First Neonates with Vertical Transmission of SARS-CoV-2 Infection in Late Pregnancy in West Part of Romania: Case Series
Abstract
:1. Introduction
2. Materials and Methods
2.1. Objects and Data Collection
2.2. Procedures
2.3. Specimen Collection and Virus Detection
2.4. Ethics Approval
3. Results
4. Discussion
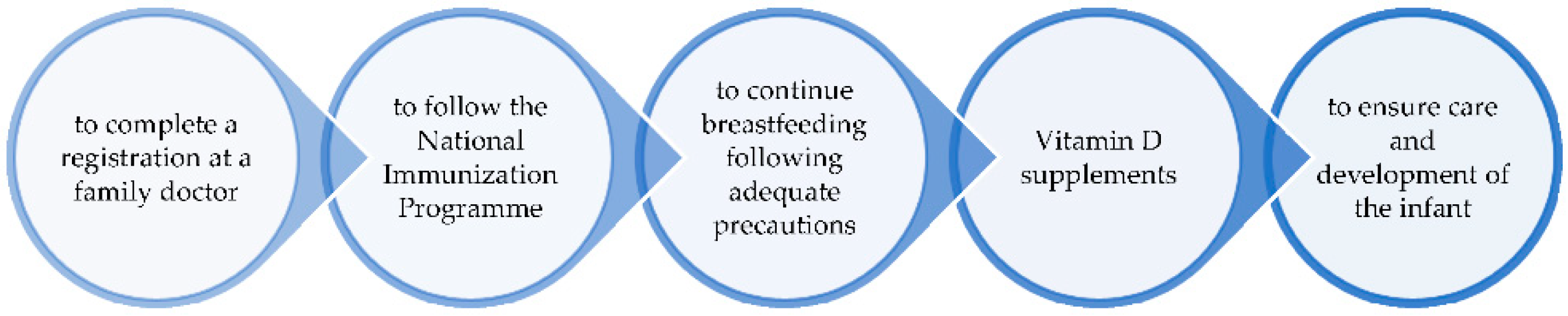
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef] [PubMed]
- National Center for Surveillance and Control of Transmissible Diseases in Bucharest, Romania: Weekly Surveillance Report of COVID-19 Infection. 2022. Available online: https://www.cnscbt.ro/index.php/analiza-cazuri-confirmate-covid19/3140-raport-saptamanal-episaptamana16-2022/file (accessed on 5 June 2022).
- Celewicz, A.; Celewicz, M.; Michalczyk, M.; Woźniakowska-Gondek, P.; Krejczy, K.; Misiek, M.; Rzepka, R. Pregnancy as a Risk Factor of Severe COVID-19. JCM 2021, 10, 5458. [Google Scholar] [CrossRef] [PubMed]
- Allotey, J.; Stallings, E.; Bonet, M.; Yap, M.; Chatterjee, S.; Kew, T.; Debenham, L.; Llavall, A.C.; Dixit, A.; Zhou, D.; et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ 2020, 370, m3320. [Google Scholar] [CrossRef] [PubMed]
- Alzamora, M.C.; Paredes, T.; Caceres, D.; Webb, C.M.; Valdez, L.M.; La Rosa, M. Severe COVID-19 during Pregnancy and Possible Vertical Transmission. Am. J. Perinatol. 2020, 37, 861–865. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.; Guo, J.; Wang, C.; Luo, F.; Yu, X.; Zhang, W.; Li, J.; Zhao, D.; Xu, D.; Gong, Q.; et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet 2020, 395, 809–815. [Google Scholar] [CrossRef] [Green Version]
- Fenizia, C.; Biasin, M.; Cetin, I.; Vergani, P.; Mileto, D.; Spinillo, A.; Gismondo, M.R.; Perotti, F.; Callegari, C.; Mancon, A.; et al. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat. Commun. 2020, 11, 5128. [Google Scholar] [CrossRef]
- Kotlyar, A.M.; Grechukhina, O.; Chen, A.; Popkhadze, S.; Grimshaw, A.; Tal, O.; Taylor, H.S.; Tal, R. Vertical transmission of coronavirus disease 2019: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2021, 224, 35–53.e3. [Google Scholar] [CrossRef]
- World Health Organization. Definition and Categorization of the Timing of Mother-to-Child Transmission of SARS-CoV-2: Scientific Brief; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Akhtar, H.; Patel, C.; Abuelgasim, E.; Harky, A. COVID-19 (SARS-CoV-2) Infection in Pregnancy: A Systematic Review. Gynecol. Obstet. Investig. 2020, 85, 295–306. [Google Scholar] [CrossRef]
- Musa, S.S.; Bello, U.M.; Zhao, S.; Abdullahi, Z.U.; Lawan, M.A.; He, D. Vertical Transmission of SARS-CoV-2: A Systematic Review of Systematic Reviews. Viruses 2021, 13, 1877. [Google Scholar] [CrossRef]
- Kalampokas, T.; Rapani, A.; Papageorgiou, M.; Grigoriadis, S.; Maziotis, E.; Anifandis, G.; Triantafyllidou, O.; Tzanakaki, D.; Neofytou, S.; Bakas, P.; et al. The Current Evidence Regarding COVID-19 and Pregnancy: Where Are We Now and Where Should We Head to Next? Viruses 2021, 13, 2000. [Google Scholar] [CrossRef]
- Vimercati, A.; De Nola, R.; Trerotoli, P.; Metta, M.E.; Cazzato, G.; Resta, L.; Malvasi, A.; Lepera, A.; Ricci, I.; Capozza, M.; et al. COVID-19 Infection in Pregnancy: Obstetrical Risk Factors and Neonatal Outcomes—A Monocentric, Single-Cohort Study. Vaccines 2022, 10, 166. [Google Scholar] [CrossRef]
- Lopes de Sousa, Á.F.; de Carvalho, H.E.F.; Oliveira LB de Schneider, G.; Camargo, E.L.S.; Watanabe, E.; de Andrade, D.; Fernandes, A.F.C.; Mendes, I.A.C.; Fronteira, I. Effects of COVID-19 Infection during Pregnancy and Neonatal Prognosis: What Is the Evidence? Int. J. Environ. Res. Public Health 2020, 17, 4176. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Yang, H.; Cao, Y.; Cheng, W.; Duan, T.; Fan, C.; Fan, S.; Feng, L.; Gao, Y.; He, F.; et al. Expert consensus for managing pregnant women and neonates born to mothers with suspected or confirmed novel coronavirus (COVID-19) infection. Int. J. Gynecol. Obstet. 2020, 149, 130–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Methodology for Surveillance of Acute Respiratory Syndrome with the New Coronavirus (COVID-19). The National Center for Surveillance and Control of Communicable Diseases from Bucharest, Romania. Available online: https://www.cnscbt.ro/index.php/info-medical/2196-metodologia-de-supraveghere-a-covid-19-actualizare-04-01-2021/file (accessed on 5 June 2022).
- Centrul Național de Supraveghereşi Control al BolilorTransmisibile—Calendarul National de Vaccinare. Available online: https://www.cnscbt.ro/index.php/calendarul-national-de-vaccinare (accessed on 5 June 2022).
- Sănătății, M. OrdinprivindmodificareașicompletareaOrdinuluiministruluisănătății nr. 1.513/2020—MinisterulSănătății. Available online: https://www.ms.ro/2020/10/28/ordin-privind-modificarea-si-completarea-ordinului-ministrului-sanatatii-nr-1-513-2020/ (accessed on 5 June 2022).
- Cai, J.; Tang, M.; Gao, Y.; Zhang, H.; Yang, Y.; Zhang, D.; Wang, H.; Liang, H.; Zhang, R.; Wu, B. Cesarean Section or Vaginal Delivery to Prevent Possible Vertical Transmission From a Pregnant Mother Confirmed With COVID-19 to a Neonate: A Systematic Review. Front. Med. 2021, 8, 634949. [Google Scholar] [CrossRef] [PubMed]
- Trippella, G.; Ciarcià, M.; Ferrari, M.; Buzzatti, C.; Maccora, I.; Azzari, C.; Dani, C.; Galli, L.; Chiappini, E. COVID-19 in Pregnant Women and Neonates: A Systematic Review of the Literature with Quality Assessment of the Studies. Pathogens 2020, 9, 485. [Google Scholar] [CrossRef] [PubMed]
- Harding, B.R.; Vora, F. Report of a Confirmed SARS-CoV-2 Positive Newborn after Delivery Despite Negative SARS-CoV-2 Testing on Both Parents. AJP Rep. 2021, 11, e80–e83. [Google Scholar] [CrossRef]
- Olivini, N.; Calo Carducci, F.; Santilli, V.; De Ioris, M.; Scarselli, A.; Alario, D.; Geremia, C.; Lombardi, M.; Marabotto, C.; Mariani, R.; et al. A neonatal cluster of novel coronavirus disease 2019: Clinical management and considerations. Ital. J. Pediatrics 2020, 46, 180. [Google Scholar] [CrossRef]
- Zeng, L.; Xia, S.; Yuan, W.; Yan, K.; Xiao, F.; Shao, J.; Zhou, W. Neonatal Early-Onset Infection With SARS-CoV-2 in 33 Neonates Born to Mothers With COVID-19 in Wuhan, China. JAMA Pediatr. 2020, 174, 722–725. [Google Scholar] [CrossRef] [Green Version]
- Dong, L.; Tian, J.; He, S.; Zhu, C.; Wang, J.; Liu, C.; Yang, J. Possible Vertical Transmission of SARS-CoV-2 From an Infected Mother to Her Newborn. JAMA 2020, 323, 1846–1848. [Google Scholar] [CrossRef] [Green Version]
- Flannery, D.D.; Gouma, S.; Dhudasia, M.B.; Mukhopadhyay, S.; Pfeifer, M.R.; Woodford, E.C.; Triebwasser, J.E.; Gerber, J.S.; Morris, J.S.; Weirick, M.E.; et al. Assessment of Maternal and Neonatal Cord Blood SARS-CoV-2 Antibodies and Placental Transfer Ratios. JAMA Pediatr. 2021, 175, 594–600. [Google Scholar] [CrossRef]
- Yockey, L.J.; Iwasaki, A. Interferons and Proinflammatory Cytokines in Pregnancy and Fetal Development. Immunity 2018, 49, 397–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC. Coronavirus Disease 2019 (COVID-19). Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html (accessed on 5 June 2022).
- Shah, M.D.; Saugstad, O.D. Newborns at risk of COVID-19. J. Perinat. Med. 2020, 48, 423–425. [Google Scholar] [CrossRef]
- Fan, S.; Yan, S.; Liu, X.; Liu, P.; Huang, L.; Wang, S. Human Coronavirus Infections and Pregnancy. Matern. Fetal Med. 2021, 3, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Wesołowska, A.; Orczyk-Pawiłowicz, M.; Bzikowska-Jura, A.; Gawrońska, M.; Walczak, B. Protecting Breastfeeding during the COVID-19 Pandemic: A Scoping Review of Perinatal Care Recommendations in the Context of Maternal and Child Well-Being. Int. J. Environ. Res. Public Health 2022, 19, 3347. [Google Scholar] [CrossRef] [PubMed]
- García, H.; Allende-López, A.; Morales-Ruíz, P.; Miranda-Novales, G.; Villasis-Keever, M.Á. COVID-19 in Neonates with Positive RT–PCR Test. Systematic Review. Arch. Med. Res. 2022, 53, 252–262. [Google Scholar] [CrossRef]
- Hascoët, J.-M.; Jellimann, J.-M.; Hartard, C.; Wittwer, A.; Jeulin, H.; Franck, P.; Morel, O. Case Series of COVID-19 Asymptomatic Newborns With Possible Intrapartum Transmission of SARS-CoV-2. Front. Pediatr. 2020, 8, 568979. [Google Scholar] [CrossRef]
- Amorim dos Santos, J.; Normando, A.G.C.; Carvalho da Silva, R.L.; Acevedo, A.C.; De Luca Canto, G.; Sugaya, N.; Santos-Silva, A.R.; Guerra, E.N.S. Oral Manifestations in Patients with COVID-19: A Living Systematic Review. J. Dent. Res. 2021, 100, 141–154. [Google Scholar] [CrossRef]
- Riad, A.; Gomaa, E.; Hockova, B.; Klugar, M. Oral candidiasis of COVID-19 patients: Case report and review of evidence. J. Cosmet. Dermatol. 2021, 20, 1580–1584. [Google Scholar] [CrossRef]
- Chen, Y.-N.; Hsu, J.-F.; Chu, S.-M.; Lai, M.-Y.; Lin, C.; Huang, H.-R.; Yang, P.-H.; Chiang, M.-C.; Tsai, M.-H. Clinical and Microbiological Characteristics of Neonates with Candidemia and Impacts of Therapeutic Strategies on the Outcomes. J. Fungi 2022, 8, 465. [Google Scholar] [CrossRef]
- Garcia-Vidal, C.; Sanjuan, G.; Moreno-García, E.; Puerta-Alcalde, P.; Garcia-Pouton, N.; Chumbita, M.; Fernandez-Pittol, M.; Pitart, C.; Inciarte, A.; Bodro, M.; et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: A retrospective cohort study. Clin. Microbiol. Infect. 2021, 27, 83–88. [Google Scholar] [CrossRef]
- de Oliveira Santos, G.C.; Vasconcelos, C.C.; Lopes, A.J.O.; de Sousa Cartágenes, M.d.S.; Filho, A.K.D.B.; do Nascimento, F.R.F.; Ramos, R.M.; Pires, E.R.R.B.; de Andrade, M.S.; Rocha, F.M.G.; et al. Candida Infections and Therapeutic Strategies: Mechanisms of Action for Traditional and Alternative Agents. Front. Microbiol. 2018, 9, 1351. [Google Scholar] [CrossRef] [PubMed]
- Buonsenso, D.; Costa, S.; Sanguinetti, M.; Cattani, P.; Posteraro, B.; Marchetti, S.; Carducci, B.; Lanzone, A.; Tamburrini, E.; Vento, G.; et al. Neonatal Late Onset Infection with Severe Acute Respiratory Syndrome Coronavirus 2. Am. J. Perinatol. 2020, 37, 869–872. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Yang, M.; Lai, C.-L. Long COVID-19 Syndrome: A Comprehensive Review of Its Effect on Various Organ Systems and Recommendation on Rehabilitation Plans. Biomedicines 2021, 9, 966. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Demographic and anthropometric characteristics | |||
| Place of birth | CEHPBT | CEHPBT | Secondary maternity |
| Gestational age (weeks) | 38 | 39 | 39 |
| Type of birth | Vaginal | C-section | C-section |
| Presentation at birth | Cephalic | Cephalic | Cephalic |
| Gender | male | male | male |
| Weight at birth (g) | 2990 | 3270 | 2900 |
| Length at birth (cm) | 50 | 52 | 50 |
| Head circumference (cm) | 33 | 34 | 31 |
| Chest circumference (cm) | 33 | 34 | 32 |
| Ponderal index (2PI) | 2.39 | 2.32 | 2.32 |
| Classification based on PI | AGA | AGA | AGA |
| Transition to extrauterine life—Apgar score | |||
| Appearance | General cyanosis | Acrocyanosis | Acrocyanosis |
| Pulse | >100 | >100 | >100 |
| Grimace | PRS | PRS | PRS |
| Activity | Active | Active | Active |
| Respiration | Vigorous cry | Vigorous cry | Vigorous cry |
| At 1 min | 8 | 9 | 9 |
| At 5 min | 10 | 10 | 10 |
| Parameters | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| RDS | mild | none | none |
| Jaundice | |||
| DOL—1 | moderate | none | none |
| DOL—2 | moderate | mild | mild |
| DOL—3, 4 | moderate | mild | moderate |
| DOL—5, 6 | intense | mild | moderate |
| DOL—7 | moderate | in regression | in regression |
| Oral candidiasis | |||
| DOL—1, 2 | no | no | no |
| DOL—3–5 | yes | yes | yes |
| DOL—6 | yes | no | yes |
| DOL—7 | yes | discharged | discharged |
| Nappy rash | |||
| DOL—1–3 | no | no | no |
| DOL—4–7 | yes | no | no |
| Parameters | Patient 1 | Patient 2 | Patient 3 | Reference Range | ||||
|---|---|---|---|---|---|---|---|---|
| DOL-1 | DOL-3 | DOL-5 | DOL-1 | DOL-2 | DOL-3 | DOL-2 | Age 0–month | |
| Leukocytes | 11.2 | 8.18 | 9.00 | 20.52 | 12.38 | NA | 12.76 | 9–30 × 103/μL |
| Granulocytes | 6.3 | 4.19 | 1.21 | 13.87 | 8.50 | NA | 7.78 | 1–20 × 103/μL |
| Lymphocytes | 4.3 | 1.94 | 5.47 | 5.11 | 2.60 | NA | 2.95 | 2–11 × 103/μL |
| Hemoglobin | 18.1 | 16.8 | 17.5 | 16.5 | 16.8 | NA | 19.2 | 13.4–19.9 g/dL |
| Hematocrit | 51.9 | 46.1 | 48.6 | 47.9 | 47.7 | NA | 52.5 | 42–65% |
| Thrombocytes | 253.000 | 172.000 | 178.000 | 183.000 | 180.000 | NA | 246.000 | 242.000–378.000/μL |
| 1 CRP | 7.4 | 0.99 | <5 | 32.36 | NA | 10.35 | <0.5 | <0.5 mg/dL |
| 2 ALT | 33 | NA | 38 | 24 | NA | NA | 12 | 0–35 U/L |
| 3 AST | 86 | NA | 69 | 50 | NA | NA | 73 | 14–36 U/L |
| 4 CK | NA | NA | NA | 305 | NA | NA | 942 | 65–580 U/L |
| 5 TB | 6.2 | 11.2 | 13.6 | - | NA | NA | 8.55 | <6.0 mg/dL |
| 6 LDH | NA | NA | NA | 668 | NA | NA | 735 | 160–450 U/L |
| Ferritin | NA | 359 | 627 | 216 | NA | NA | 92 | 25–200 μg/L |
| IgG anti SpikeS1 quantitative | NA | NA | <2 | <2 | NA | NA | 187 | <17.8 7 BAU = NEGATIVE;>17.8 BAU = POSITIVE |
| Anti-SARS-CoV-2 TOTAL (IgA IgM IgG) | NA | NA | 0.05 | 0.09 | NA | NA | NA | 0.00–0.99 8 s/co = UNEREACTIVE;≥1.00 REACTIVE |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iacob, D.; Enatescu, I.; Dima, M.; Bernad, E.; Pantea, M.; Bozgan, D.; Bernad, S.; Craina, M. First Neonates with Vertical Transmission of SARS-CoV-2 Infection in Late Pregnancy in West Part of Romania: Case Series. Diagnostics 2022, 12, 1668. https://doi.org/10.3390/diagnostics12071668
Iacob D, Enatescu I, Dima M, Bernad E, Pantea M, Bozgan D, Bernad S, Craina M. First Neonates with Vertical Transmission of SARS-CoV-2 Infection in Late Pregnancy in West Part of Romania: Case Series. Diagnostics. 2022; 12(7):1668. https://doi.org/10.3390/diagnostics12071668
Chicago/Turabian StyleIacob, Daniela, Ileana Enatescu, Mirabela Dima, Elena Bernad, Manuela Pantea, Daiana Bozgan, Sandor Bernad, and Marius Craina. 2022. "First Neonates with Vertical Transmission of SARS-CoV-2 Infection in Late Pregnancy in West Part of Romania: Case Series" Diagnostics 12, no. 7: 1668. https://doi.org/10.3390/diagnostics12071668
APA StyleIacob, D., Enatescu, I., Dima, M., Bernad, E., Pantea, M., Bozgan, D., Bernad, S., & Craina, M. (2022). First Neonates with Vertical Transmission of SARS-CoV-2 Infection in Late Pregnancy in West Part of Romania: Case Series. Diagnostics, 12(7), 1668. https://doi.org/10.3390/diagnostics12071668







