A Pilot Study of the Computerized Brief Smell Identification Test
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Phenyl Ethyl Alcohol Odor Detection Threshold Test
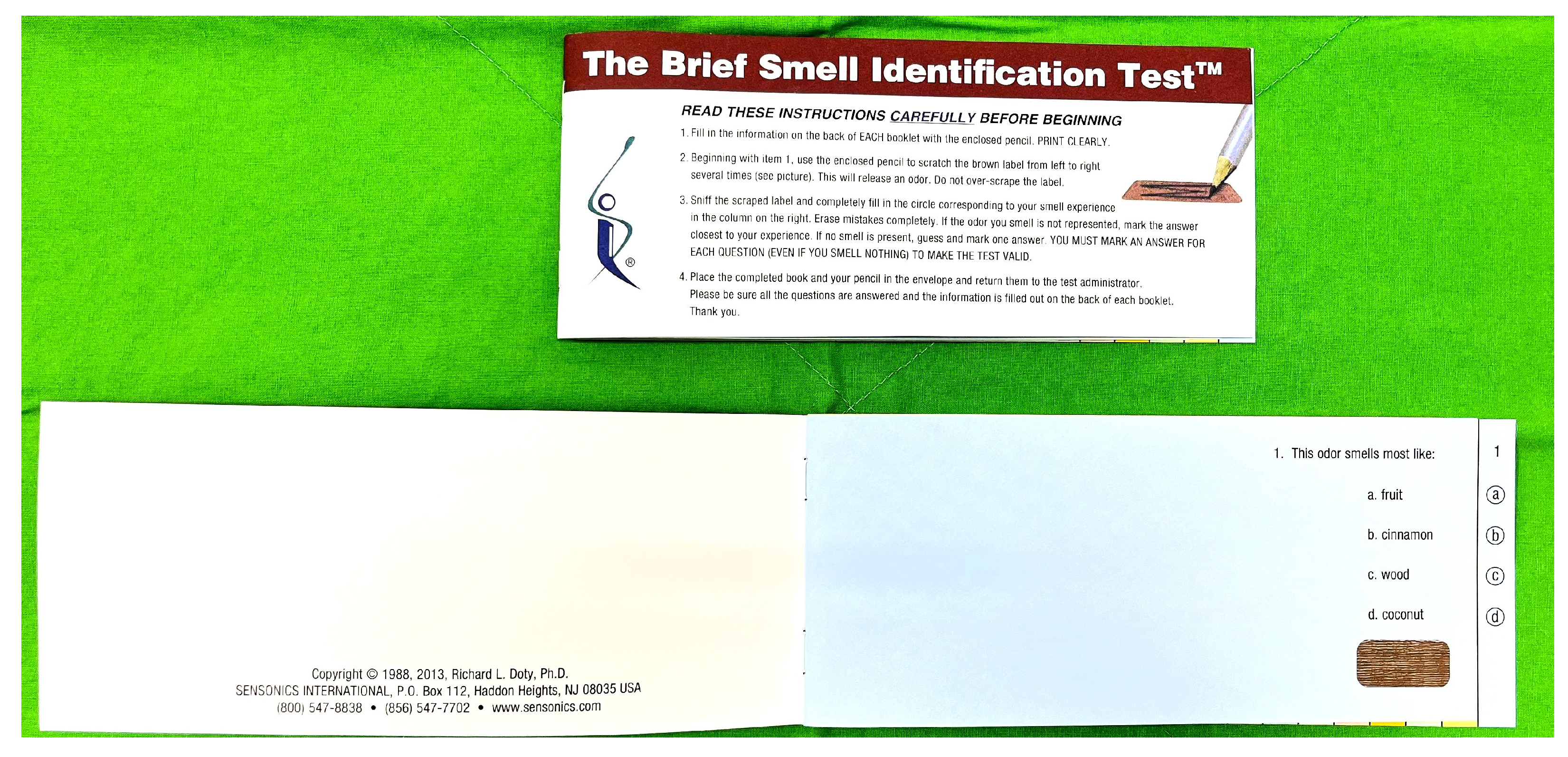
2.3. Brief Smell Identification Test
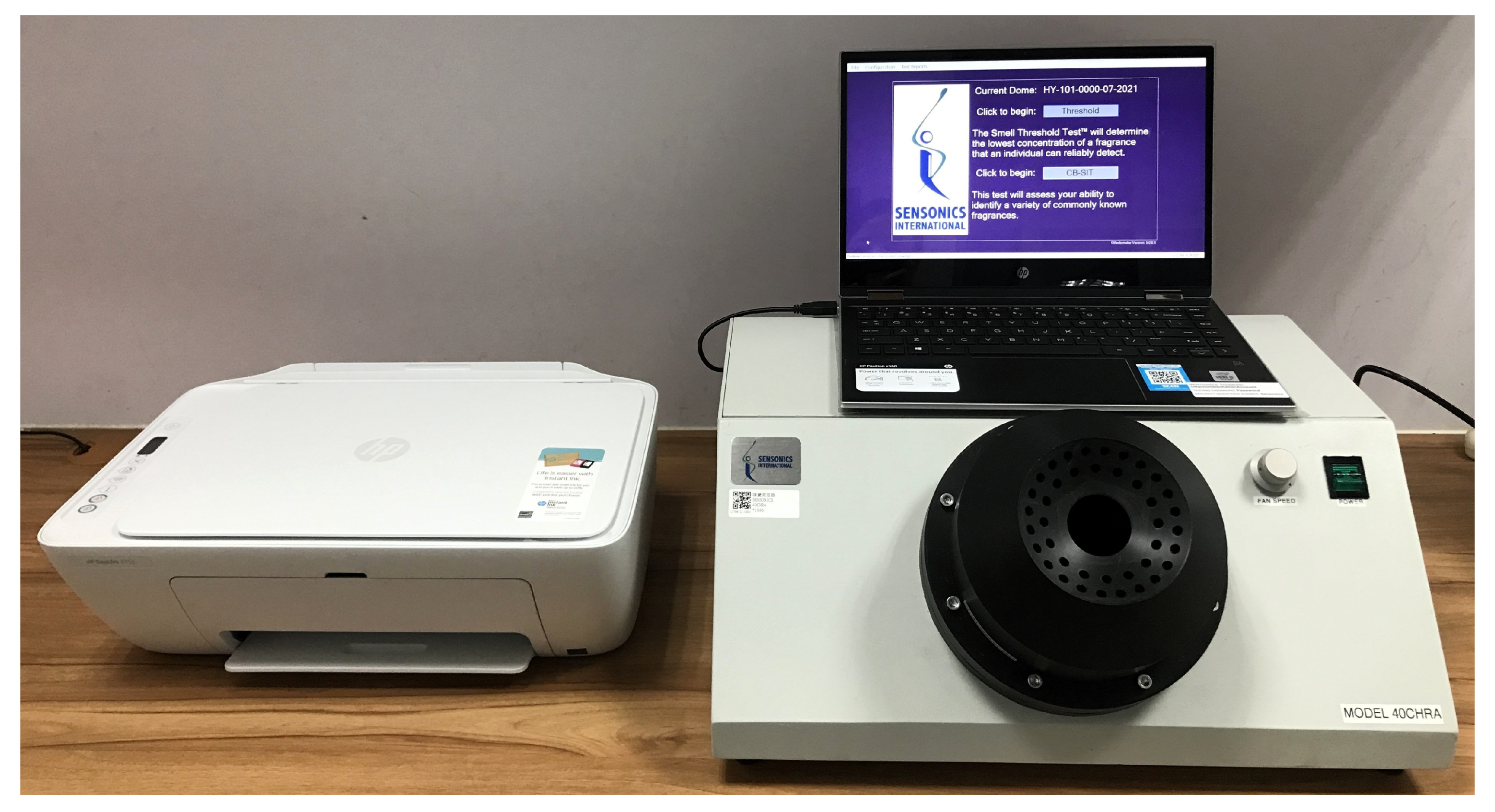
2.4. Computerized Brief Smell Identification Test
2.5. Statistical Analysis
3. Results
3.1. Patients
3.2. Test–Retest Reliability
3.3. Healthy Group
3.4. Hyposmic Patients
3.5. Anosmic Patients
3.6. Comparison among Healthy Volunteers, Hyposmic Patients, and Anosmic Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feng, G.; Zhuang, Y.; Yao, F.; Ye, Y.; Wan, Q.; Zhou, W. Development of the Chinese Smell Identification Test. Chem. Senses 2019, 44, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Hummel, T.; Sekinger, B.; Wolf, S.R.; Pauli, E.; Kobal, G. ‘Sniffin’ sticks’: Olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem. Senses 1997, 22, 39–52. [Google Scholar] [CrossRef] [PubMed]
- Boesveldt, S.; Verbaan, D.; Knol, D.L.; Visser, M.; van Rooden, S.M.; van Hilten, J.J.; Berendse, H.W. A comparative study of odor identification and odor discrimination deficits in Parkinson’s disease. Mov. Disord. 2008, 23, 1984–1990. [Google Scholar] [CrossRef] [PubMed]
- Jiang, R.S.; Kuo, L.T.; Wu, S.H.; Su, M.C.; Liang, K.L. Validation of the applicability of the traditional Chinese version of the University of Pennsylvania Smell Identification Test in patients with chronic rhinosinusitis. Allergy Rhinol. (Provid.) 2014, 5, 28–35. [Google Scholar] [CrossRef]
- Double, K.L.; Rowe, D.B.; Hayes, M.; Chan, D.K.; Blackie, J.; Corbett, A.; Joffe, R.; Fung, V.S.; Morris, J.; Halliday, G.M. Identifying the pattern of olfactory deficits in Parkinson disease using the brief smell identification test. Arch. Neurol. 2003, 60, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Toledano, A.; González, E.; Rodríguez, G.; Galindo, N. The validity of CCCRC test in patients with nasal polyposis. Rhinology 2007, 45, 54–58. [Google Scholar]
- Doty, R.L.; Marcus, A.; Lee, W.W. Development of the 12-item Cross-Cultural Smell Identification Test (CC-SIT). Laryngoscope 1996, 106, 353–356. [Google Scholar] [CrossRef]
- Seo, M.Y.; Choi, W.S.; Lee, S.H. Clinical features of olfactory dysfunction in COVID-19 patients. J. Korean Med. Sci. 2021, 36, e161. [Google Scholar] [CrossRef]
- Wang, S.M.; Kang, D.W.; Um, Y.H.; Kim, S.; Lee, C.U.; Lim, H.K. Olfactory dysfunction is associated with cerebral amyloid deposition and cognitive function in the trajectory of Alzheimer’s disease. Biomolecules 2023, 13, 1336. [Google Scholar] [CrossRef]
- Menon, C.; Westervelt, H.J.; Jahn, D.R.; Dressel, J.A.; O’Bryant, S.E. Normative performance on the Brief Smell Identification Test (BSIT) in a multi-ethnic bilingual cohort: A Project FRONTIER study. Clin. Neuropsychol. 2013, 27, 946–961. [Google Scholar] [CrossRef]
- Rebholz, H.; Pfaffeneder-Mantai, F.; Knoll, W.; Hassel, A.W.; Frank, W.; Kleber, C. Olfactory dysfunction in SARS-CoV-2 infection: Focus on odorant specificity and chronic persistence. Am. J. Otolaryngol. 2021, 42, 103014. [Google Scholar] [CrossRef]
- Dengiz, R.; Haytoğlu, S.; Görgülü, O.; Doğru, M.; Arıkan, O.K. Effect of septorhinoplasty on olfactory function: Assessment using the Brief Smell Identification Test. Turk. Arch. Otorhinolaryngol. 2015, 53, 4–9. [Google Scholar] [CrossRef]
- Kjelvik, G.; Sando, S.B.; Aasly, J.; Engedal, K.A.; White, L.R. Use of the Brief Smell Identification Test for olfactory deficit in a Norwegian population with Alzheimer’s disease. Int. J. Geriatr. Psychiatry 2007, 22, 1020–1024. [Google Scholar] [CrossRef]
- Schriever, V.A.; Körner, J.; Beyer, R.; Viana, S.; Seo, H.S. A computer-controlled olfactometer for a self-administered odor identification test. Eur. Arch. Otorhinolaryngol. 2011, 268, 1293–1297. [Google Scholar] [CrossRef]
- Mueller, C.A.; Grassinger, E.; Naka, A.; Temmel, A.F.; Hummel, T.; Kobal, G. A self-administered odor identification test procedure using the “Sniffin’ Sticks”. Chem. Senses 2006, 31, 595–598. [Google Scholar] [CrossRef]
- Jiang, R.S.; Liang, K.L. A pilot study of the Self-Administered Computerized Olfactory Testing System. Am. J. Rhinol. Allergy 2015, 29, e55–e58. [Google Scholar] [CrossRef]
- Doty, R.L.; Kamath, V. The influences of age on olfaction: A review. Front. Psychol. 2014, 5, 20. [Google Scholar] [CrossRef]
- Assanasen, P.; Tunsuriyawong, P.; Pholpornphisit, W.; Chatameteekul, M.; Bunnag, C. Smell detection threshold in Thai adults. J. Med. Assoc. Thai. 2009, 92, 813–816. [Google Scholar]
- Kandemir, S.; Pamuk, A.E.; Habipoğlu, Y.; Özel, G.; Bayar Muluk, N.; Kılıç, R. Olfactory acuity based on Brief Smell Identification Test (BSIT®) in migraine patients with and without aura: A cross-sectional, controlled study. Auris Nasus Larynx 2022, 49, 613–617. [Google Scholar] [CrossRef]
- El Rassi, E.; Mace, J.C.; Steele, T.O.; Alt, J.A.; Soler, Z.M.; Fu, R.; Smith, T.L. Sensitivity analysis and diagnostic accuracy of the Brief Smell Identification Test in patients with chronic rhinosinusitis. Int. Forum. Allergy Rhinol. 2016, 6, 287–292. [Google Scholar] [CrossRef]
- Haytoğlu, S.; Dengiz, R.; Muluk, N.B.; Kuran, G.; Arikan, O.K. Effects of septoplasty on olfactory function evaluated by the Brief Smell Identification Test: A study of 116 patients. Ear Nose Throat J. 2017, 96, 433–438. [Google Scholar] [CrossRef]
- Aniteli, M.B.; Marson, F.A.L.; Cunha, F.R.; Sakano, E. Correlation and agreement of olfactory perception assessed by the Connecticut Chemosensory Clinical Research Center olfactory test and the Brief-Smell Identification Test. Braz. J. Otorhinolaryngol. 2022, 88, 858–866. [Google Scholar] [CrossRef]
- Goudsmit, N.; Coleman, E.; Seckinger, R.A.; Wolitzky, R.; Stanford, A.D.; Corcoran, C.; Goetz, R.R. A brief smell identification test discriminates between deficit and non-deficit schizophrenia. Psychiatry Res. 2003, 120, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Young, V.M.; Bernal, R.; Pollet, E.; Serrano-Rubio, L.; Gaona, C.; Himali, J.J.; Seshadri, S.; González, D.A.; Gonzales, M.M. Deep sleep, olfactory loss, and cognition in early-stage Parkinson’s disease: Pilot study results. Gerontol. Geriatr. Med. 2024, 10, 23337214241262925. [Google Scholar] [CrossRef]
- Liu, H.; Du, W.; Li, S.; Jin, Y.; Chen, H.; Su, W. China’s modified version of Sniffin’ Sticks 12-Identification Test used in Chinese Parkinson’s disease and multiple system patients: Comparison of three olfactory testing methods. Parkinsons. Dis. 2024, 2024, 3561881. [Google Scholar] [CrossRef]
- Taş, B.M.; Alpaydın, T.; Akçalı, S.; Kaygusuz, S.; Özlük Erol, Ö.; Şencan, Z.; Cömert, E.; Bayar Muluk, N.; Özel, G. Evaluation of clinical features and olfactory functions in COVID-19: A multicentre study. Cureus 2023, 15, e40027. [Google Scholar] [CrossRef]
| Item | B-SIT Score | First Test | Second Test | p-Value | cB-SIT Score | First Test | Second Test | p-Value |
|---|---|---|---|---|---|---|---|---|
| Score | 9.3 ± 1.4 | 10.4 ± 1.0 | 0.003 | 9.1 ± 1.3 | 9.1 ± 1.5 | 0.717 | ||
| 1. Cinnamon | 63.3% | 60.0% | 1.000 | 93.3% | 76.7% | 0.125 | ||
| 2. Turpentine | 90.0% | 86.7% | 1.000 | Rubber tire | 90.0% | 86.7% | 1.000 | |
| 3. Lemon | 46.7% | 80.0% | 0.013 | 50.0% | 53.3% | 1.000 | ||
| 4. Smoke | 66.7% | 86.7% | 0.070 | 90.0% | 90.0% | 1.000 | ||
| 5. Chocolate | 93.3% | 100% | 0.500 | 23.3% | 20.0% | 1.000 | ||
| 6. Rose | 56.7% | 80.0% | 0.065 | 90.0% | 90.0% | 1.000 | ||
| 7. Paint thinner | 96.7% | 100% | 1.000 | Licorice | 86.7% | 86.7% | 1.000 | |
| 8. Banana | 43.3% | 63.3% | 0.109 | 23.3% | 33.3% | 0.375 | ||
| 9. Pineapple | 96.7% | 96.7% | 1.000 | 96.7% | 100% | 1.000 | ||
| 10. Gasoline | 83.3% | 86.7% | 1.000 | Apple | 70.0% | 76.7% | 0.754 | |
| 11. Soap | 90.0% | 96.7% | 0.500 | 96.7% | 100% | 1.000 | ||
| 12. Onion | 100% | 100% | 96.7% | 100% | 1.000 |
| Item | Score Type | Healthy Volunteers | Hyposmic Patients | Anosmic Patients | p |
|---|---|---|---|---|---|
| Score | B-SIT | 9.3 ± 1.5 | 6.5 ± 2.5 | 4.3 ± 2.3 | <0.001 a |
| cB-SIT | 8.6 ± 1.7 | 5.6 ± 1.9 | 4.5 ± 1.4 | <0.001 a | |
| p | 0.008 b | 0.04 b | 0.435 | ||
| Cinnamon | B-SIT | 71.7% | 23.3% | 10.0% | <0.001 a |
| cB-SIT | 80.5% | 33.3% | 23.3% | <0.001 a | |
| p | 0.077 | 0.508 | 0.289 | ||
| Turpentine | B-SIT | 93.3% | 56.7% | 43.3% | <0.001 a |
| Rubber tire | cB-SIT | 83.3% | 63.3% | 66.7% | 0.069 |
| p | 0.180 | 0.774 | 0.167 | ||
| Lemon | B-SIT | 51.7% | 40.0% | 33.3% | 0.222 |
| cB-SIT | 45.0% | 26.7% | 23.3% | 0.069 | |
| p | 0.523 | 0.344 | 0.549 | ||
| Smoke | B-SIT | 55.0% | 33.3% | 16.7% | 0.002 a |
| cB-SIT | 85.0% | 36.7% | 33.3% | <0.001 a | |
| p | <0.001 a | 1.000 | 0.227 | ||
| Chocolate | B-SIT | 90.0% | 80.0% | 43.3% | <0.001 a |
| cB-SIT | 20.0% | 40.0% | 36.7% | 0.084 | |
| p | <0.001 a | 0.004 a | 0.804 | ||
| Rose | B-SIT | 58.3% | 33.3% | 23.3% | 0.003 a |
| cB-SIT | 85.0% | 30.0% | 16.7% | <0.001 a | |
| p | <0.001 a | 1.000 | 0.727 | ||
| Paint thinner | B-SIT | 95.0% | 76.7% | 33.3% | <0.001 a |
| Licorice | cB-SIT | 91.7% | 50.0% | 43.3% | <0.001 a |
| p | 0.727 | 0.039 b | 0.607 | ||
| Banana | B-SIT | 50.0% | 53.3% | 33.3% | 0.229 |
| cB-SIT | 20.0% | 30.0% | 13.3% | 0.276 | |
| p | 0.001 a | 0.118 | 0.070 | ||
| Pineapple | B-SIT | 91.7% | 53.3% | 40.0% | <0.001 a |
| cB-SIT | 90.0% | 43.3% | 40.0% | <0.001 a | |
| p | 1.000 | 0.581 | 1.000 | ||
| Gasoline | B-SIT | 80.0% | 53.3% | 43.3% | 0.001 a |
| Apple | cB-SIT | 58.3% | 46.7% | 56.7% | 0.564 |
| p | 0.015 b | 0.815 | 0.388 | ||
| Soap | B-SIT | 95.0% | 63.3% | 53.3% | <0.001 a |
| cB-SIT | 93.3% | 73.3% | 50.0% | <0.001 a | |
| p | 1.000 | 0.581 | 1.000 | ||
| Onion | B-SIT | 98.3% | 80.0% | 53.3% | <0.001 a |
| cB-SIT | 98.3% | 86.7% | 46.7% | <0.001 a | |
| p | 1.000 | 0.625 | 0.727 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, R.-S.; Chiang, Y.-F. A Pilot Study of the Computerized Brief Smell Identification Test. Diagnostics 2024, 14, 2121. https://doi.org/10.3390/diagnostics14192121
Jiang R-S, Chiang Y-F. A Pilot Study of the Computerized Brief Smell Identification Test. Diagnostics. 2024; 14(19):2121. https://doi.org/10.3390/diagnostics14192121
Chicago/Turabian StyleJiang, Rong-San, and Yi-Fang Chiang. 2024. "A Pilot Study of the Computerized Brief Smell Identification Test" Diagnostics 14, no. 19: 2121. https://doi.org/10.3390/diagnostics14192121
APA StyleJiang, R.-S., & Chiang, Y.-F. (2024). A Pilot Study of the Computerized Brief Smell Identification Test. Diagnostics, 14(19), 2121. https://doi.org/10.3390/diagnostics14192121






