Ultra-High-Resolution Electrocardiography Enables Earlier Detection of Transmural and Subendocardial Myocardial Ischemia Compared to Conventional Electrocardiography
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Animals
2.3. The Model of Acute Transmural Myocardial Ischemia in the Rat
2.4. The Model of Gradual Subendocardial Ischemia in Pigs
2.5. Registration of UHR ECG and Signal Processing
2.6. Statistical Analysis
3. Results
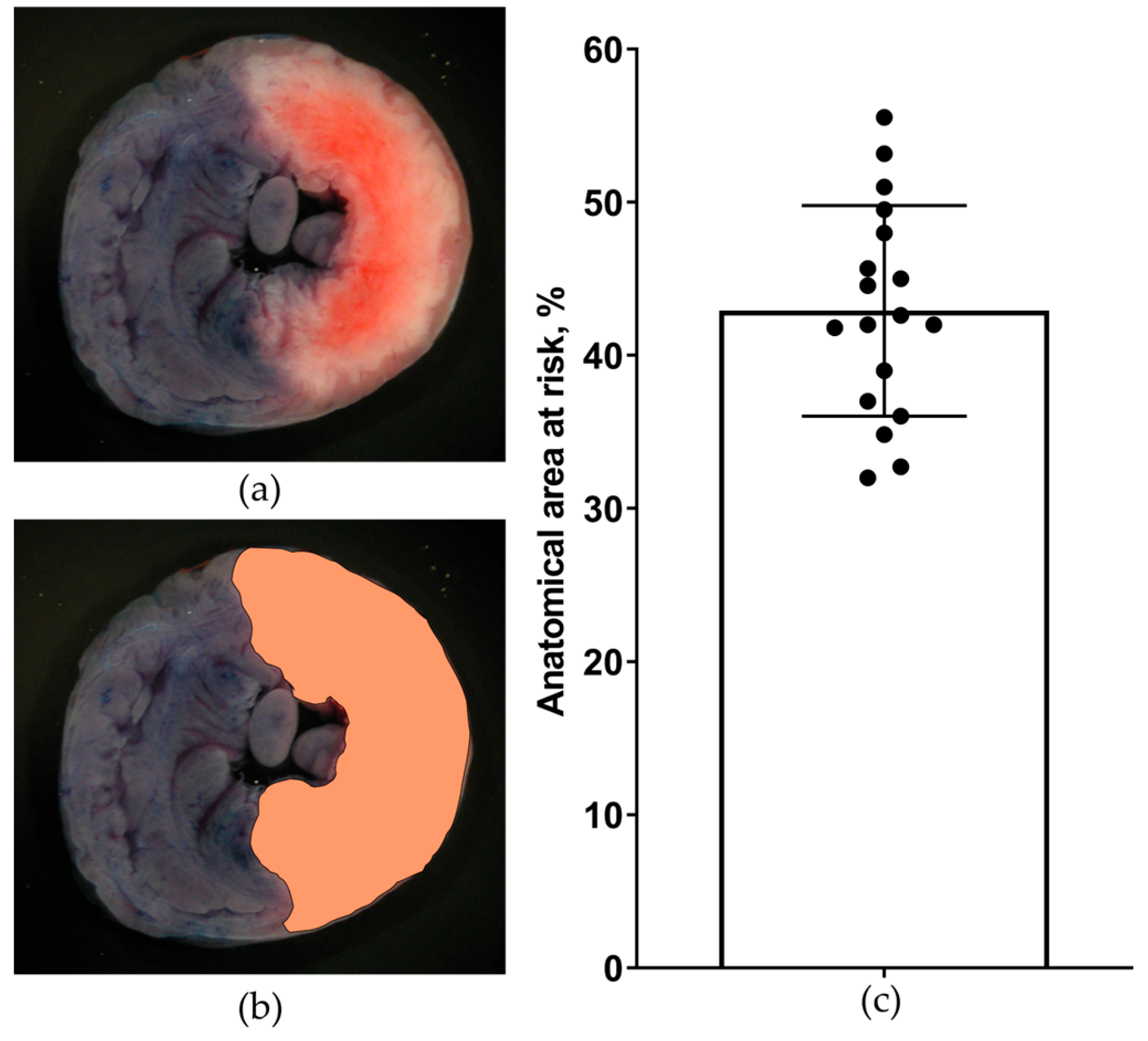
3.1. Verification of Transmural and Subendocardial Ischemia
3.2. Physiological Monitoring
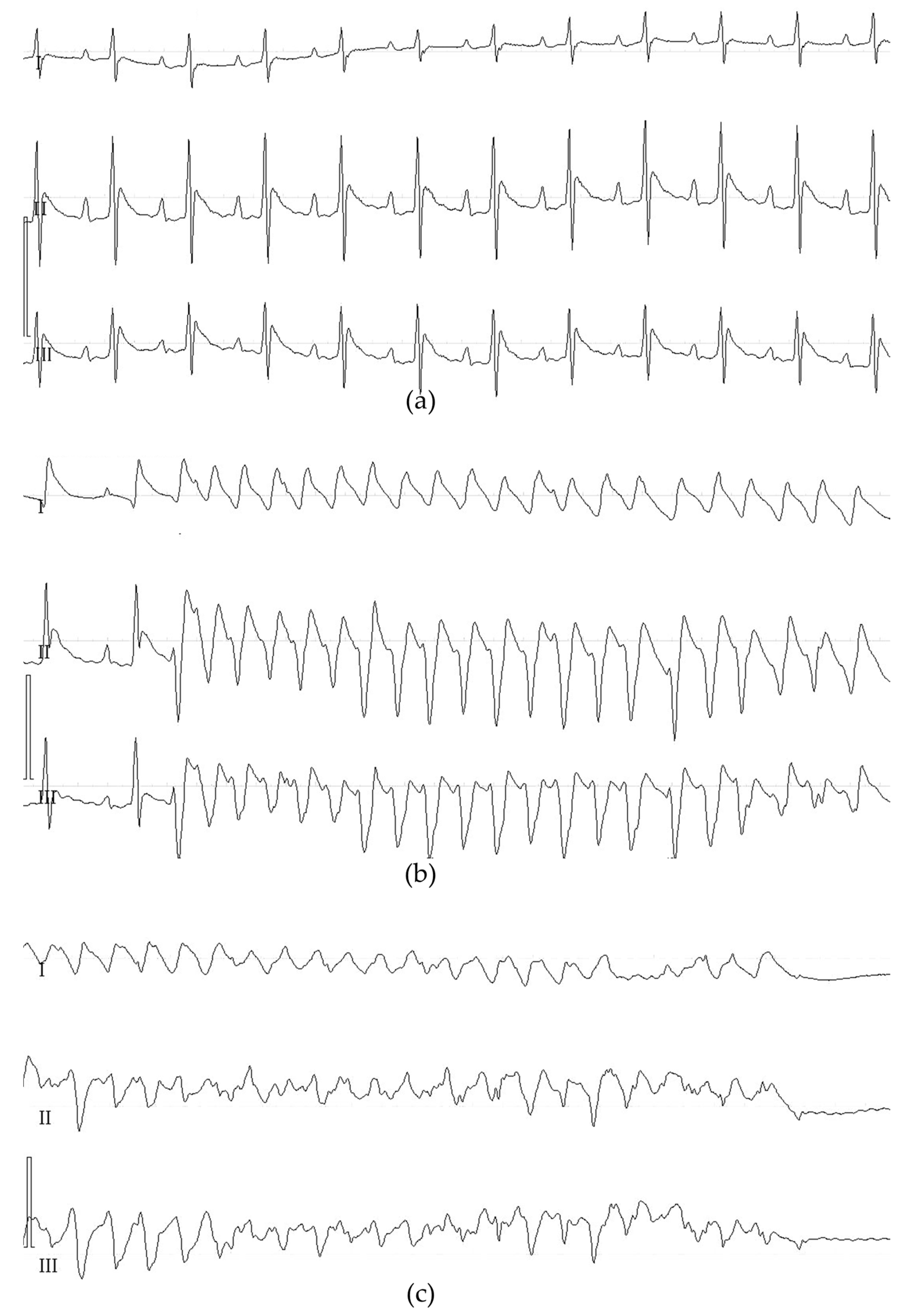
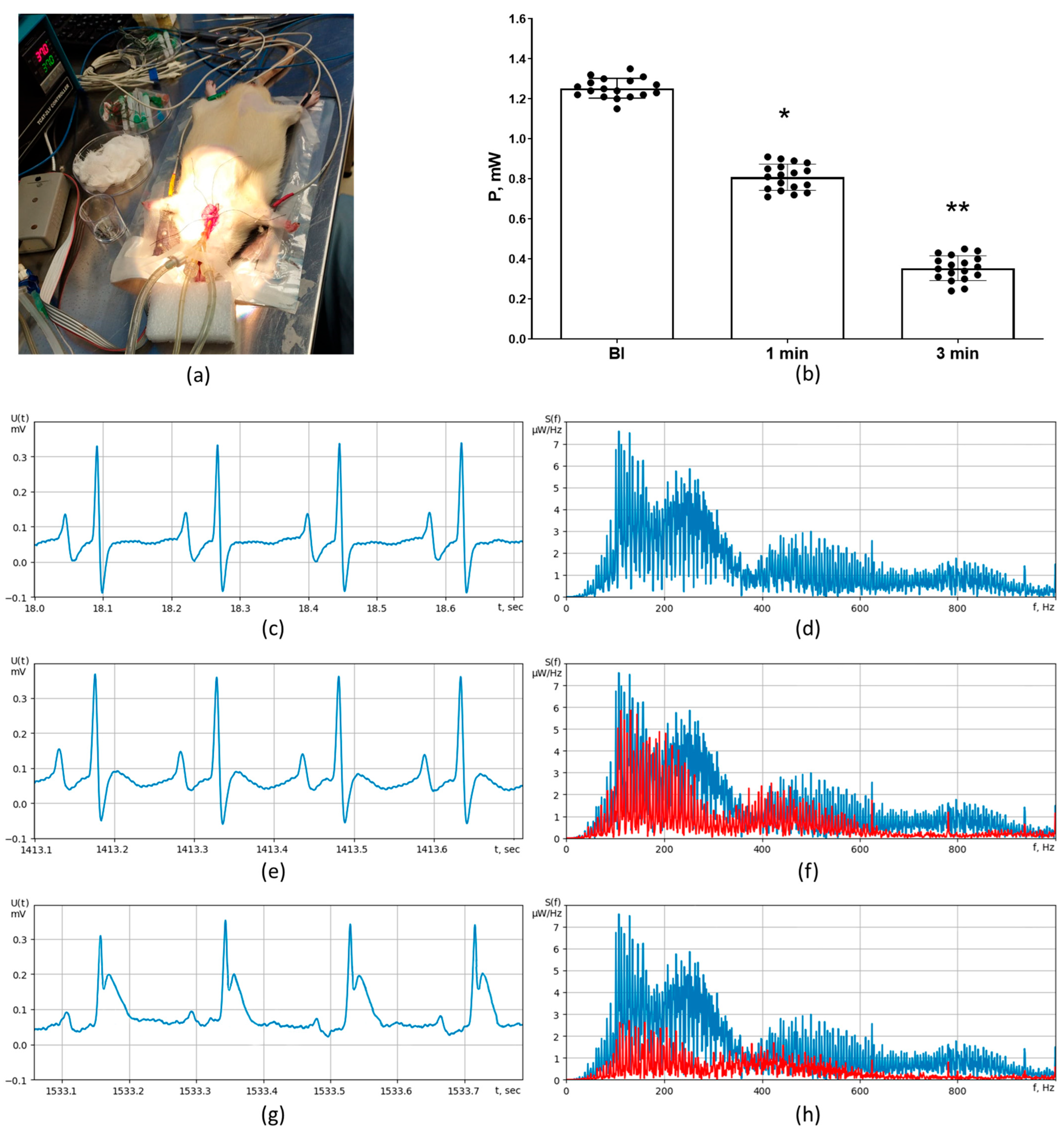
3.3. ECG Detection of Transmural Ischemia in Rats
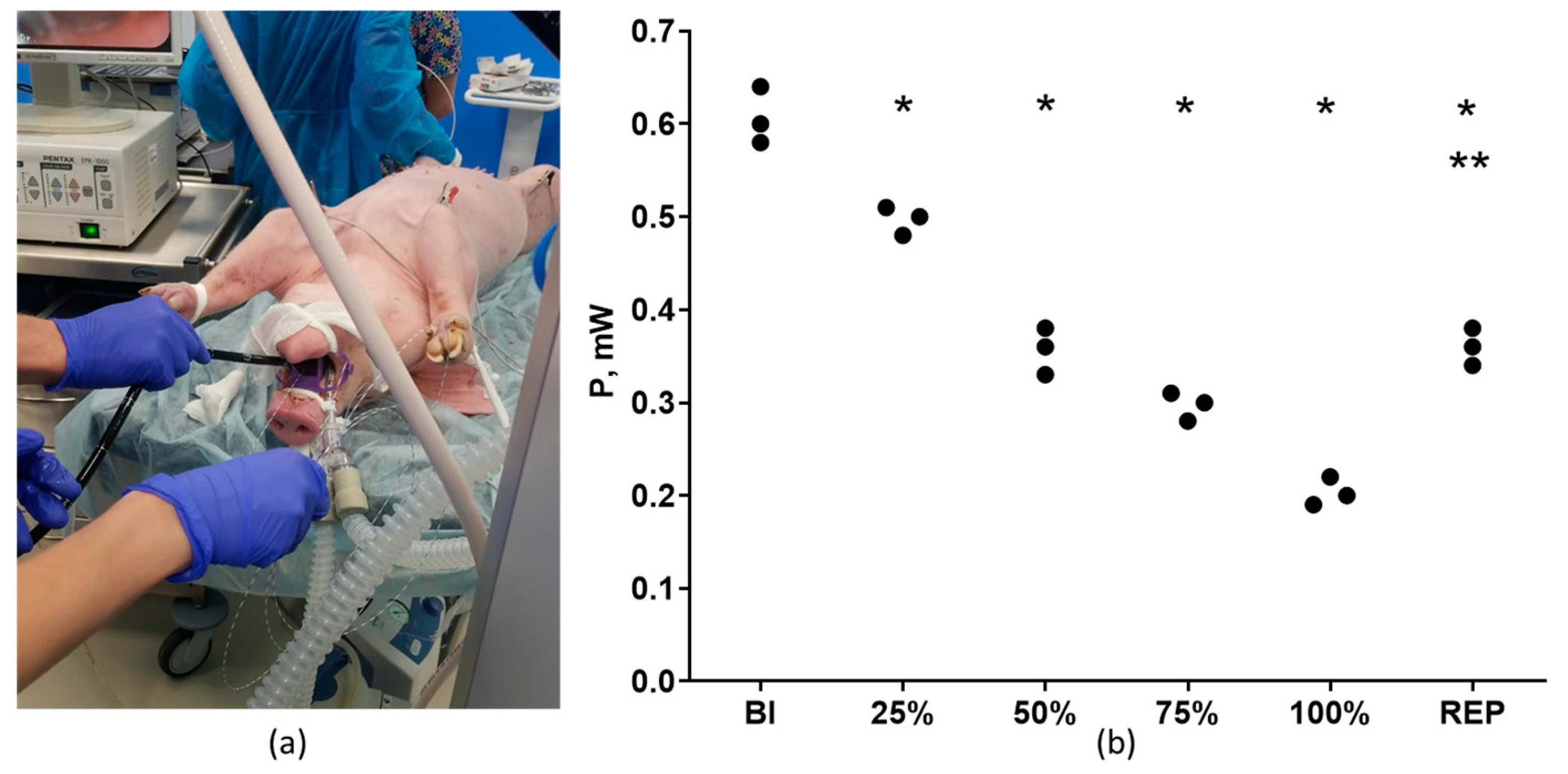
3.4. ECG Detection of Subendocardial and Transmural Ischemia in Pigs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Dai, H.; Much, A.A.; Maor, E.; Asher, E.; Younis, A.; Xu, Y.; Lu, Y.; Liu, X.; Shu, J.; Bragazzi, N.L. Global, regional, and national burden of ischaemic heart disease and its attributable risk factors, 1990-2017: Results from the Global Burden of Disease Study 2017. Eur. Heart J. Qual. Care Clin. Outcomes 2022, 8, 50–60. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart disease and stroke statistics-2023 update: A report from the American Heart Association. Circulation 2023, 147, e93–e621. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; Fernandez-Ortiz, A.; Fernandez-Friera, L.; Garcia-Lunar, I.; Andres, V.; Fuster, V. Progression of early subclinical atherosclerosis (PESA) study: JACC focus seminar 7/8. J. Am. Coll. Cardiol. 2021, 78, 156–179. [Google Scholar] [CrossRef]
- Gianrossi, R.; Detrano, R.; Mulvihill, D.; Lehmann, K.; Dubach, P.; Colombo, A.; McArthur, D.; Froelicher, V. Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis. Circulation 1989, 80, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.J.; Pahlm, O.; Warren, J.W.; Sapp, J.L.; Horacek, B.M. Criteria for ECG detection of acute myocardial ischemia: Sensitivity versus specificity. J. Electrocardiol. 2018, 51, S12–S17. [Google Scholar] [CrossRef] [PubMed]
- Maniar, Y.; Blumenthal, R.S.; Alfaddagh, A. The role of coronary artery calcium in allocating pharmacotherapy for primary prevention of cardiovascular disease: The ABCs of CAC. Clin. Cardiol. 2022, 45, 1107–1113. [Google Scholar] [CrossRef]
- Zampella, E.; Assante, R.; Acampa, W.; Gaudieri, V.; Nappi, C.; Mannarino, T.; D’Antonio, A.; Buongiorno, P.; Panico, M.; Mainolfi, C.G.; et al. Incremental value of 18F-FDG cardiac PET imaging over dobutamine stress echocardiography in predicting myocardial ischemia in patients with suspected coronary artery disease. J. Nucl. Cardiol. 2022, 29, 3028–3038. [Google Scholar] [CrossRef]
- Yu, J.; Qian, L.; Sun, W.; Nie, Z.; Zheng, D.; Han, P.; Shi, H.; Zheng, C.; Yang, F. Automated total and vessel-specific coronary artery calcium (CAC) quantification on chest CT: Direct comparison with CAC scoring on non-contrast cardiac CT. BMC Med. Imaging 2022, 22, 177. [Google Scholar] [CrossRef]
- Mroczka, T.; Lewandowski, P.; Maniewski, R.; Liebert, A.; Spioch, M.; Steinbach, K. Effectiveness of high resolution ECG spectral analysis in discrimination of patients prone to ventricular tachycardia and fibrillation. Med. Sci. Monit. 2000, 6, 1018–1026. [Google Scholar]
- Suszko, A.M.; Chakraborty, P.; Viswanathan, K.; Barichello, S.; Sapp, J.; Talajic, M.; Laksman, Z.; Yee, R.; Woo, A.; Spears, D.; et al. Automated quantification of abnormal QRS peaks from high-resolution ECGs predicts late ventricular arrhythmias in hypertrophic cardiomyopathy: A 5-year prospective multicenter study. J. Am. Heart Assoc. 2022, 11, e026025. [Google Scholar] [CrossRef]
- Pettersson, J.; Pahlm, O.; Carro, E.; Edenbrandt, L.; Ringborn, M.; Sornmo, L.; Warren, S.G.; Wagner, G.S. Changes in high-frequency QRS components are more sensitive than ST-segment deviation for detecting acute coronary artery occlusion. J. Am. Coll. Cardiol. 2000, 36, 1827–1834. [Google Scholar] [CrossRef]
- Zaitchenko, K.V. Method of analog two-channel ECG signal processing with ultrahigh resolution from one standard lead. In Proceedings of the 5th Russian-Bavarian Conference on Biomedical Engineering, Munich, Germany, 1–4 July 2009. [Google Scholar]
- Zaichenko, K.V.; Kulin, A.N.; Zharinov, O.O. Estimation of micropotentials of electrocardiograms of diagnostics of heart diseases. In Proceedings of the EMBEC’99, Vienna, Austria, 4–7 November 2009. [Google Scholar]
- Galagudza, M.M.; Sonin, D.L.; Vlasov, T.D.; Kurapeev, D.I.; Shlyakhto, E.V. Remote vs. local ischaemic preconditioning in the rat heart: Infarct limitation, suppression of ischaemic arrhythmia and the role of reactive oxygen species. Int. J. Exp. Pathol. 2016, 97, 66–74. [Google Scholar] [CrossRef]
- Galagudza, M.M.; Nekrasova, M.K.; Nifontov, E.M.; Syrenskii, A.V. Resistance of the myocardium to ischemia and the efficacy of ischemic preconditioning in experimental diabetes mellitus. Neurosci. Behav. Physiol. 2007, 37, 489–493. [Google Scholar] [CrossRef]
- Brenner, G.B.; Giricz, Z.; Garamvolgyi, R.; Makkos, A.; Onodi, Z.; Sayour, N.V.; Gergely, T.G.; Baranyai, T.; Petnehazy, O.; Korosi, D.; et al. Post-myocardial infarction heart failure in closed-chest coronary occlusion/reperfusion model in Göttingen minipigs and Landrace pigs. J. Vis. Exp. 2021, 170, e61901. [Google Scholar] [CrossRef]
- Gulyaev, U.V.; Zaichenko, K.V. High-resolution electrocardiography. Task. Problem. Prospects. Biomed. Radioelectron. 2013, 9, 5–16. [Google Scholar]
- Zaichenko, K.V.; Zhmyleva, A.A.; Khrapov, S.O.; Logachev, E.P.; Gurevich, B.S. Application of modern technologies in new ultra-high resolution electrocardiography method. In Proceedings of the 2020 Ural Symposium on Biomedical Engineering, Radioelectronics and Information Technology (USBEREIT), Yekaterinburg, Russia, 14–15 May 2020; pp. 4–7. [Google Scholar] [CrossRef]
- Zaichenko, K.V.; Kordyukova, A.A.; Logachev, E.P.; Luchkova, M.N. Application of radar techniques of signal processing for ultra-high resolution electrocardiography. Biomed. Eng. 2021, 55, 31–35. [Google Scholar] [CrossRef]
- Zaichenko, K.V.; Gurevich, B.S. Spectral processing of bioelectric signals. Biomed. Eng. 2021, 55, 17–20. [Google Scholar] [CrossRef]
- Zaichenko, K.; Gurevich, B.; Kordyukova, A.; Logachev, E. Wavelet analysis application for digital processing of ultra-high resolution electrocardiac signals. In Proceedings of the 2022 Ural-Siberian Conference on Biomedical Engineering, Radioelectronics and Information Technology (USBEREIT), Yekaterinburg, Russia, 19–21 September 2022; pp. 20–23. [Google Scholar] [CrossRef]
- Libby, P.; Theroux, P. Pathophysiology of coronary artery disease. Circulation 2005, 111, 3481–3488. [Google Scholar] [CrossRef] [PubMed]
- Okada, J.I.; Fujiu, K.; Yoneda, K.; Iwamura, T.; Washio, T.; Komuro, I.; Hisada, T.; Sugiura, S. Ionic mechanisms of ST segment elevation in electrocardiogram during acute myocardial infarction. J. Physiol. Sci. 2020, 70, 36. [Google Scholar] [CrossRef] [PubMed]
- Klabunde, R.E. Cardiac electrophysiology: Normal and ischemic ionic currents and the ECG. Adv. Physiol. Educ. 2017, 41, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth universal definition of myocardial infarction (2018). Circulation 2018, 138, e618–e651. [Google Scholar] [CrossRef]
- Gould, K.L.; Nguyen, T.; Kirkeeide, R.; Roby, A.E.; Bui, L.; Kitkungvan, D.; Patel, M.B.; Madjid, M.; Haynie, M.; Lai, D.; et al. Subendocardial and transmural myocardial ischemia: Clinical characteristics, prevalence, and outcomes with and without revascularization. JACC Cardiovasc. Imaging 2023, 16, 78–94. [Google Scholar] [CrossRef]
- Li, D.; Li, C.Y.; Yong, A.C.; Kilpatrick, D. Source of electrocardiographic ST changes in subendocardial ischemia. Circ. Res. 1998, 82, 957–970. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Shao, D.B.; Zhang, F.X.; Zhang, J.; Yuan, W.; Man, Y.L.; Du, W.; Liu, B.X.; Wang, D.W.; Li, X.R.; et al. Establishment and evaluation of a swine model of acute myocardial infarction and reperfusion-ventricular fibrillation-cardiac arrest using the interventional technique. J. Chin. Med. Assoc. 2013, 76, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Josephson, R.A.; Shefrin, E.; Lakatta, E.G.; Brant, L.J.; Fleg, J.L. Can serial exercise testing improve the prediction of coronary events in asymptomatic individuals? Circulation 1990, 81, 20–24. [Google Scholar] [CrossRef]
- Rywik, T.M.; O’Connor, F.C.; Gittings, N.S.; Wright, J.G.; Khan, A.A.; Fleg, J.L. Role of nondiagnostic exercise-induced ST-segment abnormalities in predicting future coronary events in asymptomatic volunteers. Circulation 2002, 106, 2787–2792. [Google Scholar] [CrossRef]
- Istolahti, T.; Nieminen, T.; Huhtala, H.; Lyytikainen, L.P.; Kahonen, M.; Lehtimaki, T.; Eskola, M.; Anttila, I.; Jula, A.; Rissanen, H.; et al. Long-term prognostic significance of the ST level and ST slope in the 12-lead ECG in the general population. J. Electrocardiol. 2020, 58, 176–183. [Google Scholar] [CrossRef]


| VTA Characteristics | Value (n = 24) |
|---|---|
| Number of animals with VTA | 22 (92%) |
| Number of VTA episodes per 1 animal | 2.6 ± 0.8 |
| Time to onset of the first episode of VTA, s | 243 ± 45 |
| Total duration of VTA, s | 48 ± 22 |
| Number of animals with persistent VF | 4 (17%) |
| Physiological Parameters | Prior to Thoracotomy | 5 min Prior to Ischemia | 5 min Ischemia | 10 min Ischemia |
|---|---|---|---|---|
| MAP, mm Hg | 116 ± 12 | 118 ± 14 | 110 ± 9 | 112 ± 16 |
| HR, beats/min | 422 ± 25 | 406 ± 29 | 412 ± 32 | 401 ± 18 |
| Body temperature, °C | 37.2 ± 0.4 | 36.9 ± 0.6 | 37.0 ± 0.5 | 37.5 ± 0.7 |
| Stage of the Experiment | Maximal ST Segment Deviation from the Isoelectric Line, mm | Signal Power P in the HF Channel of UHR ECG, mW |
|---|---|---|
| Baseline | 0 | 0.61 ± 0.05 |
| Reduction 25% | 0.0 ± 0.05 | 0.52 ± 0.05 * |
| Reduction 50% | 2.2 ± 0.21 * | 0.36 ± 0.04 * |
| Reduction 75% | 2.8 ± 0.34 * | 0.31 ± 0.03 * |
| Reduction 100% | 3.7 ± 0.42 * | 0.20 ± 0.02 * |
| Complete reperfusion | 1.9 ± 0.15 *,** | 0.37 ± 0.04 *,** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaichenko, K.V.; Kordyukova, A.A.; Sonin, D.L.; Galagudza, M.M. Ultra-High-Resolution Electrocardiography Enables Earlier Detection of Transmural and Subendocardial Myocardial Ischemia Compared to Conventional Electrocardiography. Diagnostics 2023, 13, 2795. https://doi.org/10.3390/diagnostics13172795
Zaichenko KV, Kordyukova AA, Sonin DL, Galagudza MM. Ultra-High-Resolution Electrocardiography Enables Earlier Detection of Transmural and Subendocardial Myocardial Ischemia Compared to Conventional Electrocardiography. Diagnostics. 2023; 13(17):2795. https://doi.org/10.3390/diagnostics13172795
Chicago/Turabian StyleZaichenko, Kirill V., Anna A. Kordyukova, Dmitry L. Sonin, and Michael M. Galagudza. 2023. "Ultra-High-Resolution Electrocardiography Enables Earlier Detection of Transmural and Subendocardial Myocardial Ischemia Compared to Conventional Electrocardiography" Diagnostics 13, no. 17: 2795. https://doi.org/10.3390/diagnostics13172795
APA StyleZaichenko, K. V., Kordyukova, A. A., Sonin, D. L., & Galagudza, M. M. (2023). Ultra-High-Resolution Electrocardiography Enables Earlier Detection of Transmural and Subendocardial Myocardial Ischemia Compared to Conventional Electrocardiography. Diagnostics, 13(17), 2795. https://doi.org/10.3390/diagnostics13172795






