Analysis of PTPN22 −1123 G>C, +788 G>A and +1858 C>T Polymorphisms in Patients with Primary Sjögren’s Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Healthy Controls
2.2. Genotyping of rs2488457 −1123 G>C, rs33996649 +788 G>A and rs2476601 +1858 C>T Polymorphisms
2.3. RNA Extraction and Reverse Transcription
2.4. Quantitative PCR (qPCR)
2.5. Anti-SSA/Ro and Anti-SSB/La Serum Level Determination
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics
3.2. Genotype Distribution of PTPN22 rs2488457 (−1123 G>C), rs33996649 (+788 G>A), and rs2476601 (+1858 C>T) Polymorphisms
3.3. PTPN22 rs2488457 (−1123 G>C), rs33996649 (+788 G>A), and rs2476601 (+1858 C>T) Haplotypes
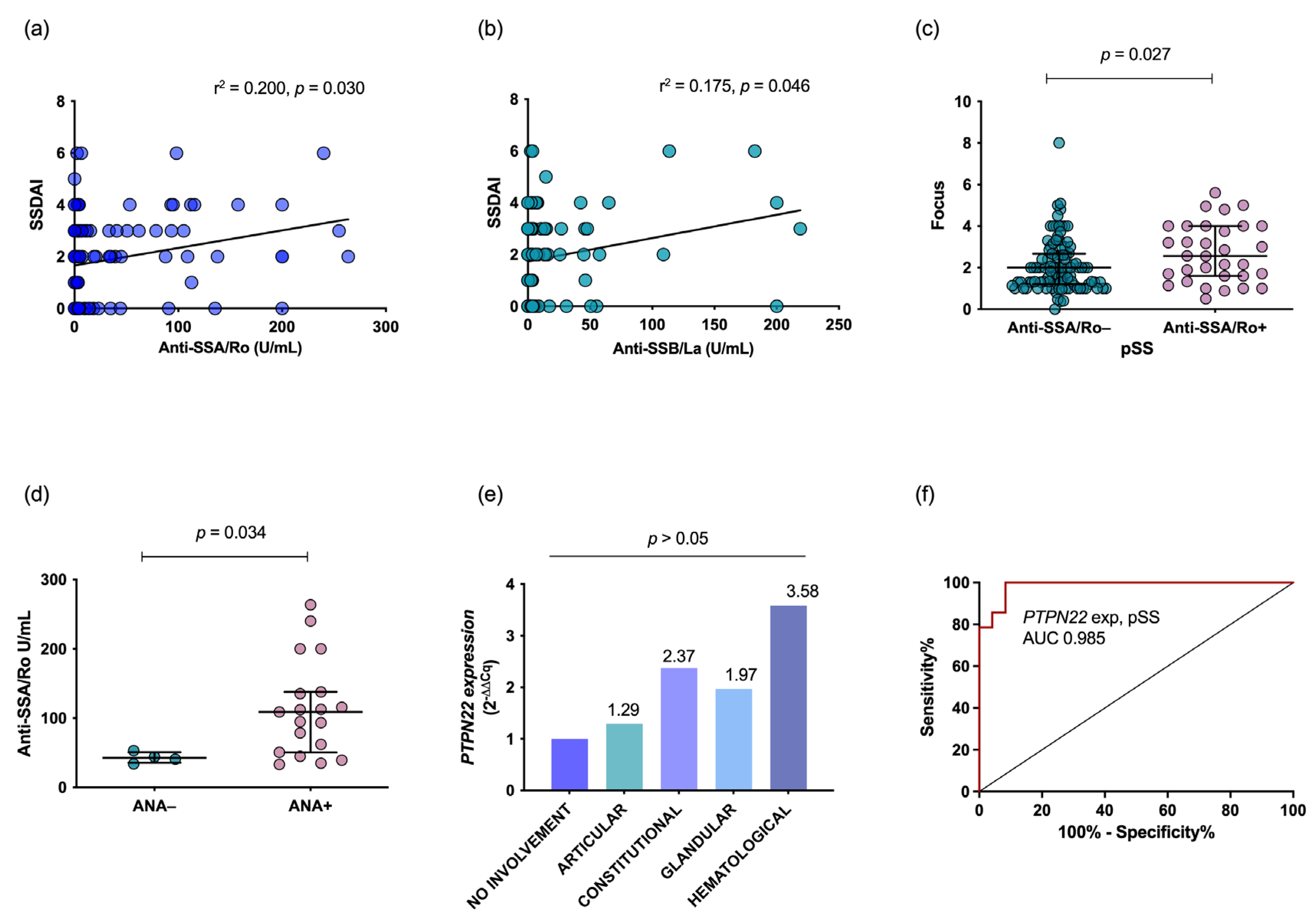
3.4. PTPN22 mRNA Expression and Clinical Association
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brito-Zerón, P.; Baldini, C.; Bootsma, H.; Bowman, S.J.; Jonsson, R.; Mariette, X.; Sivils, K.; Theander, E.; Tzioufas, A.; Ramos-Casals, M. Sjögren syndrome. Nat. Rev. Dis. Prim. 2016, 2, 16047. [Google Scholar] [CrossRef] [PubMed]
- Agmon-Levin, N.; Lian, Z.; Shoenfeld, Y. Explosion of autoimmune diseases and the mosaic of old and novel factors. Cell. Mol. Immunol. 2011, 8, 189–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitsias, D.I.; Kapsogeorgou, E.K.; Moutsopoulos, H.M. Sjögren’s syndrome: Why autoimmune epithelitis? Oral Dis. 2006, 12, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Bottini, N.; Musumeci, L.; Alonso, A.; Rahmouni, S.; Nika, K.; Rostamkhani, M.; MacMurray, J.; Meloni, G.F.; Lucarelli, P.; Pellecchia, M.; et al. A functional variant of lymphoid tyrosine phosphatase is associated with type I diabetes. Nat. Genet. 2004, 36, 337–338. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Deshpande, P.; Pryshchep, S.; Colmegna, I.; Liarski, V.; Weyand, C.M.; Goronzy, J.J. ERK-Dependent T Cell Receptor Threshold Calibration in Rheumatoid Arthritis. J. Immunol. 2009, 183, 8258–8267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.-S.; Korman, B.; Le, J.M.; Kastner, D.L.; Remmers, E.F.; Gregersen, P.K.; Bae, S.-C. Genetic risk factors for rheumatoid arthritis differ in caucasian and Korean populations. Arthritis Rheum. 2009, 60, 364–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stanford, S.M.; Bottini, N. PTPN22: The archetypal non-HLA autoimmunity gene. Nat. Rev. Rheumatol. 2014, 10, 602–611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, S.A.; Criswell, L.A. PTPN22: Its role in SLE and autoimmunity. Autoimmunity 2007, 40, 582–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burn, G.L.; Svensson, L.; Sanchez-Blanco, C.; Saini, M.; Cope, A.P. Why is PTPN22 a good candidate susceptibility gene for autoimmune disease? FEBS Lett. 2011, 585, 3689–3698. [Google Scholar] [CrossRef] [Green Version]
- Kawasaki, E.; Awata, T.; Ikegami, H.; Kobayashi, T.; Maruyama, T.; Nakanishi, K.; Shimada, A.; Uga, M.; Kurihara, S.; Kawabata, Y.; et al. Systematic search for single nucleotide polymorphisms in a lymphoid tyrosine phosphatase gene (PTPN22): Association between a promoter polymorphism and type 1 diabetes in Asian populations. Am. J. Med. Genet. Part A 2006, 140, 586–593. [Google Scholar] [CrossRef]
- Huang, J.-J.; Qiu, Y.-R.; Li, H.-X.; Sun, D.-H.; Yang, J.; Yang, C.-L. A PTPN22 promoter polymorphism −1123G>C is associated with RA pathogenesis in Chinese. Rheumatol. Int. 2012, 32, 767–771. [Google Scholar] [CrossRef]
- Liu, F.; Liu, J.; Zheng, T.-S.; Li, Q.; Wang, C.; Pan, X.-P.; Lu, H.; Zhao, Y.-W. The −1123G>C Variant of PTPN22 Gene Promoter is Associated with Latent Autoimmune Diabetes in Adult Chinese Hans. Cell Biochem. Biophys. 2012, 62, 273–279. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, H.; Xia, B.; Wang, P.; Jiang, T.; Song, M.; Wu, J. Association of PTPN22 gene (rs2488457) polymorphism with ulcerative colitis and high levels of PTPN22 mRNA in ulcerative colitis. Int. J. Color. Dis. 2013, 28, 1351–1358. [Google Scholar] [CrossRef]
- Machado-Contreras, J.R.; Muñoz-Valle, J.F.; Cruz, A.; Salazar-Camarena, D.C.; Marín-Rosales, M.; Palafox-Sánchez, C.A. Distribution of PTPN22 polymorphisms in SLE from western Mexico: Correlation with mRNA expression and disease activity. Clin. Exp. Med. 2016, 16, 399–406. [Google Scholar] [CrossRef]
- Muñoz-Valle, J.F.; Padilla-Gutiérrez, J.R.; Hernández-Bello, J.; Ruiz-Noa, Y.; Valle, Y.; Palafox-Sánchez, C.A.; Parra-Rojas, I.; Gutiérrez-Ureña, S.R.; Rangel-Villalobos, H. Polimorfismo −1123G>C en el gen PTPN22 y anticuerpos antipéptido citrulinado cíclico en la artritis reumatoide. Med. Clin. 2017, 149, 95–100. [Google Scholar] [CrossRef]
- Orrù, V.; Tsai, S.J.; Rueda, B.; Fiorillo, E.; Stanford, S.M.; Dasgupta, J.; Hartiala, J.; Zhao, L.; Ortego-Centeno, N.; D’Alfonso, S.; et al. A loss-of-function variant of PTPN22 is associated with reduced risk of systemic lupus erythematosus. Hum. Mol. Genet. 2009, 18, 569–579. [Google Scholar] [CrossRef]
- López-Cano, D.J.; Cadena-Sandoval, D.; Beltrán-Ramírez, O.; Barbosa-Cobos, R.E.; Sánchez-Muñoz, F.; Amezcua-Guerra, L.M.; Juárez-Vicuña, Y.; Aguilera-Cartas, M.C.; Moreno, J.; Bautista-Olvera, J.; et al. The PTPN22 R263Q polymorphism confers protection against systemic lupus erythematosus and rheumatoid arthritis, while PTPN22 R620W confers susceptibility to Graves’ disease in a Mexican population. Inflamm. Res. 2017, 66, 775–781. [Google Scholar] [CrossRef]
- Kyogoku, C.; Langefeld, C.D.; Ortmann, W.A.; Lee, A.; Selby, S.; Carlton, V.E.H.; Chang, M.; Ramos, P.; Baechler, E.C.; Batliwalla, F.M.; et al. Genetic Association of the R620W Polymorphism of Protein Tyrosine Phosphatase PTPN22 with Human SLE. Am. J. Hum. Genet. 2004, 75, 504–507. [Google Scholar] [CrossRef] [Green Version]
- Torres-Carrillo, N.M.; Ruiz-Noa, Y.; Martínez-Bonilla, G.E.; Leyva-Torres, S.D.; Torres-Carrillo, N.; Palafox-Sánchez, C.A.; Navarro-Hernández, R.E.; Rangel-Villalobos, H.; Oregón-Romero, E.; Muñoz-Valle, J.F. The +1858C/T PTPN22 gene polymorphism confers genetic susceptibility to rheumatoid arthritis in Mexican population from the Western Mexico. Immunol. Lett. 2012, 147, 41–46. [Google Scholar] [CrossRef]
- Gomez, L.M.; Anaya, J.-M.; Gonzalez, C.I.; Pineda-Tamayo, R.; Otero, W.; Arango, A.; Martín, J. PTPN22 C1858T polymorphism in Colombian patients with autoimmune diseases. Genes Immun. 2005, 6, 628–631. [Google Scholar] [CrossRef] [Green Version]
- Shiboski, C.H.; Shiboski, S.C.; Seror, R.; Criswell, L.A.; Labetoulle, M.; Lietman, T.M.; Rasmussen, A.; Scofield, H.; Vitali, C.; Bowman, S.J.; et al. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren’s Syndrome: A Consensus and Data-Driven Methodology Involving Three International Patient Cohorts. Arthritis Rheum. 2017, 76, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Gorodezky, C.; Alaez, C.; Vázquez-García, M.N.; de la Rosa, G.; Infante, E.; Balladares, S.; Toribio, R.; Pérez-Luque, E.; Muñoz, L. The Genetic structure of Mexican Mestizos of different locations: Tracking back their origins through MHC genes, blood group systems, and microsatellites. Hum. Immunol. 2001, 62, 979–991. [Google Scholar] [CrossRef] [PubMed]
- Vitali, C.; Palombi, G.; Baldini, C.; Benucci, M.; Bombardieri, S.; Covelli, M.; Del Papa, N.; De Vita, S.; Epis, O.; Franceschini, F.; et al. Sjögren’s syndrome disease damage index and disease activity index: Scoring systems for the assessment of disease damage and disease activity in Sjögren’s syndrome, derived from an analysis of a cohort of Italian patients. Arthritis Rheum. 2007, 56, 2223–2231. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.A.; Dykes, D.D.; Polesky, H.F. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988, 16, 55404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padilla-Gutiérrez, J.R.; Valle, Y.; Mercado, M.V.-D.; Maldonado, M.; Muñoz-Valle, J.F. A new PCR-RFLP assay for –1123 G>C polymorphism in the PTPN22 gene: Allele and genotype frequencies in a western Mexican population. Clin. Chem. Lab. Med. 2009, 47, 491–493. [Google Scholar] [CrossRef]
- Chomczynski, P.; Sacchi, N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal. Biochem. 1987, 162, 156–159. [Google Scholar] [CrossRef]
- Bustin, S.A.; Benes, V.; Garson, J.A.; Hellemans, J.; Huggett, J.; Kubista, M.; Mueller, R.; Nolan, T.; Pfaffl, M.W.; Shipley, G.L.; et al. The MIQE Guidelines: Minimum Information for Publication of Quantitative Real-Time PCR Experiments. Clin. Chem. 2009, 55, 611–622. [Google Scholar] [CrossRef] [Green Version]
- Huggett, J.F.; Dheda, K.; Bustin, S.; Zumla, A. Real-time RT-PCR normalisation; strategies and considerations. Genes Immun. 2005, 6, 279–284. [Google Scholar] [CrossRef] [Green Version]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef]
- Yong, Y.; He, L. SHEsis, a powerful software platform for analyses of linkage disequilibrium, haplotype construction, and genetic association at polymorphism loci. Cell Res. 2005, 15, 97–98. [Google Scholar] [CrossRef] [Green Version]
- Notarangelo, L.D. Immunodeficiency and immune dysregulation associated with proximal defects of T cell receptor signaling. Curr. Opin. Immunol. 2014, 31, 97–101. [Google Scholar] [CrossRef] [Green Version]
- Mustelin, T.; Bottini, N.; Stanford, S.M. The Contribution of PTPN22 to Rheumatic Disease. Arthritis Rheumatol. 2019, 71, 486–495. [Google Scholar] [CrossRef]
- Diaz-Gallo, L.M.; Espino-Paisán, L.; Fransen, K.; Gómez-García, M.; Van Sommeren, S.; Cardeña, C.; Rodrigo, L.; Mendoza, J.L.; Taxonera, C.; Martin, J.; et al. Differential association of two PTPN22 coding variants with Crohn’s disease and ulcerative colitis. J. Transl. Med. 2010, 8, 1–2. [Google Scholar] [CrossRef] [Green Version]
- Ramírez-Pérez, S.; Sánchez-Zuno, G.A.; Chavarría-Buenrostro, L.E.; Montoya-Buelna, M.; Reyes-Pérez, I.V.; Ramírez-Dueñas, M.G.; Palafox-Sánchez, C.A.; Martínez-Bonilla, G.E.; Muñoz-Valle, J.F. PTPN22 +788 G>A (R263Q) Polymorphism is Associated with mRNA Expression but it is not a Susceptibility Marker for Rheumatoid Arthritis Patients from Western Mexico. Biochem. Genet. 2019, 57, 455–465. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, L.; Taib, W.R.W.; Topless, R.; Steer, S.; González-Escribano, M.F.; Balsa, A.; Pascual-Salcedo, D.; González-Gay, M.A.; Raya, E.; Fernandez-Gutierrez, B.; et al. The PTPN22 R263Q polymorphism is a risk factor for rheumatoid arthritis in Caucasian case-control samples. Arthritis Rheum. 2011, 63, 365–372. [Google Scholar] [CrossRef]
- Martínez-Cortés, G.; Salazar-Flores, J.; Haro-Guerrero, J.; Rubi-Castellanos, R.; Velarde-Félix, J.S.; Muñoz-Valle, J.F.; López-Casamichana, M.; Carrillo-Tapia, E.; Canseco-Avila, L.M.; Bravi, C.M.; et al. Maternal admixture and population structure in Mexican-Mestizos based on mtDNA haplogroups. Am. J. Phys. Anthropol. 2013, 151, 526–537. [Google Scholar] [CrossRef]
- Rangel-Villalobos, H.; Salazar-Flores, J.; Dondiego, R.; Anaya-Palafox, M.; Nuño-Arana, I.; Canseco-Ávila, L.; Flores-Flores, G.; Romero-Rentería, O.; Morales-Vallejo, M.; Muñoz-Valle, J.; et al. “South to North increasing gradient of paternal European ancestry throughout the Mexican territory: Evidence of Y-linked short tandem repeats”. Forensic Sci. Int. Genet. Suppl. Ser. 2009, 2, 448–450. [Google Scholar] [CrossRef]
- rs114764573 (SNP)—Population Genetics—Ensembl Genome Browser 107. Available online: https://www.ensembl.org/Homo_sapiens/Variation/Population?db=core;r=5:176529260-176530260;v=rs114764573;vdb=variation;vf=193970798 (accessed on 14 September 2022).
- Rincón, J.F.M.; Cano, D.L.; Morales, S.J.; Jiménez, M.L.R.; Cobos, R.E.B.; Bello, J.R. The functional PTPN22 C1858T polymorphism confers risk for rheumatoid arthritis in patients from Central Mexico. Clin. Rheumatol. 2016, 35, 1457–1462. [Google Scholar] [CrossRef]
- Viken, M.K.; Olsson, M.; Flåm, S.T.; Førre, Ø.; Kvien, T.K.; Thorsby, E.; Lie, B.A. The PTPN22 promoter polymorphism –1123G>C association cannot be distinguished from the 1858C>T association in a Norwegian rheumatoid arthritis material. Tissue Antigens 2007, 70, 190–197. [Google Scholar] [CrossRef]
- Cohen, S.; Dadi, H.; Shaoul, E.; Sharfe, N.; Roifman, C.M. Cloning and Characterization of a Lymphoid-Specific, Inducible Human Protein Tyrosine Phosphatase, Lyp. Blood 1999, 93, 2013–2024. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-H.; Tai, T.-S.; Lu, B.; Iannaccone, C.; Cernadas, M.; Weinblatt, M.; Shadick, N.; Miaw, S.-C.; Ho, I.-C. PTPN22.6, a Dominant Negative Isoform of PTPN22 and Potential Biomarker of Rheumatoid Arthritis. PLoS ONE 2012, 7, e33067. [Google Scholar] [CrossRef] [PubMed]
- Maine, C.J.; Marquardt, K.; Cheung, J.; Sherman, L.A. PTPN22 Controls the Germinal Center by Influencing the Numbers and Activity of T Follicular Helper Cells. J. Immunol. 2014, 192, 1415–1424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katakura, K.; Lee, J.; Rachmilewitz, D.; Li, G.; Eckmann, L.; Raz, E. Toll-like receptor 9–induced type I IFN protects mice from experimental colitis. J. Clin. Investig. 2005, 115, 695–702. [Google Scholar] [CrossRef] [Green Version]
- Baldini, C.; Ferro, F.; Elefante, E.; Bombardieri, S. Biomarkers for Sjögren’s syndrome. Biomark. Med. 2018, 12, 275–286. [Google Scholar] [CrossRef]
- Shiboski, S.C.; Shiboski, C.H.; Criswell, L.A.; Baer, A.N.; Challacombe, S.; Lanfranchi, H.; Schiodt, M.; Umehara, H.; Vivino, F.; Zhao, Y.; et al. American College of Rheumatology classification criteria for Sjögren’s syndrome: A data-driven, expert consensus approach in the Sjögren’s International Collaborative Clinical Alliance Cohort. Arthritis Care Res. 2012, 64, 475–487. [Google Scholar] [CrossRef]

| SNP | Primer | Sequence | Enzyme | Products/Genotype |
|---|---|---|---|---|
| rs2488457 (−1123 G>C) | Forward | 5′-CCA TTG AGA GGT TAT GCG AGCT-3′ | SacI | 205 pb, G/G 205, 183 and 22pb, G/C 183 and 22pb, C/C |
| Reverse | 5′-CAA CCA CCT TGC TGA CAA CAT TG-3′ | |||
| rs33996649 (+788 G>A) | Forward | 5′-GAT GGA GCA AGA CTC AGA CAC-3′ | MspI | 234 pb A/A 234, 91 and 143 pb, G/A 91, 143pb G/G |
| Reverse | 5′-CCC CAT GTT AGA AGA GCA GAT-3 | |||
| rs2476601 (+1858 C>T) | Forward | 5′ ATTTGCTTCAACGG AATTT-3′ | XcmI | 412 pb, C/C 412, 246 and 166bp, C/T 246 and 166 pb, T/T |
| Reverse | 5′-CAT GCT GCT ATT GCT CTG CT-3′ |
| pSS (n = 150) | |
|---|---|
| Characteristics | |
| Gender, Female/Male | 150/0 |
| Age, years a | 55 (±10) |
| Disease duration, years b | 2.3 (1–5.5) |
| Inflammation markers | |
| ESR, mm/h a | 25 (±16) |
| CRP, mg/dL a | 5.04 (±4.6) |
| Antibodies | |
| Anti-Ro+, IU/mL, n (%) | 35/127 (23.3) |
| Anti-La+, IU/mL, n (%) | 20/127 (13) |
| Glandular tests | |
| Schirmer test positive, n (%) | 120 (80) |
| MSG biopsy, focus ≥ 1, n (%) | 143 (98) |
| Focus score a | 2.3 (±1.7) |
| Clinical domains c | |
| Constitutional, n (%) | 81 (54) |
| Glandular, n (%) | 12 (8) |
| Articular, n (%) | 62 (41.3) |
| Hematologic, n (%) | 9 (6) |
| Vascular, n (%) | 3 (2) |
| Sjögren’s syndrome indices | |
| SSDDI a | 1 (±1) |
| SSDAI a | 3 (±1) |
| Treatments | |
| Prednisone, n (%) | 14 (10) |
| Azathioprine, n (%) | 24 (17) |
| Methotrexate, n (%) | 39 (27) |
| Antimalarials, n (%) | 76 (57) |
| SNP | pSS n = 150 (%) | HC n = 180 (%) | p Value | Pc Value | OR (CI 95%) |
|---|---|---|---|---|---|
| rs2488457 (−1123 G>C) | |||||
| Genotype | |||||
| GG | 78 (52) | 94 (52.2) | 1 | 1 | - |
| GC | 61 (40.7) | 72 (40) | 0.864 | 1 | 0.927 (0.406–2.211) |
| CC | 11 (7.3) | 14 (7.8) | 0.899 | 1 | 0.947 (0.426–2.189) |
| Allele | |||||
| G | 217 (72.3) | 260 (72.2) | 1 | - | - |
| C | 83 (27.7) | 100 (27.8) | 0.974 | - | 0.995 (0.708–1.399) |
| rs33996649 (+788 G>A) | |||||
| Genotype | |||||
| GG | 145 (96.6) | 177 (98.3) | 1 | 1 | - |
| GA | 4 (2.7) | 3 (1.7) | 0.706 * | 1 | 1.628 (0.432–6.534) |
| AA | 1 (0.7) | 0 | 0.452 * | 0.904 | - |
| Allele | |||||
| G | 296 (98.7) | 357 (99.2) | 1 | - | - |
| A | 4 (1.3) | 3 (0.8) | 0.708 * | - | 1.608 (0.429–6.420) |
| rs2476601 (+1858 C>T) | |||||
| Genotype | |||||
| CC | 147 (98) | 178 (98.9) | 1 | 1 | - |
| CT | 2 (1.3) | 2 (1.1) | 0.849 * | 1 | 1.211 (0.188–7.801) |
| TT | 1 (0.7) | 0 | 0.272 * | 0.544 | - |
| Allele | |||||
| C | 296 (98.7) | 358 (99.4) | 1 | - | - |
| T | 4 (1.3) | 2 (0.6) | 0.295 * | - | 2.419 (0.556–12.78) |
| Haplotypes | |||||
| GGC | 212.01 (70.7) | 255.44 (71) | 1 | - | - |
| CGC | 78.99 (26.3) | 99.56 (27.7) | 0.773 | - | 0.950 (0.670–1.338) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menchaca-Tapia, P.A.; Marín-Rosales, M.; Salazar-Camarena, D.C.; Cruz, A.; Oregon-Romero, E.; Tapia-Llanos, R.; Muñoz-Valle, J.F.; Palafox-Sánchez, C.A. Analysis of PTPN22 −1123 G>C, +788 G>A and +1858 C>T Polymorphisms in Patients with Primary Sjögren’s Syndrome. Diagnostics 2023, 13, 899. https://doi.org/10.3390/diagnostics13050899
Menchaca-Tapia PA, Marín-Rosales M, Salazar-Camarena DC, Cruz A, Oregon-Romero E, Tapia-Llanos R, Muñoz-Valle JF, Palafox-Sánchez CA. Analysis of PTPN22 −1123 G>C, +788 G>A and +1858 C>T Polymorphisms in Patients with Primary Sjögren’s Syndrome. Diagnostics. 2023; 13(5):899. https://doi.org/10.3390/diagnostics13050899
Chicago/Turabian StyleMenchaca-Tapia, Paula Annahi, Miguel Marín-Rosales, Diana Celeste Salazar-Camarena, Alvaro Cruz, Edith Oregon-Romero, Raziel Tapia-Llanos, José Francisco Muñoz-Valle, and Claudia Azucena Palafox-Sánchez. 2023. "Analysis of PTPN22 −1123 G>C, +788 G>A and +1858 C>T Polymorphisms in Patients with Primary Sjögren’s Syndrome" Diagnostics 13, no. 5: 899. https://doi.org/10.3390/diagnostics13050899







