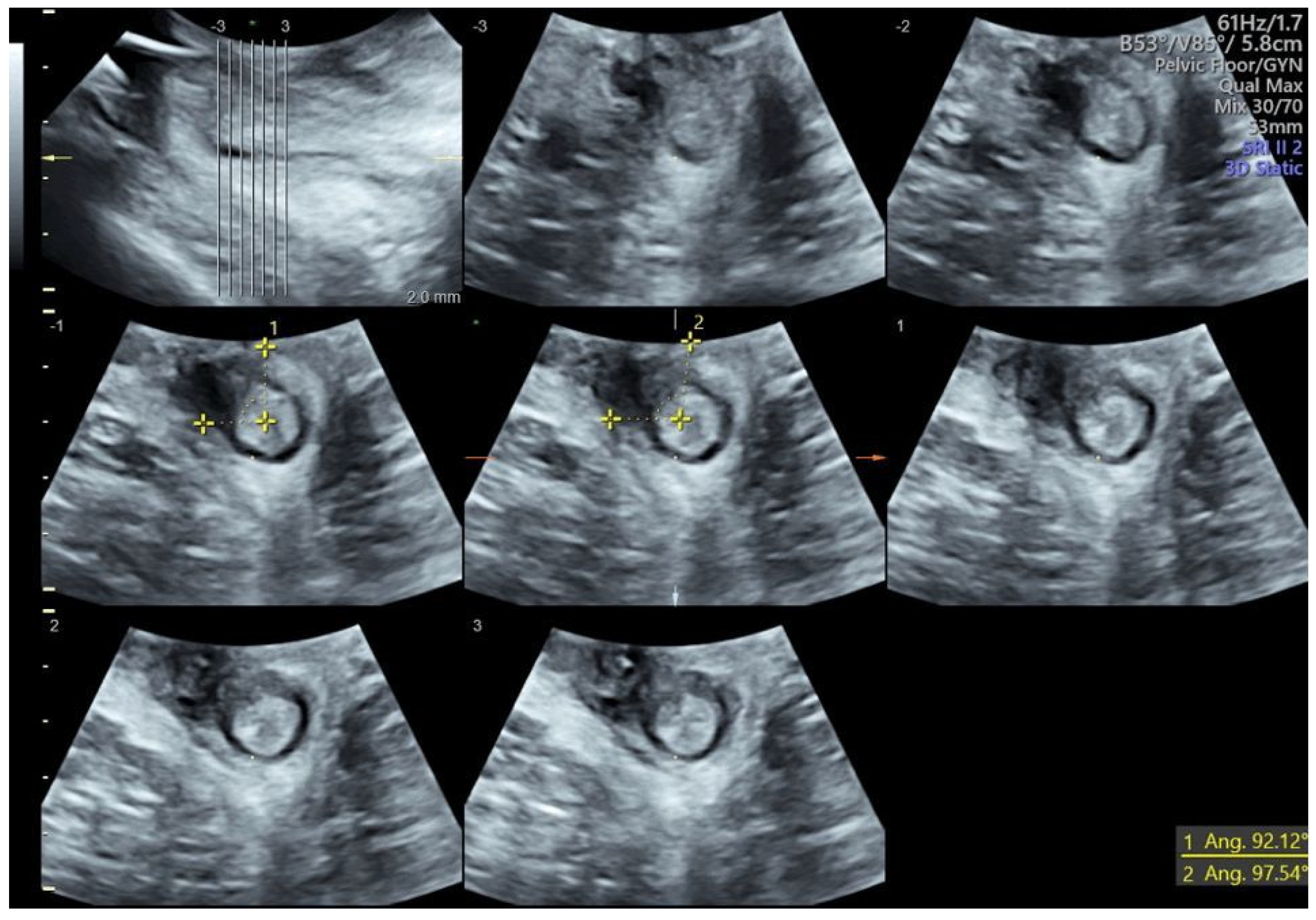
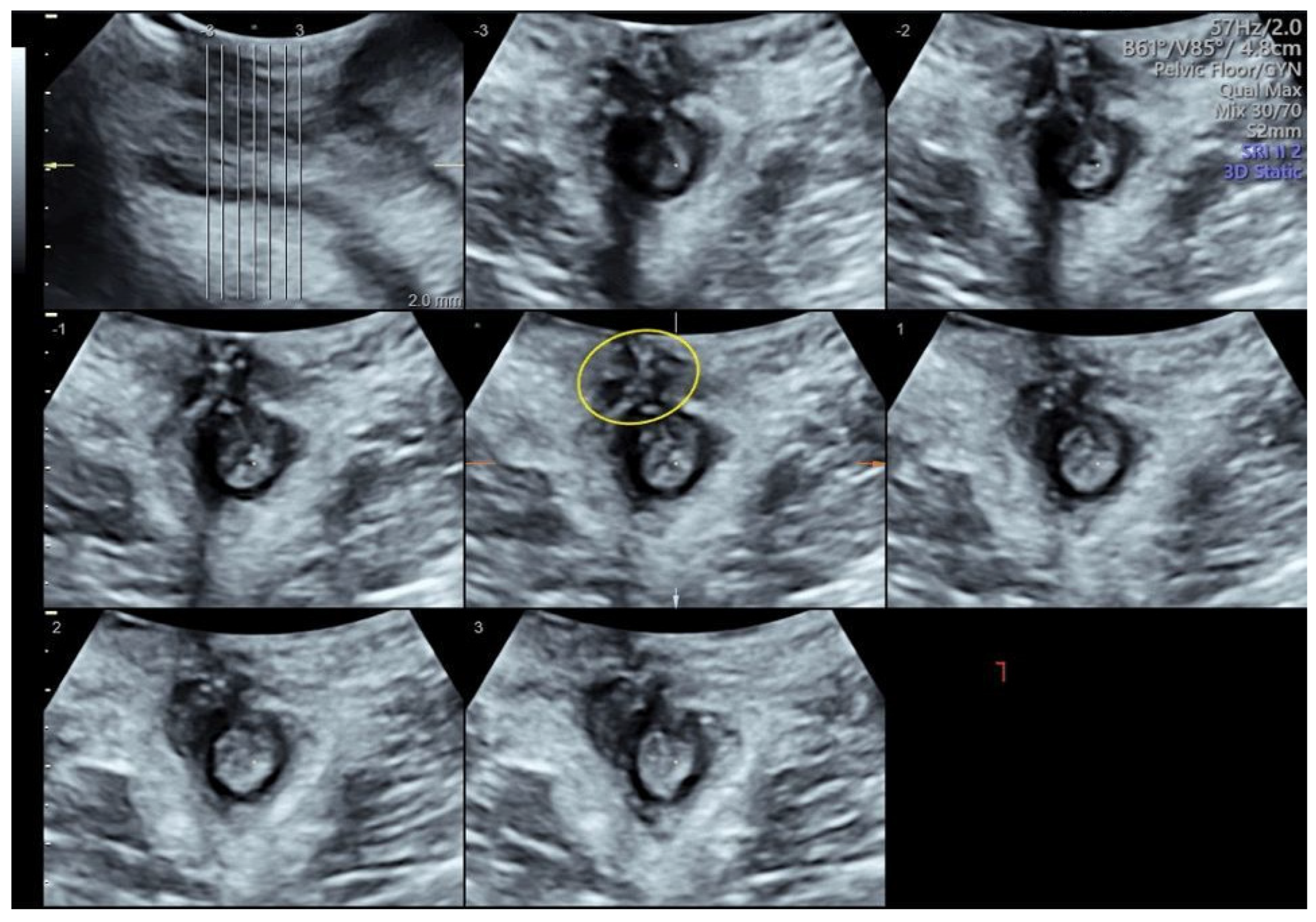
Three-Dimensional Transperineal Ultrasound Guiding Early Secondary Repair of Obstetric Anal Sphincter Injury in an Incontinent Patient without Suture Dehiscence
Abstract
:Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hehir, M.P.; O’Connor, H.D.; Higgins, S.; Robson, M.S.; McAuliffe, F.M.; Boylan, P.C.; Malone, F.D.; Mahony, R. Obstetric Anal Sphincter Injury, Risk Factors and Method of Delivery—An 8-Year Analysis across Two Tertiary Referral Centers. J. Matern.-Fetal Neonatal Med. 2013, 26, 1514–1516. [Google Scholar] [CrossRef] [PubMed]
- Friedman, A.M.; Ananth, C.V.; Prendergast, E.; D’Alton, M.E.; Wright, J.D. Evaluation of Third-Degree and Fourth-Degree Laceration Rates as Quality Indicators. Obstet. Gynecol. 2015, 125, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Ampt, A.J.; Patterson, J.A.; Roberts, C.L.; Ford, J.B. Obstetric Anal Sphincter Injury Rates among Primiparous Women with Different Modes of Vaginal Delivery. Int. J. Gynecol. Obstet. 2015, 131, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Meister, M.R.L.; Cahill, A.G.; Conner, S.N.; Woolfolk, C.L.; Lowder, J.L. Predicting Obstetric Anal Sphincter Injuries in a Modern Obstetric Population. Am. J. Obstet. Gynecol. 2016, 215, 310.e1–310.e7. [Google Scholar] [CrossRef] [PubMed]
- Hehir, M.P.; Rubeo, Z.; Flood, K.; Mardy, A.H.; O’Herlihy, C.; Boylan, P.C.; D’Alton, M.E. Anal Sphincter Injury in Vaginal Deliveries Complicated by Shoulder Dystocia. Int. Urogynecol. J. 2018, 29, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Cichowski, S.; Rogers, R. Prevention and Management of Obstetric Lacerations at Vaginal Delivery. Obstet. Gynecol. 2018, 132, e87–e102. [Google Scholar] [CrossRef]
- Wilson, A.N.; Homer, C.S.E. Third- and Fourth-degree Tears: A Review of the Current Evidence for Prevention and Management. Aust. N. Z. J. Obs. Gynaecol. 2020, 60, 175–182. [Google Scholar] [CrossRef]
- Kapoor, D.S.; Thakar, R.; Sultan, A.H. Obstetric Anal Sphincter Injuries: Review of Anatomical Factors and Modifiable Second Stage Interventions. Int. Urogynecol. J. 2015, 26, 1725–1734. [Google Scholar] [CrossRef]
- Frenette, P.; Crawford, S.; Schulz, J.; Ospina, M.B. Impact of Episiotomy During Operative Vaginal Delivery on Obstetrical Anal Sphincter Injuries. J. Obstet. Gynaecol. Can. 2019, 41, 1734–1741. [Google Scholar] [CrossRef]
- Okeahialam, N.A.; Wong, K.W.; Jha, S.; Sultan, A.H.; Thakar, R. Mediolateral/Lateral Episiotomy with Operative Vaginal Delivery and the Risk Reduction of Obstetric Anal Sphincter Injury (OASI): A Systematic Review and Meta-Analysis. Int. Urogynecol. J. 2022, 33, 1393–1405. [Google Scholar] [CrossRef]
- Sideris, M.; McCaughey, T.; Hanrahan, J.G.; Arroyo-Manzano, D.; Zamora, J.; Jha, S.; Knowles, C.H.; Thakar, R.; Chaliha, C.; Thangaratinam, S. Risk of Obstetric Anal Sphincter Injuries (OASIS) and Anal Incontinence: A Meta-Analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Stickelmann, A.-L.; Kennes, L.N.; Hölscher, M.; Graef, C.; Kupec, T.; Wittenborn, J.; Stickeler, E.; Najjari, L. Obstetric Anal Sphincter Injuries (OASIS): Using Transperineal Ultrasound (TPUS) for Detecting, Visualizing and Monitoring the Healing Process. BMC Women’s Health 2022, 22, 339. [Google Scholar] [CrossRef] [PubMed]
- Cotterill, N.; Norton, C.; Avery, K.N.L.; Abrams, P.; Donovan, J.L. Psychometric Evaluation of a New Patient-Completed Questionnaire for Evaluating Anal Incontinence Symptoms and Impact on Quality of Life: The ICIQ-B. Dis. Colon Rectum 2011, 54, 1235–1250. [Google Scholar] [CrossRef] [PubMed]
- Carter, D.; Ram, E.; Engel, T. Combined 3D Endoanal Ultrasound and Transperineal Ultrasound Improves the Detection of Anal Sphincter Defects. Diagnostics 2023, 13, 682. [Google Scholar] [CrossRef] [PubMed]
- Okeahialam, N.; Thakar, R.; Kleprlikova, H.; Taithongchai, A.; Sultan, A. Early Re-Suturing of Dehisced Obstetric Perineal Wounds: A 13-Year Experience. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 254, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Okeahialam, N.A.; Thakar, R.; Sultan, A.H. Early Secondary Repair of Obstetric Anal Sphincter Injuries (OASIs): Experience and a Review of the Literature. Int. Urogynecol. J. 2021, 32, 1611–1622. [Google Scholar] [CrossRef] [PubMed]
- Ros, C.; Martínez-Franco, E.; Wozniak, M.M.; Cassado, J.; Santoro, G.A.; Elías, N.; López, M.; Palacio, M.; Wieczorek, A.P.; Espuña-Pons, M. Postpartum Two- and Three-Dimensional Ultrasound Evaluation of Anal Sphincter Complex in Women with Obstetric Anal Sphincter Injury. Ultrasound Obs. Gynecol. 2017, 49, 508–514. [Google Scholar] [CrossRef]
- Hakim, S.; Santoso, B.I.; Djusad, S.; Moegni, F.; Surya, R.; Kurniawan, A.P. Diagnostic Capabilities of Transperineal Ultrasound (TPUS) to Evaluate Anal Sphincter Defect Post Obstetric Anal Sphincter Injury (OASIS)? A Systematic Review. J. Ultrasound 2023, 26, 393–399. [Google Scholar] [CrossRef]
- Volløyhaug, I.; Taithongchai, A.; Arendsen, L.; Van Gruting, I.; Sultan, A.H.; Thakar, R. Is Endoanal, Introital or Transperineal Ultrasound Diagnosis of Sphincter Defects More Strongly Associated with Anal Incontinence? Int. Urogynecol. J. 2020, 31, 1471–1478. [Google Scholar] [CrossRef]
- Barbosa, M.; Christensen, P.; Møller-Bek, K.; Brogaard, L.; Glavind-Kristensen, M. Can Ultrasound 10 Days after Obstetric Anal Sphincter Injury Predict Anal Incontinence at Long-Term Follow-Up? Int. Urogynecol. J. 2021, 32, 2511–2520. [Google Scholar] [CrossRef]
- Arona, A.J.; al-Marayati, L.; Grimes, D.A.; Ballard, C.A. Early Secondary Repair of Third- and Fourth-Degree Perineal Lacerations after Outpatient Wound Preparation. Obs. Gynecol. 1995, 86, 294–296. [Google Scholar] [CrossRef] [PubMed]
- Soerensen, M.M.; Bek, K.M.; Buntzen, S.; Højberg, K.-E.; Laurberg, S. Long-Term Outcome of Delayed Primary or Early Secondary Reconstruction of the Anal Sphincter after Obstetrical Injury. Dis. Colon Rectum 2008, 51, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, M.; Glavind-Kristensen, M.; Christensen, P. Early Secondary Repair of Obstetric Anal Sphincter Injury: Postoperative Complications, Long-Term Functional Outcomes, and Impact on Quality of Life. Tech. Coloproctol. 2020, 24, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Nordenstam, J.; Mellgren, A.; Altman, D.; López, A.; Johansson, C.; Anzén, B.; Li, Z.-Z.; Zetterström, J. Immediate or Delayed Repair of Obstetric Anal Sphincter Tears-a Randomised Controlled Trial. BJOG 2008, 115, 857–865. [Google Scholar] [CrossRef]
- Abdool, Z.; Sultan, A.H.; Thakar, R. Ultrasound Imaging of the Anal Sphincter Complex: A Review. BJR 2012, 85, 865–875. [Google Scholar] [CrossRef]
- García-Mejido, J.A.; Gutiérrez Palomino, L.; Fernández Palacín, A.; Sainz-Bueno, J.A. Aplicabilidad de la ecografía transperineal en 3/4D para el diagnóstico de lesiones del esfínter anal durante el posparto inmediato [Applicability of 3/4D transperineal ultrasound for the diagnosis of anal sphincter injury during the immediate pospartum]. Cir. Cir. 2017, 85, 80–86. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orsi, M.; Cappuccio, G.; Kurihara, H.; Rossi, G.; Perugino, G.; Ferrazzi, E.; Coppola, C. Three-Dimensional Transperineal Ultrasound Guiding Early Secondary Repair of Obstetric Anal Sphincter Injury in an Incontinent Patient without Suture Dehiscence. Diagnostics 2024, 14, 68. https://doi.org/10.3390/diagnostics14010068
Orsi M, Cappuccio G, Kurihara H, Rossi G, Perugino G, Ferrazzi E, Coppola C. Three-Dimensional Transperineal Ultrasound Guiding Early Secondary Repair of Obstetric Anal Sphincter Injury in an Incontinent Patient without Suture Dehiscence. Diagnostics. 2024; 14(1):68. https://doi.org/10.3390/diagnostics14010068
Chicago/Turabian StyleOrsi, Michele, Giuseppe Cappuccio, Hayato Kurihara, Gabriele Rossi, Giuseppe Perugino, Enrico Ferrazzi, and Carmela Coppola. 2024. "Three-Dimensional Transperineal Ultrasound Guiding Early Secondary Repair of Obstetric Anal Sphincter Injury in an Incontinent Patient without Suture Dehiscence" Diagnostics 14, no. 1: 68. https://doi.org/10.3390/diagnostics14010068
APA StyleOrsi, M., Cappuccio, G., Kurihara, H., Rossi, G., Perugino, G., Ferrazzi, E., & Coppola, C. (2024). Three-Dimensional Transperineal Ultrasound Guiding Early Secondary Repair of Obstetric Anal Sphincter Injury in an Incontinent Patient without Suture Dehiscence. Diagnostics, 14(1), 68. https://doi.org/10.3390/diagnostics14010068





