Reliability Analysis of Vertebral Landmark Labelling on Lumbar Spine X-ray Images
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Ethics Approval
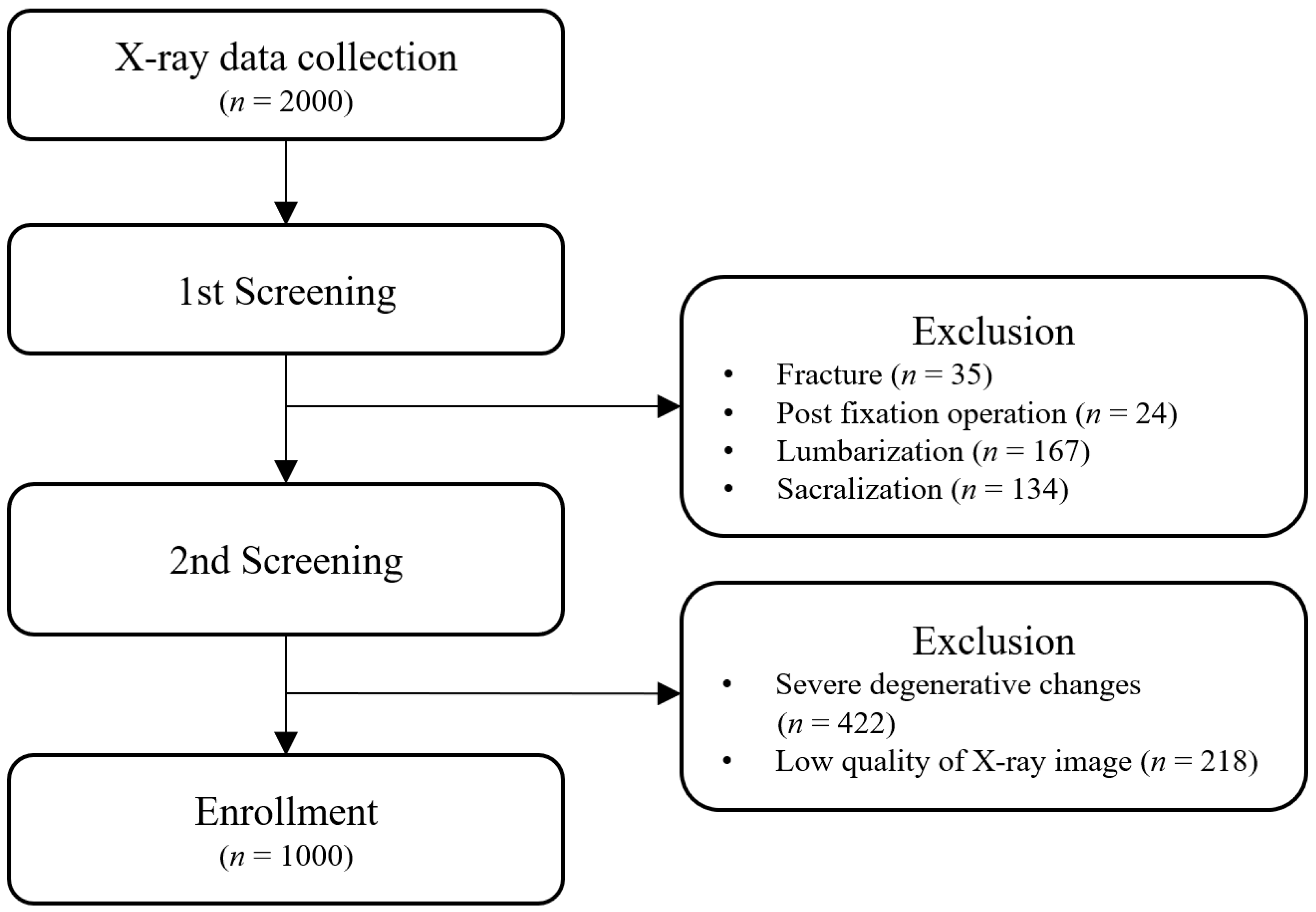
2.2. Inclusion and Exclusion Criteria of X-ray Images in the Study
2.2.1. Inclusion Criteria
- (a)
- Male or female sex and age 18–80 years;
- (b)
- L-spine X-ray performed at the Neurosurgery of Catholic Kwandong University International St. Mary’s Hospital from February 2014 to May 2019.
2.2.2. Exclusion Criteria
- (a)
- History of lumbar surgery for inducing structural changes in the lumbar vertebrae (e.g., fracture and screw fixation);
- (b)
- Severe lumbar degenerative changes or structural abnormalities of the lumbar spine;
- (c)
- Low quality of X-ray image, which was considered unsuitable for labelling.
2.3. Rater Groups for Landmark Labelling
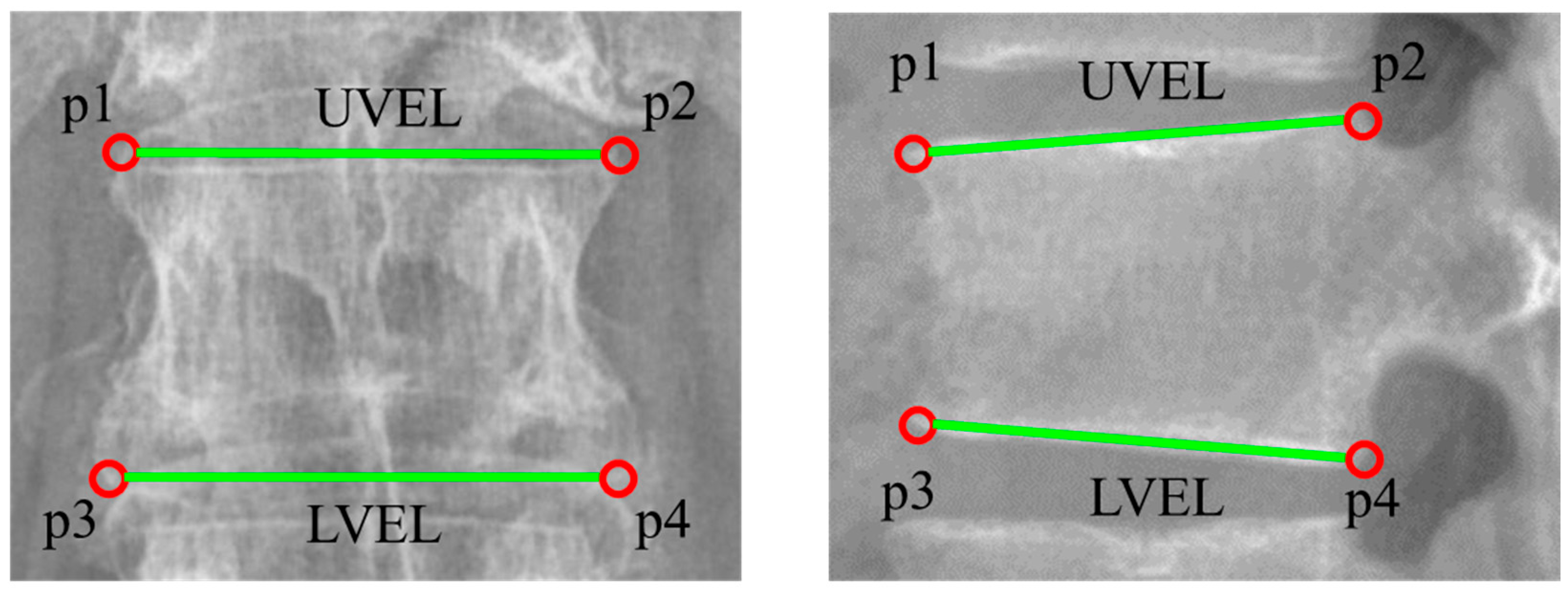
2.4. SOP for Landmark Labelling
- (a)
- The UVEL and LVEL must be parallel to the upper and lower vertebral endplates, respectively.
- (b)
- The landmark points must be marked on the vertebral body margins (border lines). When the margins appear as two lines due to rotation of the vertebra, the landmark points should be marked on the outer line.
- (c)
- Lines created by connecting landmark points vertically must be parallel and close to the outer margin of the vertebral body; this would be helpful in the evaluation of laterolisthesis in AP view images and of anterolisthesis and retrolisthesis in LAT view images. For the evaluation of anterolisthesis and retrolisthesis in LAT view images, landmark points should be located close to the anterior vertebral line and the posterior vertebral line.
- (d)
- If variations due to osteophytes and degenerative changes are observed, they can be ignored. Assuming that the vertebral body is an ideal cylinder shape, the UVEL and LVEL should be close to the diameter of the cylinder bases (top and bottom circles). If the margins of upper and lower vertebral endplates are convex, the UVEL and LVEL can be seen as penetrating the vertebral body. If the margins of the upper and lower vertebral endplates are concave, the UVEL and LVEL can be seen outside the vertebral body.
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Iguchi, T.; Wakami, T.; Kurihara, A.; Kasahara, K.; Yoshiya, S.; Nishida, K. Lumbar multilevel degenerative spondylolisthesis: Radiological evaluation and factors related to anterolisthesis and retrolisthesis. J. Spinal. Disord. Technol. 2002, 15, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Janicki, J.A.; Alman, B. Scoliosis: Review of diagnosis and treatment. Paediatr. Child Health 2007, 12, 771–776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaléat-Valayer, E.; Mac-Thiong, J.M.; Paquet, J.; Berthonnaud, E.; Siani, F.; Roussouly, P. Sagittal spino-pelvic alignment in chronic low back pain. Eur. Spine J. 2011, 20 (Suppl. S5), 634–640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berthonnaud, E.; Dimnet, J.; Roussouly, P.; Labelle, H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal. Disord. Technol. 2005, 18, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Malfair, D.; Flemming, A.K.; Dvorak, M.F.; Munk, P.L.; Vertinsky, A.T.; Heran, M.K.; Graeb, D.A. Radiographic evaluation of scoliosis: Review. AJR Am. J. Roentgenol. 2010, 194 (Suppl. S3), S8–S22. [Google Scholar] [CrossRef] [Green Version]
- Safari, A.; Parsaei, H.; Zamani, A.; Pourabbas, B. A Semi-Automatic Algorithm for Estimating Cobb Angle. J. Biomed. Phys. Eng. 2019, 9, 317–326. [Google Scholar] [CrossRef]
- Keenan, B.E.; Izatt, M.T.; Askin, G.N.; Labrom, R.D.; Bennett, D.D.; Pearcy, M.J.; Adam, C.J. Sequential Magnetic Resonance Imaging Reveals Individual Level Deformities of Vertebrae and Discs in the Growing Scoliotic Spine. Spine Deform. 2017, 5, 197–207. [Google Scholar] [CrossRef]
- Lechner, R.; Putzer, D.; Dammerer, D.; Liebensteiner, M.; Bach, C.; Thaler, M. Comparison of two- and three-dimensional measurement of the Cobb angle in scoliosis. Int. Orthop. 2017, 41, 957–962. [Google Scholar] [CrossRef] [Green Version]
- Lee, T.T.; Jiang, W.W.; Cheng, C.L.K.; Lai, K.K.; To, M.K.T.; Castelein, R.M.; Cheung, J.P.Y.; Zheng, Y.P. A Novel Method to Measure the Sagittal Curvature in Spinal Deformities: The Reliability and Feasibility of 3D Ultrasound Imaging. Ultrasound Med. Biol. 2019, 45, 2725–2735. [Google Scholar] [CrossRef]
- Horng, M.H.; Kuok, C.P.; Fu, M.J.; Lin, C.J.; Sun, Y.N. Cobb Angle Measurement of Spine from X-ray Images Using Convolutional Neural Network. Comput. Math. Methods Med. 2019, 2019, 6357171. [Google Scholar] [CrossRef] [Green Version]
- Park, T.Y.; Moon, T.W.; Cho, D.C.; Lee, J.H.; Ko, Y.S.; Hwang, E.H.; Heo, K.H.; Choi, T.Y.; Shin, B.C. An introduction to Chuna manual medicine in Korea: History, insurance coverage, education, and clinical research in Korean literature. Integr. Med. Res. 2014, 3, 49–59. [Google Scholar] [CrossRef] [Green Version]
- Jenkins, H.J.; Downie, A.S.; Moore, C.S.; French, S.D. Current evidence for spinal X-ray use in the chiropractic profession: A narrative review. Chiropr. Man. Therap. 2018, 26, 48. [Google Scholar] [CrossRef] [Green Version]
- Senzon, S.A. The Chiropractic Vertebral Subluxation Part 8: Terminology, Definitions, and Historicity from 1966 to 1980. J. Chiropr. Humanit. 2019, 25, 114–129. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, C.G.; Jo, D.C.; Moon, S.J.; Park, T.Y.; Ko, Y.S.; Nam, H.W.; Lee, J.H. Diagnostic X-ray from the Perspective of Chuna Manual Medicine, Based on the Listing System of Spinal and Pelvic Subluxation. J. Korea CHUNA Man. Med. Spine Nerves 2014, 9, 1–14. [Google Scholar]
- Lee, J.; Cho, J.H.; Kim, K.W.; Lee, J.H.; Kim, M.R.; Kim, J.; Kim, M.Y.; Cho, H.W.; Lee, Y.J.; Lee, S.H.; et al. Chuna Manual Therapy vs Usual Care for Patients with Nonspecific Chronic Neck Pain: A Randomized Clinical Trial. JAMA Netw. Open. 2021, 4, e2113757. [Google Scholar] [CrossRef]
- Lim, K.T.; Hwang, E.H.; Cho, J.H.; Jung, J.Y.; Kim, K.W.; Ha, I.H.; Kim, M.R.; Nam, K.; Lee, A.M.H.; Lee, J.H.; et al. Comparative effectiveness of Chuna manual therapy versus conventional usual care for non-acute low back pain: A pilot randomized controlled trial. Trials 2019, 20, 216. [Google Scholar] [CrossRef] [Green Version]
- Lee, N.W.; Kim, G.H.; Heo, I.; Kim, K.W.; Ha, I.H.; Lee, J.H.; Hwang, E.H.; Shin, B.C. Chuna (or Tuina) Manual Therapy for Musculoskeletal Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid. Based Complement Altern. Med. 2017, 2017, 8218139. [Google Scholar] [CrossRef] [Green Version]
- Shin, B.C.; Cho, H.W.; Hwang, E.H.; Sul, J.U.; Shin, M.S.; Nam, H.W. An literatural study of listing system of spinal subluxation. J. Korea CHUNA Man. Med. Spine Nerves 2011, 6, 141–148. [Google Scholar]
- Segundo, S.T.; Filho, E.S.V.; Lenza, M.; Santos, D.D.; Rosemberg, L.A.; Ferretti, M. Interobserver reproducibility of radiographic evaluation of lumbar spine instability. Einstein 2016, 14, 378–383. [Google Scholar] [CrossRef]
- Zhang, C.; Wang, J.; He, J.; Gao, P.; Xie, G. Automated vertebral landmarks and spinal curvature estimation using non-directional part affinity fields. Neurocomputing 2021, 438, 280–289. [Google Scholar] [CrossRef]
- Yeh, Y.C.; Weng, C.-H.; Huang, Y.-J.; Fu, C.-J.; Tsai, T.-T.; Yeh, C.-Y. Deep learning approach for automatic landmark detection and alignment analysis in whole-spine lateral radiographs. Sci. Rep. 2021, 11, 7618. [Google Scholar] [CrossRef] [PubMed]
- Vu, N.H.; Trieu, N.M.; Tuan, H.N.A.; Khoa, T.D.; Thinh, N.T. Review: Facial Anthropometric, Landmark Extraction, and Nasal Reconstruction Technology. Appl. Sci. 2022, 12, 9548. [Google Scholar] [CrossRef]
- Cao, Z.; Hidalgo, G.; Simon, T.; Wei, S.; Sheikh, Y. OpenPose: Realtime Multi-Person 2D Pose Estimation Using Part Affinity Fields. IEEE Trans. Pattern Anal. Mach. Intell. 2021, 43, 172–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gstoettner, M.; Sekyra, K.; Walochnik, N.; Winter, P.; Wachter, R.; Bach, C.M. Inter- and intraobserver reliability assessment of the Cobb angle: Manual versus digital measurement tools. Eur. Spine J. 2007, 16, 1587–1592. [Google Scholar] [CrossRef] [Green Version]
- Prestigiacomo, F.G.; Hulsbosch, M.H.H.M.; Bruls, V.E.J.; Nieuwenhuis, J.J. Intra- and inter-observer reliability of Cobb angle measurements in patients with adolescent idiopathic scoliosis. Spine Deform. 2022, 10, 79–86. [Google Scholar] [CrossRef]
- Dimar, J.R., 2nd; Carreon, L.Y.; Labelle, H.; Djurasovic, M.; Weidenbaum, M.; Brown, C.; Roussouly, P. Intra- and inter-observer reliability of determining radiographic sagittal parameters of the spine and pelvis using a manual and a computer-assisted methods. Eur. Spine J. 2008, 17, 1373–1379. [Google Scholar] [CrossRef] [Green Version]
- Wu, W.; Liang, J.; Du, Y.; Tan, X.; Xiang, X.; Wang, W.; Ru, N.; Le, J. Reliability and reproducibility analysis of the Cobb angle and assessing sagittal plane by computer-assisted and manual measurement tools. BMC Musculoskelet. Disord. 2014, 15, 33. [Google Scholar] [CrossRef] [Green Version]
- Kiefer, L.S.; Fabian, J.; Lorbeer, R.; Machann, J.; Storz, C.; Kraus, M.S.; Wintermeyer, E.; Schlett, C.; Roemer, F.; Nikolaou, K.; et al. Inter- and intra-observer variability of an anatomical landmark-based, manual segmentation method by MRI for the assessment of skeletal muscle fat content and area in subjects from the general population. Br. J. Radiol. 2018, 91, 20180019. [Google Scholar] [CrossRef]
- Tanure, M.C.; Pinheiro, A.P.; Oliveira, A.S. Reliability assessment of Cobb angle measurements using manual and digital methods. Spine J. 2010, 10, 769–774. [Google Scholar] [CrossRef]
- Moftian, N.; Samad-Soltani, T.; Salahzadeh, Z.; Pourfeizi, H.; Gheibi, Y.; Fazlollahi, A.; Rezaei, P. Computer-aided measurement system using image processing for measuring Cobb angle in scoliosis. Middle East J. Rehabil. Health Stud. 2021, 9, e111360. [Google Scholar] [CrossRef]
- Zhang, J.; Lou, E.; Shi, X.; Wang, Y.; Hill, D.L.; Raso, J.V.; Le, L.H.; Lv, L. A computer-aided Cobb angle measurement method and its reliability. J. Spinal Disord. Technol. 2010, 23, 383–387. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Tomomitsu, T.; Murase, K.; Sone, T.; Fukunaga, M. Comparison of vertebral morphometry in the lumbar vertebrae by T1-weighted sagittal MRI and radiograph. Eur. J. Radiol. 2005, 56, 102–106. [Google Scholar] [CrossRef]
- Diacinti, D.; Guglielmi, G. Vertebral morphometry. Radiol. Clin. North Am. 2010, 48, 561–575. [Google Scholar] [CrossRef]
- Korean Society of Chuna Manual Medicine for Spine & Nerves. Chuna Manual Medicine, 2.5th ed.; Society of Chuna Manual Medicine for Spine & Nerves: Seoul, Republic of Korea, 2017. [Google Scholar]
- Holt, K.; Russell, D.; Cooperstein, R.; Young, M.; Sherson, M.; Haavik, H. Interexaminer reliability of a multidimensional battery of tests used to assess for vertebral subluxations. Chiropr. J. Aust. 2018, 46, 100–117. [Google Scholar]
- Nolet, P.S.; Yu, H.; Côté, P.; Meyer, A.-L.; Kristman, V.L.; Sutton, D.; Murnaghan, K.; Lemeunier, N. Reliability and validity of manual palpation for the assessment of patients with low back pain: A systematic and critical review. Chiropr. Man. Therap. 2021, 29, 33. [Google Scholar] [CrossRef]
- Lopes, M.A.; Coleman, R.R.; Cremata, E.J. Radiography and clinical decision-making in chiropractic. Dose Response 2021, 19, 15593258211044844. [Google Scholar] [CrossRef]
- Engelke, K.; Stampa, B.; Steiger, P.; Fuerst, T.; Genant, H.K. Automated quantitative morphometry of vertebral heights on spinal radiographs: Comparison of a clinical workflow tool with standard 6-point morphometry. Arch. Osteoporos. 2019, 14, 18. [Google Scholar] [CrossRef]
- Fard, A.P.; Ferrantelli, J.; Dupuis, A.-L.; Mahoor, M.H. Sagittal Cervical Spine Landmark Point Detection in X-ray Using Deep Convolutional Neural Networks. IEEE Access 2022, 10, 59413–59427. [Google Scholar] [CrossRef]
| AP | LAT | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | |||||||
| Mean (SD) † | ICC (95% CI) | Mean (SD) † | ICC (95% CI) | p-Value †† | Mean (SD) † | ICC (95% CI) | Mean (SD) † | ICC (95% CI) | p-Value †† | |
| L1_p1 | 1.454 (0.898) | 0.991 (0.990, 0.992) | 1.397 (0.763) | 0.992 (0.991, 0.993) | 0.748 | 1.164 (0.737) | 0.995 (0.994, 0.995) | 1.047 (0.682) | 0.996 (0.995, 0.996) | 0.506 |
| L1_p2 | 1.602 (1.060) | 0.991 (0.989, 0.992) | 1.538 (0.847) | 0.991 (0.990, 0.992) | 0.777 | 1.711 (1.079) | 0.990 (0.988, 0.991) | 1.487 (0.840) | 0.993 (0.992, 0.993) | 0.135 |
| L1_p3 | 1.794 (1.163) | 0.987 (0.985, 0.988) | 1.798 (0.931) | 0.988 (0.987, 0.989) | 0.992 | 1.181 (0.717) | 0.995 (0.994, 0.995) | 1.042 (0.693) | 0.996 (0.995, 0.996) | 0.399 |
| L1_p4 | 1.979 (1.294) | 0.985 (0.983, 0.987) | 1.787 (0.992) | 0.988 (0.986, 0.989) | 0.489 | 1.498 (0.972) | 0.991 (0.990, 0.992) | 1.350 (0.824) | 0.993 (0.992, 0.994) | 0.437 |
| L2_p1 | 1.641 (0.992) | 0.989 (0.988, 0.991) | 1.667 (0.832) | 0.990 (0.989, 0.991) | 0.909 | 1.183 (0.744) | 0.995 (0.994, 0.995) | 1.129 (0.687) | 0.995 (0.995, 0.996) | 0.749 |
| L2_p2 | 1.723 (1.091) | 0.989 (0.988, 0.991) | 1.748 (0.914) | 0.989 (0.987, 0.990) | 0.920 | 1.582 (0.968) | 0.990 (0.989, 0.991) | 1.504 (0.820) | 0.991 (0.990, 0.992) | 0.657 |
| L2_p3 | 1.932 (1.209) | 0.987 (0.985, 0.988) | 1.997 (1.005) | 0.987 (0.986, 0.988) | 0.807 | 1.287 (0.772) | 0.994 (0.993, 0.995) | 1.127 (0.744) | 0.995 (0.994, 0.995) | 0.366 |
| L2_p4 | 2.130 (1.354) | 0.984 (0.982, 0.986) | 1.985 (1.012) | 0.988 (0.986, 0.989) | 0.617 | 1.523 (0.953) | 0.990 (0.989, 0.991) | 1.342 (0.811) | 0.993 (0.992, 0.994) | 0.298 |
| L3_p1 | 1.778 (1.063) | 0.988 (0.987, 0.990) | 1.814 (0.943) | 0.989 (0.988, 0.990) | 0.890 | 1.197 (0.751) | 0.995 (0.994, 0.995) | 1.228 (0.743) | 0.994 (0.994, 0.995) | 0.847 |
| L3_p2 | 1.910 (1.199) | 0.988 (0.986, 0.989) | 1.835 (0.963) | 0.989 (0.987, 0.990) | 0.753 | 1.565 (0.988) | 0.990 (0.988, 0.991) | 1.500 (0.819) | 0.991 (0.990, 0.992) | 0.716 |
| L3_p3 | 1.935 (1.224) | 0.987 (0.985, 0.989) | 2.054 (1.042) | 0.988 (0.986, 0.989) | 0.686 | 1.280 (0.786) | 0.994 (0.993, 0.994) | 1.112 (0.704) | 0.995 (0.994, 0.996) | 0.308 |
| L3_p4 | 2.245 (1.437) | 0.984 (0.982, 0.986) | 2.141 (1.103) | 0.986 (0.985, 0.988) | 0.771 | 1.452 (0.926) | 0.991 (0.990, 0.992) | 1.347 (0.827) | 0.992 (0.991, 0.993) | 0.573 |
| L4_p1 | 1.926 (1.190) | 0.986 (0.984, 0.988) | 1.928 (1.004) | 0.988 (0.986, 0.989) | 0.990 | 1.261 (0.846) | 0.994 (0.993, 0.995) | 1.329 (0.860) | 0.992 (0.991, 0.993) | 0.700 |
| L4_p2 | 2.133 (1.368) | 0.985 (0.983, 0.987) | 2.000 (1.077) | 0.986 (0.985, 0.988) | 0.641 | 1.538 (0.973) | 0.990 (0.989, 0.991) | 1.473 (0.821) | 0.991 (0.989, 0.992) | 0.709 |
| L4_p3 | 2.043 (1.276) | 0.983 (0.981, 0.985) | 2.066 (1.134) | 0.986 (0.984, 0.988) | 0.941 | 1.371 (0.880) | 0.992 (0.991, 0.993) | 1.165 (0.737) | 0.994 (0.994, 0.995) | 0.320 |
| L4_p4 | 2.406 (1.519) | 0.976 (0.973, 0.979) | 2.144 (1.240) | 0.985 (0.983, 0.986) | 0.443 | 1.437 (0.894) | 0.992 (0.991, 0.993) | 1.336 (0.870) | 0.992 (0.991, 0.993) | 0.605 |
| L5_p1 | 2.805 (1.914) | 0.960 (0.954, 0.964) | 2.492 (1.512) | 0.970 (0.966, 0.974) | 0.312 | 1.355 (1.085) | 0.992 (0.991, 0.993) | 1.534 (0.976) | 0.990 (0.989, 0.991) | 0.420 |
| L5_p2 | 3.076 (2.116) | 0.957 (0.951, 0.962) | 2.530 (1.581) | 0.970 (0.966, 0.973) | 0.164 | 1.565 (1.086) | 0.989 (0.987, 0.990) | 1.478 (0.928) | 0.990 (0.989, 0.991) | 0.683 |
| L5_p3 | 3.381 (2.279) | 0.937 (0.929, 0.945) | 3.036 (2.041) | 0.948 (0.942, 0.954) | 0.446 | 1.617 (1.451) | 0.986 (0.984, 0.988) | 1.320 (1.285) | 0.989 (0.988, 0.991) | 0.205 |
| L5_p4 | 3.606 (2.485) | 0.935 (0.926, 0.942) | 2.918 (2.126) | 0.947 (0.940, 0.953) | 0.204 | 1.599 (1.279) | 0.988 (0.986, 0.990) | 1.520 (1.191) | 0.988 (0.987, 0.990) | 0.703 |
| AP | LAT | |||
|---|---|---|---|---|
| Mean (SD) † | ICC (95% CI) | Mean (SD) † | ICC (95% CI) | |
| L1_p1 | 1.469 (0.935) | 0.991 (0.990, 0.993) | 1.197 (0.822) | 0.989 (0.986, 0.991) |
| L1_p2 | 1.563 (1.054) | 0.991 (0.988, 0.992) | 1.670 (1.065) | 0.984 (0.981, 0.987) |
| L1_p3 | 1.782 (1.128) | 0.988 (0.985, 0.990) | 1.185 (0.808) | 0.989 (0.986, 0.990) |
| L1_p4 | 1.883 (1.310) | 0.986 (0.983, 0.989) | 1.480 (1.017) | 0.985 (0.981, 0.988) |
| L2_p1 | 1.674 (0.992) | 0.990 (0.987, 0.991) | 1.229 (0.810) | 0.988 (0.985, 0.990) |
| L2_p2 | 1.702 (1.083) | 0.990 (0.987, 0.992) | 1.605 (1.014) | 0.983 (0.979, 0.986) |
| L2_p3 | 1.919 (1.168) | 0.987 (0.984, 0.989) | 1.255 (0.808) | 0.987 (0.984, 0.990) |
| L2_p4 | 2.008 (1.306) | 0.987 (0.983, 0.989) | 1.484 (1.005) | 0.985 (0.982, 0.988) |
| L3_p1 | 1.774 (1.073) | 0.989 (0.987, 0.991) | 1.263 (0.830) | 0.986 (0.983, 0.989) |
| L3_p2 | 1.801 (1.115) | 0.990 (0.988, 0.992) | 1.602 (1.033) | 0.983 (0.979, 0.986) |
| L3_p3 | 1.933 (1.200) | 0.989 (0.986, 0.991) | 1.237 (0.835) | 0.988 (0.985, 0.990) |
| L3_p4 | 2.107 (1.352) | 0.987 (0.984, 0.989) | 1.442 (0.982) | 0.988 (0.985, 0.990) |
| L4_p1 | 1.902 (1.135) | 0.988 (0.985, 0.990) | 1.307 (0.865) | 0.986 (0.983, 0.988) |
| L4_p2 | 1.986 (1.264) | 0.987 (0.984, 0.990) | 1.561 (0.997) | 0.985 (0.981, 0.988) |
| L4_p3 | 2.037 (1.293) | 0.985 (0.981, 0.988) | 1.285 (0.884) | 0.988 (0.984, 0.990) |
| L4_p4 | 2.236 (1.496) | 0.981 (0.976, 0.984) | 1.417 (0.952) | 0.990 (0.987, 0.992) |
| L5_p1 | 2.677 (1.710) | 0.966 (0.957, 0.972) | 1.410 (0.924) | 0.988 (0.985, 0.990) |
| L5_p2 | 2.722 (1.787) | 0.967 (0.960, 0.972) | 1.593 (1.073) | 0.988 (0.985, 0.990) |
| L5_p3 | 3.330 (2.308) | 0.937 (0.922, 0.947) | 1.521 (1.741) | 0.984 (0.981, 0.987) |
| L5_p4 | 3.430 (2.450) | 0.934 (0.920, 0.946) | 1.645 (1.480) | 0.988 (0.985, 0.990) |
| AP | LAT | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | |||||||
| Mean (SD) † | ICC (95% CI) | Mean (SD) † | ICC (95% CI) | p-Value †† | Mean (SD) † | ICC (95% CI) | Mean (SD) † | ICC (95% CI) | p-Value †† | |
| L1_UVEL | 0.716 (0.603) | 0.921 (0.909, 0.930) | 0.678 (0.566) | 0.907 (0.895, 0.917) | 0.664 | 1.170 (0.944) | 0.938 (0.930, 0.945) | 1.162 (0.940) | 0.938 (0.922, 0.950) | 0.958 |
| L1_LVEL | 0.797 (0.660) | 0.909 (0.896, 0.919) | 0.723 (0.617) | 0.901 (0.886, 0.914) | 0.419 | 1.054 (0.894) | 0.947 (0.934, 0.955) | 0.978 (0.813) | 0.952 (0.938, 0.961) | 0.618 |
| L2_UVEL | 0.735 (0.614) | 0.917 (0.905, 0.928) | 0.677 (0.570) | 0.909 (0.896, 0.920) | 0.583 | 1.089 (0.877) | 0.942 (0.933, 0.949) | 1.078 (0.873) | 0.940 (0.921, 0.952) | 0.949 |
| L2_LVEL | 0.764 (0.650) | 0.915 (0.905, 0.926) | 0.664 (0.560) | 0.921 (0.908, 0.930) | 0.303 | 0.942 (0.787) | 0.959 (0.952, 0.964) | 0.982 (0.812) | 0.952 (0.941, 0.959) | 0.732 |
| L3_UVEL | 0.669 (0.604) | 0.925 (0.913, 0.935) | 0.613 (0.530) | 0.930 (0.922, 0.938) | 0.572 | 1.024 (0.837) | 0.952 (0.945, 0.958) | 1.088 (0.862) | 0.944 (0.933, 0.952) | 0.623 |
| L3_LVEL | 0.635 (0.573) | 0.939 (0.931, 0.945) | 0.572 (0.498) | 0.942 (0.933, 0.949) | 0.543 | 0.918 (0.786) | 0.967 (0.963, 0.971) | 0.982 (0.807) | 0.960 (0.949, 0.967) | 0.544 |
| L4_UVEL | 0.686 (0.600) | 0.923 (0.913, 0.933) | 0.621 (0.560) | 0.926 (0.916, 0.934) | 0.562 | 1.024 (0.852) | 0.963 (0.957, 0.967) | 1.149 (0.928) | 0.947 (0.937, 0.955) | 0.343 |
| L4_LVEL | 0.754 (0.682) | 0.905 (0.892, 0.915) | 0.662 (0.611) | 0.915 (0.894, 0.927) | 0.433 | 1.062 (0.884) | 0.969 (0.965, 0.972) | 1.097 (0.915) | 0.961 (0.952, 0.967) | 0.794 |
| L5_UVEL | 0.950 (0.828) | 0.817 (0.796, 0.835) | 0.877 (0.790) | 0.827 (0.800, 0.849) | 0.499 | 1.229 (1.029) | 0.962 (0.955, 0.967) | 1.319 (1.102) | 0.951 (0.941, 0.957) | 0.561 |
| L5_LVEL | 1.042 (0.913) | 0.777 (0.755, 0.799) | 1.033 (0.909) | 0.759 (0.708, 0.793) | 0.933 | 1.451 (1.322) | 0.950 (0.943, 0.956) | 1.532 (1.401) | 0.939 (0.924, 0.949) | 0.702 |
| AP | LAT | |||
|---|---|---|---|---|
| Mean (SD) † | ICC (95% CI) | Mean (SD) † | ICC (95% CI) | |
| L1_UVEL | 0.661 (0.548) | 0.931 (0.916, 0.943) | 1.141 (0.953) | 0.944 (0.928, 0.956) |
| L1_LVEL | 0.718 (0.614) | 0.918 (0.899, 0.931) | 1.055 (0.916) | 0.948 (0.930, 0.960) |
| L2_UVEL | 0.678 (0.566) | 0.921 (0.903, 0.935) | 1.049 (0.887) | 0.946 (0.928, 0.958) |
| L2_LVEL | 0.677 (0.573) | 0.926 (0.909, 0.939) | 0.936 (0.748) | 0.957 (0.947, 0.965) |
| L3_UVEL | 0.606 (0.525) | 0.933 (0.918, 0.945) | 1.066 (0.875) | 0.942 (0.928, 0.954) |
| L3_LVEL | 0.577 (0.503) | 0.942 (0.928, 0.952) | 0.906 (0.787) | 0.963 (0.953, 0.970) |
| L4_UVEL | 0.643 (0.572) | 0.933 (0.917, 0.943) | 1.067 (0.893) | 0.953 (0.941, 0.960) |
| L4_LVEL | 0.689 (0.640) | 0.924 (0.907, 0.938) | 1.037 (0.862) | 0.960 (0.951, 0.968) |
| L5_UVEL | 0.901 (0.791) | 0.839 (0.801, 0.865) | 1.240 (1.007) | 0.957 (0.947, 0.964) |
| L5_LVEL | 0.979 (0.871) | 0.801 (0.764, 0.834) | 1.486 (1.448) | 0.942 (0.929, 0.952) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, J.-S.; Kim, J.I.; Ku, B.; Lee, J.-H. Reliability Analysis of Vertebral Landmark Labelling on Lumbar Spine X-ray Images. Diagnostics 2023, 13, 1411. https://doi.org/10.3390/diagnostics13081411
Jang J-S, Kim JI, Ku B, Lee J-H. Reliability Analysis of Vertebral Landmark Labelling on Lumbar Spine X-ray Images. Diagnostics. 2023; 13(8):1411. https://doi.org/10.3390/diagnostics13081411
Chicago/Turabian StyleJang, Jun-Su, Joong Il Kim, Boncho Ku, and Jin-Hyun Lee. 2023. "Reliability Analysis of Vertebral Landmark Labelling on Lumbar Spine X-ray Images" Diagnostics 13, no. 8: 1411. https://doi.org/10.3390/diagnostics13081411
APA StyleJang, J.-S., Kim, J. I., Ku, B., & Lee, J.-H. (2023). Reliability Analysis of Vertebral Landmark Labelling on Lumbar Spine X-ray Images. Diagnostics, 13(8), 1411. https://doi.org/10.3390/diagnostics13081411









