Investigation and Causes of Spontaneous (Non-Diabetic) Hypoglycaemia in Adults: Pitfalls to Avoid
Abstract
1. Introduction
2. Pathophysiology of Hypoglycaemia
3. Verification of Hypoglycaemia
3.1. Biochemical Definition
3.2. Neuroglycopaenia
3.3. Whipple’s Triad
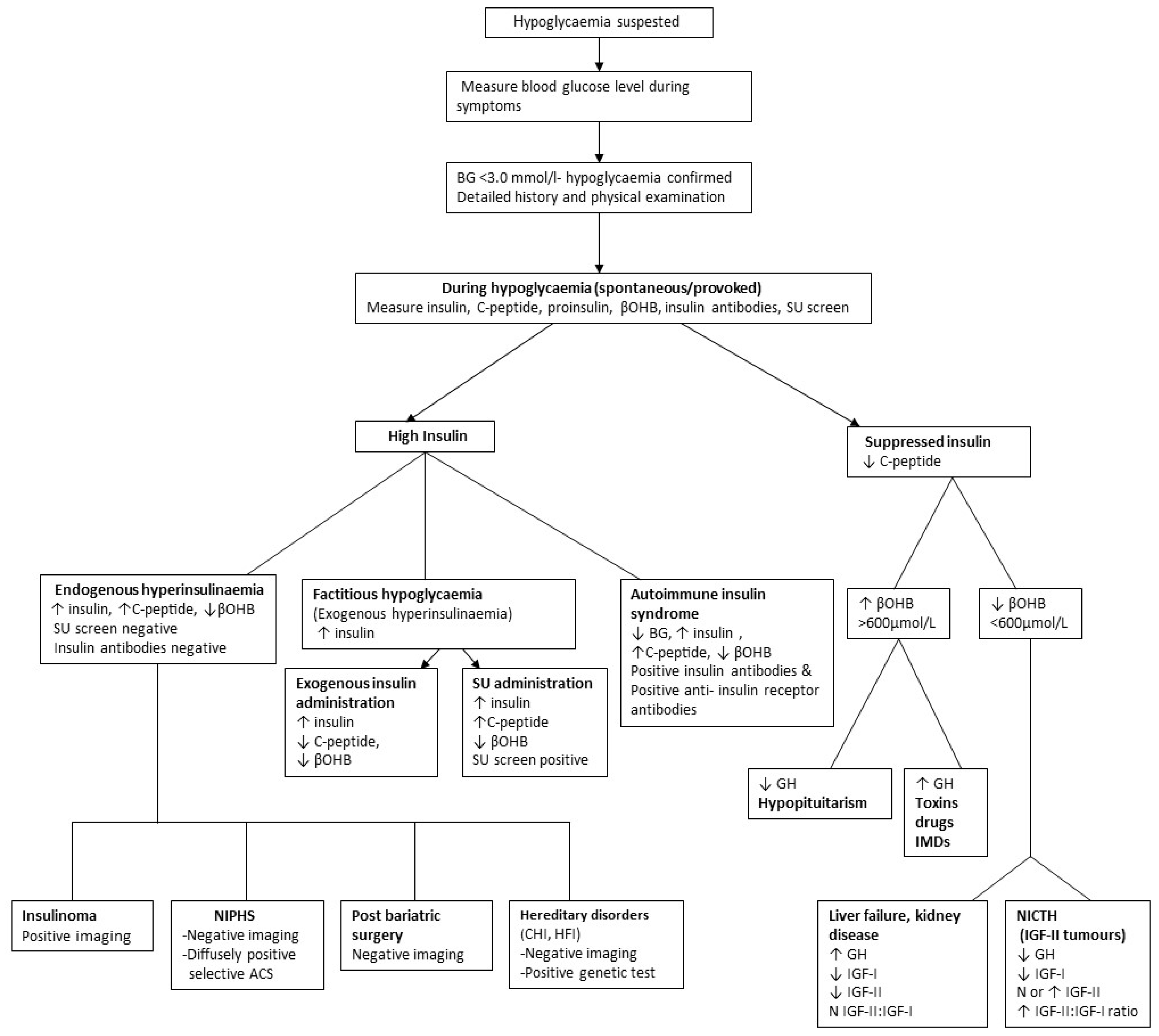
4. Investigation of Documented Hypoglycaemia
4.1. Patients Who Are Ill
4.2. Apparently Well Individuals
4.3. Tests for Provoking Hypoglycaemia
4.3.1. Overnight Fast
4.3.2. Prolonged Fast
4.3.3. Mixed Meal Test
| HYPERINSULINEMIC HYPOGLYCAEMIA | Endogenous hyperinsulinaemia: Insulinoma, upper gastrointestinal tract surgery including bariatric surgery. Non-insulinoma pancreatogenous hypoglycemia syndrome (NIPHS) Autoimmune insulin syndrome Factitious hypoglycaemia: Administration of insulin, sulfonylurea |
| HYPOINSULINEMIC HYPOGLYCAEMIA | Alcohol Drugs Critical illnesses: Hepatic, renal, or cardiac failure, sepsis, malaria Endocrinopathy: Hypoadrenalism, hypopituitarism Non-islet cell tumour hypoglycaemia (NITCH): Mesenchymal, epithelial and hematopoietic tumours Inherited metabolic disorders: Glycogen storage disorders, disorders of gluconeogenesis, mitochondrial diseases, fatty acid oxidation disorders, hereditary fructose intolerance |
| Drug Type | Drug |
|---|---|
| Antimicrobials | Fluoroquinolones—clinafloxacin Pentamidine Quinolones—gatifloxacin, ciprofloxacin, moxifloxacin, levofloxacin Sulfamethoxazole |
| Anti-malarials | Artesunate Quinine Quinidine |
| Antipsychotics | Lithium Valproate—in neonatal exposure |
| Analgesic | Salicylates—especially in children |
| Cardiac agents | Beta blockers Angiotensin-converting enzyme inhibitors Disopyramide Cibenzoline Indomethacin |
| Other | Ethanol Insulin Growth Factor 1 Mifepristone—in labour Somatostatin analogues |
5. Differential Diagnosis of Documented Hypoglycaemia
5.1. Postprandial (Alimentary) Hypoglycaemia
5.2. Fasting (Non-Prandial) Hypoglycaemia
5.2.1. Hyperinsulinaemic Hypoglycaemia
5.2.2. Hypoinsulinaemic Hypoglycaemia
6. Analytical Considerations: Insulin, C-Peptide, Proinsulin and Their Antibodies
7. Pitfalls to Avoid
- Failure to recognise sub-acute neuroglycopaenic symptoms as a clinical manifestation of spontaneous hypoglycaemia, leading to delayed or missed diagnosis.
- Failure to use appropriate cut-offs dependent on sample type (serum or whole blood) for defining biochemical hypoglycaemia, erroneously confirming or excluding hypoglycaemia.
- Failure to recognise spurious hypoglycaemia and pseudohypoglycaemia.
- Failure to confirm hypoglycaemia by not documenting Whipple’s triad.
- Failure to recognise the limitations of blood glucose meters and continuous glucose monitoring (CGM) in the identification of biochemical hypoglycaemia.
- Inappropriate use of obsolete investigations, such as the prolonged oral glucose tolerance test.
- Failure to follow protocols for the prolonged fast, particularly in terminating the fast prematurely before laboratory-confirmed hypoglycaemia and failure to test for (subtle) neuroglycopenia.
- Failure to recognise that a few healthy individuals may have plasma glucose concentrations in the range of 3.0 mmol/L or less following prolonged fasting.
- Failure to provide hypoglycaemic samples for measurement of pancreatic hormones, counter-regulatory hormones and non-glucose substrates.
- Measurement of pancreatic hormones, counter-regulatory hormones and non-glucose substrates in non-hypoglycaemic samples.
- Failure to recognise assay limitations, in particular very specific insulin immunoassays failing to detect pure proinsulinomas and exogenous insulin abuse.
- Failure to exclude factitious and accidental hypoglycaemia, AIS and NIPHS before diagnosing insulinoma.
- Failure to recognise that insulinoma may very rarely present with hypoinsulinaemia and ketosis (c-peptide and proinsulin always inappropriately raised).
- Failure to measure insulin antibodies in a hypoglycaemic sample with high insulin levels and mislabelling it as factitious hypoglycaemia.
- Failure to recognise that IA and IAA may be of no immunoassay and clinico-pathological significance or be of no clinico-pathological significance but interfere in laboratory immunoassays, giving rise to erroneous laboratory results and clinical confusion.
- Failure to exclude causes of fasting hypoglycaemia before diagnosing idiopathic postprandial (alimentary) hypoglycaemia.
- Failure to recognise that low serum cortisol during hypoglycaemia may erroneously indicate hypoadrenalism, hence the need for appropriate stimulation tests for confirmation of endocrinopathy.
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Gama, R.; Teale, J.D.; Marks, V. Best Practice No 173: Clinical and laboratory investigation of adult spontaneous hypoglycaemia. J. Clin. Pathol. 2003, 56, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.E.; Gerich, J.E. Glucose counter-regulation, hypoglycemia, and intensive insulin therapy in diabetes mellitus. N. Engl. J. Med. 1985, 313, 232–341. [Google Scholar]
- Mitrakou, A.; Ryan, C.; Veneman, T.; Mokan, M.; Jenssen, T.; Kiss, I.; Durrant, J.; Cryer, P.; Gerich, J. Hierarchy of glycemic thresholds for counterregulatory hormone secretion, symptoms, and cerebral dysfunction. Am. J. Physiol. Metab. 1991, 260 Pt 1, E67–E74. [Google Scholar] [CrossRef] [PubMed]
- Service, F.J. Hypoglycemic disorders. N. Engl. J. Med. 1995, 332, 1144–1152. [Google Scholar] [CrossRef]
- Heller, S.R.; Cryer, P.E. Hypoinsulinemia is not critical to glucose recovery from hypoglycemia in humans. Am. J. Physiol. 1991, 261 Pt 1, E41-8. [Google Scholar] [CrossRef] [PubMed]
- Kotwal, N.; Pandit, A. Variability of capillary blood glucose monitoring measured on home glucose monitoring devices. Indian J. Endocrinol. Metab. 2012, 16, S248–S251. [Google Scholar] [CrossRef] [PubMed]
- Arem, R.; Jeang, M.K.; Blevens, T.C.; Waddell, C.C.; Field, J.B. Polycythemia rubra vera and artifactual hypoglycemia. Arch. Intern. Med. 1982, 142, 2199–2201. [Google Scholar] [CrossRef]
- Grzych, G.; Roland, E.; Beauvais, D.; Maboudou, P.; Lippi, G. Leukocytosis interference in clinical chemistry: Shall we still interpret test results without hematological data? J. Med. Biochem. 2020, 39, 66–71. [Google Scholar] [CrossRef]
- El Khoury, M.; Yousuf, F.; Martin, V.; Cohen, R.M. Pseudohypoglycemia: A cause for unreliable finger-stick glucose measurements. Endocr. Pract. 2008, 14, 337–339. [Google Scholar] [CrossRef]
- Marks, V.; Teale, J.D. Investigation of hypoglycaemia. Clin. Endocrinol. 1996, 44, 133–136. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, R.; Gama, R.; Marks, V. Hypoglycemia. In Encyclopedia of Human Nutrition; Caballero, B., Ed.; Elsevier: Amsterdam, The Netherlands, 2023; pp. 401–411. [Google Scholar]
- Tesfaye, N.; Seaquist, E.R. Neuroendocrine responses to hypoglycemia. Ann. N. Y. Acad. Sci. 2010, 1212, 12–28. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.E. Hypoglycemia, functional brain failure, and brain death. J. Clin. Investig. 2007, 117, 868–870. [Google Scholar] [CrossRef] [PubMed]
- Whipple, A. The surgical therapy of hyperinsulinism. J. Int. Chir. 1938, 3, 237–276. [Google Scholar]
- Ilias, I.; Diamantopoulos, A.; Pratikaki, M.; Botoula, E.; Jahaj, E.; Athanasiou, N.; Tsipilis, S.; Zacharis, A.; Vassiliou, A.G.; Vassiliadi, D.A.; et al. Glycemia, Beta-Cell Function and Sensitivity to Insulin in Mildly to Critically Ill Covid-19 Patients. Medicina 2021, 57, 68. [Google Scholar] [CrossRef] [PubMed]
- Miguélez, M.; Velasco, C.; Camblor, M.; Cedeño, J.; Serrano, C.; Bretón, I.; Arhip, L.; Motilla, M.; Carrascal, M.; Olivares, P.; et al. Nutritional management and clinical outcome of critically ill patients with COVID-19: A retrospective study in a tertiary hospital. Clin. Nutr. 2021, 41, 2940–2946. [Google Scholar] [CrossRef] [PubMed]
- Yaghji, N.I.; Kan, E.K.; Akcan, S.; Colak, R.; Atmaca, A. Hydroxychloroquine Sulfate Related Hypoglycemia in A Non-Diabetic COVİD-19 Patient: A Case Report and Literature Review. Postgrad. Med. 2021, 133, 548–551. [Google Scholar] [CrossRef]
- Ilias, I.; Milionis, C. COVID-19, colchicine and glycemia. Med. Hypotheses 2021, 149, 110547. [Google Scholar] [CrossRef]
- Cryer, P.E.; Axelrod, L.; Grossman, A.B.; Heller, S.R.; Montori, V.M.; Seaquist, E.R.; Service, F.J. Evaluation and management of adult hypoglycemic disorders: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2009, 94, 709–728. [Google Scholar] [CrossRef]
- Griffiths, M.; Gama, R. Adult spontaneous hypoglycaemia. Br. J. Hosp. Med. 2005, 66, 277–283. [Google Scholar] [CrossRef]
- Medagama, A.; Widanapahirana, H.; Prasanga, T. The availability and validity of safety information of over the counter herbal products for use in diabetes in Sri Lanka: A cross sectional study. J. Intercult. Ethnopharmacol. 2015, 4, 264–269. [Google Scholar] [CrossRef]
- Hui, H.; Tang, G.; Go, V.L. Hypoglycemic herbs and their action mechanisms. Chin. Med. 2009, 4, 11. [Google Scholar] [CrossRef]
- Murad, M.H.; Coto-Yglesias, F.; Wang, A.T.; Sheidaee, N.; Mullan, R.J.; Elamin, M.B.; Erwin, P.J. Clinical review: Drug-induced hypoglycemia: A systematic review. J. Clin. Endocrinol. Metab. 2009, 94, 741–745. [Google Scholar] [CrossRef]
- Zagaria, M. Avoiding Drug-Induced Hypoglycemia in the Older Adult. US Pharm. 2019, 44, 4–8. [Google Scholar]
- Marks, V.; Teale, J.D. Drug-induced hypoglycemia. Endocrinol. Metab. Clin. N. Am. 1999, 28, 555–577. [Google Scholar] [CrossRef]
- Karahan, S.; Erden, A.; Esmeray, K.; Karagoz, H.; Gumuscu, H.H.; Basak, M.; Cetinkaya, A.; Avci, D.; Poyrazoglu, O.K. Acute liver failure caused by mushroom poisoning: A case report and review of the literature. Int. Med. Case Rep. J. 2013, 6, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Marks, V.; Teale, J.D. Hypoglycemic disorders. Clin. Lab Med. 2001, 21, 79–97. [Google Scholar] [PubMed]
- Gama, R.; Anderson, N.R.; Marks, V. ‘Glucose meter hypoglycaemia’: Often a non-disease. Ann. Clin. Biochem. 2000, 37 Pt 5, 731–732. [Google Scholar] [CrossRef]
- Bansal, N.; Weinstock, R. Non-Diabetic Hypoglycemia South Dartmouth: Endotext. 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK355894/ (accessed on 5 May 2023).
- Marks, V. Recognition and differential diagnosis of spontaneous hypoglycaemia. Clin. Endocrinol. 1992, 37, 309–316. [Google Scholar] [CrossRef]
- Service, F.J.; Natt, N. The prolonged fast. J. Clin. Endocrinol. Metab. 2000, 85, 3973–3974. [Google Scholar] [CrossRef]
- Hirshberg, B.; Livi, A.; Bartlett, D.L.; Libutti, S.K.; Alexander, H.R.; Doppman, J.L.; Skarulis, M.C.; Gorden, P. Forty-eight-hour fast: The diagnostic test for insulinoma. J. Clin. Endocrinol. Metab. 2000, 85, 3222–3226. [Google Scholar] [CrossRef]
- Service, F.J. Classification of hypoglycemic disorders. Endocrinol. Metab. Clin. N. Am. 1999, 28, 501–517. [Google Scholar] [CrossRef] [PubMed]
- Lefèbvre, P.J.; Andreani, D.; Marks, V.; Creutzfeldt, W. Statement on postprandial hypoglycemia. Diabetes Care 1988, 11, 439–440. [Google Scholar] [CrossRef]
- Johnson, D.D.; Dorr, K.E.; Swenson, W.M.; Service, F.J. Reactive hypoglycemia. JAMA 1980, 243, 1151–1155. [Google Scholar] [CrossRef]
- Yager, J.; Young, R.T. Non-hypoglycemia is an epidemic condition. N. Engl. J. Med. 1974, 291, 907–908. [Google Scholar] [CrossRef] [PubMed]
- De León, D.D.; Stanley, C.A. Determination of insulin for the diagnosis of hyperinsulinemic hypoglycemia. Best Pract. Res. Clin. Endocrinol. Metab. 2013, 27, 763–769. [Google Scholar] [CrossRef]
- Shah, P.; A Rahman, S.; Demirbilek, H.; Güemes, M.; Hussain, K. Hyperinsulinaemic hypoglycaemia in children and adults. Lancet Diabetes Endocrinol. 2016, 5, 729–742. [Google Scholar] [CrossRef]
- Mohammadi, A.; Sulaiman, R.A.; Grossman, A.B. Pasireotide and octreotide in the treatment of severe late dumping syndrome. Clin. Case Rep. 2017, 5, 1608–1611. [Google Scholar] [CrossRef]
- Salehi, M.; Gastaldelli, A.; D’Alessio, D.A. Altered islet function and insulin clearance cause hyperinsulinemia in gastric bypass patients with symptoms of postprandial hypoglycemia. J. Clin. Endocrinol. Metab. 2014, 99, 2008–2017. [Google Scholar] [CrossRef] [PubMed]
- Salehi, M.; Gastaldelli, A.; D’Alessio, D.A. Blockade of glucagon-like peptide 1 receptor corrects postprandial hypoglycemia after gastric bypass. Gastroenterology 2014, 146, 669–680. [Google Scholar] [CrossRef]
- Sulaiman, R.A. Postprandial hypoglycaemia in adults: Pathogenesis, diagnosis and management. J. Lab. Precis. Med. 2021, 6, 13. [Google Scholar] [CrossRef]
- Hirata, Y.; Nishimura, H.; Tominaga, M.; Ishizu, H.; Arimichi, M.; Ogushi, T.; Ouchi, N.; Motomura, S.; Nakamura, Y. Spontaneous hypoglycemia with insulin-autoimmunity. Nihon Naika Gakkai Zasshi 1972, 61, 1296–1304. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lupsa, B.C.; Chong, A.Y.; Cochran, E.K.; Soos, M.A.; Semple, R.K.; Gorden, P. Autoimmune forms of hypoglycemia. Medicine 2009, 88, 141–153. [Google Scholar] [CrossRef]
- Redmon, J.B.; Nuttall, F.Q. Autoimmune hypoglycemia. Endocrinol. Metab. Clin. N. Am. 1999, 28, 603–618. [Google Scholar] [CrossRef]
- Arioglu, E.; Andewelt, A.; Diabo, C.; Bell, M.; Taylor, S.I.; Gorden, P. Clinical course of the syndrome of autoantibodies to the insulin receptor (type B insulin resistance): A 28-year perspective. Medicine 2002, 81, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.E.; Fenn, J.S.; Ford, C.; Gama, R. Autoimmune hypoglycaemia: A narrative review from the laboratory perspective. J. Lab. Precis. Med. 2021, 6, 20. [Google Scholar] [CrossRef]
- Waldron-Lynch, F.; Inzucchi, S.E.; Menard, L.; Tai, N.; Preston-Hurlburt, P.; Hui, P.; McClaskey, J.; Hagopian, W.A.; Meffre, E.; Marks, P.W.; et al. Relapsing and remitting severe hypoglycemia due to a monoclonal anti-insulin antibody heralding a case of multiple myeloma. J. Clin. Endocrinol. Metab. 2012, 97, 4317–4323. [Google Scholar] [CrossRef][Green Version]
- Anlauf, M.; Wieben, D.; Perren, A.; Sipos, B.; Komminoth, P.; Raffel, A.; Kruse, M.L.; Fottner, C.; Knoefel, W.T.; Mönig, H.; et al. Persistent hyperinsulinemic hypoglycemia in 15 adults with diffuse nesidioblastosis: Diagnostic criteria, incidence, and characterisation of beta-cell changes. Am. J. Surg. Pathol. 2005, 29, 524–533. [Google Scholar] [CrossRef]
- Thompson, G.B.; Service, F.; Andrews, J.C.; Lloyd, R.V.; Natt, N.; van Heerden, J.A.; Grant, C.S. Noninsulinoma pancreatogenous hypoglycemia syndrome: An update in 10 surgically treated patients. Surgery 2000, 128, 937–945, discussion 44-5. [Google Scholar] [CrossRef]
- Douillard, C.; Mention, K.; Dobbelaere, D.; Wemeau, J.-L.; Saudubray, J.-M.; Vantyghem, M.-C. Hypoglycaemia related to inherited metabolic diseases in adults. Orphanet J. Rare Dis. 2012, 7, 26. [Google Scholar] [CrossRef]
- Dawson, C. Inherited metabolic disorders associated with hypoglycaemia in adulthood: A narrative review. J. Lab. Precis. Med. 2021, 6, 19. [Google Scholar] [CrossRef]
- Brun, J.F.; Fedou, C.; Mercier, J. Postprandial reactive hypoglycemia. Diabetes Metab. 2000, 26, 337–351. [Google Scholar]
- Celli, R.; Tang, L.H.; Cai, G.; Freedman-Weiss, M.; Colunga, M.; Salem, R.R.; Majumdar, S.; Jain, D. Proinsulin Expressing Neuroendocrine Tumors of the Pancreas: An Underrecognized Entity. Pancreas 2019, 48, 55–59. [Google Scholar] [CrossRef]
- Murtha, T.D.; Lupsa, B.C.; Majumdar, S.; Jain, D.; Salem, R.R. A Systematic Review of Proinsulin-Secreting Pancreatic Neuroendocrine Tumors. J. Gastrointest. Surg. 2017, 21, 1335–1341. [Google Scholar] [CrossRef] [PubMed]
- Kwon, E.B.; Jeong, H.R.; Shim, Y.S.; Lee, H.S.; Hwang, J.S. Multiple Endocrine Neoplasia Type 1 Presenting as Hypoglycemia due to Insulinoma. J. Korean Med. Sci. 2016, 31, 1003–1006. [Google Scholar] [CrossRef] [PubMed]
- Perros, P.; Henderson, A.K.; Carter, D.C.; Toft, A.D. Lesson of the week. Are spontaneous hypoglycaemia, raised plasma insulin and C peptide concentrations, and abnormal pancreatic images enough to diagnose insulinoma? BMJ 1997, 314, 496–497. [Google Scholar] [CrossRef][Green Version]
- Garla, V.; Sonani, H.; Palabindala, V.; Gomez-Sanchez, C.; Subauste, J.; Lien, L.F. Non-islet Cell Hypoglycemia: Case Series and Review of the Literature. Front. Endocrinol. 2019, 10, 316. [Google Scholar] [CrossRef]
- Taylor, S.I.; Grunberger, G.; Marcus-Samuels, B.; Underhill, L.H.; Dons, R.F.; Ryan, J.; Roddam, R.F.; Rupe, C.E.; Gorden, P. Hypoglycemia associated with antibodies to the insulin receptor. N. Engl. J. Med. 1982, 307, 1422–1426. [Google Scholar] [CrossRef] [PubMed]
- Parfitt, C.; Church, D.; Armston, A.; Couchman, L.; Evans, C.; Wark, G.; McDonald, T. Commercial insulin immunoassays fail to detect commonly prescribed insulin analogues. Clin. Biochem. 2015, 48, 1354–1357. [Google Scholar] [CrossRef]
- Egan, A.M.; Galior, K.D.; Maus, A.D.; Fatica, E.; Simha, V.; Shah, P.; Singh, R.J.; Vella, A. Pitfalls in Diagnosing Hypoglycemia Due to Exogenous Insulin: Validation and Utility of an Insulin Analog Assay. Mayo Clin. Proc. 2022, 97, 1994–2004. [Google Scholar] [CrossRef]
- Marks, V.; Teale, J.D. Tumours producing hypoglycaemia. Diabetes/Metab. Res. Rev. 1991, 7, 79–91. [Google Scholar] [CrossRef]
- Kantarova, D.; Sagova, I.; Stancik, M.; Sadlonova, J. Hypoglycemia associated with non-islet cell tumors. Neoplasma 2015, 62, 841–845. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Likhari, T.; Magzoub, S.; Griffiths, M.J.; Buch, H.N.; Gama, R. Screening for Addison’s disease in patients with type 1 diabetes mellitus and recurrent hypoglycaemia. Postgrad. Med J. 2007, 83, 420–421. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, M.J.; Gama, R. Adult Spontaneous Hypoglycaemia; Hospital Medicine: London, UK, 2005; Volume 66. [Google Scholar]
- Kim, N.H.; Kim, D.L.; Choi, K.M.; Baik, S.H.; Choi, D.S. Serum insulin, proinsulin and proinsulin/insulin ratio in type 2 diabetic patients: As an index of beta-cell function or insulin resistance. Korean J. Intern. Med. 2000, 15, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Sheehan, M.T.; Thompson, G.B.; Service, F.J. Insulinoma in chronic renal failure: A case report. J. Clin. Endocrinol. Metab. 2002, 87, 4889–4891. [Google Scholar] [CrossRef] [PubMed][Green Version]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elghobashy, M.; Gama, R.; Sulaiman, R.A. Investigation and Causes of Spontaneous (Non-Diabetic) Hypoglycaemia in Adults: Pitfalls to Avoid. Diagnostics 2023, 13, 3275. https://doi.org/10.3390/diagnostics13203275
Elghobashy M, Gama R, Sulaiman RA. Investigation and Causes of Spontaneous (Non-Diabetic) Hypoglycaemia in Adults: Pitfalls to Avoid. Diagnostics. 2023; 13(20):3275. https://doi.org/10.3390/diagnostics13203275
Chicago/Turabian StyleElghobashy, Maiar, Rousseau Gama, and Raashda Ainuddin Sulaiman. 2023. "Investigation and Causes of Spontaneous (Non-Diabetic) Hypoglycaemia in Adults: Pitfalls to Avoid" Diagnostics 13, no. 20: 3275. https://doi.org/10.3390/diagnostics13203275
APA StyleElghobashy, M., Gama, R., & Sulaiman, R. A. (2023). Investigation and Causes of Spontaneous (Non-Diabetic) Hypoglycaemia in Adults: Pitfalls to Avoid. Diagnostics, 13(20), 3275. https://doi.org/10.3390/diagnostics13203275






