Trajectory of Diastolic Function after Heart Transplantation as Assessed by Left Atrial Deformation Analysis
Abstract
1. Introduction
2. Methods
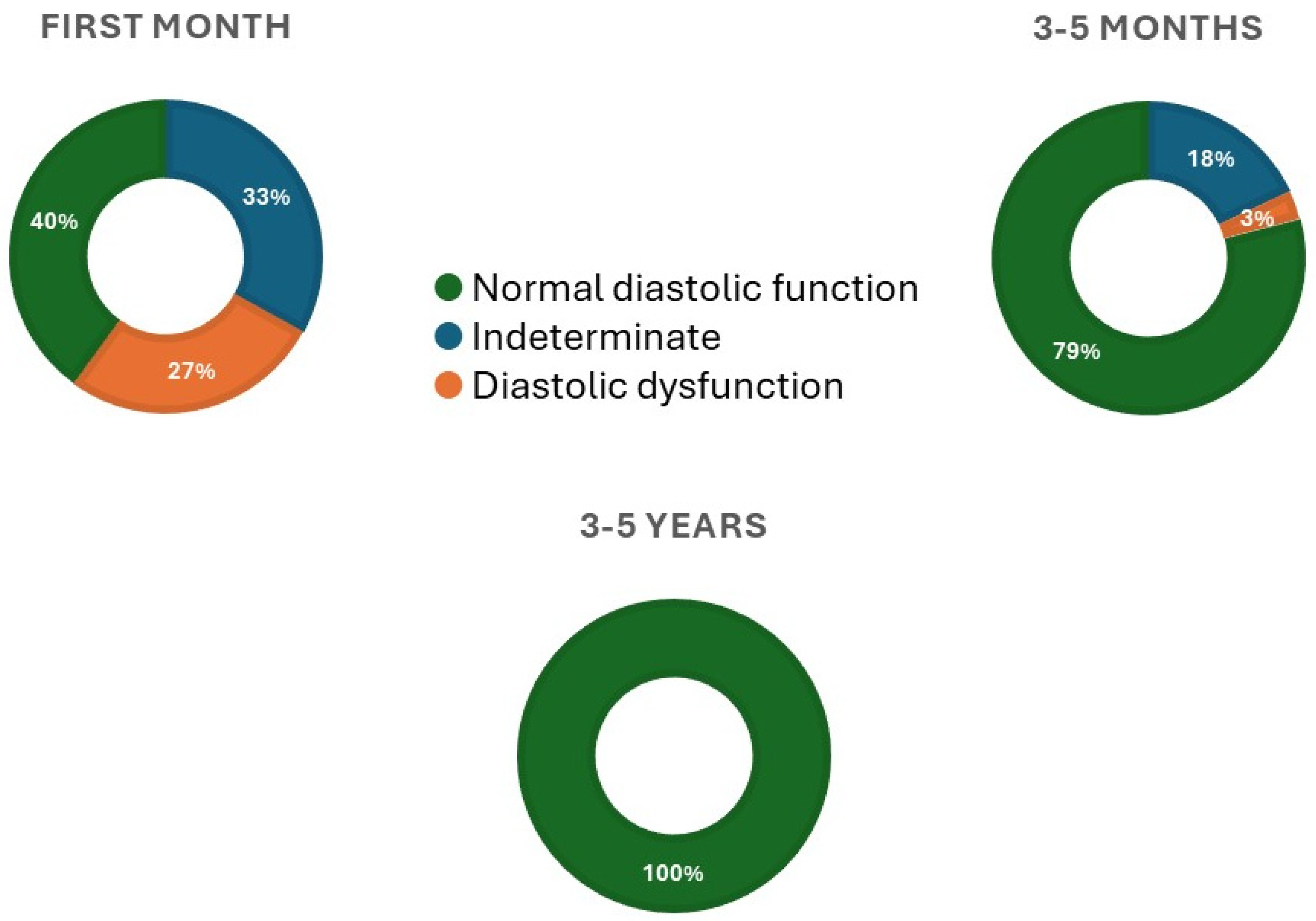
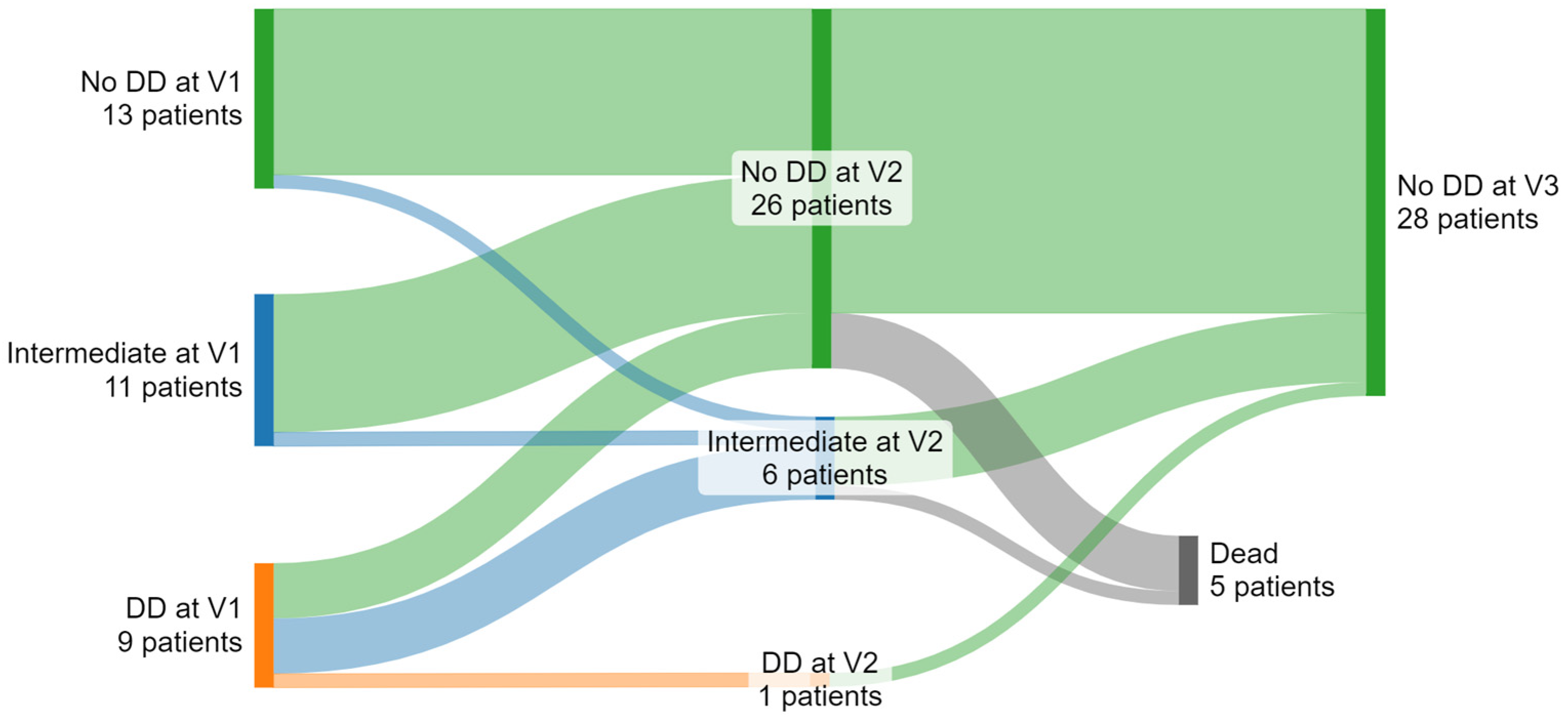
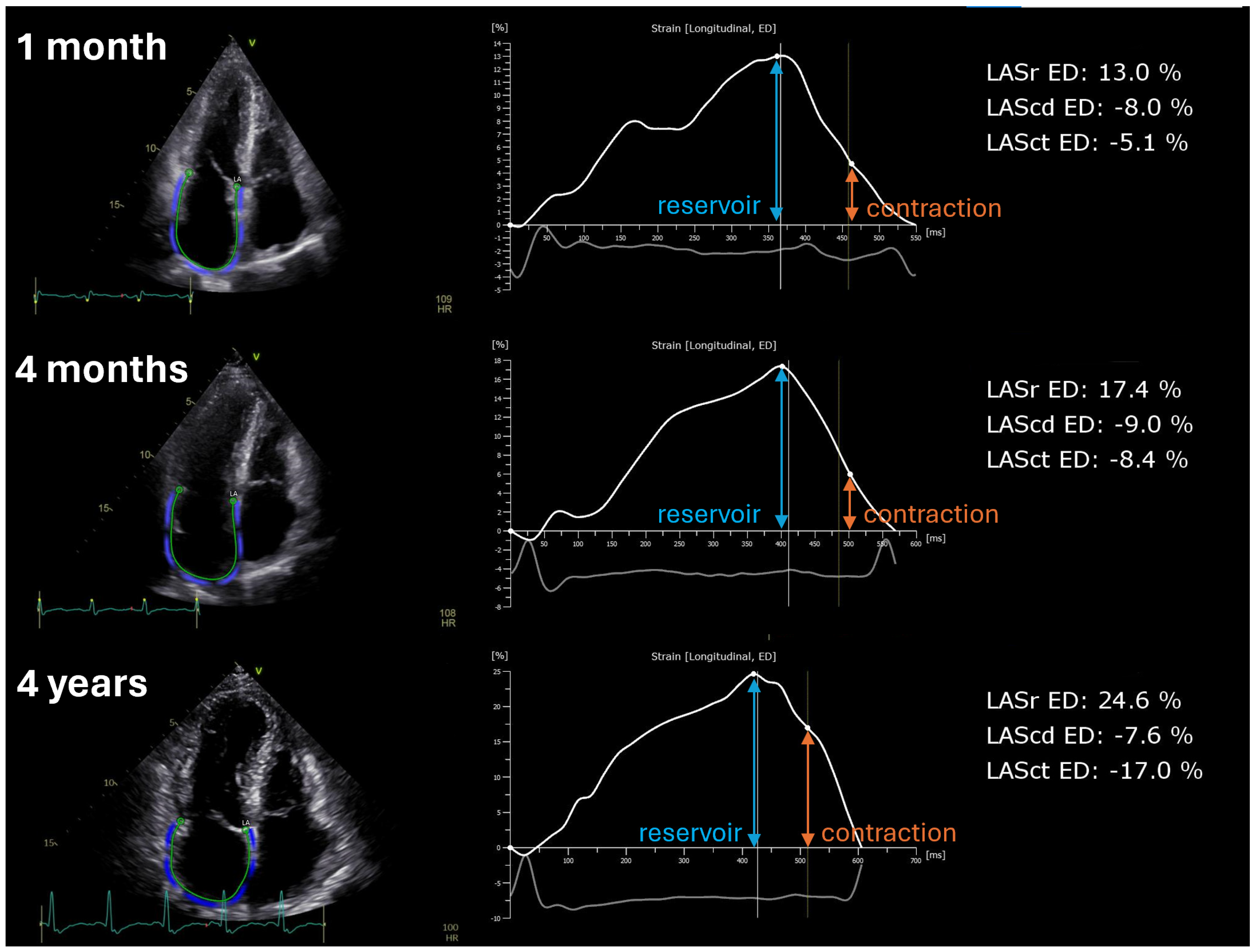
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tallaj, J.A.; Kirklin, J.K.; Brown, R.N.; Rayburn, B.K.; Bourge, R.C.; Benza, R.L.; Pinderski, L.; Pamboukian, S.; McGiffin, D.C.; Naftel, D.C. Post-heart transplant diastolic dysfunction is a risk factor for mortality. J. Am. Coll. Cardiol. 2007, 50, 1064–1069. [Google Scholar] [CrossRef] [PubMed]
- Sciaccaluga, C.; Fusi, C.; Landra, F.; Barilli, M.; Lisi, M.; Mandoli, G.E.; D’ascenzi, F.; Focardi, M.; Valente, S.; Cameli, M. Diastolic function in heart transplant: From physiology to echocardiographic assessment and prognosis. Front. Cardiovasc. Med. 2022, 9, 969270. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F., 3rd; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef] [PubMed]
- Zhubi Bakija, F.; Bagyura, Z.; Fábián, A.; Ferencz, A.; Kiss, L.; Szenczi, O.; Vadas, R.; Dósa, E.; Nguyen, D.T.; Csobay-Novák, C.; et al. Long-term prognostic value of left atrial longitudinal strain in an elderly community-based cohort. Geroscience 2023, 45, 613–625. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Diego, S.; Ruiz-Ortiz, M.; Delgado-Ortega, M.; Kim, J.; Weinsaft, J.W.; Sánchez-Fernández, J.J.; Ortega-Salas, R.; Carnero-Montoro, L.; Carrasco-Ávalos, F.; López-Aguilera, J.; et al. The Role of Left Atrial Longitudinal Strain in the Diagnosis of Acute Cellular Rejection in Heart Transplant Recipients. J. Clin. Med. 2022, 11, 4987. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, R.; Rodrigues, A.C.T.; Vieira, M.L.C.; Fischer, C.H.; Monaco, C.G.; Filho, E.B.L.; Bacal, F.; Caixeta, A.; Morhy, S.S. Evaluation of the myocardial deformation in the diagnosis of rejection after heart transplantation. Front. Cardiovasc. Med. 2022, 9, 991016. [Google Scholar] [CrossRef] [PubMed]
- Cruz, C.; Hajjar, L.A.; Bacal, F.; Lofrano-Alves, M.S.; Lima, M.S.M.; Abduch, M.C.; Vieira, M.L.C.; Chiang, H.P.; Salviano, J.B.C.; da Silva Costa, I.B.S.; et al. Usefulness of speckle tracking echocardiography and biomarkers for detecting acute cellular rejection after heart transplantation. Cardiovasc. Ultrasound. 2021, 19, 6. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Xie, Y.; Qiao, W.; Tian, F.; Sun, W.; Wang, Y.; Wu, C.; Li, H.; Yi, L.; Zhong, Y.; et al. Impaired left atrial function in clinically well heart transplant patients. Int. J. Cardiovasc. Imaging 2021, 37, 1937–1945. [Google Scholar] [CrossRef] [PubMed]
- Pathan, F.; D’Elia, N.; Nolan, M.T.; Marwick, T.H.; Negishi, K. Normal Ranges of Left Atrial Strain by Speckle-Tracking Echocardiography: A Systematic Review and Meta-Analysis. J. Am. Soc. Echocardiogr. 2017, 30, 59–70.e8. [Google Scholar] [CrossRef] [PubMed]
- Velleca, A.; Shullo, M.A.; Dhital, K.; Azeka, E.; Colvin, M.; DePasquale, E.; Farrero, M.; García-Guereta, L.; Jamero, G.; Khush, K.; et al. The International Society for Heart and Lung Transplantation (ISHLT) guidelines for the care of heart transplant recipients. J. Heart Lung Transplant. 2023, 42, e1–e141. [Google Scholar] [CrossRef] [PubMed]
| HTX Patients at 1st Assessment (n = 33) | |
|---|---|
| Age (years) | 52 (46; 58) |
| Sex [female, n (%)] | 9 (27%) |
| Height (cm) | 176 (168; 182) |
| Weight (kg) | 77 (69; 84) |
| BMI (kg/m2) | 25.0 (22.0; 29.7) |
| BSA (m2) | 1.94 (1.82; 2.06) |
| SBP (mmHg) | 117 (100; 130) |
| DBP (mmHg) | 75 (62; 80) |
| HR (1/min) | 80 (76; 94) |
| Preoperative PVR (Wood units) | 2.8 (1.9; 4.4) |
| Donor age (years) | 46 (37; 55) |
| Donor sex [Female, n (%)] | 11 (33%) |
| Etiology | |
| Nonischemic dilated cardiomyopathy [n (%)] | 16 (49%) |
| Ischemic dilated cardiomyopathy [n (%)] | 10 (30%) |
| Other, nonspecified [n (%)] | 7 (21%) |
| Comorbidities | |
| Systemic hypertension [n (%)] | 14 (42%) |
| Diabetes mellitus [n (%)] | 8 (24%) |
| COPD/asthma [n (%)] | 6 (18%) |
| 1st Assessment | 2nd Assessment | 3rd Assessment | Overall p | |
|---|---|---|---|---|
| Days since HTX | 17 (13; 22) | 115 (101; 125) | 1492 (1377; 1560) | NA |
| NT-proBNP (pg/mL) | 4560 (2421; 7205) ab | 711 (517; 1098) ac | 374 (177; 717) bc | <0.001 |
| GFR (mL/min/1.73 m2) | 82 (55; 90) | 69 (49; 84) | 64 (47; 88) | 0.268 |
| Echocardiography | ||||
| LVIDd (mm) | 45.0 (42.0; 48.0) | 44.5 (42.0; 48.0) | 46.0 (43.5; 48.0) | 0.809 |
| IVSd (mm) | 12.0 (11.0; 14.0) b | 13.0 (11.0; 14.0) c | 11.0 (10.0; 13.0) bc | 0.004 |
| PWd (mm) | 11.0 (10.0; 11.0) | 10.0 (9.0; 11.0) | 10.0 (9.3; 12.0) | 0.103 |
| RWT (%) | 46.8 (43.0; 52.4) | 44.7 (38.1; 50.0) | 45.5 (40.4; 52.5) | 0.058 |
| LVMi (g/m2) | 102.4 (80.4; 116.1) | 92.1 (82.0; 107.8) | 89.0 (75.3; 102.8) | 0.275 |
| LVEDVi (mL/m2) | 48.8 (39.0; 56.2) | 47.7 (41.4; 52.5) | 45.3 (41.5; 53.9) | 0.446 |
| LVESVi (mL/m2) | 17.5 (13.3; 21.8) | 17.4 (15.1; 20.3) | 19.4 (16.9; 23.6) | 0.331 |
| LVEF (%) | 64.0 (60.0; 66.0) b | 62.0 (60.0; 64.0) c | 57.0 (55.0; 60.0) bc | <0.001 |
| LV GLS (%) | −12.4 (−14.5; −10.5) | −12.6 (−15.3; −9.8) | −15.3 (−18.1; −12.2) | 0.070 |
| RVd (mm) | 33.0 (29.5; 36.0) | 32.0 (29.0; 34.5) | 36.0 (33.0; 38.0) | 0.058 |
| TAPSE (mm) | 11.0 (9.0; 14.0) a | 14.0 (12.0; 16.0) a | 13.0 (11.3; 15.0) | 0.013 |
| TR Vmax (m/s) | 2.6 (2.5; 2.8) | 2.6 (2.3; 2.7) c | 2.1 (1.7; 2.5) c | <0.001 |
| E (cm/s) | 95.0 (84.0; 119.0) ab | 85.0 (69.5; 98.5) a | 84.0 (67.0; 94.0) b | 0.001 |
| A (cm/s) | 48.0 (42.0; 70.0) | 47.0 (42.0; 65.0) | 43.5 (35.0; 54.3) | 0.786 |
| E/A | 2.03 (1.50; 2.35) | 1.61 (1.48; 1.91) | 1.76 (1.41; 2.22) | 0.058 |
| DT (ms) | 163.0 (137.0; 182.5) | 163.0 (150.0; 181.5) | 171.0 (151.0; 200.0) | 0.502 |
| Mitral lateral s′ (cm/s) | 10.0 (9.0; 11.0) | 11.0 (9.0; 12.0) | 10.0 (9.2; 11.5) | 0.698 |
| Mitral lateral e′ (cm/s) | 11.0 (9.0; 13.5) ab | 15.0 (11.0; 16.0) a | 15.2 (13.2; 16.3) b | 0.001 |
| Mitral lateral a′ (cm/s) | 5.0 (4.0; 7.0) ab | 7.0 (5.0; 8.7) ac | 8.3 (6.9; 9.5) bc | <0.001 |
| Mitral medial s′ (cm/s) | 8.0 (7.0; 9.0) | 9.0 (8.0; 10.0) | 8.7 (7.5; 9.3) | 0.617 |
| Mitral medial e′ (cm/s) | 7.0 (6.0; 8.0) b | 8.0 (7.0; 9.0) | 8.5 (7.7; 9.5) b | 0.002 |
| Mitral medial a′ (cm/s) | 6.3 (6.0; 8.0) b | 8.0 (5.7; 8.0) | 8.8 (7.6; 9.6) b | 0.003 |
| E/e′ average | 10.5 (8.7; 12.5) ab | 7.9 (6.6; 9.1) a | 6.5 (5.8; 8.0) b | 0.002 |
| LAVi (ml/m2) | 53.1 (43.9; 67.9) b | 49.0 (37.5; 59.6) c | 33.6 (28.6; 40.6) bc | <0.001 |
| LA reservoir strain ED (%) | 13.0 (7.0; 16.3) ab | 14.9 (13.1; 18.2) a | 20.0 (15.5; 21.8) b | 0.003 |
| LA conduit strain ED (%) | −8.5 (−13.4; −4.35) | −9.3 (−13.2; −5.9) | −10.9 (−12.6; −9.0) | 0.195 |
| LA contraction strain ED (%) | −4.3 (−5.8; −1.2) b | −4.5 (−8.9; −1.4) c | −8.1 (−11.0; −5.8) bc | 0.015 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Edvi, B.; Assabiny, A.; Teszák, T.; Tolvaj, M.; Fábián, A.; Hartyánszky, I.; Pólos, M.; Lakatos, B.K.; Vágó, H.; Sax, B.; et al. Trajectory of Diastolic Function after Heart Transplantation as Assessed by Left Atrial Deformation Analysis. Diagnostics 2024, 14, 1136. https://doi.org/10.3390/diagnostics14111136
Edvi B, Assabiny A, Teszák T, Tolvaj M, Fábián A, Hartyánszky I, Pólos M, Lakatos BK, Vágó H, Sax B, et al. Trajectory of Diastolic Function after Heart Transplantation as Assessed by Left Atrial Deformation Analysis. Diagnostics. 2024; 14(11):1136. https://doi.org/10.3390/diagnostics14111136
Chicago/Turabian StyleEdvi, Borbála, Alexandra Assabiny, Tímea Teszák, Máté Tolvaj, Alexandra Fábián, István Hartyánszky, Miklós Pólos, Bálint Károly Lakatos, Hajnalka Vágó, Balázs Sax, and et al. 2024. "Trajectory of Diastolic Function after Heart Transplantation as Assessed by Left Atrial Deformation Analysis" Diagnostics 14, no. 11: 1136. https://doi.org/10.3390/diagnostics14111136
APA StyleEdvi, B., Assabiny, A., Teszák, T., Tolvaj, M., Fábián, A., Hartyánszky, I., Pólos, M., Lakatos, B. K., Vágó, H., Sax, B., Merkely, B., & Kovács, A. (2024). Trajectory of Diastolic Function after Heart Transplantation as Assessed by Left Atrial Deformation Analysis. Diagnostics, 14(11), 1136. https://doi.org/10.3390/diagnostics14111136





