Hyperspectral Imaging Detects Clitoral Vascular Issues in Gender-Affirming Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Surgical Technique
2.3. HSI Imaging
2.4. Statistics
3. Results
3.1. Study Cohort
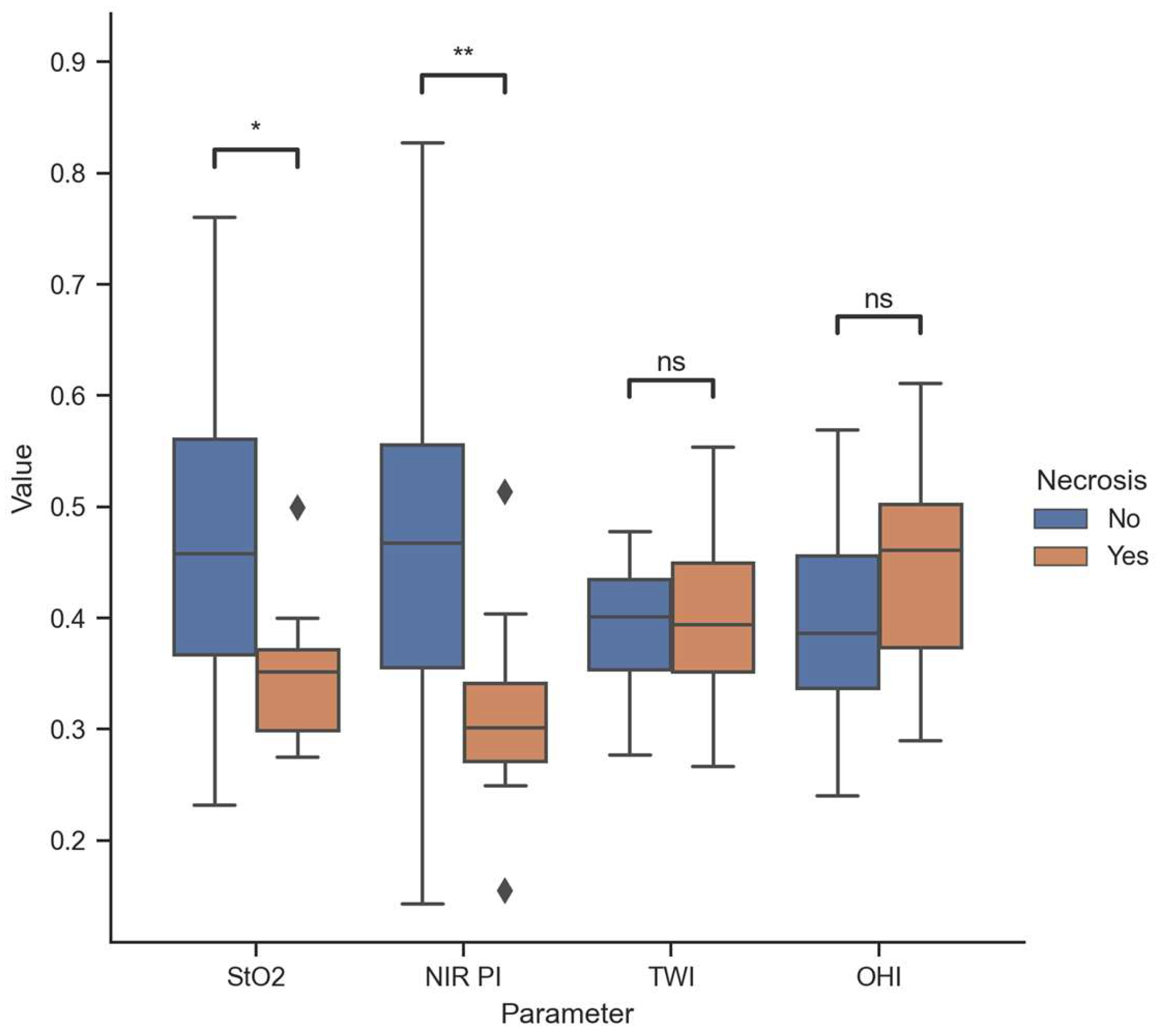
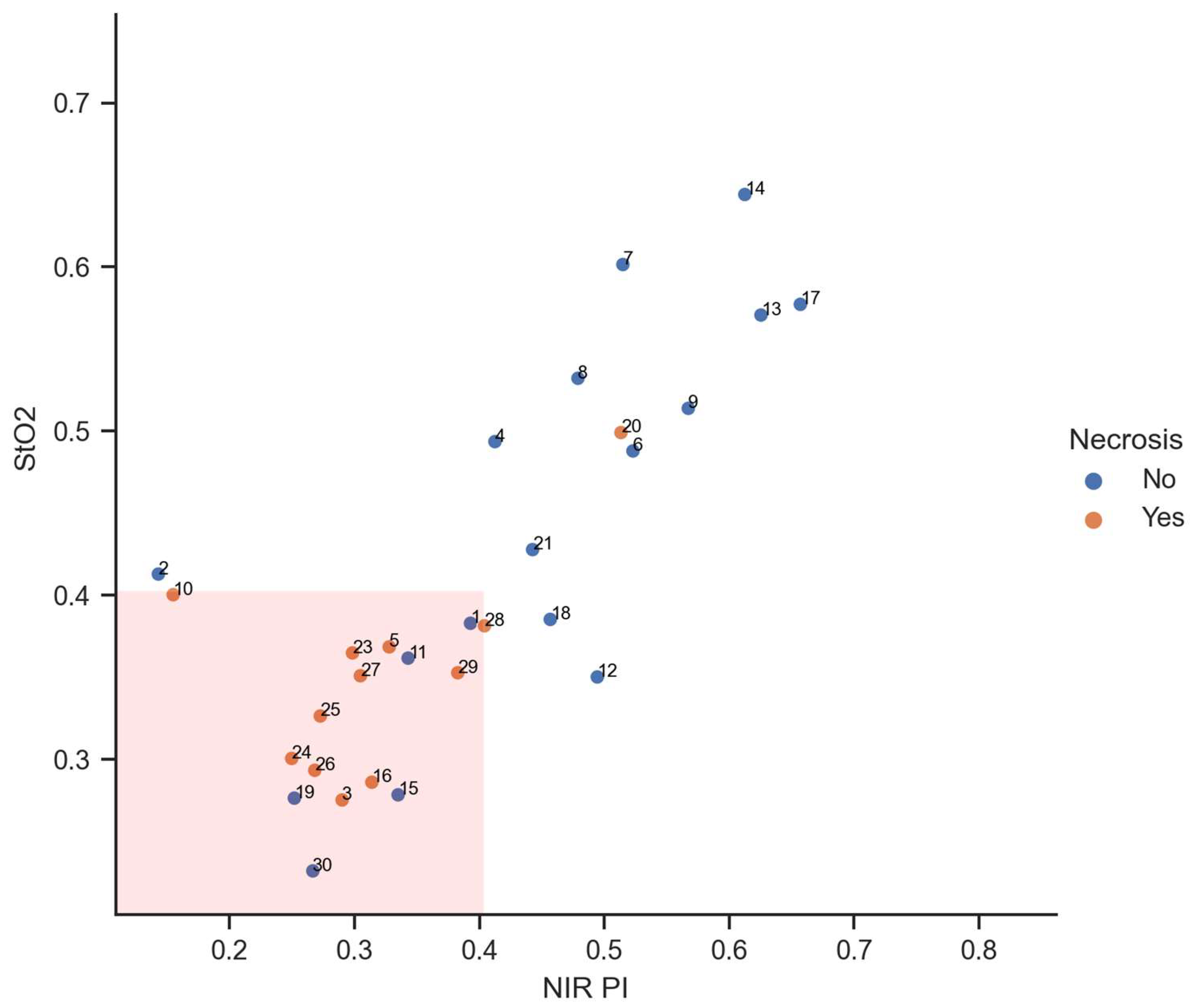
3.2. HSI Data
3.3. Diagnostic Accuracy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, Q.; He, X.; Wang, Y.; Liu, H.; Xu, D.; Guo, F. Review of spectral imaging technology in biomedical engineering: Achievements and challenges. J. Biomed. Opt. 2013, 18, 100901. [Google Scholar] [CrossRef] [PubMed]
- Schultz, R.A.; Nielsen, T.; Zavaleta, J.R.; Ruch, R.; Wyatt, R.; Garner, H.R. Hyperspectral imaging: A novel approach for microscopic analysis. Cytometry 2001, 43, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Smith, R.T.; Tkaczyk, T.S. Snapshot hyperspectral retinal camera with the Image Mapping Spectrometer (IMS). Biomed. Opt. Express 2012, 3, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Guenot, D.; Alexander, J.; Selvander, M. Compact snapshot hyperspectral camera for ophthalmology. Opt. Contin. 2024, 3, 565. [Google Scholar] [CrossRef]
- Holmer, A.; Tetschke, F.; Marotz, J.; Malberg, H.; Markgraf, W.; Thiele, C.; Kulcke, A. Oxygenation and perfusion monitoring with a hyperspectral camera system for chemical based tissue analysis of skin and organs. Physiol. Meas. 2016, 37, 2064–2078. [Google Scholar] [CrossRef] [PubMed]
- Holmer, A.; Marotz, J.; Wahl, P.; Dau, M.; Kämmerer, P.W. Hyperspectral imaging in perfusion and wound diagnostics—Methods and algorithms for the determination of tissue parameters. Biomed. Tech. 2018, 63, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Aloupogianni, E.; Ishikawa, M.; Kobayashi, N.; Obi, T. Hyperspectral and multispectral image processing for gross-level tumor detection in skin lesions: A systematic review. J. Biomed. Opt. 2022, 27, 060901. [Google Scholar] [CrossRef]
- Jayachandran, M.; Rodriguez, S.; Solis, E.; Lei, J.; Godavarty, A. Critical Review of Noninvasive Optical Technologies for Wound Imaging. Adv. Wound Care 2016, 5, 349–359. [Google Scholar] [CrossRef]
- Lemmens, S.; van Eijgen, J.; van Keer, K.; Jacob, J.; Moylett, S.; de Groef, L.; Vancraenendonck, T.; de Boever, P.; Stalmans, I. Hyperspectral Imaging and the Retina: Worth the Wave? Transl. Vis. Sci. Technol. 2020, 9, 9. [Google Scholar] [CrossRef]
- Schulz, T.; Marotz, J.; Seider, S.; Langer, S.; Leuschner, S.; Siemers, F. Burn depth assessment using hyperspectral imaging in a prospective single center study. Burns 2022, 48, 1112–1119. [Google Scholar] [CrossRef]
- Schulz, T.; Nuwayhid, R.; Houschyar, K.S.; Langer, S.; Kohler, L. Diagnostical accuracy of hyperspectral imaging after free flap surgery. J. Plast. Surg. Hand Surg. 2023, 58, 48–55. [Google Scholar] [CrossRef]
- Barberio, M.; Benedicenti, S.; Pizzicannella, M.; Felli, E.; Collins, T.; Jansen-Winkeln, B.; Marescaux, J.; Viola, M.G.; Diana, M. Intraoperative Guidance Using Hyperspectral Imaging: A Review for Surgeons. Diagnostics 2021, 11, 2066. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Mao, X.; Wang, Y.; Tao, X.; Chu, J.; Li, Q. Automatic generation of pathological benchmark dataset from hyperspectral images of double stained tissues. Opt. Laser Technol. 2023, 163, 109331. [Google Scholar] [CrossRef]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 0-89042-555-8. [Google Scholar]
- Meerwijk, E.L.; Sevelius, J.M. Transgender Population Size in the United States: A Meta-Regression of Population-Based Probability Samples. Am. J. Public. Health 2017, 107, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Dhejne, C.; Öberg, K.; Arver, S.; Landén, M. An analysis of all applications for sex reassignment surgery in Sweden, 1960-2010: Prevalence, incidence, and regrets. Arch. Sex. Behav. 2014, 43, 1535–1545. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.; Honig, S.C. Gender-Affirming Surgery: Current Concepts. Curr. Urol. Rep. 2018, 19, 62. [Google Scholar] [CrossRef]
- Hess, J.; Hess-Busch, Y.; Kronier, J.; Rübben, H.; Rossi Neto, R. Modified Preparation of the Neurovascular Bundle in Male to Female Transgender Patients. Urol. Int. 2016, 96, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Coleman, E.; Radix, A.E.; Bouman, W.P.; Brown, G.R.; de Vries, A.L.C.; Deutsch, M.B.; Ettner, R.; Fraser, L.; Goodman, M.; Green, J.; et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int. J. Transgend. Health 2022, 23, S1–S259. [Google Scholar] [CrossRef]
- Abraham, F. Genitalumwandlung an zwei männlichen Transvestiten. Z. Sex. Sex. 1931, 18, 223–226. [Google Scholar]
- Sohn, M.; Bosinski, H.A.G. Gender identity disorders: Diagnostic and surgical aspects. J. Sex. Med. 2007, 4, 1193–1207, quiz 1208. [Google Scholar] [CrossRef]
- Eicher, W. Transsexualität—Standards of Care. Zentralblatt Gynäkologie 1995, 117, 61–66. [Google Scholar]
- Salvador, J.; Massuda, R.; Andreazza, T.; Koff, W.J.; Silveira, E.; Kreische, F.; de Souza, L.; de Oliveira, M.H.; Rosito, T.; Fernandes, B.S.; et al. Minimum 2-year follow up of sex reassignment surgery in Brazilian male-to-female transsexuals. Psychiatry Clin. Neurosci. 2012, 66, 371–372. [Google Scholar] [CrossRef] [PubMed]
- Hess, J.; Rossi Neto, R.; Panic, L.; Rübben, H.; Senf, W. Satisfaction with male-to-female gender reassignment surgery. Dtsch. Arztebl. Int. 2014, 111, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, A.A. Sexuality before and after male-to-female sex reassignment surgery. Arch. Sex. Behav. 2005, 34, 147–166. [Google Scholar] [CrossRef] [PubMed]
- Karim, R.B.; Hage, J.J.; Mulder, J.W. Neovaginoplasty in male transsexuals: Review of surgical techniques and recommendations regarding eligibility. Ann. Plast. Surg. 1996, 37, 669–675. [Google Scholar] [CrossRef]
- de Vries, A.L.C.; McGuire, J.K.; Steensma, T.D.; Wagenaar, E.C.F.; Doreleijers, T.A.H.; Cohen-Kettenis, P.T. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics 2014, 134, 696–704. [Google Scholar] [CrossRef]
- Meier, A.C.; Papadopulos, N. Lebensqualität nach geschlechtsangleichenden Operationen—Eine Übersicht. Handchir. Mikrochir. Plast. Chir. 2021, 53, 556–563. [Google Scholar] [CrossRef]
- Baranyi, A.; Piber, D.; Rothenhäusler, H.-B. Mann-zu-Frau-Transsexualismus. Ergebnisse geschlechtsangleichender Operationen in einer biopsychosozialen Perspektive. Wien. Med. Wochenschr. 2009, 159, 548–557. [Google Scholar] [CrossRef]
- Kraemer, B.; Delsignore, A.; Schnyder, U.; Hepp, U. Body image and transsexualism. Psychopathology 2008, 41, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Weitze, C.; Osburg, S. Transsexualism in Germany: Empirical data on epidemiology and application of the German Transsexuals' Act during its first ten years. Arch. Sex. Behav. 1996, 25, 409–425. [Google Scholar] [CrossRef]
- Liu, Z.-W.; Faddegon, S.; Olweny, E.O.; Best, S.L.; Jackson, N.; Raj, G.V.; Zuzak, K.J.; Cadeddu, J.A. Renal oxygenation during partial nephrectomy: A comparison between artery-only occlusion versus artery and vein occlusion. J. Endourol. 2013, 27, 470–474. [Google Scholar] [CrossRef] [PubMed]
- Jansen-Winkeln, B.; Holfert, N.; Köhler, H.; Moulla, Y.; Takoh, J.P.; Rabe, S.M.; Mehdorn, M.; Barberio, M.; Chalopin, C.; Neumuth, T.; et al. Determination of the transection margin during colorectal resection with hyperspectral imaging (HSI). Int. J. Color. Dis. 2019, 34, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Köhler, H.; Jansen-Winkeln, B.; Maktabi, M.; Barberio, M.; Takoh, J.; Holfert, N.; Moulla, Y.; Niebisch, S.; Diana, M.; Neumuth, T.; et al. Evaluation of hyperspectral imaging (HSI) for the measurement of ischemic conditioning effects of the gastric conduit during esophagectomy. Surg. Endosc. 2019, 33, 3775–3782. [Google Scholar] [CrossRef] [PubMed]
- Thiem, D.G.E.; Römer, P.; Blatt, S.; Al-Nawas, B.; Kämmerer, P.W. New Approach to the Old Challenge of Free Flap Monitoring-Hyperspectral Imaging Outperforms Clinical Assessment by Earlier Detection of Perfusion Failure. J. Pers. Med. 2021, 11, 1101. [Google Scholar] [CrossRef] [PubMed]
- Kohler, L.H.; Köhler, H.; Kohler, S.; Langer, S.; Nuwayhid, R.; Gockel, I.; Spindler, N.; Osterhoff, G. Hyperspectral Imaging (HSI) as a new diagnostic tool in free flap monitoring for soft tissue reconstruction: A proof of concept study. BMC Surg. 2021, 21, 222. [Google Scholar] [CrossRef]
- Schulz, T.; Leuschner, S.; Siemers, F.; Marotz, J.; Houschyar, K.; Corterier, C.C. Assessing flap perfusion after free tissue transfer using hyperspectral imaging (HSI). Eur. J. Plast. Surg. 2021, 44, 497–506. [Google Scholar] [CrossRef]
- Schulz, T.; Marotz, J.; Stukenberg, A.; Reumuth, G.; Houschyar, K.S.; Siemers, F. Hyperspektralimaging zum postoperativen Lappenmonitoring von lokoregionären Lappenplastiken. Handchir. Mikrochir. Plast. Chir. 2020, 52, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Thiem, D.G.E.; Frick, R.W.; Goetze, E.; Gielisch, M.; Al-Nawas, B.; Kämmerer, P.W. Hyperspectral analysis for perioperative perfusion monitoring-a clinical feasibility study on free and pedicled flaps. Clin. Oral. Investig. 2021, 25, 933–945. [Google Scholar] [CrossRef]
- Degett, T.H.; Andersen, H.S.; Gögenur, I. Indocyanine green fluorescence angiography for intraoperative assessment of gastrointestinal anastomotic perfusion: A systematic review of clinical trials. Langenbecks Arch. Surg. 2016, 401, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Osterkamp, J.; Strandby, R.; Nerup, N.; Svendsen, M.; Svendsen, L.; Achiam, M. Quantitative fluorescence angiography detects dynamic changes in gastric perfusion. Surg. Endosc. 2021, 35, 6786–6795. [Google Scholar] [CrossRef]
- Maktabi, M.; Köhler, H.; Ivanova, M.; Neumuth, T.; Rayes, N.; Seidemann, L.; Sucher, R.; Jansen-Winkeln, B.; Gockel, I.; Barberio, M.; et al. Classification of hyperspectral endocrine tissue images using support vector machines. Int. J. Med. Robot. 2020, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Maktabi, M.; Köhler, H.; Ivanova, M.; Jansen-Winkeln, B.; Takoh, J.; Niebisch, S.; Rabe, S.M.; Neumuth, T.; Gockel, I.; Chalopin, C. Tissue classification of oncologic esophageal resectates based on hyperspectral data. Int. J. Comput. Assist. Radiol. Surg. 2019, 14, 1651–1661. [Google Scholar] [CrossRef] [PubMed]
- Jansen-Winkeln, B.; Barberio, M.; Chalopin, C.; Schierle, K.; Diana, M.; Köhler, H.; Gockel, I.; Maktabi, M. Feedforward Artificial Neural Network-Based Colorectal Cancer Detection Using Hyperspectral Imaging: A Step towards Automatic Optical Biopsy. Cancers 2021, 13, 967. [Google Scholar] [CrossRef] [PubMed]
- Hennig, S.; Jansen-Winkeln, B.; Köhler, H.; Knospe, L.; Chalopin, C.; Maktabi, M.; Pfahl, A.; Hoffmann, J.; Kwast, S.; Gockel, I.; et al. Novel Intraoperative Imaging of Gastric Tube Perfusion during Oncologic Esophagectomy-A Pilot Study Comparing Hyperspectral Imaging (HSI) and Fluorescence Imaging (FI) with Indocyanine Green (ICG). Cancers 2021, 14, 97. [Google Scholar] [CrossRef] [PubMed]

| Variables | Group A/N = 17 | Group B/N = 13 | p-Value |
|---|---|---|---|
| Age in years | 34 ± 14 | 40 ± 16 | 0.34 |
| BMI | 26 ± 4 | 24 ± 5 | 0.16 |
| ASA classification | |||
| Grade I | 13/76% | 10/76% | 0.97 |
| Grade II | 4/23% | 3/23% | 0.97 |
| Grade III | 0 | 0 | - |
| Grade IV | 0 | 0 | - |
| Diagnosis | |||
| Hypertension | 1/5% | 2/9% | 0.39 |
| Dyslipoproteinaemia | 0 | 1/7% | 0.24 |
| Diabetes mellitus type II | 1/5% | 1/7% | 0.84 |
| Lung diseases | 1/5% | 0 | 0.37 |
| Alcohol abuse | 0 | 0 | - |
| Smoking | 5/29% | 5/38% | 0.6 |
| Liver diseases | 0 | 0 | - |
| Medications | |||
| Duration of hormone therapy in months | 32 ± 18 | 39 ± 15 | 0.25 |
| Cut-Stitch Time in minutes | 226 ± 22 | 211 ± 17 | 0.18 |
| Actual Necrosis | |||
|---|---|---|---|
| Predicted necrosis | 11 (true positive) | 5 (false positive) | 16 |
| 1 (false negative) | 13 (true negative) | 14 | |
| 12 | 18 | 30 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schulz, T.; Köhler, H.; Kohler, L.H.; Langer, S.; Nuwayhid, R. Hyperspectral Imaging Detects Clitoral Vascular Issues in Gender-Affirming Surgery. Diagnostics 2024, 14, 1252. https://doi.org/10.3390/diagnostics14121252
Schulz T, Köhler H, Kohler LH, Langer S, Nuwayhid R. Hyperspectral Imaging Detects Clitoral Vascular Issues in Gender-Affirming Surgery. Diagnostics. 2024; 14(12):1252. https://doi.org/10.3390/diagnostics14121252
Chicago/Turabian StyleSchulz, Torsten, Hannes Köhler, Lukas Herbert Kohler, Stefan Langer, and Rima Nuwayhid. 2024. "Hyperspectral Imaging Detects Clitoral Vascular Issues in Gender-Affirming Surgery" Diagnostics 14, no. 12: 1252. https://doi.org/10.3390/diagnostics14121252






