First Molecular Characterization of Chronic Hepatitis B Carriers in Timbuktu, Mali
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects and Samples
2.2. HBV Viral Load
2.3. Serology—AgHBs, AcHBs, AcHBe, AgHBc
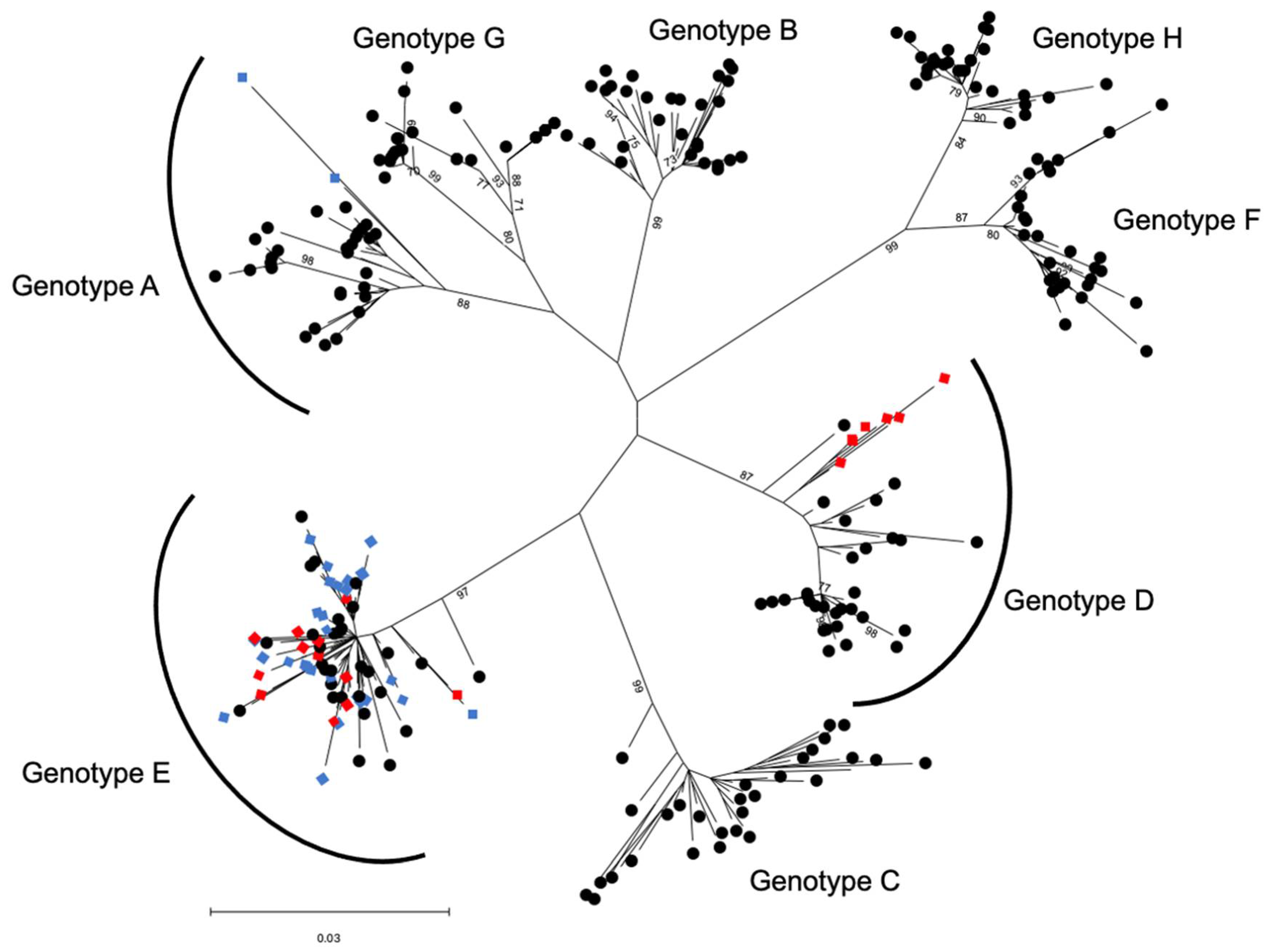
2.4. HBV Genotyping
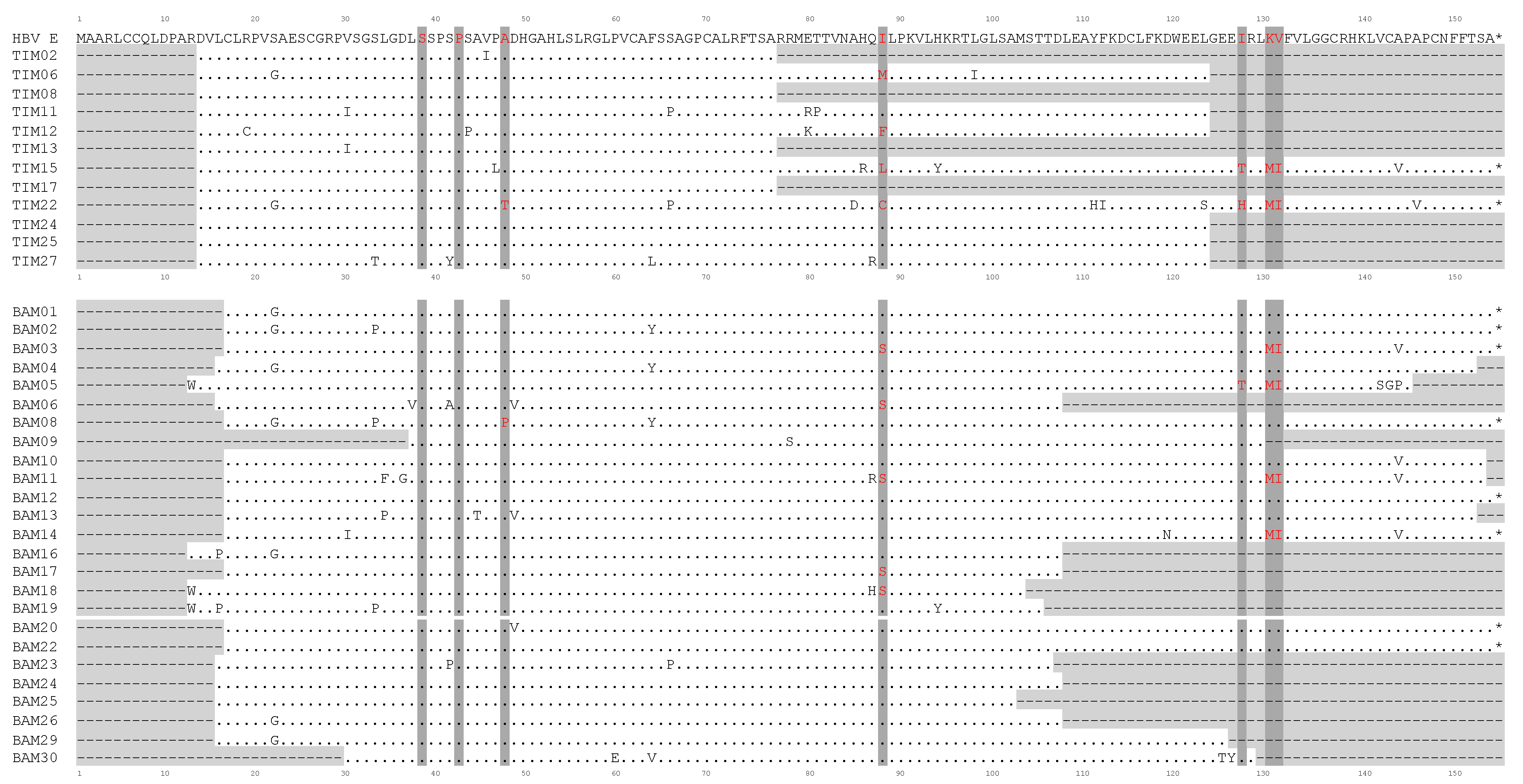
2.5. Analysis of the HBV HBx Gene Status
2.6. Phylogenetic Analysis of Viral HBS Genes
2.7. TP53 R249S Amplification, Library Construction and Deep Sequencing with Ion Torrent Proton
2.8. Bioinformatics and Statistical Analyses
3. Results
3.1. Characteristics of the Hepatitis B Carriers for Timbuktu, Mali
3.2. Serological and Viral Load Characteristics of Chronic Carriers in Timbuktu, Mali
3.3. Genotype and HBx Characteristics of HBV Chronic Carriers in Timbuktu and Bamako
3.4. Exposure to Alfatoxin in Bamako and Timbuktu
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schweitzer, A.; Horn, J.; Mikolajczyk, R.T.; Krause, G.; Ott, J.J. Estimations of Worldwide Prevalence of Chronic Hepatitis B Virus Infection: A Systematic Review of Data Published between 1965 and 2013. Lancet 2015, 386, 1546–1555. [Google Scholar] [CrossRef] [PubMed]
- Petruzziello, A. Epidemiology of Hepatitis B Virus (HBV) and Hepatitis C Virus (HCV) Related Hepatocellular Carcinoma. Open Virol. J. 2018, 12, 26–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Assih, M.; Ouattara, A.K.; Diarra, B.; Yonli, A.T.; Compaore, T.R.; Obiri-Yeboah, D.; Djigma, F.W.; Karou, S.; Simpore, J. Genetic Diversity of Hepatitis Viruses in West-African Countries from 1996 to 2018. World J. Hepatol. 2018, 10, 807–821. [Google Scholar] [CrossRef]
- Pujol, F.H.; Navas, M.-C.; Hainaut, P.; Chemin, I. Worldwide Genetic Diversity of HBV Genotypes and Risk of Hepatocellular Carcinoma. Cancer Lett. 2009, 286, 80–88. [Google Scholar] [CrossRef]
- Gouas, D.; Shi, H.; Hainaut, P. The Aflatoxin-Induced TP53 Mutation at Codon 249 (R249S): Biomarker of Exposure, Early Detection and Target for Therapy. Cancer Lett. 2009, 286, 29–37. [Google Scholar] [CrossRef]
- Szymañska, K.; Chen, J.-G.; Cui, Y.; Gong, Y.Y.; Turner, P.C.; Villar, S.; Wild, C.P.; Parkin, D.M.; Hainaut, P. TP53 R249S Mutations, Exposure to Aflatoxin, and Occurrence of Hepatocellular Carcinoma in a Cohort of Chronic Hepatitis B Virus Carriers from Qidong, China. Cancer Epidemiol. Biomark. Prev. 2009, 18, 1638–1643. [Google Scholar] [CrossRef] [Green Version]
- Szymańska, K.; Lesi, O.A.; Kirk, G.D.; Sam, O.; Taniere, P.; Scoazec, J.-Y.; Mendy, M.; Friesen, M.D.; Whittle, H.; Montesano, R.; et al. Ser-249TP53 Mutation in Tumour and Plasma DNA of Hepatocellular Carcinoma Patients from a High Incidence Area in the Gambia, West Africa. Int. J. Cancer 2004, 110, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Marchio, A.; Amougou Atsama, M.; Béré, A.; Komas, N.-P.; Noah Noah, D.; Atangana, P.J.A.; Camengo-Police, S.-M.; Njouom, R.; Bekondi, C.; Pineau, P. Droplet Digital PCR Detects High Rate of TP53 R249S Mutants in Cell-Free DNA of Middle African Patients with Hepatocellular Carcinoma. Clin. Exp. Med. 2018, 18, 421–431. [Google Scholar] [CrossRef] [Green Version]
- Thongbai, C.; Sa-nguanmoo, P.; Kranokpiruk, P.; Poovorawan, K.; Poovorawan, Y.; Tangkijvanich, P. Hepatitis B Virus Genetic Variation and TP53 R249S Mutation in Patients with Hepatocellular Carcinoma in Thailand. Asian Pac. J. Cancer Prev. 2013, 14, 3555–3559. [Google Scholar] [CrossRef] [Green Version]
- Cohen, D.; Ghosh, S.; Shimakawa, Y.; Ramou, N.; Garcia, P.S.; Dubois, A.; Guillot, C.; Kakwata-Nkor Deluce, N.; Tilloy, V.; Durand, G.; et al. Hepatitis B Virus PreS2Δ38-55 Variants: A Newly Identified Risk Factor for Hepatocellular Carcinoma. JHEP Rep. 2020, 2, 100144. [Google Scholar] [CrossRef]
- Villar, S.; Le Roux-Goglin, E.; Gouas, D.A.; Plymoth, A.; Ferro, G.; Boniol, M.; Lereau, M.; Bah, E.; Hall, A.J.; Wild, C.P.; et al. Seasonal Variation in TP53 R249S-Mutated Serum DNA with Aflatoxin Exposure and Hepatitis B Virus Infection. Environ. Health Perspect. 2011, 119, 1635–1640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Traoré, F.; Gormally, E.; Villar, S.; Friesen, M.D.; Groopman, J.D.; Vernet, G.; Diallo, S.; Hainaut, P.; Maiga, M.Y. Molecular Characteristics of Hepatitis B and Chronic Liver Disease in a Cohort of HB Carriers from Bamako, Mali. BMC Infect. Dis. 2015, 15, 180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diarra, A.; Kouriba, B.; Baby, M.; Murphy, E.; Lefrere, J.-J. HIV, HCV, HBV and Syphilis Rate of Positive Donations among Blood Donations in Mali: Lower Rates among Volunteer Blood Donors. Transfus. Clin. Biol. 2009, 16, 444–447. [Google Scholar] [CrossRef] [PubMed]
- Diarra, M.; Konate, A.; Minta, D.; Sounko, A.; Dembele, M.; Toure, C.S.; Kalle, A.; Traore, H.H.; Maiga, M.Y. Epidemiologic Aspects of Human Immunodeficiency Virus and Hepatitis Virus Infections. Mali Med. 2006, 21, 27–30. [Google Scholar] [PubMed]
- Koné, M.C.; Sidibé, E.T.; Mallé, K.K.; Beye, S.A.; Lurton, G.; Dao, S.; Diarra, M.T.; Dao, S. Seroprevalence of Human Immunodeficiency Virus, Hepatitis B Virus and Hepatitis C Virus among Blood Donors in Segou, Mali. Med. Sante Trop. 2012, 22, 97–98. [Google Scholar] [CrossRef]
- MacLean, B.; Hess, R.F.; Bonvillain, E.; Kamate, J.; Dao, D.; Cosimano, A.; Hoy, S. Seroprevalence of Hepatitis B Surface Antigen among Pregnant Women Attending the Hospital for Women & Children in Koutiala, Mali. S. Afr. Med. J. 2012, 102, 47–49. [Google Scholar]
- Maiga, M.Y.; Dembele, M.; Maiga, I.; Sanago, B.; Sangare, D.; Traoré, H.A. Case-Control Study of Hepatitis C HBs Ag and Antivirus Antibodies in Chronic Hepatopathies. Santé 2002, 12, 389–392. [Google Scholar]
- Maiga, Y.I.; Gassin, M.; Rhaly, A.A.; Pillot, J.; Marjolet, M.; Morel, D.; Dicko, K.; Dicko, I. Prevalence of Hepatitis B Virus in Women of Childbearing Age in Mali. Bull. Soc. Pathol. Exot. 1990, 83, 93–99. [Google Scholar]
- Hussein, W.M.; Anwar, W.A.; Attaleb, M.; Mazini, L.; Försti, A.; Trimbitas, R.-D.; Khyatti, M. A Review of the Infection-Associated Cancers in North African Countries. Infect. Agent Cancer 2016, 11, 35. [Google Scholar] [CrossRef] [Green Version]
- Khelifa, F.; Thibault, V. Characteristics of hepatitis B viral strains in chronic carrier patients from North-East Algeria. Pathol. Biol. 2009, 57, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Madihi, S.; Syed, H.; Lazar, F.; Zyad, A.; Benani, A. A Systematic Review of the Current Hepatitis B Viral Infection and Hepatocellular Carcinoma Situation in Mediterranean Countries. BioMed. Res. Int. 2020, 2020, 7027169. [Google Scholar] [CrossRef]
- Gourari, S.; Brichler, S.; Le Gal, F.; Abdou-Chekaraou, M.; Beloufa, M.A.; Khelifa, R.; Djaballah, H.; Boufekane, M.; Nani, A.; Afredj, N.; et al. Hepatitis B Virus and Hepatitis Delta Virus Subtypes Circulating in Algeria and Seroprevalence of HDV Infection. J. Med. Virol. 2019, 91, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Alavian, S.M.; Haghbin, H. Relative Importance of Hepatitis B and C Viruses in Hepatocellular Carcinoma in EMRO Countries and the Middle East: A Systematic Review. Hepat. Mon. 2016, 16, e35106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gouas, D.A.; Villar, S.; Ortiz-Cuaran, S.; Legros, P.; Ferro, G.; Kirk, G.D.; Lesi, O.A.; Mendy, M.; Bah, E.; Friesen, M.D.; et al. TP53 R249S Mutation, Genetic Variations in HBX and Risk of Hepatocellular Carcinoma in The Gambia. Carcinogenesis 2012, 33, 1219–1224. [Google Scholar] [CrossRef] [Green Version]
- Fang, X.; Wu, H.-H.; Ren, J.-J.; Liu, H.-Z.; Li, K.-Z.; Li, J.-L.; Tang, Y.-P.; Xiao, C.-C.; Huang, T.-R.; Deng, W. Associations between Serum HBX Quasispecies and Their Integration in Hepatocellular Carcinoma. Int. J. Clin. Exp. Pathol. 2017, 10, 11857–11866. [Google Scholar]
- Ortiz-Cuaran, S.; Villar, S.; Gouas, D.; Ferro, G.; Plymoth, A.; Khuhaprema, T.; Kalalak, A.; Sangrajrang, S.; Friesen, M.D.; Groopman, J.D.; et al. Association between HBX Status, Aflatoxin-Induced R249S TP53 Mutation and Risk of Hepatocellular Carcinoma in a Case-Control Study from Thailand. Cancer Lett. 2013, 331, 46–51. [Google Scholar] [CrossRef]
- Iavarone, M.; Trabut, J.-B.; Delpuech, O.; Carnot, F.; Colombo, M.; Kremsdorf, D.; Bréchot, C.; Thiers, V. Characterisation of Hepatitis B Virus X Protein Mutants in Tumour and Non-Tumour Liver Cells Using Laser Capture Microdissection. J. Hepatol. 2003, 39, 253–261. [Google Scholar] [CrossRef]
- Ma, N.-F.; Lau, S.H.; Hu, L.; Xie, D.; Wu, J.; Yang, J.; Wang, Y.; Wu, M.-C.; Fung, J.; Bai, X.; et al. COOH-Terminal Truncated HBV X Protein Plays Key Role in Hepatocarcinogenesis. Clin. Cancer Res. 2008, 14, 5061–5068. [Google Scholar] [CrossRef] [Green Version]
- Ali, A.; Abdel-Hafiz, H.; Suhail, M.; Al-Mars, A.; Zakaria, M.K.; Fatima, K.; Ahmad, S.; Azhar, E.; Chaudhary, A.; Qadri, I. Hepatitis B Virus, HBx Mutants and Their Role in Hepatocellular Carcinoma. World J. Gastroenterol. 2014, 20, 10238–10248. [Google Scholar] [CrossRef]
- Kim, H.; Lee, S.-A.; Kim, B.-J. X Region Mutations of Hepatitis B Virus Related to Clinical Severity. World J. Gastroenterol. 2016, 22, 5467–5478. [Google Scholar] [CrossRef] [PubMed]
- An, P.; Xu, J.; Yu, Y.; Winkler, C.A. Host and Viral Genetic Variation in HBV-Related Hepatocellular Carcinoma. Front. Genet. 2018, 9, 261. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Stecher, G.; Li, M.; Knyaz, C.; Tamura, K. MEGA X: Molecular Evolutionary Genetics Analysis across Computing Platforms. Mol. Biol. Evol. 2018, 35, 1547–1549. [Google Scholar] [CrossRef] [PubMed]
- Kidd-Ljunggren, K.; Miyakawa, Y.; Kidd, A.H. Genetic Variability in Hepatitis B Viruses. J. Gen. Virol. 2002, 83, 1267–1280. [Google Scholar] [CrossRef] [PubMed]
- Norder, H.; Couroucé, A.-M.; Coursaget, P.; Echevarria, J.M.; Lee, S.-D.; Mushahwar, I.K.; Robertson, B.H.; Locarnini, S.; Magnius, L.O. Genetic Diversity of Hepatitis B Virus Strains Derived Worldwide: Genotypes, Subgenotypes, and HBsAg Subtypes. Intervirology 2004, 47, 289–309. [Google Scholar] [CrossRef]
- Gouas, D.A.; Shi, H.; Hautefeuille, A.H.; Ortiz-Cuaran, S.L.; Legros, P.C.; Szymanska, K.J.; Galy, O.; Egevad, L.A.; Abedi-Ardekani, B.; Wiman, K.G.; et al. Effects of the TP53 p.R249S Mutant on Proliferation and Clonogenic Properties in Human Hepatocellular Carcinoma Cell Lines: Interaction with Hepatitis B Virus X Protein. Carcinogenesis 2010, 31, 1475–1482. [Google Scholar] [CrossRef] [Green Version]
- Tamura, K.; Nei, M. Estimation of the Number of Nucleotide Substitutions in the Control Region of Mitochondrial DNA in Humans and Chimpanzees. Mol. Biol. Evol. 1993, 10, 512–526. [Google Scholar]
- Stecher, G.; Tamura, K.; Kumar, S. Molecular Evolutionary Genetics Analysis (MEGA) for MacOS. Mol. Biol. Evol. 2020, 37, 1237–1239. [Google Scholar] [CrossRef]
- Jiang, P.; Chan, C.W.M.; Chan, K.C.A.; Cheng, S.H.; Wong, J.; Wong, V.W.-S.; Wong, G.L.H.; Chan, S.L.; Mok, T.S.K.; Chan, H.L.Y.; et al. Lengthening and Shortening of Plasma DNA in Hepatocellular Carcinoma Patients. Proc. Natl. Acad. Sci. USA 2015, 112, E1317–E1325. [Google Scholar] [CrossRef] [Green Version]
- Fernandez-Cuesta, L.; Perdomo, S.; Avogbe, P.H.; Leblay, N.; Delhomme, T.M.; Gaborieau, V.; Abedi-Ardekani, B.; Chanudet, E.; Olivier, M.; Zaridze, D.; et al. Identification of Circulating Tumor DNA for the Early Detection of Small-Cell Lung Cancer. EBioMedicine 2016, 10, 117–123. [Google Scholar] [CrossRef] [Green Version]
- Le Calvez-Kelm, F.; Foll, M.; Wozniak, M.B.; Delhomme, T.M.; Durand, G.; Chopard, P.; Pertesi, M.; Fabianova, E.; Adamcakova, Z.; Holcatova, I.; et al. KRAS Mutations in Blood Circulating Cell-Free DNA: A Pancreatic Cancer Case-Control. Oncotarget 2016, 7, 78827–78840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perdomo, S.; Avogbe, P.H.; Foll, M.; Abedi-Ardekani, B.; Facciolla, V.L.; Anantharaman, D.; Chopard, P.; Calvez-Kelm, F.L.; Vilensky, M.; Polesel, J.; et al. Circulating Tumor DNA Detection in Head and Neck Cancer: Evaluation of Two Different Detection Approaches. Oncotarget 2017, 8, 72621–72632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delhomme, T.M.; Avogbe, P.H.; Gabriel, A.A.G.; Alcala, N.; Leblay, N.; Voegele, C.; Vallée, M.; Chopard, P.; Chabrier, A.; Abedi-Ardekani, B.; et al. Needlestack: An Ultra-Sensitive Variant Caller for Multi-Sample next Generation Sequencing Data. NAR Genom. Bioinform. 2020, 2, a021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aeberhard, W.H.; Cantoni, E.; Heritier, S. Robust Inference in the Negative Binomial Regression Model with an Application to Falls Data. Biometrics 2014, 70, 920–931. [Google Scholar] [CrossRef]
- Hübschen, J.M.; Andernach, I.E.; Muller, C.P. Hepatitis B Virus Genotype E Variability in Africa. J. Clin. Virol. 2008, 43, 376–380. [Google Scholar] [CrossRef]
- Toyé, R.M.; Cohen, D.; Pujol, F.H.; Sow-Sall, A.; Lô, G.; Hoshino, K.; Mizokami, M.; Zoulim, F.; Lemoine, M.; Touré-Kane, C.; et al. Hepatitis B Virus Genotype Study in West Africa Reveals an Expanding Clade of Subgenotype A4. Microorganisms 2021, 9, 623. [Google Scholar] [CrossRef]
- Kramvis, A.; Kew, M.C. Epidemiology of Hepatitis B Virus in Africa, Its Genotypes and Clinical Associations of Genotypes. Hepatol. Res. 2007, 37, S9–S19. [Google Scholar] [CrossRef]
- Kramvis, A. Molecular Characteristics and Clinical Relevance of African Genotypes and Subgenotypes of Hepatitis B Virus. S. Afr. Med. J. 2018, 108, 17–21. [Google Scholar] [CrossRef]
- Ingasia, L.A.O.; Wose Kinge, C.; Kramvis, A. Genotype E: The Neglected Genotype of Hepatitis B Virus. World J. Hepatol. 2021, 13, 1875–1891. [Google Scholar] [CrossRef]
- Al-Qahtani, A.A.; Al-Anazi, M.R.; Nazir, N.; Ghai, R.; Abdo, A.A.; Sanai, F.M.; Al-Hamoudi, W.K.; Alswat, K.A.; Al-Ashgar, H.I.; Khan, M.Q.; et al. Hepatitis B Virus (HBV) X Gene Mutations and Their Association with Liver Disease Progression in HBV-Infected Patients. Oncotarget 2017, 8, 105115–105125. [Google Scholar] [CrossRef] [Green Version]
- Pandey, M.K.; Kumar, R.; Pandey, A.K.; Soni, P.; Gangurde, S.S.; Sudini, H.K.; Fountain, J.C.; Liao, B.; Desmae, H.; Okori, P.; et al. Mitigating Aflatoxin Contamination in Groundnut through A Combination of Genetic Resistance and Post-Harvest Management Practices. Toxins 2019, 11, 315. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Participants in Timbuktu | Percentage (%) | Participants in Bamako | Percentage (%) |
|---|---|---|---|---|
| Age group | ||||
| 18–29 | 15 | 50 | 13 | 43 |
| 30–39 | 3 | 10 | 14 | 47 |
| 40–49 | 10 | 33.3 | 3 | 10 |
| 50–59 | 2 | 6.7 | 0 | 0 |
| Gender | ||||
| Male | 24 | 80 | 30 | 100 |
| Female | 5 | 20 | 0 | 0 |
| Occupation | ||||
| Employee (private or civil) | 10 | 33.3 | UN | UN |
| Student | 9 | 30 | UN | UN |
| Trader | 6 | 20 | UN | UN |
| Farmer | 4 | 13.3 | UN | UN |
| Housewife | 1 | 3.3 | UN | UN |
| Timbuktu | Bamako | |||
|---|---|---|---|---|
| Parameters | Number (Total 30 Samples) | Percentage (%) | Number (Total 30 Samples) | Percentage (%) |
| Serology | ||||
| AgHBs Timbuktu | ||||
| Positive | 29 | 96.7 | NR | NR |
| Negative | 0 | 0 | NR | NR |
| Unknown | 1 | 3.3 | NR | NR |
| AgHBs Centre d’Infectiologie Charles Mérieux | ||||
| Positive | 29 | 96.7 | 30 | 100 |
| Negative | 1 | 3.3 | 0 | 0 |
| AcHBs | ||||
| Positive | 2 | 6.7 | 3 | 10 |
| Negative | 28 | 93.3 | 27 | 90 |
| AgHBe | ||||
| Positive | 0 | 0 | 15 | 50 |
| Negative | 30 | 100 | 15 | 50 |
| AcHBe | ||||
| Positive | 29 | 96.7 | NT | NT |
| Negative | 1 | 3.3 | NT | NT |
| AcHBc | ||||
| Positive | 3 | 10 | 2 | 6.7 |
| Negative | 27 | 90 | 28 | 93.3 |
| Viral load | ||||
| Undetectable | 20 | 66.7 | 0 | 0 |
| Between 2000 and 20,000 UI/ml | 1 | 3.3 | 1 | 3.3 |
| >20,000 UI/ml | 9 | 30 | 29 | 96.7 |
| Genotyping of HBV | ||||
| Genotype E | 13 | 44.8 | 28 | 93.3 |
| Genotype D | 7 | 24.1 | 0 | 0 |
| Genotype A | 0 | 0 | 2 | 6.7 |
| Could not be determined | 9 | 31.1 | 0 | 0 |
| HBx status | ||||
| Full length HBx | 2 | 3.4 | 14 | 43.3 |
| Truncated HBx | 13 | 51.7 | 13 | 50 |
| No amplification product (failure of PCR/deletion of HBx) | 14 | 41.4 | 3 | 6.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lawrence, P.; Chabane, M.; Abrouk, L.; Thiesson, A.; Berthé, D.; Diarra, A.B.; Bengaly, K.; Traoré, B.; Kassogué, D.; Durand, G.; et al. First Molecular Characterization of Chronic Hepatitis B Carriers in Timbuktu, Mali. Diagnostics 2023, 13, 375. https://doi.org/10.3390/diagnostics13030375
Lawrence P, Chabane M, Abrouk L, Thiesson A, Berthé D, Diarra AB, Bengaly K, Traoré B, Kassogué D, Durand G, et al. First Molecular Characterization of Chronic Hepatitis B Carriers in Timbuktu, Mali. Diagnostics. 2023; 13(3):375. https://doi.org/10.3390/diagnostics13030375
Chicago/Turabian StyleLawrence, Philip, Mawlouda Chabane, Lucie Abrouk, Adrien Thiesson, Diakaridia Berthé, Amadou B. Diarra, Karim Bengaly, Brehima Traoré, Djibril Kassogué, Geoffroy Durand, and et al. 2023. "First Molecular Characterization of Chronic Hepatitis B Carriers in Timbuktu, Mali" Diagnostics 13, no. 3: 375. https://doi.org/10.3390/diagnostics13030375








