.M.; Werner, B.C.; Yarboro, S.R. Obesity is associated with increased postoperative complications after operative management of tibial shaft fractures. Injury 2016, 47, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Er, M.S.; Verim, O.; Eroglu, M.; Altinel, L.; Gokce, B.; Tasgetiren, S. Biomechanical evaluation of syndesmotic screw design via finite element analysis and Taguchi’s method. J. Am. Podiatr. Med. Assoc. 2015, 105, 14–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ricci, P.L.; Maas, S.; Kelm, J.; Gerich, T. Finite element analysis of the pelvis including gait muscle forces: An investigation into the effect of rami fractures on load transmission. J. Exp. Orthop. 2018, 5, 33. [Google Scholar] [CrossRef] [Green Version]
- Kakkar, R.; Siddique, M.S. Stresses in the ankle joint and total ankle replacement design. Foot Ankle Surg. 2011, 17, 58–63. [Google Scholar] [CrossRef]
- Burdett, R.G. Forces predicted at the ankle during running. Med. Sci. Sports Exerc. 1982, 14, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Mugnai, R.; Tarallo, L.; Capra, F.; Catani, F. Biomechanical comparison between stainless steel, titanium and carbon-fiber reinforced polyetheretherketone volar locking plates for distal radius fractures. Orthop. Traumatol. Surg. Res. 2018, 104, 877–882. [Google Scholar] [CrossRef]
- MacLeod, A.; Simpson, A.H.R.W.; Pankaj, P. Experimental and numerical investigation into the influence of loading conditions in biomechanical testing of locking plate fracture fixation devices. Bone Joint Res. 2018, 7, 111–120. [Google Scholar] [CrossRef]
- World Health Organization (WHO). European Programme of Work: United Action for Better Health. Available online: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/data-and-statistics (accessed on 1 May 2022).
- Jarosz, M.; Rychlik, E. Overweight and obesity among adults in Poland, 1983–2005. Adv. Med. Sci. 2008, 53, 158–166. [Google Scholar] [CrossRef] [Green Version]
- Rodgers, M.M. Dynamic biomechanics of the normal foot and ankle during walking and running. Phys. Ther. 1988, 68, 1822–1830. [Google Scholar] [CrossRef]
- Stauffer, R.N.; Chao, E.Y.; Brewster, R.C. Force and motion analysis of the normal, diseased, and prosthetic ankle joint. Clin. Orthop. Relat. Res. 1977, 127, 189–196. [Google Scholar] [CrossRef]
- Seireg, A.; Arvikar, R.J. A mathematical model for evaluation of forces in lower extremeties of the musculo-skeletal system. J. Biomech. 1973, 6, 313–326. [Google Scholar] [CrossRef]
- Steel vs. Titanium–Comparison–Pros and Cons. Available online: https://material-properties.org/steel-vs-titanium-comparison-pros-and-cons/ (accessed on 1 May 2022).
- Musbahi, O.; Hamilton, T.W.; Crellin, A.J.; Mellon, S.J.; Kendrick, B.; Murray, D.W. The effect of obesity on revision rate in unicompartmental knee arthroplasty: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3467–3477. [Google Scholar] [CrossRef]
- Polat, A.E.; Polat, B.; Gürpınar, T.; Çarkçı, E.; Güler, O. The effect of morbid obesity (BMI ≥ 35 kg/m2) on functional outcome and complication rate following unicompartmental knee arthroplasty: A case-control study. J. Orthop. Surg. Res. 2019, 14, 266. [Google Scholar] [CrossRef] [Green Version]
- Xu, S.; Lim, W.-A.J.; Chen, J.Y.; Lo, N.N.; Chia, S.-L.; Tay, D.K.J.; Hao, Y.; Yeo, S.J. The influence of obesity on clinical outcomes of fixed-bearing unicompartmental knee arthroplasty. Bone Jt. J. 2019, 101-B, 213–220. [Google Scholar] [CrossRef]
- Nettrour, J.F.; Ellis, R.T.; Hansen, B.J.; Keeney, J.A. High Failure Rates for Unicompartmental Knee Arthroplasty in Morbidly Obese Patients: A Two-Year Minimum Follow-Up Study. J. Arthroplast. 2020, 35, 989–996. [Google Scholar] [CrossRef] [Green Version]
- Parratte, S.; Pesenti, S.; Argenson, J.-N. Obesity in orthopedics and trauma surgery. Orthop. Traumatol. Surg. Res. 2014, 100, S91–S97. [Google Scholar] [CrossRef] [Green Version]
| Body Mass (kg) | No. of Patients | % |
|---|---|---|
| ≤70 | 722 | 36.0 |
| 70–80 | 363 | 18.1 |
| ≥80 | 922 | 45.9 |
| In total | ||
| ≥75 kg | 1139 | 56.7 |
| ≥100 kg | 237 | 11.8 |
| BMI (kg/m2) | <18.5 | 18.5–24.9 | 25.0–29.9 | >30 | Together |
|---|---|---|---|---|---|
| mean | 17.4 | 22.5 | 27.4 | 33.9 | 27.2 |
| SD | 1.2 | 1.8 | 1.4 | 3.6 | 5.2 |
| min | 12.4 | 18.5 | 25.0 | 30.0 | 12.4 |
| max | 18.4 | 24.9 | 29.9 | 57.6 | 57.6 |
| No. of patients | 39 | 682 | 756 | 530 | 2007 |
| % | 1.9% | 34.0% | 37.6% | 26.4% | 100.0% |
| Height (cm) | Body Mass (kg) | Age (Years) | BMI (kg/m2) | |
|---|---|---|---|---|
| mean | 169.1 | 78.1 | 55.2 | 27.2 |
| SD | 10.2 | 17.0 | 18.5 | 5.1 |
| min | 140 | 31 | 18 | 12.4 |
| max | 201 | 155 | 98 | 57.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szczęsny, G.; Kopec, M.; Szolc, T.; Kowalewski, Z.L.; Małdyk, P. Deformation of the Titanium Plate Stabilizing the Lateral Ankle Fracture Due to Its Overloading in Case of the Young, Obese Patient: Case Report Including the Biomechanical Analysis. Diagnostics 2022, 12, 1479. https://doi.org/10.3390/diagnostics12061479
Szczęsny G, Kopec M, Szolc T, Kowalewski ZL, Małdyk P. Deformation of the Titanium Plate Stabilizing the Lateral Ankle Fracture Due to Its Overloading in Case of the Young, Obese Patient: Case Report Including the Biomechanical Analysis. Diagnostics. 2022; 12(6):1479. https://doi.org/10.3390/diagnostics12061479
Chicago/Turabian StyleSzczęsny, Grzegorz, Mateusz Kopec, Tomasz Szolc, Zbigniew L. Kowalewski, and Paweł Małdyk. 2022. "Deformation of the Titanium Plate Stabilizing the Lateral Ankle Fracture Due to Its Overloading in Case of the Young, Obese Patient: Case Report Including the Biomechanical Analysis" Diagnostics 12, no. 6: 1479. https://doi.org/10.3390/diagnostics12061479
APA StyleSzczęsny, G., Kopec, M., Szolc, T., Kowalewski, Z. L., & Małdyk, P. (2022). Deformation of the Titanium Plate Stabilizing the Lateral Ankle Fracture Due to Its Overloading in Case of the Young, Obese Patient: Case Report Including the Biomechanical Analysis. Diagnostics, 12(6), 1479. https://doi.org/10.3390/diagnostics12061479








