User Perceptions of Avatar-Based Patient Monitoring for Intensive Care Units: An International Exploratory Sequential Mixed-Methods Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Approval and Consent
2.2. Study Design
2.3. Previous Study
2.4. Participant Interviews and Online Survey
2.4.1. Part I: Participant Interviews
2.4.2. Part II: Online Survey
2.5. Statistical Analysis
3. Results
3.1. Study and Participant Characteristics
3.2. Part I: Participant Interviews
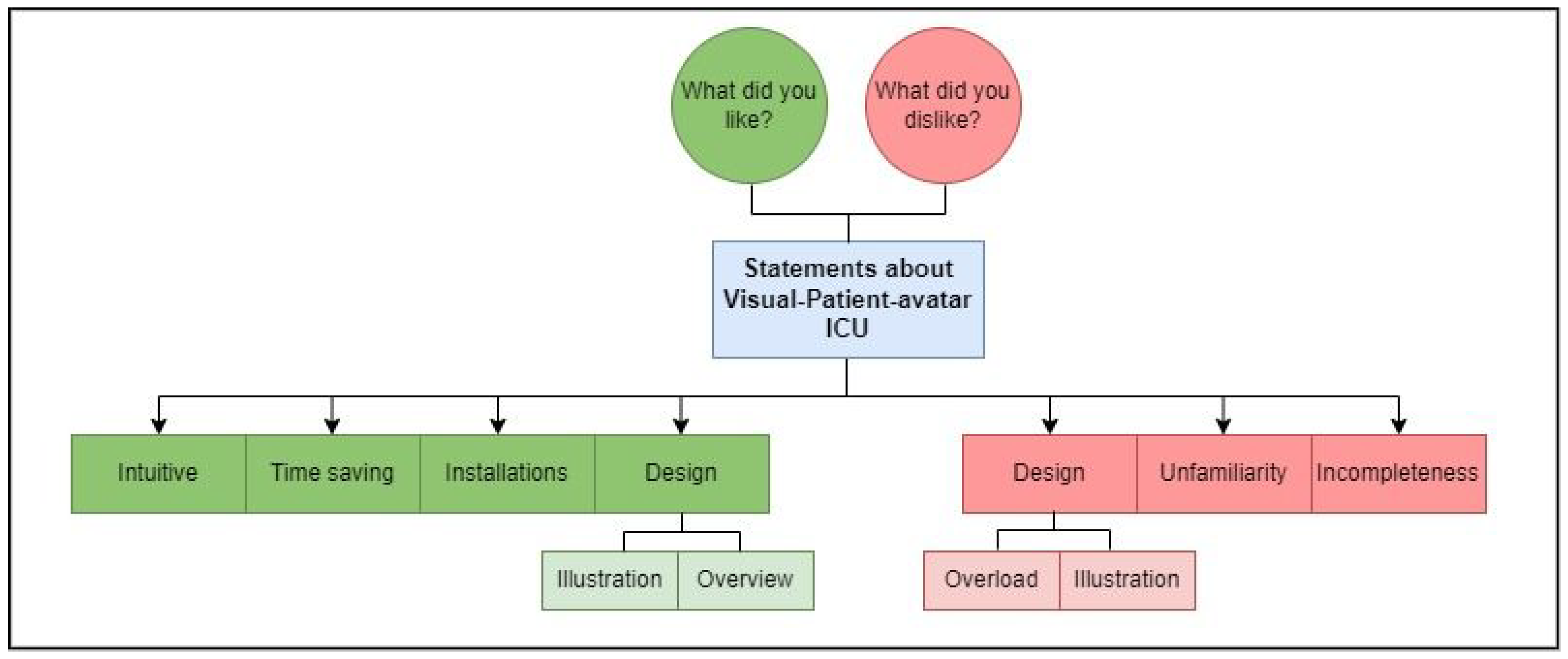
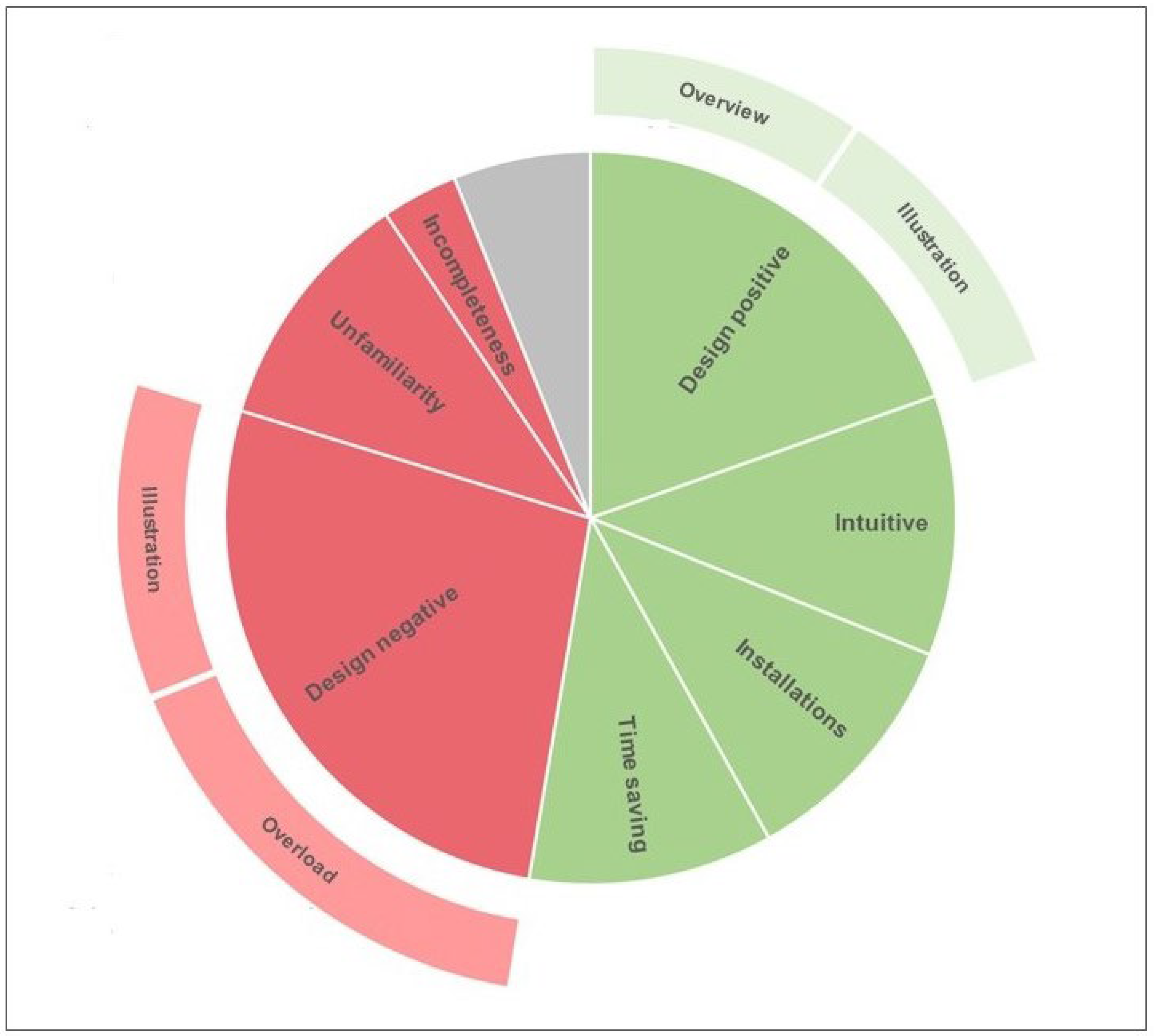
3.2.1. Coding Template
3.2.2. Positive Statements about Visual Patient Avatar ICU
Design
Intuitiveness
Time Saving
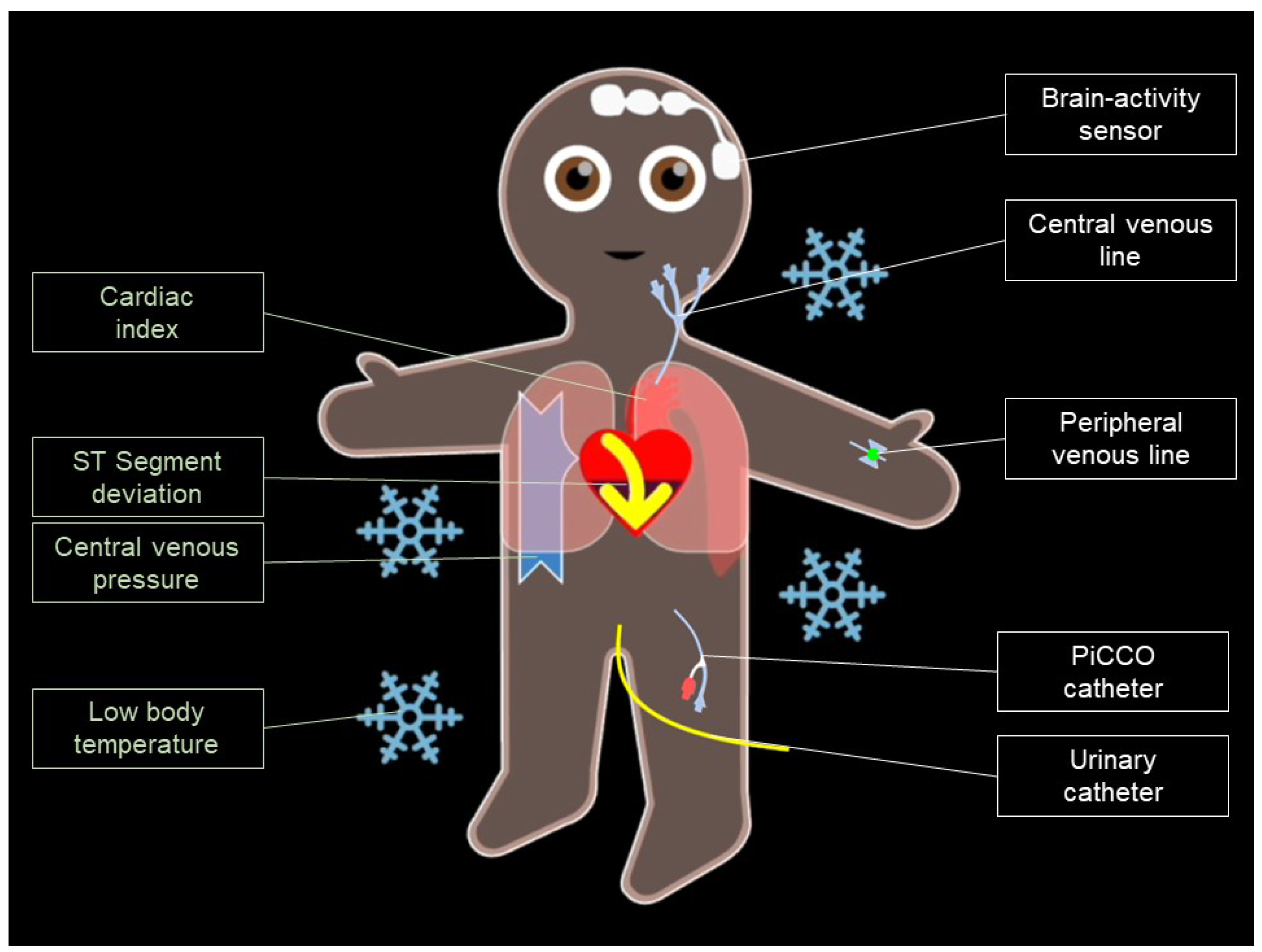
Patient Inserted Devices
3.2.3. Negative Statements about Visual Patient Avatar ICU
Design
Unfamiliarity
Incompleteness
3.3. Part II: Online Survey
4. Discussion
4.1. Principal Findings
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Participant #01POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Installations are clearer][Deviations can be detected more quickly]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Nothing]
- Participant #02POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Easier visualization of devices][Easier to see when something is REALLY wrong]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Takes time to get used (hard for an old dog to learn new tricks) to it but it seems rather intuitive after a while][Too many parameters at once are hard to discern in 15 s when you are used to the monitor]
- Participant #03POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[There is a lot of potential in recognizing pathological values more quickly with an additional visual aid.][There is certainly a fast learning curve in interpreting the visual patient]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[but it is not completely intuitive and some amount of training is needed]
- Participant #04POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Quicker overview than conventional monitor]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[No numbers][Installations could be better visualized]
- Participant #05POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Catheter easier to remember]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Too cluttered][Too much information in one image]
- Participant #06POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Installations][Colored markings]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Overload of information][Unclear]
- Participant #07POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[You can remember more][Especially installations]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Watch training videos several times, could not remember meaning of parameters]
- Participant #08POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[You can see everything at a glance, you don’t have to switch to another line][You can quickly see if everything is okay or not okay. In the recovery room, it is important to see whether I am within the normal range. Numbers are not so relevant at first.][Colored markings]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[When some parameters are not in the normal range, it is harder to tell the difference][For the recovery room, I would rather wish to be able to switch back and forth between the monitor types than to have a split monitor.]
- Participant #09POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Serious problems are clearly presented immediately]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Training/some experience with it nevertheless necessary.][Too many overlays in the torso area (colors Spo2, Fio2)][Display of installations of questionable usefulness (pointless for supervisors, not useful for emergency intervention team for clarity)]
- Participant #10POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Quick visual overview of the problems][Color highlighting of complications][Installations immediately clear]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Training]
- Participant #11POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Single utilization with numerical trend display]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Split in In Norm Representation and Pathological]
- Participant #12POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Visualization of the organ systems][Installations seen at a glance][Possibility to recognize the ST elevation by color]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Tidal volume not flashy enough]
- Participant #13POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Simple overview of the overall situation]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU[Too many visual parameters in the thoracic area (CI, Tidal, etc…]
- Participant #14POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Looks cute]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[I have to learn the particular look for what exactly stands for what. It’s a habit, of course. The values for conventional monitoring are learned during raining, but the appearance of the “symbols” is not]
- Participant #15POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Better overview]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Some parameters displayed too complicated]
- Participant #16POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Display heart rate and temperature]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Display ZVD]
- Participant #17POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[You get a very fast first impression of the patient]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[The graphics could look more professional]
- Participant #18POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Visual overview in less time than with formal parameters]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Overlapping information in the thoracic region]
- Participant #19POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Intuitive][Installations very well visualized]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[-]
- Participant #20POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[The idea that “changes” pop up and are thus “differently” perceived][Installations are more recognizable because you see where they are]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Saturation low: how low is it? 90% ? 70%?]
- Participant #21POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Faster overview over medical installations]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Picture crowded]
- Participant #22POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[The color marking is clear and pleasant][With sufficient training it is certainly easier to quickly get an overview of the patient’s vital signs]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Partially very much, with overlapping of different vital parameters thereby the admission of individual parameters is felt more heavily one gets][However with some practice out on which one to pay attention]
- Participant #23POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Great if it works ]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Differences in respiration O2 capnometry etc. should be better distinguishable]
- Participant #24POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Can imagine that you get good support in everyday work][But serious things are noticed quickly!]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[With many parameters at the same time it looks a bit overloaded.][It would be nice to have a function to visualize only values that deviate from the norm][Once you have become familiar with it and have memorized the individual parameters, a matter of practice, like probably everything else]
- Participant #25POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[I find the color representation good]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Realization of the catheter was complicated for me]
- Participant #26POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Simple handling][Easy understanding]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Colors sometimes a bit confusing]
- Participant #27POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Positive overview]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Sensory overload in the first moment]
- Participant #28POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Quick overview of critical parameters][Very helpful when observing multiple patients at the same time]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[-]
- Participant #29POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Alarm summary]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Complex visualization resp. Ventilation—relatively long period of observation concerning CO2 and respiratory rate]
- Participant #30POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[You capture a lot of information at a glance]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[I could not intuitively interpret the colors]
- Participant #31POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[In fact, the Visual Patient provides a quick and][Sufficient overview of the measured parameters]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Color scheme partly in need of revision]
- Participant #32POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Ground (intuitive?) feeling about the individual values is retained longer]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[“Actual”/acute problem of the patient is difficult to grasp (stimulus overload)]
- Participant #33POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Accesses easier to detect (less urgent on intensive)][Probably faster to learn][Main problems more quickly detectable for the inexperienced]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[In unstable patients (especially tachycardia+tachypnea “overloaded” monitor]
- Participant #34POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Isolated problems are better representable]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Partially too superimposed, especially with high blood pressure & fast heart rate][“Strobe”]
- Participant #35POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Catheters are quicker and easier to remember]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Too much information in one image][It takes time to get used to it]
- Participant #36POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Simple overview]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Overwhelming, if a lot of devices are installed]
- Participant #37POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Accesses and vital signs can be acquired more quickly]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[For europe use, caucasian patients]
- Participant #38POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Easy to learn][Problems are quickly recognizable][Good overview of the accesses]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Sometimes too confusing][Difficult to get used to, when you are used to the old system][Presentation sometimes not intuitive]
- Participant #39POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Fewer values/numbers][More intuitive decision-making possible after practice phase]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[A period of habituation is necessary]
- Participant #40POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Situations are color-coded][Accesses are easier to recognize][Temperature is easier to recognize][Oxygenation is easier to recognize]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Pictograms not easy to recognize for me][Presentation a little too infantile for me]
- Participant #41POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Simple and easy to understand]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Some parameters like arterial blood pressure are difficult to see]
- Participant #42POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[It is much more intuitive][and perhaps doesn’t make you think as much because it discerns what is right and what is wrong]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Too many variables are integrated in the same image][Perhaps it would be useful to do it in two different figures]
- Participant #43POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Global vision][Useful maybe to screen stable vs unstable patient initially][Cool for lines and devices]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Overlap of colors and parameters]
- Participant #44POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[The practicality of easily recognizing slight alterations, when they are not yet established problems, to manage the threshold of complications and avoid them][The visual memory is in occasions more complete and][Provides data that a priori much ascended we do not take into account][A different learning for a more complete approach.]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[The visualization of a doll omits all the information that gives us the morphology of the curves]
- Participant #45POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[The simplicity of a more visual image]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[A very saturated drawing perhaps]
- Participant #46POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[It is a good method of monitoring]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Training needed]
- Participant #47POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[It is easy to visualize where devices such as IVs and catheters are located]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[It is quite overwhelming when you have a high heart rate and it blinks a lot]
- Participant #48POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[Very intuitive]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Blood pressure, Oxygen Inspiration and Tidal Volume were confusing]
- Participant #49POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[It’s easier to visualize]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[More practice is necessary]
- Participant #50POSITIVE: What did you LIKE about Visual-Patient-avatar ICU?[See the problem quickly]NEGATIVE: What did you DISLIKE about Visual-Patient-avatar ICU?[Sometimes too much information]
References
- Görges, M.; Kück, K.; Koch, S.H.; Agutter, J.M.; Westenskow, D.R. A Far-View Intensive Care Unit Monitoring Display Enables Faster Triage. Dimens. Crit. Care Nurs. 2011, 30, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Wright, M.C.; Taekman, J.M.; Endsley, M.R. Objective measures of situation awareness in a simulated medical environment. Heart 2004, 13, i65–i71. [Google Scholar] [CrossRef]
- Neuraz, A.; Guérin, C.; Payet, C.; Polazzi, S.; Aubrun, F.; Dailler, F.; Lehot, J.-J.; Piriou, V.; Neidecker, J.; Rimmelé, T.; et al. Patient Mortality Is Associated with Staff Resources and Workload in the ICU: A Multicenter Observational Study. Crit. Care Med. 2015, 43, 1587–1594. [Google Scholar] [CrossRef] [PubMed]
- Knight, L.D. Staffing Ratios and Patient Outcomes: Looking Beyond Nurses, Doctors, and Survival at ICU Discharge. Crit. Care Med. 2016, 44, e107–e108. [Google Scholar] [CrossRef] [PubMed]
- Pastores, S.M. Staffing Ratios and Workload in Critically Ill Patients: Do They Impact Outcomes? Crit. Care Med. 2015, 43, 1775–1776. [Google Scholar] [CrossRef] [PubMed]
- Endsley, M.R. A Systematic Review and Meta-Analysis of Direct Objective Measures of Situation Awareness: A Comparison of SAGAT and SPAM. Hum. Factors J. Hum. Factors Ergon. Soc. 2019, 63, 124–150. [Google Scholar] [CrossRef]
- Schulz, C.M.; Endsley, M.R.; Kochs, E.F.; Gelb, A.W.; Wagner, K.J. Situation awareness in anesthesia: Concept and research. Anesthesiology 2013, 118, 729–742. [Google Scholar] [CrossRef] [PubMed]
- Oury, J.D.; Ritter, F.E. How User-Centered Design Supports Situation Awareness for Complex Interfaces; Human–Computer Interaction Series; Vanderdonckt, J., Liao, Q.V., Eds.; Springer: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Endsley, M.R. Designing for Situation Awareness an Approach to User-Centered Design, 2nd ed.; CRC Press Inc.: Boca Raton, FL, USA, 2011. [Google Scholar]
- Gasciauskaite, G.; Lunkiewicz, J.; Roche, T.R.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Human-centered visualization technologies for patient monitoring are the future: A narrative review. Crit. Care 2023, 27, 254. [Google Scholar] [CrossRef]
- Tscholl, D.W.; Rössler, J.; Said, S.; Kaserer, A.; Spahn, D.R.; Nöthiger, C.B. Situation Awareness-Oriented Patient Monitoring with Visual Patient Technology: A Qualitative Review of the Primary Research. Sensors 2020, 20, 2112. [Google Scholar] [CrossRef] [PubMed]
- Philips. A New Way to See Your Patient’s Vitals Takes Shape. Available online: https://www.philips.co.uk/healthcare/technology/visual-patient-avatar (accessed on 23 September 2023).
- Wittgenstein, L. Tractatus Logico-Philosophicus; Routledge & Kegan Paul: London, UK, 1922. [Google Scholar]
- Degani, A.; Jorgensen, C.C.; Iverson, D.; Shafto, M.; Olson, L. On Organization of Information: Approach and Early Work; NASA Ames Research Center: Mountain View, CA, USA, 2009.
- Wetli, D.J.; Bergauer, L.; Nöthiger, C.B.; Roche, T.R.; Spahn, D.R.; Tscholl, D.W.; Said, S. Improving Visual-Patient-Avatar Design Prior to Its Clinical Release: A Mixed Qualitative and Quantitative Study. Diagnostics 2022, 12, 555. [Google Scholar] [CrossRef]
- Tscholl, D.W.; Handschin, L.; Neubauer, P.; Weiss, M.; Seifert, B.; Spahn, D.R.; Noethiger, C.B. Using an animated patient avatar to improve perception of vital sign information by an-aesthesia professionals. Br. J. Anaesth. 2018, 121, 662–671. [Google Scholar] [CrossRef]
- Roche, T.R.; Said, S.; Braun, J.; Maas, E.J.; Machado, C.; Grande, B.; Kolbe, M.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Avatar-based patient monitoring in critical anaesthesia events: A randomised high-fidelity simulation study. Br. J. Anaesth. 2021, 126, 1046–1054. [Google Scholar] [CrossRef]
- Garot, O.; Rössler, J.; Pfarr, J.; Ganter, M.T.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Avatar-based versus conventional vital sign display in a central monitor for monitoring multiple patients: A multicenter computer-based laboratory study. BMC Med. Inform. Decis. Mak. 2020, 20, 26. [Google Scholar] [CrossRef] [PubMed]
- Bergauer, L.; Braun, J.; Roche, T.R.; Meybohm, P.; Hottenrott, S.; Zacharowski, K.; Raimann, F.J.; Rivas, E.; López-Baamonde, M.; Ganter, M.T.; et al. Avatar-based patient monitoring improves information transfer, diagnostic confidence and reduces perceived workload in intensive care units: Computer-based, multicentre comparison study. Sci. Rep. 2023, 13, 5908. [Google Scholar] [CrossRef] [PubMed]
- Guetterman, T.C.; Fetters, M.D.; Creswell, J.W. Integrating Quantitative and Qualitative Results in Health Science Mixed Methods Research through Joint Displays. Ann. Fam. Med. 2015, 13, 554–561. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Viera, A.J.; Garrett, J.M. Understanding interobserver agreement: The kappa statistic. Fam. Med. 2005, 37, 360–363. [Google Scholar]
- Koch, G.G.; Landis, J.R.; Freeman, J.L.; Freeman, D.H., Jr.; Lehnen, R.G. A general methodology for the analysis of experiments with repeated measurement of cate-gorical data. Biometrics 1977, 33, 133–158. [Google Scholar] [CrossRef]
- Tscholl, D.W.; Weiss, M.; Handschin, L.; Spahn, D.R.; Nöthiger, C.B. User perceptions of avatar-based patient monitoring: A mixed qualitative and quantitative study. BMC Anesthesiol. 2018, 18, 188. [Google Scholar] [CrossRef] [PubMed]
- Rössler, J.; Kaserer, A.; Albiez, B.; Braun, J.; Breckwoldt, J.; Spahn, D.R.; Nöthiger, C.; Tscholl, D.W. Correction: Comparing Classroom Instruction to Individual Instruction as an Approach to Teach Avatar-Based Patient Monitoring with Visual Patient: Simulation Study. JMIR Med. Educ. 2020, 6, e24459. [Google Scholar] [CrossRef] [PubMed]
- Pitiriga, V.; Bakalis, J.; Theodoridou, K.; Kanellopoulos, P.; Saroglou, G.; Tsakris, A. Lower risk of bloodstream infections for peripherally inserted central catheters compared to central venous catheters in critically ill patients. Antimicrob. Resist. Infect. Control 2022, 11, 137. [Google Scholar] [CrossRef] [PubMed]
- Mimoz, O.; Moreira, R.; Frasca, D.; Boisson, M.; Dahyot-Fizelier, C. Practice assessment of central venous lines care in surgical ICU of French university hospitals. Ann. Fr. Anesth. Reanim. 2010, 29, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Carrer, S.; Bocchi, A.; Bortolotti, M.; Braga, N.; Gilli, G.; Candini, M.; Tartari, S. Effect of different sterile barrier precautions and central venous catheter dressing on the skin colonization around the insertion site. Minerva Anestesiol. 2005, 71, 197–206. [Google Scholar]
- Bacuzzi, A.; Cecchin, A.; Bosco, A.D.; Cantone, G.; Cuffari, S. Recommendations and reports about central venous catheter-related infection. Surg. Infect. 2006, 7 (Suppl. S2), S65–S67. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, F.K.; Lapkin, S.; Molloy, L.; Sim, J. Healthcare-associated infections in adult intensive care units: A multisource study examining nurses’ safety attitudes, quality of care, missed care, and nurse staffing. Intensive Crit. Care Nurs. 2023, 78, 103480. [Google Scholar] [CrossRef]
- Akbas, S.; Said, S.; Roche, T.R.; Nöthiger, C.B.; Spahn, D.R.; Tscholl, D.W.; Bergauer, L. User Perceptions of Different Vital Signs Monitor Modalities during High-Fidelity Simulation: Semiquantitative Analysis. JMIR Hum. Factors 2022, 9, e34677. [Google Scholar] [CrossRef]
- Ochieng, P.A. An Analysis of the Strengths and Limitation of Qualitative and Quantitative Research Paradigms. Probl. Educ. 21st Century 2009, 13, 13–38. [Google Scholar]

| Part I: Participant Interviews | Part II: Online Survey | |
|---|---|---|
| Period of data collection | 23 June 2021–27 August 2021 | 28 July 2021–15 October 2021 |
| Total number of participants | 50 | 40 |
| Number of nurses (%) | 25 (50%) | 21 (52.5%) |
| Number of physicians (%) | 25 (50%) | 19 (47.5%) |
| Number of female participants (%) | 19 (38%) | 17(42.5%) |
| Median (IQR) age in years | 37.0 (33.0–43.8) | 37 (32.75–42.75) |
| Median (IQR) work experience in years | 10.5 (7.2–16.8) | 10 (7–17.25) |
| Major Topic | Subtheme | Examples |
|---|---|---|
| Design positive 29 of 139 (21%) statements | Overview 14 of 139 (10%) statements | Participant #15: Better overview. Participant #30: You capture a lot of information at a glance. |
| Illustration positive 15 of 139 (11%) statements | Participant #12: Possibility to recognize the ST elevation by color. Participant #40: Situations are color-coded. | |
| Intuitive 17 of 139 (12%) statements | Participant #26: Easy understanding. Participant #42: It is much more intuitive. | |
| Time saving 16 of 139 (12%) statements | Participant #1: Deviations can be detected more quickly. Participant #8: You can quickly see if everything is okay or not okay. | |
| Installations 16 of 139 (12%) statements | Participant #10: Installations immediately clear. Participant #43: Cool for lines and devices. | |
| Design negative 40 of 139 (29%) statements | Overload 24 of 139 (17%) statements | Participant #5: Too much information in one image. Participant #38: Sometimes too confusing. |
| Illustration negative 16 of 139 (12%) statements | Participant #17: The graphics could look more professional. Participant #41: Some parameters, like arterial blood pressure are difficult to see. | |
| Unfamiliarity 16 of 139 (12%) statements | Participant #35: It takes time to get used to it. Participant #46: Training needed. | |
| Incompleteness 5 of 139 (4%) statements | Participant #20: Saturation low: how low is it? 90% or 70%? Participant #44: Omits all the information that gives us the morphology of the curves. | |
| Not codable 9 of 148 (6%) statements | Participant #1: Nothing. Participant # 23: Great, if it works. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lunkiewicz, J.; Gasciauskaite, G.; Roche, T.R.; Akbas, S.; Nöthiger, C.B.; Ganter, M.T.; Meybohm, P.; Hottenrott, S.; Zacharowski, K.; Raimann, F.J.; et al. User Perceptions of Avatar-Based Patient Monitoring for Intensive Care Units: An International Exploratory Sequential Mixed-Methods Study. Diagnostics 2023, 13, 3391. https://doi.org/10.3390/diagnostics13213391
Lunkiewicz J, Gasciauskaite G, Roche TR, Akbas S, Nöthiger CB, Ganter MT, Meybohm P, Hottenrott S, Zacharowski K, Raimann FJ, et al. User Perceptions of Avatar-Based Patient Monitoring for Intensive Care Units: An International Exploratory Sequential Mixed-Methods Study. Diagnostics. 2023; 13(21):3391. https://doi.org/10.3390/diagnostics13213391
Chicago/Turabian StyleLunkiewicz, Justyna, Greta Gasciauskaite, Tadzio Raoul Roche, Samira Akbas, Christoph B. Nöthiger, Michael T. Ganter, Patrick Meybohm, Sebastian Hottenrott, Kai Zacharowski, Florian Jürgen Raimann, and et al. 2023. "User Perceptions of Avatar-Based Patient Monitoring for Intensive Care Units: An International Exploratory Sequential Mixed-Methods Study" Diagnostics 13, no. 21: 3391. https://doi.org/10.3390/diagnostics13213391
APA StyleLunkiewicz, J., Gasciauskaite, G., Roche, T. R., Akbas, S., Nöthiger, C. B., Ganter, M. T., Meybohm, P., Hottenrott, S., Zacharowski, K., Raimann, F. J., Rivas, E., López-Baamonde, M., Beller, E. A., Tscholl, D. W., & Bergauer, L. (2023). User Perceptions of Avatar-Based Patient Monitoring for Intensive Care Units: An International Exploratory Sequential Mixed-Methods Study. Diagnostics, 13(21), 3391. https://doi.org/10.3390/diagnostics13213391









