Brochoscopic Airway Clearance Therapy vs. Conventional Sputum Aspiration: The Future of Flexible Brochoscopes in Intensive Care Units?
Abstract
:1. Introduction
2. Materials and Methods
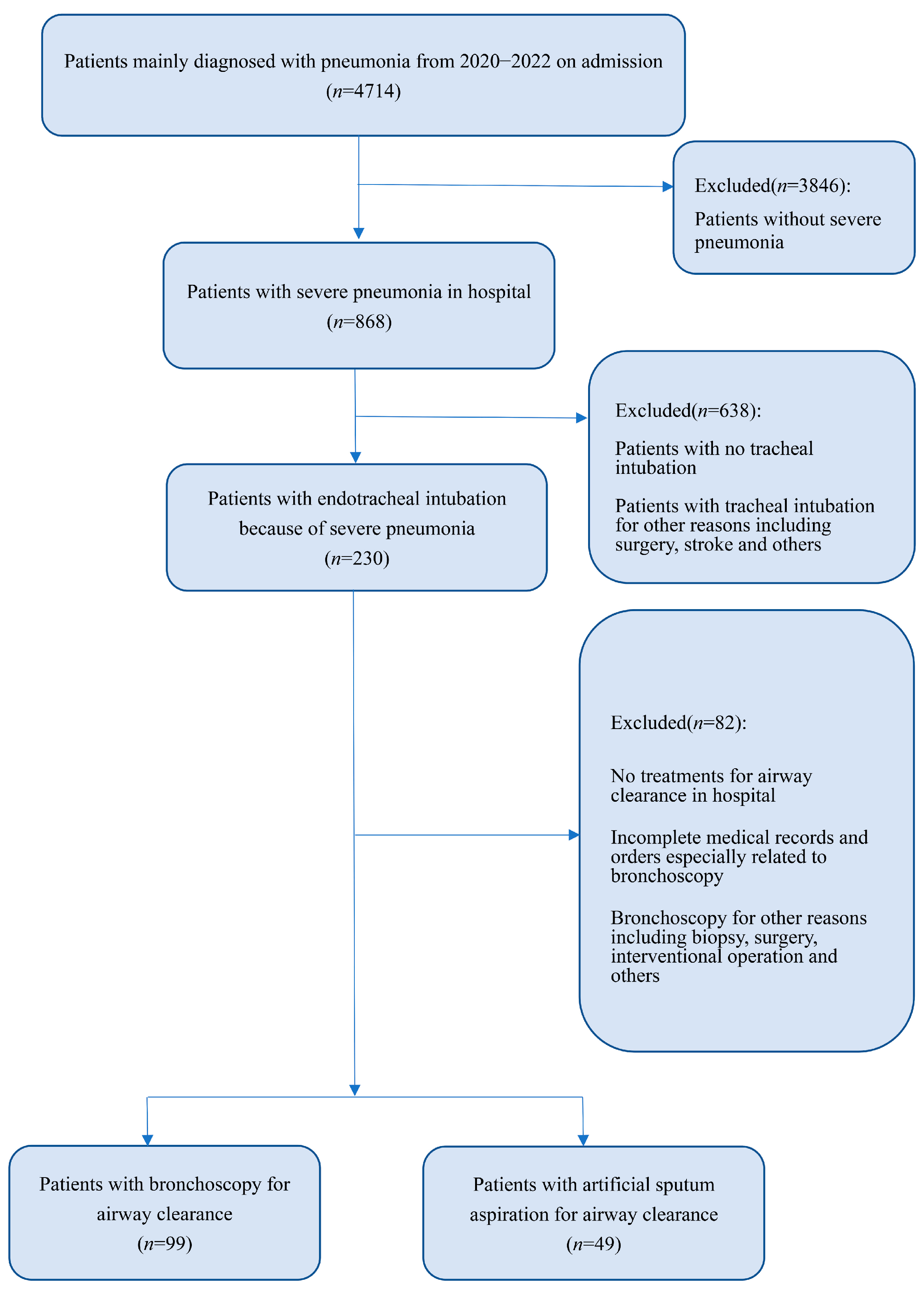
2.1. Patients
2.2. Treatment Methods
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Baseline Cohort Characteristics
3.2. Preoperative and Postoperative Blood Laboratory Results
3.3. Comparison of Changes of Important Indicators
3.4. The Kaplan–Meier Analysis and Survival Curves
3.5. Univariate and Multivariate COX Regression Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Bhutta, Z.A. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Mandell, L.A.; Wunderink, R.G.; Anzueto, A.; Bartlett, J.G.; Campbell, G.D.; Dean, N.C.; Dowell, S.F.; File, T.M., Jr.; Musher, D.M.; Niederman, M.S.; et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2007, 44 (Suppl. 2), S27–S72. [Google Scholar] [CrossRef] [PubMed]
- Reyes, L.F.; Garcia-Gallo, E.; Pinedo, J.; Saenz-Valcarcel, M.; Celi, L.; Rodriguez, A.; Waterer, G. Scores to Predict Long-term Mortality in Patients with Severe Pneumonia Still Lacking. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2021, 72, e442–e443. [Google Scholar] [CrossRef]
- Alves, D.; Grainha, T.; Pereira, M.O.; Lopes, S.P. Antimicrobial materials for endotracheal tubes: A review on the last two decades of technological progress. Acta Biomater. 2023, 158, 32–55. [Google Scholar] [CrossRef] [PubMed]
- Cillóniz, C.; Torres, A.; Niederman, M.S. Management of pneumonia in critically ill patients. BMJ Clin. Res. Ed. 2021, 375, e065871. [Google Scholar] [CrossRef]
- Hoo, Z.H.; Daniels, T.; Wildman, M.J.; Teare, M.D.; Bradley, J.M. Airway clearance techniques used by people with cystic fibrosis in the UK. Physiotherapy 2015, 101, 340–348. [Google Scholar] [CrossRef]
- Korkmaz Ekren, P.; Basarik Aydogan, B.; Gurgun, A.; Tasbakan, M.S.; Bacakoglu, F.; Nava, S. Can fiberoptic bronchoscopy be applied to critically ill patients treated with noninvasive ventilation for acute respiratory distress syndrome? Prospective observational study. BMC Pulm. Med. 2016, 16, 89. [Google Scholar] [CrossRef] [PubMed]
- Luo, F.; Darwiche, K.; Singh, S.; Torrego, A.; Steinfort, D.P.; Gasparini, S.; Liu, D.; Zhang, W.; Fernandez-Bussy, S.; Herth, F.J.F.; et al. Performing Bronchoscopy in Times of the COVID-19 Pandemic: Practice Statement from an International Expert Panel. Respir. Int. Rev. Thorac. Dis. 2020, 99, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flanders, S.A.; et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef] [PubMed]
- Respiratory Branch of the Chinese Medical Association; Respiratory Endoscopy Committee of the Chinese Medical Association. Expert consensus on the clinical application of single-use (disposable) flexible bronchoscopes. Chin. J. Tuberc. Respir. Dis. 2023, 46, 41–48. [Google Scholar] [CrossRef]
- Karbasy, S.H.; Sabertanha, A.; Bayati, M.; Meshkini, A.; Fatemeh Shakhs Emampour, B. Study of the effect of added bronchoscopic suction to routine treatment of ventilator associated pneumonia patients in surgical ICU. J. Pak. Med. Assoc. 2021, 71, 1326–1331. [Google Scholar] [CrossRef]
- Zhao, H.; Gu, H.; Liu, T.; Ge, J.; Shi, G. Analysis of curative effect of adjuvant therapy with bronchoalveolar lavage on COPD patients complicated with pneumonia. Exp. Ther. Med. 2018, 16, 3799–3804. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhao, H.R.; Wei, H.L.; Chen, C.; Qiu, R.X.; Ren, X.L.; Zhang, L.; Gao, Y.Q. Efficacy of Bronchoalveolar Lavage as Adjunct Therapy in the Treatment of Neonatal Severe Pneumonia: A Prospective Case-Control Study. J. Trop. Pediatr. 2020, 66, 528–533. [Google Scholar] [CrossRef] [PubMed]
- Pei, M.; Jiang, P.; Wang, T.; Xia, C.; Hou, R.; Sun, A.; Zou, H. Effect of bronchoalveolar lavage on the clinical efficacy, inflammatory factors, and immune function in the treatment of refractory pneumonia in children. Transl. Pediatr. 2021, 10, 921–928. [Google Scholar] [CrossRef]
- Wang, C.; Ye, S.; Wang, X.; Zhao, Y.; Ma, Q.; Wang, L. Clinical Efficacy and Safety of Mechanical Ventilation Combined with Fiberoptic Bronchoalveolar Lavage in Patients with Severe Pulmonary Infection. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 5401–5407. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Li, Z.; Cheng, W.; Zhang, B.; Zhu, W.; Lin, Z. Application of sputum suction by fiberoptic bronchoscope in patients with severe pneumonia and its effect on inflammatory factors. Am. J. Transl. Res. 2021, 13, 8409–8414. [Google Scholar]
- Wu, L.; Liu, B. The clinical effect of a bronchofiberscope in treating severe ventilator-associated pneumonia. Am. J. Transl. Res. 2021, 13, 6966–6972. [Google Scholar]
- Li, L.; Zhang, M.; Wei, Y.; Tu, X.; Lu, Z.; Cheng, Y. Clinical significance of procalcitonin in critically ill patients with pneumonia receiving bronchoalveolar lavage. Sarcoidosis Vasc. Diffus. Lung Dis. Off. J. WASOG 2022, 39, e2022031. [Google Scholar] [CrossRef]
- Zhang, L.; Li, S.; Yuan, S.; Lu, X.; Li, J.; Liu, Y.; Huang, T.; Lyu, J.; Yin, H. The Association between Bronchoscopy and the Prognoses of Patients with Ventilator-Associated Pneumonia in Intensive Care Units: A Retrospective Study Based on the MIMIC-IV Database. Front. Pharmacol. 2022, 13, 868920. [Google Scholar] [CrossRef]
- Lee, H.W.; Min, J.; Park, J.; Lee, Y.J.; Kim, S.J.; Park, J.S.; Yoon, H.I.; Lee, J.H.; Lee, C.T.; Cho, Y.J. Clinical impact of early bronchoscopy in mechanically ventilated patients with aspiration pneumonia. Respirology 2015, 20, 1115–1122. [Google Scholar] [CrossRef]
- Wu, X.; Lu, W.; Sang, X.; Xu, Y.; Wang, T.; Zhan, X.; Hao, J.; Ren, R.; Zeng, H.; Li, S. Timing of bronchoscopy and application of scoring tools in children with severe pneumonia. Ital. J. Pediatr. 2023, 49, 44. [Google Scholar] [CrossRef]
- Qiao, Z.; Yu, J.; Yu, K.; Zhang, M. The benefit of daily sputum suction via bronchoscopy in patients of chronic obstructive pulmonary disease with ventilators: A randomized controlled trial. Medicine 2018, 97, e11631. [Google Scholar] [CrossRef]
- Han, Q.; Chen, C.; Fu, R.; Tan, L.; Xia, L. Portable fibrobronchoscopic treatment for non-severe ischemic stroke-associated pneumonia patients with dysphagia: A pilot study. Neurol. Res. 2019, 41, 216–222. [Google Scholar] [CrossRef]
- Han, Q.; Chen, C.; Hu, H.Q.; Shen, J.; Yang, G.; Chen, B.; Xia, L. Effect evaluation on use of bedside fiber bronchoscope in treating stroke-associated pneumonia. Top. Stroke Rehabil. 2018, 25, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Zhao, L.; Li, J.; Shi, J. Clinical effect of antibiotic combined with fiber bronchoscope perfusion in treatment of pneumonia after severe cerebral hemorrhage. Medicine 2022, 101, e30675. [Google Scholar] [CrossRef] [PubMed]
- Baudel, J.L.; Tankovic, J.; Dahoumane, R.; Carrat, F.; Galbois, A.; Ait-Oufella, H.; Offenstadt, G.; Guidet, B.; Maury, E. Multiplex PCR performed of bronchoalveolar lavage fluid increases pathogen identification rate in critically ill patients with pneumonia: A pilot study. Ann. Intensive Care 2014, 4, 35. [Google Scholar] [CrossRef]
- Chen, H.; Bai, X.; Gao, Y.; Liu, W.; Yao, X.; Wang, J. Profile of Bacteria with ARGs Among Real-World Samples from ICU Admission Patients with Pulmonary Infection Revealed by Metagenomic NGS. Infect. Drug Resist. 2021, 14, 4993–5004. [Google Scholar] [CrossRef]
- Zhou, W.; Zhou, C.; Liu, X.; Shi, N.; Quyang, W.; Tu, D.; Xin, Y.; Ji, L. A randomised trial on the therapeutic effectiveness of bronchoalveolar lavage under fiberoptic bronchoscopy in patients with severe lung infection living in the Tibetan plateau area. Ann. Palliat. Med. 2021, 10, 3336–3342. [Google Scholar] [CrossRef]
- Lee, D.H.; Driver, B.E.; Prekker, M.E.; Puskarich, M.A.; Plummer, D.; Mojica, E.Y.; Smith, J.C.; DeVries, P.A.; Stang, J.L.; Reardon, R.F. Bronchoscopy in the emergency department. Am. J. Emerg. Med. 2022, 58, 114–119. [Google Scholar] [CrossRef]
- Mouritsen, J.M.; Ehlers, L.; Kovaleva, J.; Ahmad, I.; El-Boghdadly, K. A systematic review and cost effectiveness analysis of reusable vs. single-use flexible bronchoscopes. Anaesthesia 2020, 75, 529–540. [Google Scholar] [CrossRef] [PubMed]
- Châteauvieux, C.; Farah, L.; Guérot, E.; Wermert, D.; Pineau, J.; Prognon, P.; Borget, I.; Martelli, N. Single-use flexible bronchoscopes compared with reusable bronchoscopes: Positive organizational impact but a costly solution. J. Eval. Clin. Pract. 2018, 24, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Ho, E.; Wagh, A.; Hogarth, K.; Murgu, S. Single-Use and Reusable Flexible Bronchoscopes in Pulmonary and Critical Care Medicine. Diagnostics 2022, 12, 174. [Google Scholar] [CrossRef]
- Barron, S.P.; Kennedy, M.P. Single-Use (Disposable) Flexible Bronchoscopes: The Future of Bronchoscopy? Adv. Ther. 2020, 37, 4538–4548. [Google Scholar] [CrossRef]
- Ergan, B.; Nava, S. The use of bronchoscopy in critically ill patients: Considerations and complications. Expert Rev. Respir. Med. 2018, 12, 651–663. [Google Scholar] [CrossRef]
- Pelaia, C.; Bruni, A.; Garofalo, E.; Rovida, S.; Arrighi, E.; Cammarota, G.; Navalesi, P.; Pelaia, G.; Longhini, F. Oxygenation strategies during flexible bronchoscopy: A review of the literature. Respir. Res. 2021, 22, 253. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.M.; Arenberg, D.A.; Barjaktarevic, I.; Bhatt, S.P.; Bowler, R.P.; Christenson, S.A.; Couper, D.J.; Dransfield, M.T.; Han, M.K.; Hoffman, E.A.; et al. Safety and Tolerability of Comprehensive Research Bronchoscopy in Chronic Obstructive Pulmonary Disease. Results from the SPIROMICS Bronchoscopy Substudy. Ann. Am. Thorac. Soc. 2019, 16, 439–446. [Google Scholar] [CrossRef] [PubMed]



| Variables | Bronchoscopy n = 99 | No Bronchoscopy n = 49 | p | ≤Once Every 3 Days n = 50 | >Once Every 3 Days n = 49 | p |
|---|---|---|---|---|---|---|
| Age | 68(52, 76) | 70(60.5, 78) | 0.196 | 69(50.25, 76) | 67(54, 76) | 0.809 |
| BMI | 22.5817 ± 3.67431 | 23.7090 ± 3.70282 | 0.082 | 22.9947 ± 3.54403 | 22.1576 ± 3.79185 | 0.258 |
| Sex | 0.969 | 0.347 | ||||
| Male = 0 | 69(69.7%) | 34(69.4%) | 37(74%) | 32(65.3%) | ||
| Female = 1 | 30(30.3%) | 15(30.6%) | 13(26%) | 17(34.7%) | ||
| Comorbidities | 0.393 | 0.985 | ||||
| No = 0 | 17(17.2%) | 2(4.1%) | 9(18%) | 8(16.3%) | ||
| HBP = 1 | 3(3.0%) | 2(4.1%) | 1(2%) | 2(4.1%) | ||
| CVA = 2 | 34(34.3%) | 19(38.8%) | 18(36%) | 16(32.7%) | ||
| CHD = 3 | 16(16.2%) | 11(22.4%) | 8(16%) | 8(16.3%) | ||
| DM = 4 | 10(10.1%) | 5(10.2%) | 5(10%) | 5(10.2%) | ||
| COPD = 5 | 13(13.1%) | 6(12.2%) | 7(14%) | 6(12.2%) | ||
| Others = 6 | 6(6.1%) | 4(8.2%) | 2(4%) | 4(8.2%) | ||
| Antibiotic therapy | 0.958 | 0.946 | ||||
| B | 35(35.4%) | 16(33.3%) | 18(36.0%) | 17(34.7%) | ||
| B + F | 55(55.6%) | 28(58.3%) | 28(56.0%) | 27(55.1%) | ||
| B + V | 3(3.0%) | 2(4.2%) | 1(2.0%) | 2(4.1%) | ||
| B + F+V | 6(6.1%) | 2(4.2%) | 3(6.0%) | 3(6.1%) | ||
| Antibiotic days | 18(5, 33) | 12(6, 19) | 0.082 | 19.5(11, 46) | 15(3, 25) | 0.109 |
| Laboratory Results | Have Bronchoscopy | No Bronchoscopy | p Value |
|---|---|---|---|
| Routine blood parameters | |||
| PLT (109/L) | |||
| Pre treatment | 185(113, 311) | 172(121, 221.5) | 0.315 |
| Post treatment | 202.9502 ± 109.45456 | 160(101.5, 249) | 0.121 |
| p value | 0.224 | 0.423 | |
| WBC (109/L) | |||
| Pre treatment | 14.08(11.26, 18.61) | 16.72(13.58, 19.485) | 0.125 |
| Post treatment | 7.21(5.57, 9.48) | 11.68(7.655, 15.975) | <0.001 |
| p value | <0.001 | 0.002 | |
| N (%) | |||
| Pre treatment | 91.8(88.8, 95.0) | 92.2(88.55, 93.9) | 0.347 |
| Post treatment | 74.8(65.6, 83.2) | 84(73.6, 89.3) | 0.001 |
| p value | <0.001 | <0.001 | |
| Blood gas analysis | |||
| PH | |||
| Pre treatment | 7.32(7.22, 7.40) | 7.31(7.21, 7.37) | 0.181 |
| Post treatment | 7.40(7.39, 7.42) | 7.41(7.335, 7.4535) | 0.382 |
| p value | <0.001 | <0.001 | |
| PCO2 (mmHg) | |||
| Pre treatment | 42.8929 ± 12.15666 | 42.9(38.1, 49.95) | 0.389 |
| Post treatment | 40(37, 43) | 39(32.35, 45.95) | 0.191 |
| p value | 0.076 | 0.009 | |
| PO2 (mmHg) | |||
| Pre treatment | 66(56, 71) | 68.7(59.4, 72.5) | 0.167 |
| Post treatment | 84(77.7, 100) | 74(68.4, 96.9) | 0.005 |
| p value | <0.001 | 0.009 | |
| SO2 (mmHg) | |||
| Pre treatment | 62.2(58, 64.4) | 65(49, 75.5) | 0.225 |
| Post treatment | 89(88.9, 90) | 83(79.05, 88.85) | <0.001 |
| p value | <0.001 | <0.001 | |
| Inflammatory factors | |||
| PCT (ng/mL) | |||
| Pre treatment | 6.12(5.26, 9.90) | 5.80(4.915, 12.12) | 0.189 |
| Post treatment | 0.52(0.11,2.90) | 2.2(1.395, 4.180) | <0.001 |
| p value | <0.001 | <0.001 | |
| CRP (mg/L) | |||
| Pre treatment | 168.23(109.18, 250) | 160.6(80.33, 201.77) | 0.220 |
| Post treatment | 25.36(8.80, 71.40) | 67(17.895, 135.005) | 0.005 |
| p value | <0.001 | <0.001 | |
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Bronchoscopy | <0.001 | 0.011 | ||
| No | Reference | Reference | ||
| Yes | 0.247(0.154, 0.397) | <0.001 | 0.444(0.238, 0.829) | 0.011 |
| Tracheotomy | <0.001 | 0.023 | ||
| No | Reference | Reference | ||
| Yes | 0.364(0.235, 0.565) | <0.001 | 0.514(0.290, 0.912) | 0.023 |
| Therapy | 0.018 | 0.518 | ||
| Antibacterial | Reference | Reference | ||
| Antibacterial and antifungal | 0.559(0.374, 0.835) | 0.005 | 0.765(0.473, 1.237) | 0.275 |
| Antibacterial and antiviral | 1.743(0.539, 5.631) | 0.353 | 0.631(0.167, 2.378) | 0.496 |
| Antibacterial, antifungal and antiviral | 0.677(0.210, 2.183) | 0.513 | 1.546(0.450, 5.317) | 0.489 |
| Hormone | <0.001 | <0.001 | ||
| No | Reference | Reference | ||
| Yes | 0.363(0.241, 0.547) | <0.001 | 0.356(0.221, 0.573) | <0.001 |
| IVIG | 0.028 | 0.954 | ||
| No | Reference | Reference | ||
| Yes | 0.492(0.261, 0.926) | 0.028 | 1.023(0.478, 2.188) | 0.954 |
| Intestinal probiotic | 0.012 | 0.079 | ||
| No | Reference | Reference | ||
| Yes | 0.475(0.266, 0.847) | 0.012 | 0.497(0.228, 1.084) | 0.079 |
| Microbial species | <0.001 | 0.130 | ||
| No = 0 | Reference | Reference | ||
| Bacteria = 1 | 0.507(0.255, 1.010) | 0.054 | 0.716(0.332, 1.544) | 0.394 |
| Fungal = 2 | 0.289(0.121, 0.693) | 0.005 | 0.390(0.144, 1.054) | 0.063 |
| Bacteria and fungal = 3 | 0.240(0.120, 0.479) | <0.001 | 0.453(0.199, 1.033) | 0.060 |
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Bronchoscopy | <0.001 | <0.001 | ||
| >once every 3 days | Reference | Reference | ||
| ≤once every 3 days | 0.259(0.154, 0.437) | <0.001 | 0.285(0.163, 0.498) | <0.001 |
| Tracheotomy | 0.013 | 0.221 | ||
| No | Reference | Reference | ||
| Yes | 0.492(0.281, 0.859) | 0.013 | 0.693(0.385, 1.246) | 0.221 |
| Therapy | 0.480 | |||
| Anti-bacteria | Reference | |||
| Anti-bacteria and anti-fungal | 0.757(0.468, 1.225) | 0.257 | ||
| Anti-bacteria and anti-viral | 1.759(0.415, 7.461) | 0.444 | ||
| Anti-bacteria, anti-fungal and anti-viral | 1.155(0.346, 3.856) | 0.814 | ||
| Hormone | 0.001 | 0.007 | ||
| No | Reference | Reference | ||
| Yes | 0.445(0.271, 0.732) | 0.001 | 0.485(0.287, 0.820) | 0.007 |
| IVIG | 0.040 | 0.118 | ||
| No | Reference | Reference | ||
| Yes | 0.478(0.236, 0.968) | 0.040 | 0.562(0.272, 1.159) | 0.118 |
| Intestinal probiotic | 0.056 | |||
| No | Reference | |||
| Yes | 0.548(0.296, 1.015) | 0.056 | ||
| Microbial species | 0.087 | |||
| No = 0 | Reference | |||
| Bacteria = 1 | 0.597(0.203, 1.751) | 0.347 | ||
| Fungal = 2 | 0.378(0.113, 1.269) | 0.115 | ||
| Bacteria and fungal = 3 | 0.344(0.120, 0.985) | 0.047 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yao, A.; Liu, Z.; He, W.; Rao, H.; Wang, C.; Xie, S. Brochoscopic Airway Clearance Therapy vs. Conventional Sputum Aspiration: The Future of Flexible Brochoscopes in Intensive Care Units? Diagnostics 2023, 13, 3276. https://doi.org/10.3390/diagnostics13203276
Yao A, Liu Z, He W, Rao H, Wang C, Xie S. Brochoscopic Airway Clearance Therapy vs. Conventional Sputum Aspiration: The Future of Flexible Brochoscopes in Intensive Care Units? Diagnostics. 2023; 13(20):3276. https://doi.org/10.3390/diagnostics13203276
Chicago/Turabian StyleYao, Anjie, Zixuan Liu, Wenni He, Hanyu Rao, Changhui Wang, and Shuanshuan Xie. 2023. "Brochoscopic Airway Clearance Therapy vs. Conventional Sputum Aspiration: The Future of Flexible Brochoscopes in Intensive Care Units?" Diagnostics 13, no. 20: 3276. https://doi.org/10.3390/diagnostics13203276
APA StyleYao, A., Liu, Z., He, W., Rao, H., Wang, C., & Xie, S. (2023). Brochoscopic Airway Clearance Therapy vs. Conventional Sputum Aspiration: The Future of Flexible Brochoscopes in Intensive Care Units? Diagnostics, 13(20), 3276. https://doi.org/10.3390/diagnostics13203276





