Method Comparison and Clinical Performance of Breast Cancer Tumor Markers on Novel Multiplex Immunoassay and Automatized LOCI Technology Platforms
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Materials and Methods
2.3. Statistics
3. Results
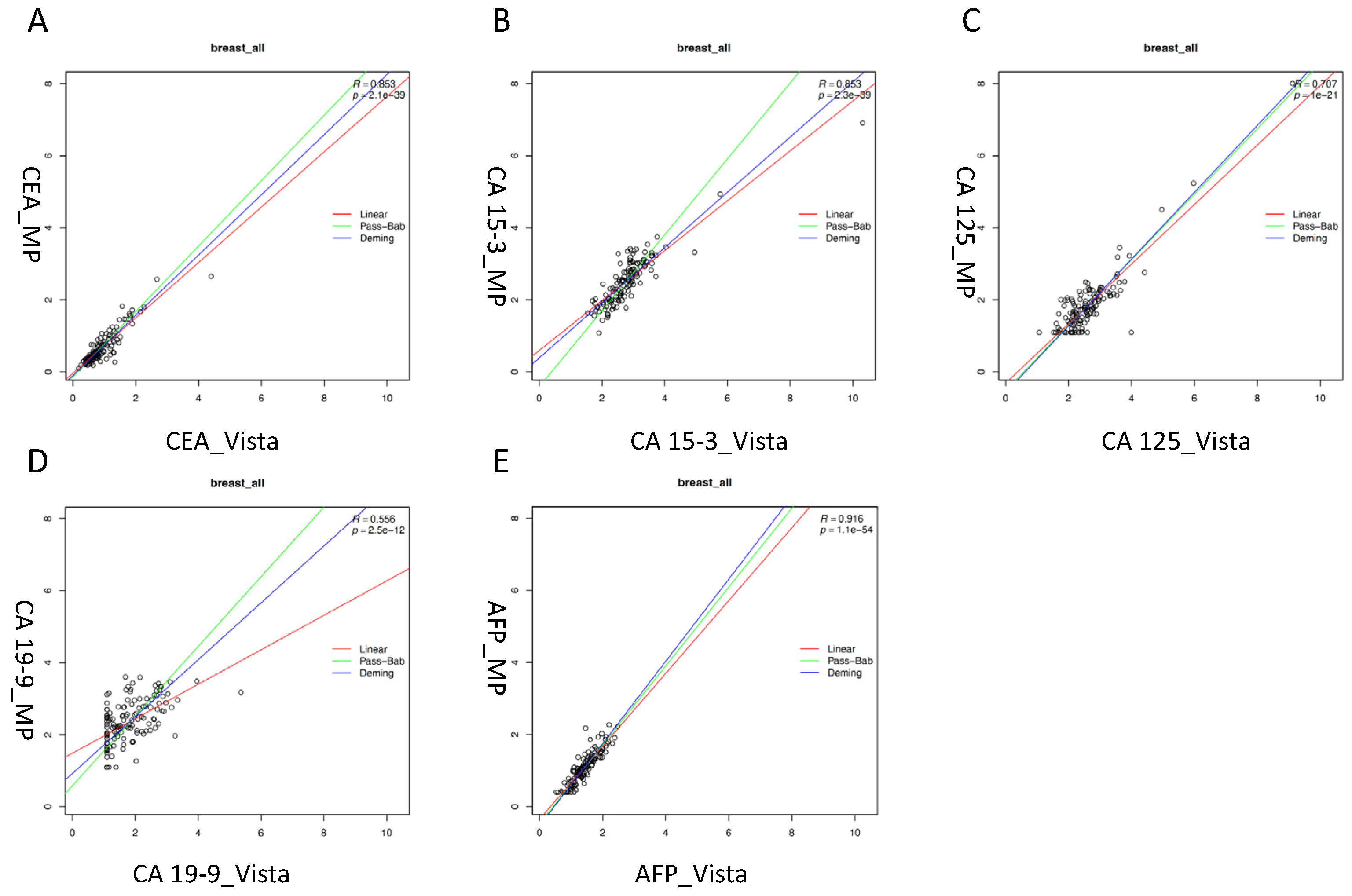
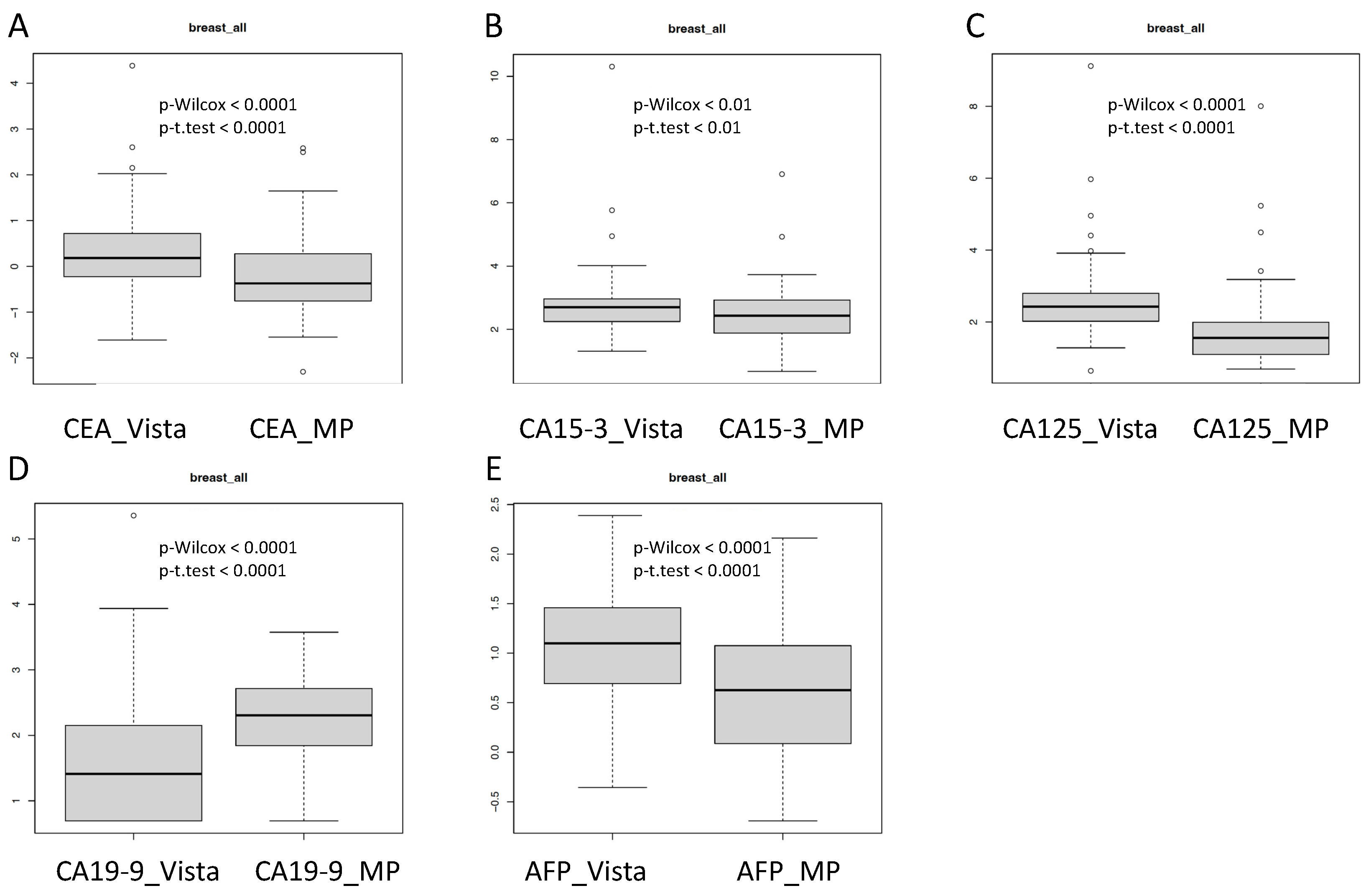
3.1. Analytical Comparison of the Multiplex and LOCI Methods
3.2. Comparison of Diagnostic Performance of the Multiplex and LOCI Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Duffy, M.J. Tumor markers in clinical practice: A review focusing on common solid cancers. Med. Princ. Pract. 2013, 22, 4–11. [Google Scholar] [CrossRef]
- Stieber, P.; Heinemann, V. Sinnvoller Einsatz von Tumormarkern/Sensible use of tumor markers. J. Lab. Med. 2008, 32, 339–360. [Google Scholar] [CrossRef]
- Holdenrieder, S.; Pagliaro, L.; Morgenstern, D.; Dayyani, F. Clinically meaningful use of blood Tumor markers in oncology. BioMed Res. Int. 2016, 2016, 9795269. [Google Scholar] [CrossRef] [PubMed]
- Hammarström, S. The carcinoembryonic antigen (CEA) family: Structures, suggested functions and expression in normal and malignant tissues. Semin. Cancer Biol. 1999, 9, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Waks, A.G.; Winer, E.P. Breast Cancer Treatment: A Review. JAMA 2019, 321, 288–300. [Google Scholar] [CrossRef] [PubMed]
- Di Gioia, D.; Dresse, M.; Mayr, D.; Nagel, D.; Heinemann, V.; Stieber, P. Serum HER2 in combination with CA 15-3 as a parameter for prognosis in patients with early breast cancer. Clin. Chim. Acta 2015, 440, 16–22. [Google Scholar] [CrossRef]
- Petersen, E.R.B.; Sørensen, P.D.; Jakobsen, E.H.; Madsen, J.S.; Brandslund, I. Serum HER-2 predicts response and resistance to trastuzumab treatment in breast cancer. Clin. Chem. Lab. Med. 2013, 51, 1483–1492. [Google Scholar] [CrossRef]
- Ryu, J.M.; Kang, D.; Cho, J.; Lee, J.E.; Kim, S.W.; Nam, S.J.; Lee, S.K.; Kim, Y.J.; Im, Y.-H.; Ahn, J.S.; et al. Prognostic Impact of Elevation of Cancer Antigen 15-3 (CA15-3) in Patients With Early Breast Cancer With Normal Serum CA15-3 Level. J. Breast Cancer 2023, 26, 126–135. [Google Scholar] [CrossRef]
- Stieber, P.; Nagel, D.; Blankenburg, I.; Heinemann, V.; Untch, M.; Bauerfeind, I.; Di Gioia, D. Diagnostic efficacy of CA 15-3 and CEA in the early detection of metastatic breast cancer—A retrospective analysis of kinetics on 743 breast cancer patients. Clin. Chim. Acta 2015, 448, 228–231. [Google Scholar] [CrossRef]
- Menon, U.; Ryan, A.; Kalsi, J.; Gentry-Maharaj, A.; Dawnay, A.; Habib, M.; Apostolidou, S.; Singh, N.; Benjamin, E.; Burnell, M.; et al. Risk Algorithm Using Serial Biomarker Measurements Doubles the Number of Screen-Detected Cancers Compared With a Single-Threshold Rule in the United Kingdom Collaborative Trial of Ovarian Cancer Screening. J. Clin. Oncol. 2015, 33, 2062–2071. [Google Scholar] [CrossRef]
- Sturgeon, C.M.; Duffy, M.J.; Hofmann, B.R.; Lamerz, R.; Fritsche, H.A.; Gaarenstroom, K.; Bonfrer, J.; Ecke, T.H.; Grossman, H.B.; Hayes, P.; et al. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines for use of tumor markers in liver, bladder, cervical, and gastric cancers. Clin. Chem. 2010, 56, e1–e48. [Google Scholar] [CrossRef] [PubMed]
- Núñez, C. Blood-based protein biomarkers in breast cancer. Clin. Chim. Acta 2019, 490, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.; Park, M.J.; Song, W.; Kim, H.S. Current immunoassay methods and their applications to clinically used biomarkers of breast cancer. Clin. Biochem. 2020, 78, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Sturgeon, C.M.; Duffy, M.J.; Stenman, U.; Lilja, H.; Brunner, N.; Chan, D.W.; Babaian, R.; Bast, R.C., Jr.; Dowell, B.; Esteva, F.J.; et al. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines for Use of Tumor Markers in Testicular, Prostate, Colorectal, Breast, and Ovarian Cancers. Clin. Chem. 2008, 54, e11–e79. [Google Scholar] [CrossRef]
- Sturgeon, C.M.; Hoffman, B.R.; Chan, D.W.; Ch’ng, S.L.; Hammond, E.; Hayes, D.F.; Liotta, L.A.; Petricoin, E.F.; Schmitt, M.; Semmes, O.J.; et al. National Academy of Clinical Biochem-istry Laboratory Medicine Practice Guidelines for Use of Tumor Markers in Clinical Practice: Quality Requirements. Clin. Chem. 2008, 54, e1–e10. [Google Scholar] [CrossRef]
- Fu, Q.; Zhu, J.; Van Eyk, J.E. Comparison of multiplex immunoassay platforms. Clin. Chem. 2010, 56, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Krishhan, V.V.; Khan, I.H.; Luciw, P.A. Multiplexed microbead immunoassays by flow cytometry for molecular profiling: Basic concepts and proteomics applications. Crit. Rev. Biotechnol. 2009, 29, 29–43. [Google Scholar] [CrossRef]
- Cohen, J.D.; Javed, A.A.; Thoburn, C.; Wong, F.; Tie, J.; Gibbs, P.; Schmidt, C.M.; Yip-Schneider, M.T.; Allen, P.J.; Schattner, M.; et al. Combined circulating tumor DNA and protein biomarker-based liquid biopsy for the earlier detection of pancreatic cancers. Proc. Natl. Acad. Sci. USA 2017, 114, 10202–10207. [Google Scholar] [CrossRef]
- Cohen, J.D.; Wang, Y.; Thoburn, C.; Afsari, B.; Danilova, L.; Douville, C.; Javed, A.A.; Wong, F.; Mattox, A.; Hruban, R.H.; et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 2018, 359, 926–930. [Google Scholar] [CrossRef]
- Sturgeon, C. Standardization of tumor markers—Priorities identified through external quality assessment. Scand. J. Clin. Lab. Investig. 2016, 245, S94–S99. [Google Scholar] [CrossRef]
- Rawlins, M.L.; Roberts, W.L. Performance characteristics of six third-generation assays for thyroid-stimulating hormone. Clin. Chem. 2004, 50, 2338–2344. [Google Scholar] [CrossRef] [PubMed]
- Weykamp, C.; Franck, P.; Gunnewiek, J.K.; de Jonge, R.; Kuypers, A.; van Loon, D.; Steigstra, H.; Cobbaert, C. Harmonisation of seven common enzyme results through EQA. Clin. Chem. Lab. Med. 2014, 52, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- Zur, B.; Holdenrieder, S.; Albers, E.; Walgenbach-Brünagel, G.; Stoffel-Wagner, B. Method comparison between Dimension Vista 1500 and Immulite 2000 XPI for determination of new LOCI tumor markers CA 15-3, CA 19-9 and CA 125. J. Immunoass. Immunochem. 2012, 33, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Holdenrieder, S.; Molina, R.; Gion, M.; Gressner, A.; Troalen, F.; Auge, J.M.; Zancan, M.; Wycislo, M.; Stieber, P. Alternative antibodies for the detection of CA125 antigen: An European Multicenter Study for the evaluation of the analytical and clinical performance of the Access® OV Monitor Assay on Beckman Coulter’s UniCel® DxI 800 immunoassay system. Clin. Chem. Lab. Med. 2008, 46, 588–599. [Google Scholar] [CrossRef]
- Hermann, N.; Dressen, K.; Schroeder, L.; Debald, M.; Schildberg, F.A.; Walgenbach-Bruenagel, G.; Hettwer, K.; Uhlig, S.; Kuhn, W.; Hartmann, G.; et al. Diagnostic relevance of a novel multiplex immunoassay biomarker panel in patients with breast cancer. Tumor Biol. 2017, 39, 1010428317711381. [Google Scholar] [CrossRef]
- Hermann, N.; Dreßen, K.; Schildberg, F.A.; Jakobs, C.; Holdenrieder, S. Methodical and pre-analytical characteristics of a multiplex cancer biomarker immunoassay. World J. Methodol. 2014, 4, 219–231. [Google Scholar] [CrossRef]
- Bundesaerztekammer. Richtlinie der Bundesärztekammer zur Qualitätssicherung laboratoriumsmedizinischer Untersuchungen–Rili-BÄK. Dtsch. Aerzteblatt 2019. Available online: https://www.aerzteblatt.de/down.asp?id=27352 (accessed on 29 July 2023). [CrossRef]
- Reinauer, H.; Wood, W.G. External quality assessment of tumour marker analysis: State of the art and consequences for estimating diagnostic sensitivity and specificity. Ger. Med. Sci. GMS e-J. 2005, 3, 30. [Google Scholar]
- Marlet, J.; Bernard, M. Comparison of LUMIPULSE® G1200 with Kryptor and Modular E170 for the Measurement of Seven Tumor Markers. J. Clin. Lab. Anal. 2016, 30, 5–12. [Google Scholar] [CrossRef]
- de Rancher, M.-A.R.; Oudart, J.-B.; Maquart, F.-X.; Monboisse, J.C.; Ramont, L. Evaluation of Lumipulse® G1200 for the measurement of six tumor markers: Comparison with AIA® 2000. Clin. Biochem. 2016, 49, 1302–1306. [Google Scholar] [CrossRef]
- Falzarano, R.; Viggiani, V.; Michienzi, S.; Longo, F.; Tudini, S.; Frati, L.; Anastasi, E. Evaluation of a CLEIA automated assay system for the detection of a panel of tumor markers. Tumor Biol. 2013, 34, 3093–3100. [Google Scholar] [CrossRef] [PubMed]
- Fatica, E.M.; Larson, B.J.; Algeciras-Schimnich, A.; Bornhorst, J.A. Performance characteristics of the BRAHMS KRYPTOR automated squamous cell carcinoma antigen assay. J. Immunol. Methods 2022, 504, 113257. [Google Scholar] [CrossRef] [PubMed]
- Chauvel, C.; Jordan, P.; Popovici, T.; Bories, P.-N. Evaluation of the new Elecsys SCC assay: Comparison with the Kryptor SCC assay. Clin. Chem. Lab. Med. 2018, 56, e56–e58. [Google Scholar] [CrossRef]
- Cheng, Y.; He, J.; Zhang, L.; Chen, X.; Ou, S. Evaluation of chemiluminescent immunoassay quantitative detection for pro-gastrin-releasing peptide (ProGRP) in serum and plasma. J. Int. Med. Res. 2020, 48, 300060519882802. [Google Scholar] [CrossRef] [PubMed]
- WHO. International Biological Reference Preparations 2018. Available online: https://cdn.who.int/media/docs/default-source/biologicals/blood-products/catalogue/alphabetical-list.pdf?sfvrsn=15455482_2 (accessed on 27 July 2023).
- Park, J.; Lee, S.; Kim, Y.; Choi, A.; Lee, H.; Lim, J.; Kim, Y.; Han, K.; Oh, E.-J. Comparison of Four Automated Carcinoembryonic Antigen Immunoassays: ADVIA Centaur XP, ARCHITECT I2000sr, Elecsys E170, and Unicel Dxi800. Ann. Lab. Med. 2018, 38, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Wojtalewicz, N.; Vierbaum, L.; Kaufmann, A.; Schellenberg, I.; Holdenrieder, S. Longitudinal Evaluation of AFP and CEA External Proficiency Testing Reveals Need for Method Harmonization. Diagnostics 2023, 13, 2019. [Google Scholar] [CrossRef]
- van Rossum, H.H.; Meng, Q.H.; Ramanathan, L.V.; Holdenrieder, S. A word of caution on using tumor biomarker reference change values to guide medical decisions and the need for alternatives. Clin. Chem. Lab. Med. 2021, 60, 553–555. [Google Scholar] [CrossRef]
- Coşkun, A.; Aarsand, A.K.; Sandberg, S.; Guerra, E.; Locatelli, M.; Díaz-Garzón, J.; Fernandez-Calle, P.; Ceriotti, F.; Jonker, N.; Bartlett, W.A.; et al. Within- and between-subject biological variation data for tumor markers based on the European Biological Variation Study. Clin. Chem. Lab. Med. 2021, 60, 543–552. [Google Scholar] [CrossRef]
- Fraser, C.G. Reference change values: The way forward in monitoring. Ann. Clin. Biochem. 2009, 46 Pt 3, 264–265. [Google Scholar] [CrossRef]
- Christenson, R.H.; Cervelli, D.R.; Sterner, J.; Bachmann, L.M.; Rebuck, H.; Gray, J.; Kelley, W.E. Analytical performance and clinical concordance of the cancer biomarkers CA 15-3, CA 19-9, CA 125 II, Carcinoembryonic Antigen, and Alpha-Fetoprotein on the Dimension Vista® System. Clin. Biochem. 2011, 44, 1128–1136. [Google Scholar] [CrossRef]
- Stieber, P.; Molina, R.; Gion, M.; Gressner, A.; Troalen, F.; Holdenrieder, S.; Auge, J.M.; Zancan, M.; Wycislo, M.; Jarrige, V. Alternative antibody for the detection of CA19-9 antigen: A European Multicenter Study for the evaluation of the analytical and clinical performance of the Access® GI Monitor Assay on the UniCel® DxI 800 Immunoassay System from Beckman Coulter. Clin. Chem. Lab. Med. 2008, 46, 600–611. [Google Scholar] [CrossRef] [PubMed]
- Molina, R.; Gion, M.; Gressner, A.; Troalen, F.; Auge, J.M.; Holdenrieder, S.; Zancan, M.; Wycislo, M.; Stieber, P. Alternative antibodies for the detection of CA15-3 antigen: An European Multicenter Study for the evaluation of the analytical and clinical performance of the Access® BR Monitor Assay on Beckman Coulter’s UniCel® DxI 800 immunoassay system. Clin. Chem. Lab. Med. 2008, 46, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.; Lijmer, J.G.; Moher, D.; Rennie, D.; de Vet, H.C.W.; et al. STARD 2015: An Updated List of Essential Items for Reporting Diagnos-tic Accuracy Studies. Clin Chem. 2015, 61, 1446–1452. [Google Scholar] [CrossRef] [PubMed]


| Number | % of Cancers | Age Median | Age Range | ||
|---|---|---|---|---|---|
| Breast Cancer | All | 77 | 100 | 58.7 | 31.3–85.8 |
| Stage 1 | 31 | 40.3 | 58.7 | 36.4–85.4 | |
| Stage 2 | 25 | 32.5 | 62.3 | 41.3–85.8 | |
| Stage 3 | 12 | 15.6 | 49.5 | 32.6–74.9 | |
| Stage 4 | 9 | 11.7 | 66.9 | 31.3–76.4 | |
| DCIS | Precancerous | 10 | 53.5 | 39.5–71.0 | |
| Benign breast disease | 31 | 53.8 | 26.6–85.4 | ||
| Healthy controls | 36 | 42.9 | 20.1–78.1 |
| Breast Cancer vs. Healthy | Breast Cancer vs. Benign Disease | |||
|---|---|---|---|---|
| Vista AUC (95% CI) | MP AUC (95% CI) | Vista AUC (95% CI) | MP AUC (95% CI) | |
| CEA | 0.81 (0.72–0.91) | 0.81 (0.72–0.91) | 0.64 (0.53–0.74) | 0.62 (0.51–0.73) |
| CA 15–3 | 0.67 (0.54–0.79) | 0.75 (0.65–0.86) | 0.66 (0.54–0.77) | 0.70 (0.60–0.81) |
| CA 125 | 0.63 (0.51–0.74) | 0.74 (0.62–0.86) | 0.54 (0.41–0.67) | 0.55 (0.42–0.68) |
| CA 19–9 | 0.64 (0.51–0.77) | 0.75 (0.65–0.86) | 0.49 (0.36–0.61) | 0.64 (0.53–0.75) |
| AFP | 0.74 (0.60–0.87) | 0.79 (0.67–0.91) | 0.50 (0.37–0.63) | 0.51 (0.38–0.63) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schröder, L.; Mallmann, M.R.; Domroese, C.M.; Wefers, N.; Dolscheid-Pommerich, R.; Stoffel-Wagner, B.; Trulson, I.; Vahldiek, K.; Klawonn, F.; Holdenrieder, S. Method Comparison and Clinical Performance of Breast Cancer Tumor Markers on Novel Multiplex Immunoassay and Automatized LOCI Technology Platforms. Diagnostics 2023, 13, 3101. https://doi.org/10.3390/diagnostics13193101
Schröder L, Mallmann MR, Domroese CM, Wefers N, Dolscheid-Pommerich R, Stoffel-Wagner B, Trulson I, Vahldiek K, Klawonn F, Holdenrieder S. Method Comparison and Clinical Performance of Breast Cancer Tumor Markers on Novel Multiplex Immunoassay and Automatized LOCI Technology Platforms. Diagnostics. 2023; 13(19):3101. https://doi.org/10.3390/diagnostics13193101
Chicago/Turabian StyleSchröder, Lars, Michael R. Mallmann, Christian M. Domroese, Natalie Wefers, Ramona Dolscheid-Pommerich, Birgit Stoffel-Wagner, Inga Trulson, Kai Vahldiek, Frank Klawonn, and Stefan Holdenrieder. 2023. "Method Comparison and Clinical Performance of Breast Cancer Tumor Markers on Novel Multiplex Immunoassay and Automatized LOCI Technology Platforms" Diagnostics 13, no. 19: 3101. https://doi.org/10.3390/diagnostics13193101
APA StyleSchröder, L., Mallmann, M. R., Domroese, C. M., Wefers, N., Dolscheid-Pommerich, R., Stoffel-Wagner, B., Trulson, I., Vahldiek, K., Klawonn, F., & Holdenrieder, S. (2023). Method Comparison and Clinical Performance of Breast Cancer Tumor Markers on Novel Multiplex Immunoassay and Automatized LOCI Technology Platforms. Diagnostics, 13(19), 3101. https://doi.org/10.3390/diagnostics13193101












