Morphological and Molecular Characterizations of Cochliomyia hominivorax (Diptera: Calliphoridae) Larvae Responsible for Wound Myiasis in French Guiana
Abstract
1. Introduction
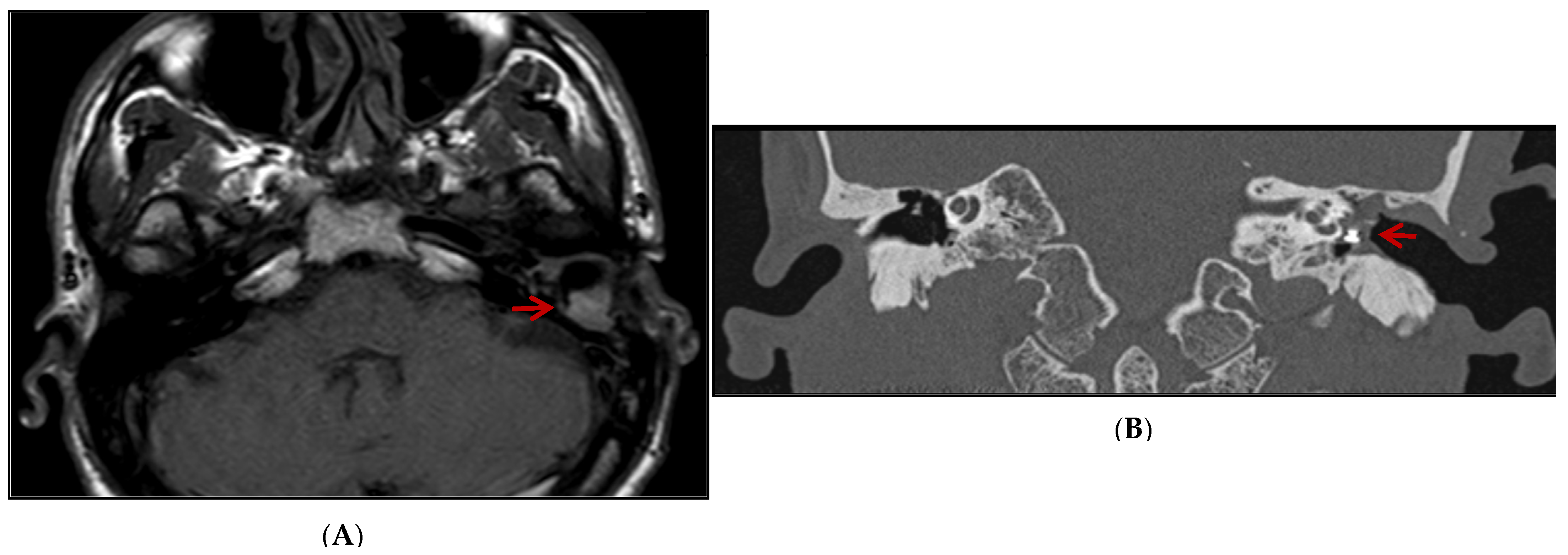
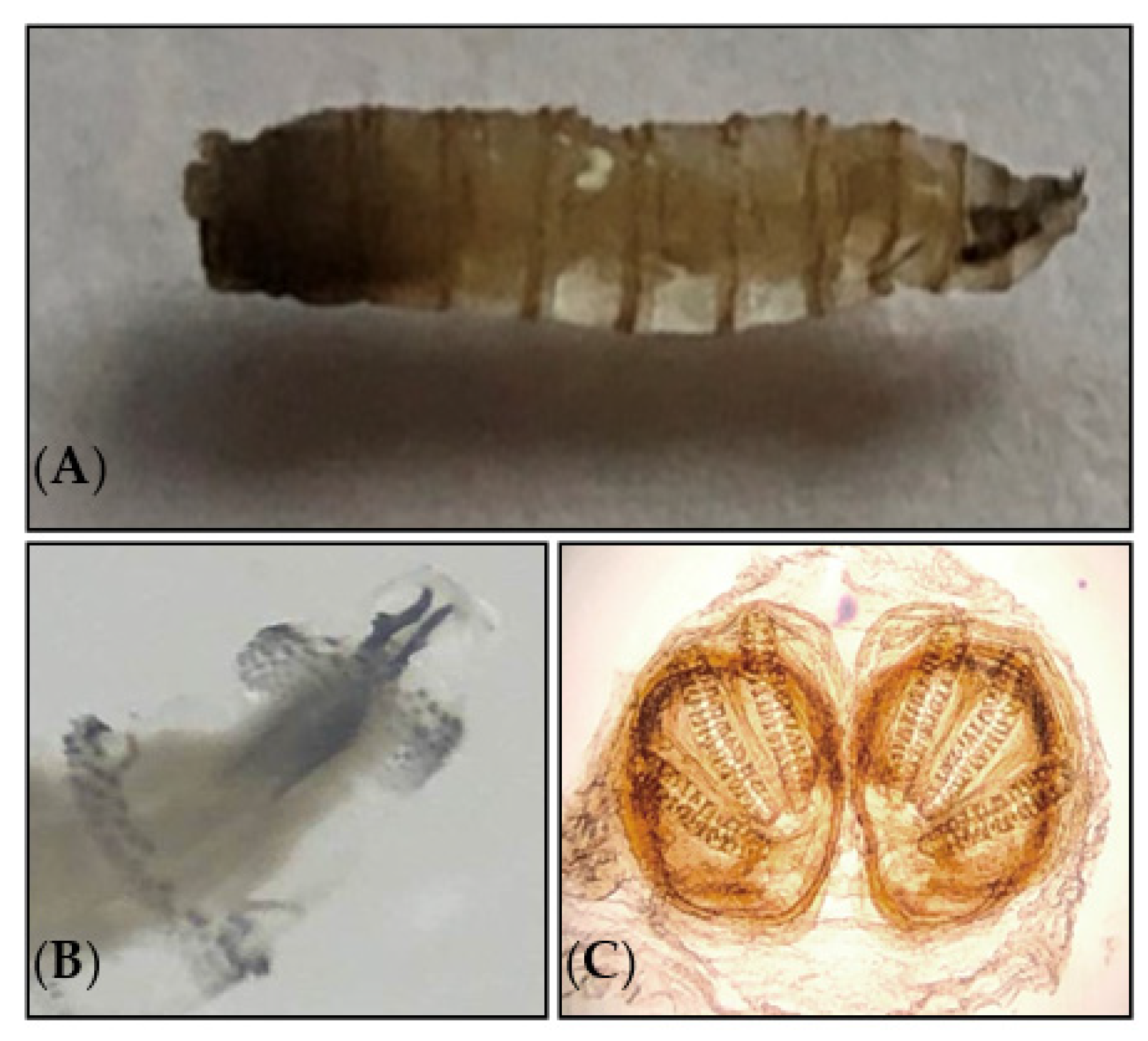
2. Case Presentation
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zumpt, F. Myiasis in Man and Animals in the Old World; Butterworth: London, UK, 1965. [Google Scholar]
- Robbins, K.; Khachemoune, A. Cutaneous myiasis: A review of the common types of myiasis. Int. J. Dermatol. 2010, 49, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.J.; Wall, R.L.; Stevens, J.R. Traumatic Myiasis: A Neglected Disease in a Changing World. Annu. Rev. Entomol. 2016, 61, 159–176. [Google Scholar] [CrossRef] [PubMed]
- Onyeama, C.O.; Njai, P.C. Cutaneous myiasis (Tumbu fly larvae): A case report. Niger. J. Paediatr. 2005, 32, 26–27. [Google Scholar] [CrossRef]
- McGarry, J.W. Tropical myiases: Neglected and well-travelled. Lancet Infect. Dis. 2014, 14, 672–674. [Google Scholar] [CrossRef]
- Kuria, S.K.; Oyedeji, A.O. Human myiasis cases originating and reported in Africa for the last two decades (1998–2018): A review. Acta Trop. 2020, 210, 105590. [Google Scholar] [CrossRef]
- Antunes, A.A.; Santos Tde, S.; Avelar, R.L.; Martins Neto, E.C.; Macedo Neres, B.; Laureano Filho, J.R. Oral and maxillofacial myiasis: A case series and literature review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, e81–e85. [Google Scholar] [CrossRef]
- Kumar, G.V.; Sowmya, G.; Shivananda, S. Chrysomya bezziana oral myiasis. J. Glob. Infect. Dis. 2011, 3, 393–395. [Google Scholar] [CrossRef]
- Dutto, M.; Pellegrino, M.; Vanin, S. Nosocomial myiasis in a patient with diabetes. J. Hosp. Infect. 2013, 83, 74–76. [Google Scholar] [CrossRef]
- Manickam, A.; Sengupta, S.; Saha, J.; Basu, S.K.; Ranjan Das, J.; Sannigrahi, R. Myiasis of the tracheostomy wound: A case report with review of literature. Otolaryngology 2015, 5, 198. [Google Scholar]
- Villalobos, G.; Vega-Memije, M.E.; Maravilla, P. Myiasis caused by Dermatobia hominis: Countries with increased risk for travelers going to neotropic areas. Int. J. Dermatol. 2016, 55, 1060–1068. [Google Scholar] [CrossRef]
- Goddard, J. Physician’s Guide to Arthropods of Medical Importance: Flies whose Maggots cause Myiasis Inhumans, 2nd ed.; CRC Press: Boca Raton, FL, USA, 1996; Volume 2, pp. 169–187. [Google Scholar]
- World Health Organization: History of the Development of the ICD. Available online: https://icd.who.int/browse10/2019/en#/B87 (accessed on 1 January 2021).
- Shearer, D.; Wall, R. Veterinary Entomology: Athropod Ectoparasites of Veterinary Importance; Chapman and Hall: London, UK; New York, NY, USA, 1997; p. 203. [Google Scholar]
- Bowering, C.K. Diabetic foot ulcers. Pathophysiology, assessment, and therapy. Can Fam. Physician 2001, 47, 1007–1016. [Google Scholar] [PubMed]
- Singh, A.; Singh, Z. Incidence of myiasis among humans-a review. Parasitol. Res. 2015, 114, 3183–3199. [Google Scholar] [CrossRef] [PubMed]
- Pallai, L.; Hodge, J.; Fishman, S.J.; Millikan, L.E.; Phelps, R.G. Case report: Myiasis—The botfly boil. Am. J. Med. Sci. 1992, 303, 245–248. [Google Scholar]
- Caissie, R.; Beaulieu, F.; Giroux, M.; Berthod, F.; Landry, P. Cutaneous myiasis: Diagnosis, treatment, and prevention. J. Oral Maxillofac. Surg. 2008, 66, 560–568. [Google Scholar] [CrossRef]
- Sherman, R.A. Wound myiasis in urban and suburban United States. Arch. Intern. Med. 2000, 160, 2004–2014. [Google Scholar] [CrossRef]
- Adisa, C.; Mbanaso, A. Furuncular myiasis of the breast caused by the larvae of the tumbu fly (Cordylobia anthropophaga). BMC Surg. 2004, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Szczurko, C.; Dompmartin, A.; Moreau, A.; Belloy, F.; Remond, B.; Leroy, D. Ultrasonography of furuncular cutaneous myiasis: Detection of Dermatobia hominis larvae and treatment. Int. J. Dermatol. 1994, 33, 282–283. [Google Scholar] [CrossRef] [PubMed]
- Giangaspero, A.; Marangi, M.; Balotta, A.; Venturelli, C.; Szpila, K.; Di Palma, A. Wound myiasis caused by Sarcophaga (Liopygia) Argyrostoma (robineau-desvoidy) (Diptera: Sarcophagidae): Additional evidences of the morphological identification dilemma and molecular investigation. Sci. World J. 2017, 2017, 9064531. [Google Scholar] [CrossRef]
- Noutsis, C.; Millikan, L.E. Myiasis. Dermatol Clin. 1994, 12, 729–736. [Google Scholar] [CrossRef]
- Gontijo, J.R.V.; Bittencourt, F.V. Wound myiasis: The role of entodermoscopy. An. Bras. Dermatol. 2018, 93, 746–748. [Google Scholar] [CrossRef]
- Marangi, M.; Hall, M.J.; Aitken, A.; Ready, P.D.; Giangaspero, A. Origins of Wohlfahrtia magnifica in Italy based on the identification of mitochondrial cytochrome b gene haplotypes. Parasitol. Res. 2016, 115, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, E.; Gaskin, K.; Wojcik, S. Sonographic Detection of Cutaneous Myiasis. Clin. Pract. Cases Emerg. Med. 2019, 3, 438–439. [Google Scholar] [CrossRef] [PubMed]
- Puthran, N.; Hegde, V.; Anupama, B.; Andrew, S. Ivermectin treatment for massive orbital myiasis in an empty socket with concomitant scalp pediculosis. Indian J. Ophthalmol. 2012, 60, 225–227. [Google Scholar] [CrossRef]
- Sunny, B.; Sulthana, L.; James, A.; Sivakumar, T. Maggot Infestation: Various Treatment Modalities. J. Am. Coll. Clin. Wound Spec. 2018, 8, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Whitworth, T. Keys to the genera and species of blow flies (Diptera: Calliphoridae) of America North of Mexico. Proc. Entomol. Soc. 2006, 108, 689–725. [Google Scholar]
- Neira, P.; Muñoz, N.; Cantero, D. Miasis auricular por Cochliomyia hominivorax (Diptera: Calliphoridae) (Coquerel, 1858) [Auricular myiasis cause by Cochliomyia hominivorax (Diptera: Calliphoridae) (Coquerel, 1858)]. Rev. Med. Chil. 2002, 130, 907–909. [Google Scholar] [CrossRef]
- Menghi, C.I.; Gatta, C.L.; Oliva, A. Otomiasis por Cochliomyia hominivorax en dos niños del conurbano bonaerense, Argentina [Otomyiasis by Cochliomyia hominivorax in two children from the outskirts of Buenos Aires, Argentina]. Rev. Argent. Microbiol. 2010, 42, 176–178. [Google Scholar]
- Lindsay, R.; Stancil, J.; Ray, J.M. Myiasis of facial wounds by Cochliomyia hominivorax sustained in a natural disaster in Haiti. Otolaryngol. Head Neck Surg. 2010, 143, 595–596. [Google Scholar] [CrossRef]
- Costa-Júnior, L.M.; Chaves, D.P.; Brito, D.R.B.; Santos, V.A.F.D.; Costa-Júnior, H.N.; Barros, A.T.M. A review on the occurrence of Cochliomyia hominivorax (Diptera: Calliphoridae) in Brazil. Rev. Bras. Parasitol. Vet. 2019, 28, 548–562. [Google Scholar] [CrossRef] [PubMed]
- Reichard, R.E.; Vargas-Teran, M.; Abu Sowa, M. Myiasis: The battle continues against screwworm infestation. Public Health Pract. 1992, 13, 130–137. [Google Scholar]
- Khurana, S.; Biswal, M.; Bhatti, H.S.; Pandav, S.S.; Gupta, A.; Chatterjee, S.S.; Lyngdoh, W.V.; Malla, N. Ophthalmomyiasis: Three cases from North India. Indian J. Med. Microbiol. 2010, 28, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Lima Júnior, S.M.; Asprino, L.; Prado, A.P.; Moreira, R.W.; de Moraes, M. Oral myiasis caused by Cochliomyia hominivorax treated nonsurgically with nitrofurazone: Report of 2 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e70–e73. [Google Scholar] [CrossRef] [PubMed]
- Duro, E.A.; Mariluis, J.C.; Mulieri, P.R. Umbilical myiasis in a human newborn. J. Perinatol. 2007, 27, 250–251. [Google Scholar] [CrossRef]
- Trombetta, L.; Oliva, A.; Galache, V.; Bava, J.; Troncoso, A. Cutaneous myiasis due to Cochliomyia hominivorax in a drug user. J. Infect. Dev. Ctries 2009, 3, 873–876. [Google Scholar] [CrossRef]
- Tai, R.; Marsh, M.A.; Rao, R.; Kurniali, P.C.; DiNino, E.; Meharg, J.V. Nasal Myiasis Caused by Cochliomyia Hominivorax in the United States: A Case Report. Am. J Infect Dis. 2011, 7, 107–109. [Google Scholar]
- Acha, P.N.; Szyfres, B. Zoonosis y Enfermedades Transmisibles Comunes al Hombre y a los Animale; Volumen III. Parasitosis; Organización Panamericana de la Salud: Washington, DC, USA, 2003; 230p. [Google Scholar]
- Visciarelli, E.; Costamagna, S.; Lucchi, L.; Basabe, N. Miasis Humana en Bahía Blanca, Argentina: Periodo 2000/2005. Neotropical. Entomol. 2007, 36, 605–611. [Google Scholar] [CrossRef]
- Batista-da-Silva, J.A.; Moya-Borja, G.E.; Queiroz, M.M. Factors of susceptibility of human myiasis caused by the New World screw-worm, Cochliomyia hominivorax in São Gonçalo, Rio de Janeiro, Brazil. J. Insect. Sci. 2011, 11, 14. [Google Scholar] [CrossRef]
- Wittenberg, R.; Cock, M.J.W. (Eds.) Invasive Alien Species: A Toolkit of Best Prevention and Management Practices; Cabi Publishing: Wallingford, UK, 2001. [Google Scholar]
- Concha, C.; Palavesam, A.; Guerrero, F.D.; Sagel, A.; Li, F.; Osborne, J.A.; Hernandez, Y.; Pardo, T.; Quintero, G.; Vasquez, M.; et al. A transgenic male-only strain of the New World screwworm for an improved control program using the sterile insect technique. BMC Biol. 2016, 14, 72. [Google Scholar] [CrossRef] [PubMed]
- Stadler, F. A Complete Guide to Maggot Therapy: Clinical Practice, Therapeutic Principles, Production, Distribution, and Ethics; Open Book Publishers: Cambridge, UK, 2022; pp. 121–142. [Google Scholar]
- Laake, E.W.; Cushing, E.C.; Parish, H.E. Biology of the Primary Screwworm Fly, Cochliomyia americana, and a Comparison of its Stages with those of C. macellaria. United States Dep. Agricul. Tech. Bull. 1936, 500, 24. [Google Scholar]
- Vargas-Terán, M.; Spradbery, J.P.; Hofmann, H.C.; Tweddle, N.E. Impact of screwworm eradication programmes using the sterile insect. Technique. In Sterile Insect Technique. Principles and Practice in Area-Wide Integrated Pest Management, 2nd ed.; Dyck, V.A., Hendrichs, J., Robinson, A.S., Eds.; CRC Press: Boca Raton, FL, USA, 2021. [Google Scholar]
- Altuna, M.; Hickner, P.V.; Castro, G.; Mirazo, S.; Pérez de León, A.A.; Arp, A.P. New World screwworm (Cochliomyia hominivorax) myiasis in feral swine of Uruguay: One Health and transboundary disease implications. Parasit. Vectors 2021, 14, 26. [Google Scholar] [CrossRef] [PubMed]
- Villamil-Gómez, W.E.; Cardona-Ospina, J.A.; Prado-Ojeda, J.S.; Hernández-Prado, H.; Figueroa, M.; Causil-Morales, P.N.; Pérez-Reyes, K.; Palechor-Ocampo, L.A.; Rodríguez-Morales, A.J. Pin-Site Myiasis Caused by Screwworm Fly in Nonhealed Wound, Colombia. Emerg Infect Dis. 2019, 25, 379–380. [Google Scholar] [CrossRef] [PubMed]
- Bailey, M.S. Tropical skin diseases in British military personnel. J. R. Army. Med. Corps. 2013, 159, 224–228. [Google Scholar] [CrossRef]
- Fatal scalp myiasis: Autopsy finding of Cochliomyia hominivorax (diptera: Calliphoridae) in the brain cavity. Can. Soc. Forensic Sci. J. 2007, 40, 183–186.
- Coronado, A.; Kowalski, A. Current status of the New World screwworm Cochliomyia hominivorax in Venezuela. Med. Vet. Entomol. 2009, 23, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Duque, F.L.; Ardila, C.M. Oral myiasis caused by the screwworm Cochliomyia hominivorax treated with subcutaneous ivermectin and creolin: Report of six cases after trauma. Dent. Traumatol. 2011, 27, 404–407. [Google Scholar] [CrossRef]
- Francesconi, F.; Lupi, O. Myiasis. Clin. Microbiol. Rev. 2012, 25, 79–105. [Google Scholar] [CrossRef]
- Carvalho, R.A.; Azeredo-Espin, A.M.L.; Torres, T.T. Deep Sequencing of New World Screw-Worm Transcripts to Discover Genes Involved in Insecticide Resistance. BMC Genom. 2010, 11, 695. [Google Scholar] [CrossRef]
- Mastrangelo, T.; Fresia, P.; Lyra, M.L.; Rodrigues, R.A.; Azeredo-Espin, A.M.L. Genetic diversity and population structure of the New World screwworm fly from the Amazon region of Brazil. Acta Trop. 2014, 138, S26–S33. [Google Scholar] [CrossRef] [PubMed]
- Arp, A.P.; Quintero, G.; Sagel, A.; Batista, R.G.; Phillips, P.L.; Hickner, P.V. The microbiome of wild and mass-reared new world screwworm, Cochliomyia hominivorax. Sci Rep. 2022, 12, 1042. [Google Scholar] [CrossRef] [PubMed]
- Mehr, Z.; Powers, N.R.; Konkol, K.A. Myiasis in a wounded soldier returning from Panama. J. Med. Entomol. 1991, 28, 553–554. [Google Scholar] [CrossRef]
- Sutherst, R.W.; Spradbery, J.P.; Maywald, G.F. The potential geographical distribution of the Old World screw-worm fly, Chrysomya bezziana. Med. Vet. Entomol. 1989, 3, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Mayer, D.G.; Atzeni, M.G.; Butler, D.G. Adaptation of CLIMEX for spatial screwworm fly population dynamics. Math. Comput. Simul. 1992, 33, 439–444. [Google Scholar] [CrossRef]
- Spradbery, J.P. Screw-worm fly: A tale of two species. Agricul. Zoolog. Rev. 1994, 6, 1–62. [Google Scholar]
- E1-Azazy, O.M.E. Wound myiasis caused by Cochliomyia hominivorax in Libya. Vet. Rec. 1989, 124, 103. [Google Scholar] [CrossRef]
- Beesley, W.N. The New World screw-worm fly in north Africa. Ann. Trop. Med. Parasitol. 1991, 85, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Chermette, R. A case of canine otitis due to screwworm, Cochliomyia hominivorax, in France. Vet. Record. 1989, 124, 641. [Google Scholar] [CrossRef] [PubMed]
- Searson, J.; Sanders, L.; Davis, G.; Tweddle, N.; Thornber, P. Screwworm Fly Myiasis in an Overseas Traveller—A Case Report. Commun. Dis. Intell. 1992, 16, 239–240. [Google Scholar]
- Galvin, T.J.; Wyss, J.H. Screwworm eradication program in Central America. Ann. N. Y. Acad. Sci. 1996, 791, 233–240. [Google Scholar] [CrossRef]
- Garris, G. On the front of defense: Veterinarian averts screwworm outbreak. J. Am. Vet. Med. Assoc. 1998, 212, 159. [Google Scholar]
- Tandonnet, S.; Cardoso, G.A.; Mariano-Martins, P.; Monfardini, R.D.; Cunha, V.A.S.; de Carvalho, R.A.; Torres, T.T. Molecular basis of resistance to organophosphate insecticides in the New World screw-worm fly. Parasit. Vectors. 2020, 13, 562. [Google Scholar] [CrossRef]
- Pradinaud, R.; Rivierez, E. Myiase furonculeuse de la paupière supérieure en Guyane Française [Furuncular myiasis of the upper eyelid in French Guiana]. Bull. Soc. Fr. Dermatol. Syphiligr. 1968, 75, 808–810. [Google Scholar] [PubMed]
- Spradbery, J.P. A Manual for the Diagnosis of the Screwworm Fly, Fisheries and Forestry; Department of Agriculture: Canberra, Australia, 2002; p. 2. [Google Scholar]
- Folmer, O.; Black, M.; Hoeh, W.; Lutz, R.; Vrijenhoek, R. DNA primers for amplification of mitochondrial cytochrome c oxidase subunit I from diverse metazoan invertebrates. Mol. Mar. Biol. Biotechnol. 1994, 3, 294–299. [Google Scholar] [PubMed]
- Szakacs, T.A.; MacPherson, P.; Sinclair, B.J.; Gill, B.D.; McCarthy, A.E. Nosocomial myiasis in a Canadian intensive care unit. CMAJ. 2007, 177, 719–720. [Google Scholar] [CrossRef][Green Version]
- Carvalho, R.W.; Santos, T.S.; Antunes, A.A.; Laureano Filho, J.R.; Anjos, E.D.; Catunda, R.B. Oral and maxillofacial myiasis associated with epidermoid carcinoma: A case report. J. Oral Sci. 2008, 50, 103–105. [Google Scholar] [CrossRef]
- Shenouda, M.; Enten, G.; Nguyen, T.; Mangar, D.; Camporesi, E. Human Botfly: A Case Report and Overview of Differential Diagnosis. J. Investig. Med. High Impact Case Rep. 2018, 6, 2324709618801692. [Google Scholar] [CrossRef]
- Ruiz-Zapata, J.D.; Figueroa-Gutiérrez, L.M.; Mesa-Franco, J.A.; Moreno-Gutierrez, P.A. Umbilical Myiasis by Cochliomyia hominivorax in an Infant in Colombia. Front. Med. (Lausanne) 2020, 6, 292. [Google Scholar] [CrossRef]
- Mathison, B.A.; Pritt, B.S. Laboratory identification of arthropod ectoparasites. Clin. Microbiol. Rev. 2014, 27, 48–67. [Google Scholar] [CrossRef] [PubMed]
- Brumpt, L.C.; Poulet, J. Observation à paris d’un cas de myiase sous-cutanée à Dermatobia contractée en Guyane. Bull. Soc. Pathol. Exot. Fil. 1965, 58, 88–92. [Google Scholar]
- Schreiber, H.A.; Renkl, A.C.; Lapinski, W.; Scharffetter-Kochanek, K.; Weiss, J.M. Myiasis after study trip to French Guiana. J. Dtsch. Dermatol. Ges. 2010, 8, 357–359. [Google Scholar] [CrossRef]
- Graveriau, C.; Peyron, F. Cutaneous myiasis. Travel Med. Infect. Dis. 2017, 16, 70–71. [Google Scholar] [CrossRef]
- Blaizot, R.; Vanhecke, C.; Le Gall, P.; Duvignaud, A.; Receveur, M.C.; Malvy, D. Furuncular myiasis for the Western dermatologist: Treatment in outpatient consultation. Int. J. Dermatol. 2018, 57, 227–230. [Google Scholar] [CrossRef]
- Couppié, P.; Roussel, M.; Rabarison, P.; Sockeel, M.J.; Sainte-Marie, D.; Marty, C.; Carme, B. Nosocomial nasal myiasis owing to Cochliomyia hominivorax: A case in French Guiana. Int. J. Dermatol. 2005, 44, 302–303. [Google Scholar] [CrossRef]
- Denion, E.; Dalens, P.H.; Couppié, P.; Aznar, C.; Sainte-Marie, D.; Carme, B.; Petitbon, J.; Pradinaud, R.; Gérard, M. External ophthalmomyiasis caused by Dermatobia hominis. A retrospective study of nine cases and a review of the literature. Acta Ophthalmol. Scand. 2004, 82, 576–584. [Google Scholar]
- Sherman, R.A. Maggot therapy for foot and leg wounds. Int. J. Low Extrem. Wounds 2002, 1, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Pierre-filho, P.D.T.P.; Minguini, N.; Pierre, L.M.; Pierre, A.M. Use of ivermectin in the treatment of orbital myiasis caused by Cochliomyia hominivorax. Scand. J. Infect. Dis. 2004, 36, 503–505. [Google Scholar] [CrossRef] [PubMed]
- Osorio, J.; Moncada, L.; Molano, A.; Valderrama, S.; Gualtero, S.; Franco-Paredes, C. Role of ivermectin in the treatment of severe orbital myiasis due to Cochliomyia hominivorax. Clin. Infect. Dis. 2006, 43, e57–e59. [Google Scholar] [CrossRef]
- Tay, S.Y.; Ramasamy, B.R.; Watson, D.A.; Montoya, M. Treatment of nasal myiasis with ivermectin irrigation. BMJ Case Rep. 2018, 2018, bcr2017224142. [Google Scholar] [CrossRef]

| Patient | Etiologic Species | Infected Location | Clinical Symptom | Treatment | Reference | |||
|---|---|---|---|---|---|---|---|---|
| Myiasis Type | Age (Years Old) | Sex | Myiasis Origin | |||||
| Cutaneous myiasis | 46 | ♂ | French Guiana | Dermatobia hominis | Scalp | Scalp inflamation and impetigo | Incision | [77] |
| Furuncular myiasis | ? | ? | French Guiana | ? | Eye | ? | ? | [69] |
| Ophthalmomyiasis (9 cases) | 1.5 months to 45 | ♂♀ | 8 (French Guiana) and 1 (Brazil) | Dermatobia hominis | Eye | Varied depending on the patient’s case | Petroleum ointment, ivermectin | [82] |
| Nosocomial myiasis | 84 | ♂ | French Guiana | Cochliomyia hominivorax | Right nasal | Posterior purulent rhinorrhoea and edema on the forehead | Oral ivermectin | [81] |
| Cutaneous myiasis | 31 | ♂ | French Guiana | Dermatobia hominis | Limbs | Inflammatory nodule | Topical disinfectants and systemic amoxicillin/clavulanic acid | [78] |
| Cutaneous myiasis | 66 | ♂ | French Guiana | Dermatobia hominis | Forearms | Inflammatory nodule | pressing the coil, paraffin oil | [79] |
| Furuncular myiasis (3 cases) | 39 1, 42 2, 59 3 | ♂ 1, ♀ 2, ♀ 3 | French guiana 1, Senegal 2, Cameroon 3 | Dermatobia hominis 1, Cordylobia anthropophaga 2, C. rodhaini 3 | Leg 1, left buttock 2, scalp & arm 3 | Punctum 1, inflammatory nodule 2, scalp nodules, pain, fatigue, and facial edema 3 | Varied depending on fly species | [80] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akhoundi, M.; Mathieu, A.; Hannachi, W.; Nasrallah, J.; Quezel, G.; Blaizot, R.; Blanchet, D.; Ben Romdhane, H.; Epelboin, L.; Izri, A. Morphological and Molecular Characterizations of Cochliomyia hominivorax (Diptera: Calliphoridae) Larvae Responsible for Wound Myiasis in French Guiana. Diagnostics 2023, 13, 2575. https://doi.org/10.3390/diagnostics13152575
Akhoundi M, Mathieu A, Hannachi W, Nasrallah J, Quezel G, Blaizot R, Blanchet D, Ben Romdhane H, Epelboin L, Izri A. Morphological and Molecular Characterizations of Cochliomyia hominivorax (Diptera: Calliphoridae) Larvae Responsible for Wound Myiasis in French Guiana. Diagnostics. 2023; 13(15):2575. https://doi.org/10.3390/diagnostics13152575
Chicago/Turabian StyleAkhoundi, Mohammad, Alexandre Mathieu, Wajih Hannachi, Jade Nasrallah, Guillaume Quezel, Romain Blaizot, Denis Blanchet, Habib Ben Romdhane, Loïc Epelboin, and Arezki Izri. 2023. "Morphological and Molecular Characterizations of Cochliomyia hominivorax (Diptera: Calliphoridae) Larvae Responsible for Wound Myiasis in French Guiana" Diagnostics 13, no. 15: 2575. https://doi.org/10.3390/diagnostics13152575
APA StyleAkhoundi, M., Mathieu, A., Hannachi, W., Nasrallah, J., Quezel, G., Blaizot, R., Blanchet, D., Ben Romdhane, H., Epelboin, L., & Izri, A. (2023). Morphological and Molecular Characterizations of Cochliomyia hominivorax (Diptera: Calliphoridae) Larvae Responsible for Wound Myiasis in French Guiana. Diagnostics, 13(15), 2575. https://doi.org/10.3390/diagnostics13152575






