Applying the German S2k-Guideline for Diagnosis and Treatment of Spondylodiscitis—A 5-Year Retrospective Evaluation of Patients without Neurological Symptoms
Abstract
:1. Introduction
2. Materials and Methods
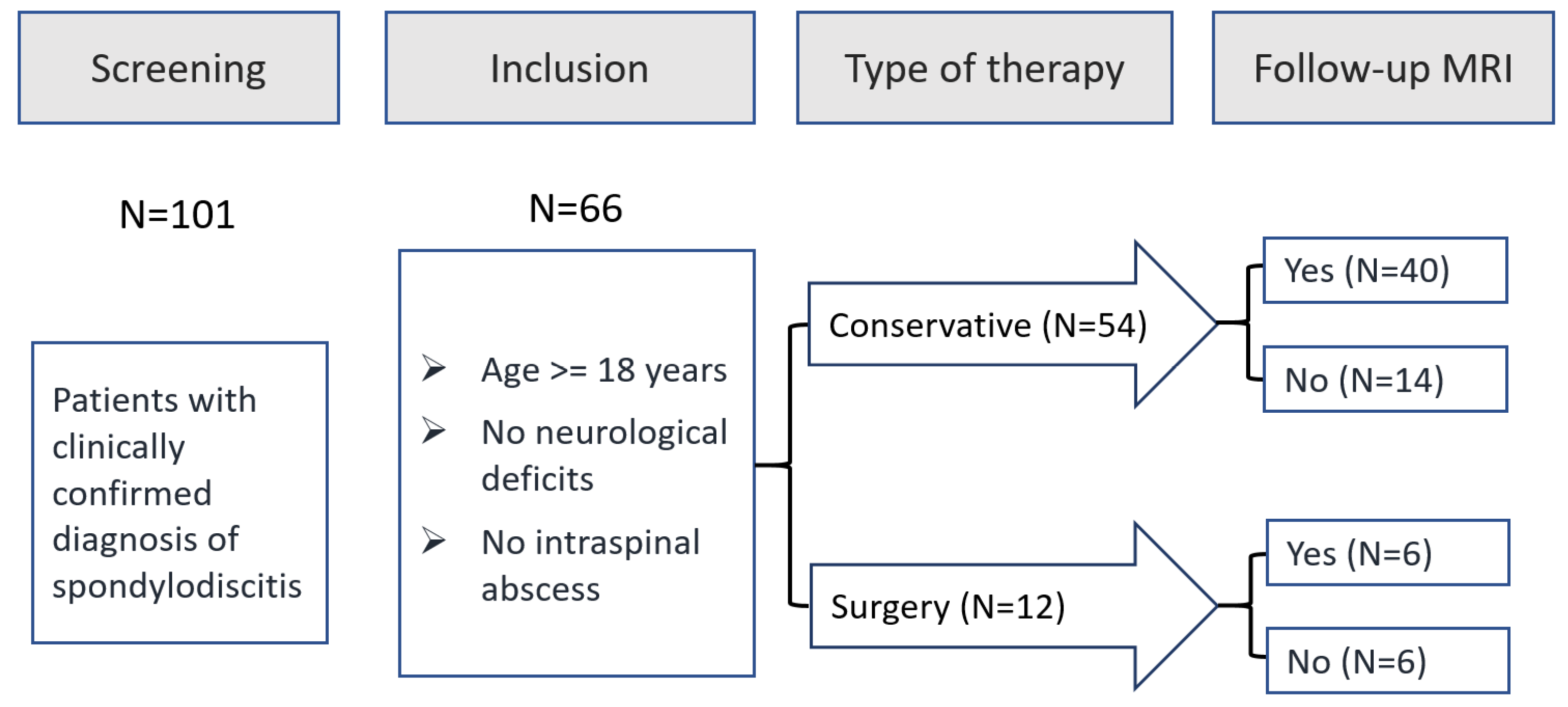
2.1. Study Design
- -
- Clinically confirmed diagnosis of spondylodiscitis
- -
- Treatment of the condition at our hospital
- -
- >=18 years of age
- -
- Neurological deficits
- -
- Intraspinal abscesses
- -
- <18 years of age
2.2. Description of the In-House Treatment Algorithm
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Conversion from Non-Operative to Operative Therapy
3.3. Short-Term Patient Outcome after Conservative/Surgical Therapy
3.4. Comparison of the In-House Standard with the S2k Treatment Guideline
| Stage | S2k-Guideline Recommendation | Expert Consensus Achieved | In-House Standard |
|---|---|---|---|
| Preclinical |
|
| Complies with the guideline |
| Anamnesis |
|
| Complies with the guideline |
| Physical Examination |
|
| Complies with the guideline |
| Diagnostics |
|
| In addition to the guideline:
|
| Therapy |
| Complies with the guideline | |
| Anti-infective therapy |
Anti-infective therapy:
|
|
|
| Pain treatment |
|
|
|
| Mobilization |
|
|
|
| Follow-up |
|
|
|
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variable | All Patients (N = 66) | Conservative (N = 54) | Surgery (N = 12) |
|---|---|---|---|
| Psoas abscess, n (%) | 32 (48.5%) | 27 (50.0%) | 5 (41.7%) |
| Carcinoma, n (%) | 14 (21.2%) | 12 (22.2%) | 2 (16.7%) |
| Coronary heart disease, n (%) | 30 (45.5%) | 26 (48.1%) | 4 (33.3%) |
| Renal insufficiency, n (%) | 32 (48.5%) | 27 (50.0%) | 5 (41.7%) |
| Diabetes mellitus, n (%) | 31 (47.0%) | 23 (42.6%) | 8 (66.7%) |
| Immunosuppressed, n (%) | 8 (12.1%) | 8 (14.8%) | 0 |
| Fever, n (%) | 13 (19.7%) | 12 (22.2%) | 1 (8.3%) |
References
- Issa, K.; Diebo, B.G.; Faloon, M.; Naziri, Q.; Pourtaheri, S.; Paulino, C.B.; Emami, A. The Epidemiology of Vertebral Osteomyelitis in the United States From 1998 to 2013. Clin. Spine Surg. A Spine Publ. 2018, 31, E102–E108. [Google Scholar] [CrossRef] [PubMed]
- Kehrer, M.; Pedersen, C.; Jensen, T.G.; Lassen, A.T. Increasing incidence of pyogenic spondylodiscitis: A 14-year population-based study. J. Infect. 2014, 68, 313–320. [Google Scholar] [CrossRef] [PubMed]
- DeStatis (Statistisches Bundesamt). Diagnosedaten der Krankenhäuser ab 2000 (Eckdaten der Vollstationären Patienten und Patientinnen). Gliederungsmerkmale: Jahre, Behandlungs-/Wohnort, ICD10; DeStatis (Statistisches Bundesamt): Wiesbaden, Germany, 2017.
- Gouliouris, T.; Aliyu, S.H.; Brown, N.M. Spondylodiscitis: Update on diagnosis and management. J. Antimicrob. Chemother. 2010, 65 (Suppl. S3), iii11–iii24. [Google Scholar] [CrossRef] [PubMed]
- Cheung, W.Y.; Luk, K.D. Pyogenic spondylitis. Int. Orthop. 2012, 36, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Kowalski, T.J.; Osmon, D.R.; Enzler, M.; Steckelberg, J.M.; Huddleston, P.M.; Nassr, A.; Mandrekar, J.M.; Berbari, E.F. Long-term outcome of pyogenic vertebral osteomyelitis: A cohort study of 260 patients. Open Forum Infect. Dis. 2014, 1, ofu107. [Google Scholar] [CrossRef] [PubMed]
- Kehrer, M.; Pedersen, C.; Jensen, T.G.; Hallas, J.; Lassen, A.T. Increased short- and long-term mortality among patients with infectious spondylodiscitis compared with a reference population. Spine J. 2015, 15, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Sobottke, R.; Röllinghoff, M.; Zarghooni, K.; Zarghooni, K.; Schlüter-Brust, K.; Delank, K.-S.; Seifert, H.; Zweig, T.; Eysel, P. Spondylodiscitis in the elderly patient: Clinical mid-term results and quality of life. Arch. Orthop. Trauma Surg. 2010, 130, 1083–1091. [Google Scholar] [CrossRef] [PubMed]
- Bhavan, K.P.; Marschall, J.; Olsen, M.A.; Fraser, V.J.; Wright, N.M.; Warren, D.K. The epidemiology of hematogenous vertebral osteomyelitis: A cohort study in a tertiary care hospital. BMC Infect. Dis. 2010, 10, 158. [Google Scholar] [CrossRef] [PubMed]
- Deutsche Wirbelsäulengesellschaft e.V., Deutsche Gesellschaft für Orthopädie und Orthopädische Chirurgie e.V. S2k-Leitlinie Diagnostik und Therapie der Spondylodiszitis (AWMF Registernummer 151-001), Version 1.0 (26.08.2020). 2020. Available online: https://register.awmf.org/de/leitlinien/detail/151-001 (accessed on 16 May 2024).
- Kowalski, T.J.; Berbari, E.F.; Huddleston, P.M.; Steckelberg, J.M.; Osmon, D.R. Do follow-up imaging examinations provide useful prognostic information in patients with spine infection? Clin. Infect. Dis. 2006, 43, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Euba, G.; Narváez, J.A.; Nolla, J.M.; Murillo, O.; Narváez, J.; Gómez-Vaquero, C.; Ariza, J. Long-term clinical and radiological magnetic resonance imaging outcome of abscess-associated spontaneous pyogenic vertebral osteomyelitis under conservative management. Semin. Arthritis Rheum. 2008, 38, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Pro Implant Foundation. Pocket Guide Diagnose & Behandlung von Wirbelsäuleninfektionen, Version 4. Available online: https://pro-implant.org/tools/pocket-guide (accessed on 16 May 2024).
- Deutsche Gesellschaft für Unfallchirurgie e.V. S3-Leitlinie Polytrauma/Schwerverletzten-Behandlung (AWMF Registernummer 187-023), Version 4.0 (31.12.2022). 2022. Available online: https://www.awmf.org/leitlinien/detail/ll/187-023.html (accessed on 16 May 2024).
- Deutsche Sepsis-Hilfe e.V. S3-Leitlinie Sepsis-Prävention, Diagnose, Therapie und Nachsorge (AWMF Registernummer 079-001), Version 3.1 (31.12.2018). 2018. Available online: https://register.awmf.org/de/leitlinien/detail/079-001 (accessed on 16 May 2024).
- Jeong, S.-J.; Choi, S.-W.; Youm, J.-Y.; Kim, H.-W.; Ha, H.-G.; Yi, J.-S. Microbiology and epidemiology of infectious spinal disease. J. Korean Neurosurg. Soc. 2014, 56, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Krogsgaard, M.R.; Wagn, P.; Bengtsson, J. Epidemiology of acute vertebral osteomyelitis in Denmark: 137 cases in Denmark 1978-1982, compared to cases reported to the National Patient Register 1991–1993. Acta Orthop. Scand. 1998, 69, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, T.; Chikuda, H.; Yasunaga, H.; Horiguchi, H.; Fushimi, K.; Saita, K. Incidence and risk factors for mortality of vertebral osteomyelitis: A retrospective analysis using the Japanese diagnosis procedure combination database. BMJ Open 2013, 3, e002412. [Google Scholar] [CrossRef] [PubMed]
- Grammatico, L.; Baron, S.; Rusch, E.; Lepage, B.; Surer, N.; Desenclos, J.C.; Besnier, J.M. Epidemiology of vertebral osteomyelitis (VO) in France: Analysis of hospital-discharge data 2002–2003. Epidemiol. Infect. 2008, 136, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Loibl, M.; Stoyanov, L.; Doenitz, C.; Brawanski, A.; Wiggermann, P.; Krutsch, W.; Nerlich, M.; Oszwald, M.; Neumann, C.; Salzberger, B.; et al. Outcome-related co-factors in 105 cases of vertebral osteomyelitis in a tertiary care hospital. Infection 2014, 42, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Bernard, L.; Dinh, A.; Ghout, I.; Simo, D.; Zeller, V.; Issartel, B.; Le Moing, V.; Belmatoug, N.; Lesprit, P.; Bru, J.P.; et al. Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: An open-label, non-inferiority, randomised, controlled trial. Lancet 2015, 385, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Park, K.-H.; Kim, D.Y.; Lee, Y.-M.; Lee, M.S.; Kang, K.-C.; Lee, J.-H.; Park, S.Y.; Moon, C.; Chong, Y.P.; Kim, S.-H.; et al. Selection of an appropriate empiric antibiotic regimen in hematogenous vertebral osteomyelitis. PLoS ONE 2019, 14, e0211888. [Google Scholar] [CrossRef] [PubMed]
- Ahn, K.-S.; Kang, C.H.; Hong, S.-J.; Kim, B.H.; Shim, E. The correlation between follow-up MRI findings and laboratory results in pyogenic spondylodiscitis. BMC Musculoskelet. Disord. 2020, 21, 428. [Google Scholar] [CrossRef] [PubMed]
- Lora-Tamayo, J.; Euba, G.; Narváez, J.A.; Murillo, O.; Verdaguer, R.; Sobrino, B.; Narváez, J.; Nolla, J.M.; Ariza, J. Changing trends in the epidemiology of pyogenic vertebral osteomyelitis: The impact of cases with no microbiologic diagnosis. Semin. Arthritis Rheum. 2011, 41, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Colmenero, J.D.; Jiménez-Mejías, M.E.; Sanchez-Lora, F.J.; Reguera, J.M.; Palomino-Nicas, J.; Martos, F.; Garcia de las Heras, J.; Pachon, J. Pyogenic, tuberculous, and brucellar vertebral osteomyelitis: A descriptive and comparative study of 219 cases. Ann. Rheum. Dis. 1997, 56, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Hellerau, K.; Baade, N.; Günther, M.; Scholten, N.; Lindemann, C.H.; Leisse, C.; Oberröhrmann, C.; Peter, S.; Jung, N.; Suarez, I.; et al. Outpatient parenteral antimicrobial therapy (OPAT) in Germany: Insights and clinical outcomes from the K-APAT cohort study. Infection 2024, 1–8, Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]

| Variable | All Patients (N = 66) | Conservative (N = 54) | Surgery (N = 12) |
|---|---|---|---|
| Age, Mean ± SD | 73.7 ± 9.7 | 74.6 ± 12.9 | 73.3 ± 8.1 |
| Gender, n (%) | |||
| Male | 36 (54.5%) | 27 (50.0%) | 9 (75.0%) |
| Female | 30 (45.5%) | 27 (50.0%) | 3 (25.0%) |
| Charlson Index, Mean ± SD | 5.97 ± 3.25 | 6.13 ± 3.35 | 5.25 ± 2.77 |
| Charlson Index, n (%) | |||
| 1–4 | 24 (36.4%) | 19 (35.2%) | 5 (41.7%) |
| 5–8 | 27 (40.9%) | 21 (38.9%) | 6 (50.0%) |
| >8 | 15 (22.7%) | 14 (25.9%) | 1 (8.3%) |
| CRP uptake, n (%) | |||
| Elevated >50 mg/L | 41 (62.1%) | 34 (63.0%) | 7 (58.3%) |
| Leukocytes uptake, n (%) | |||
| Elevated (>10,000) | 29 (43.9%) | 23 (42.6%) | 6 (50.0%) |
| Detection of Pathogen, n (%) * | 21 (31.8%) | 14 (25.9%) | 7 (58.3%) |
| Type of Pathogen, n (%) | |||
| Staph. aureus | 8 (38.1%) | 7 (50.0%) | 1 (14.3%) |
| Other pathogen | 6 (28.6%) | 2 (14.3%) | 4 (57.1%) |
| Not documented | 7 (33.3%) | 5 (35.7%) | 2 (28.6%) |
| Localization, n (%) | |||
| Cervical spine | 5 (7.6%) | 4 (7.4%) | 1 (8.3%) |
| Thoracic spine | 13 (19.7%) | 8 (14.8%) | 5 (41.7%) |
| Lumbar spine | 48 (72.7%) | 42 (77.8%) | 6 (50.0%) |
| Focus of infection, n (%) | |||
| Indeterminate | 26 (39.4%) | 19 (35.2%) | 6 (50.0%) |
| Urogenital | 15 (22.7%) | 14 (25.9%) | 1 (8.3%) |
| Extremities | 7 (10.6%) | 7 (13.0%) | 0 |
| Pulmonary | 5 (7.6%) | 5 (9.3%) | 0 |
| Oral | 5 (7.6%) | 4 (7.4%) | 1 (8.3%) |
| Implant | 4 (6.1%) | 2 (3.7%) | 2 (16.7%) |
| Local | 2 (3.0%) | 2 (3.7%) | 0 |
| Abdominal | 2 (3.0%) | 1 (1.9%) | 1 (8.3%) |
| Follow-up MRI, n (%) | 46 (69.7%) | 40 (74.1%) | 6 (50.0%) |
| All Patients (N = 12) | Follow-Up MRI (N = 6) | No Follow-Up MRI (N = 6) | ||
|---|---|---|---|---|
| Reasons for Conversion, n (%) | ||||
| Primary Reason | Secondary Reason | |||
| Initial MRI | Clinical finding | 3 (25.0%) | 3 (50.0%) | |
| Clinical finding | Initial MRI | 3 (25.0%) | 3 (50.0%) | |
| Follow-up MRI | Clinical finding | 3 (25.0%) | 3 (50.0%) | |
| Clinical finding | Follow-up MRI | 3 (25.0%) | 3 (50.0%) | |
| Variable | All Patients (N = 66) | Conservative (N = 54) | Surgery (N = 12) |
|---|---|---|---|
| Hospital stay | |||
| Length of stay, Mean ± SD * | 24.2 ± 10.1 | 22.2 ± 8.0 | 33.6 ± 12.9 |
| In-hospital mortality, n (%) | 2 (3.0%) | 2 (3.7%) | 0 |
| Labor parameters | |||
| CRP at admission, Mean ± SD | 106.2 ± 111.7 | 111.9 ± 116.2 | 80.5 ± 88.8 |
| CRP at discharge, Mean ± SD | 44.1 ± 38.5 | 44.4 ± 39.0 | 42.7 ± 37.5 |
| CRP at admission (>50 mg/L), n (%) | 41 (62.1%) | 34 (63.0%) | 7 (58.3%) |
| CRP at discharge (>50 mg/L), n (%) | 22 (33.3%) | 19 (35.2%) | 3 (25.0%) |
| Leukocytes at admission, Mean ± SD | 10.1 ± 4.1 | 10.1 ± 4.3 | 10.2 ± 3.1 |
| Leukocytes at discharge, Mean ± SD | 7.0 ± 2.9 | 7.1 ± 3.0 | 6.9 ± 2.6 |
| Leukocytes at admission (>10,000), n (%) | 29 (43.9%) | 23 (42.6%) | 6 (50.0%) |
| Leukocytes at discharge (>10,000), n (%) | 8 (12.1%) | 6 (11.1%) | 2 (16.7%) |
| Duration of antibiosis iv, Mean ± SD | 24.6 ± 18.2 | 23.5 ± 18.7 | 29.7 ± 15.5 |
| Radiological diagnosis (Follow-up), n (%) | |||
| Success of therapy ** | 19 (50.0%) | 15 (46.9%) | 4 (66.7%) |
| Failure of therapy | 19 (50.0%) | 17 (53.1%) | 2 (33.3%) |
| Follow-up treatment, n (%) | |||
| Nursing home | 37 (56.1%) | 31 (57.4%) | 6 (50.0%) |
| Ambulant/post-hospital curative treatment | 23 (34.8%) | 17 (31.5%) | 6 (50.0%) |
| Acute inpatient follow-up treatment | 4 (6.1%) | 4 (7.4%) | 0 |
| Deceased | 2 (3.0%) | 2 (3.7%) | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolster, M.; Hönning, A.; Käckenmester, W.; Goy, J.; Ekkernkamp, A.; Spranger, N. Applying the German S2k-Guideline for Diagnosis and Treatment of Spondylodiscitis—A 5-Year Retrospective Evaluation of Patients without Neurological Symptoms. Diagnostics 2024, 14, 1098. https://doi.org/10.3390/diagnostics14111098
Kolster M, Hönning A, Käckenmester W, Goy J, Ekkernkamp A, Spranger N. Applying the German S2k-Guideline for Diagnosis and Treatment of Spondylodiscitis—A 5-Year Retrospective Evaluation of Patients without Neurological Symptoms. Diagnostics. 2024; 14(11):1098. https://doi.org/10.3390/diagnostics14111098
Chicago/Turabian StyleKolster, Moritz, Alexander Hönning, Wiebke Käckenmester, Janet Goy, Axel Ekkernkamp, and Nikolai Spranger. 2024. "Applying the German S2k-Guideline for Diagnosis and Treatment of Spondylodiscitis—A 5-Year Retrospective Evaluation of Patients without Neurological Symptoms" Diagnostics 14, no. 11: 1098. https://doi.org/10.3390/diagnostics14111098
APA StyleKolster, M., Hönning, A., Käckenmester, W., Goy, J., Ekkernkamp, A., & Spranger, N. (2024). Applying the German S2k-Guideline for Diagnosis and Treatment of Spondylodiscitis—A 5-Year Retrospective Evaluation of Patients without Neurological Symptoms. Diagnostics, 14(11), 1098. https://doi.org/10.3390/diagnostics14111098





