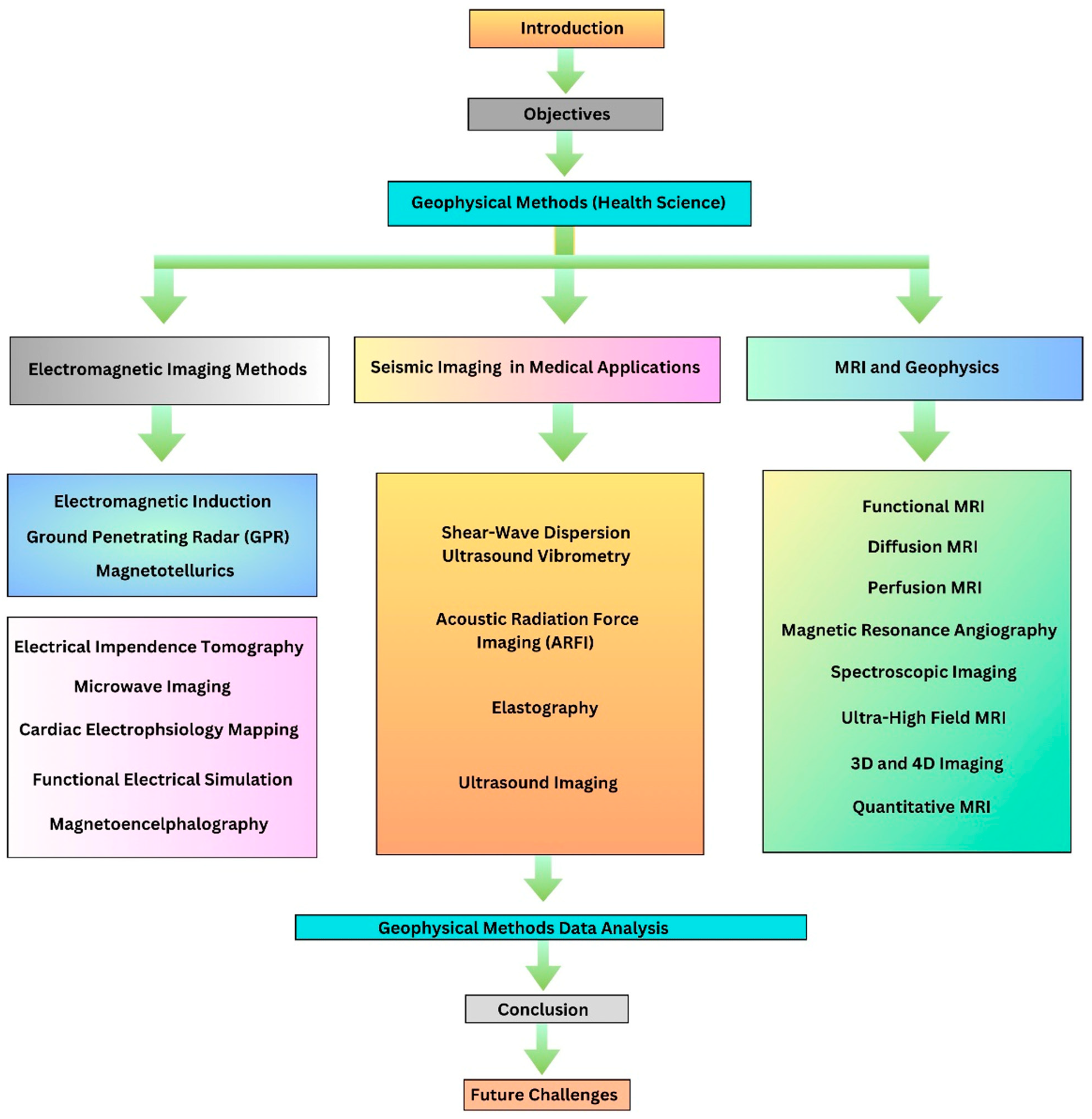
Exploring the Intersection of Geophysics and Diagnostic Imaging in the Health Sciences
Abstract
:1. Introduction
- The principles and operating processes behind various geophysical techniques used in healthcare.
- Geophysical techniques that can be adapted and used in imaging techniques.
- The incorporation of artificial intelligence (AI) and machine learning (ML) for technological advancement in geophysics-driven medical imaging.
2. Geophysical Methods in Health Sciences
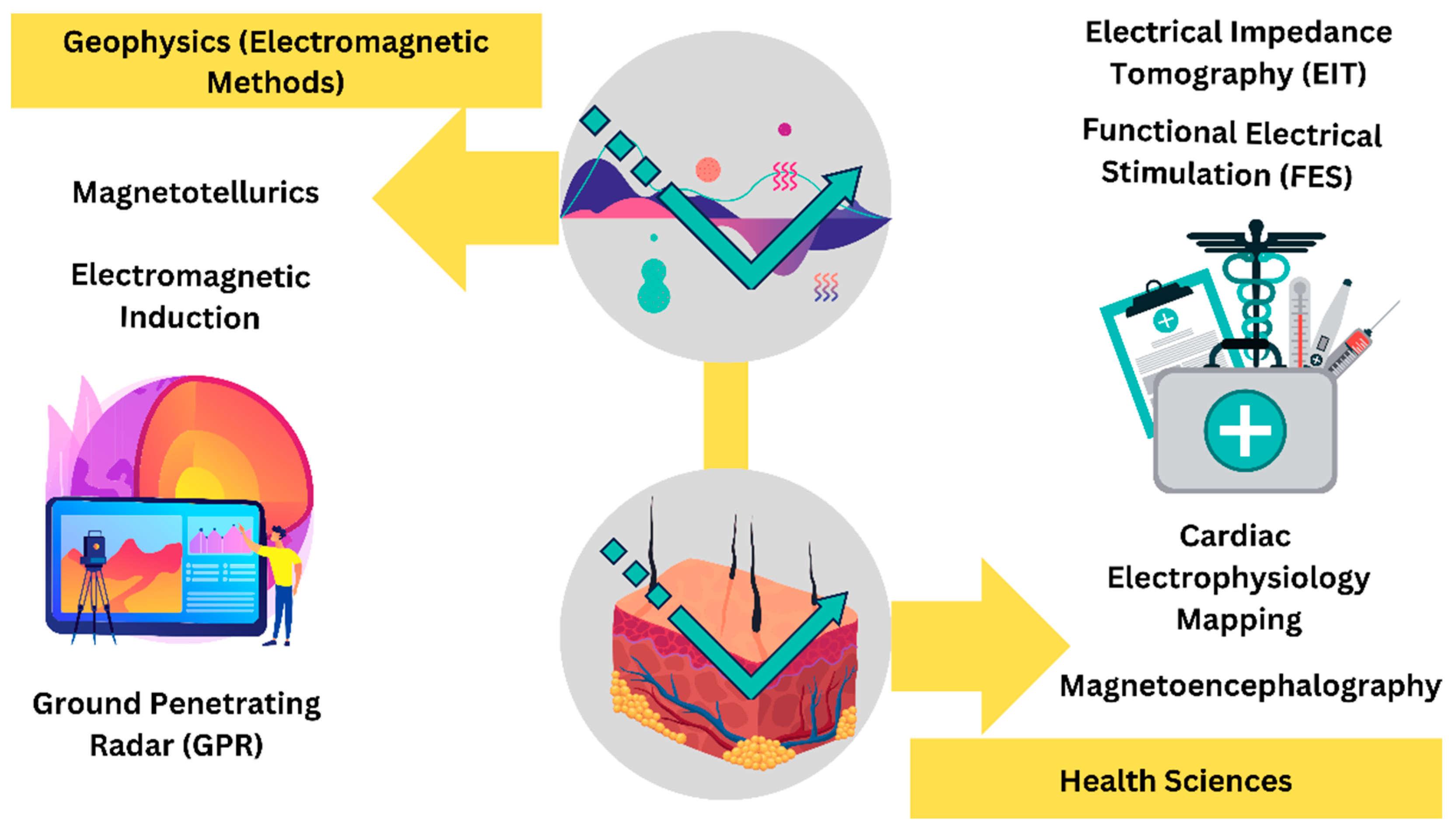
2.1. Electromagnetic Imaging Method
2.2. Seismic Imaging in Medical Applications
- v(x,z) = 2D velocity field
- = reciprocal velocity
- dl = differential distance along the ray
2.3. MRI and Geophysics
3. Geophysical Data Analysis in the Health Sciences
- Signal Processing: ECG, EEGs, EEGs, and even functional MRI data are treated as medical signals using signal processing techniques utilized in geophysics, including filtering, noise reduction, and Fourier analysis. These methods aid in pattern recognition, abnormality quantification, and information extraction from noisy data [115,116].
- Image Reconstruction: Medical imaging modalities like CT and MRI are developed from geophysical data inversion methods, which are used to rebuild subsurface structures. These techniques produce more realistic reconstructions of anatomical features by improving image quality, lowering artifacts, and boosting spatial resolution [117].
- Data Fusion: Medical data fusion uses methods for integrating various geophysical information to provide a full perspective of subsurface features. Combining data from various imaging modalities (such as MRI and PET) in medical imaging allows for a more thorough understanding of the interior organs and their activities [118,119].
- ML and AI: Medical imaging uses tomographic techniques to recreate precise images of organs and tissues. Tomographic techniques are frequently utilized in geophysics to build 3D images of subsurface objects. Examples include X-ray CT and PET scans, where cross-sectional images are produced using information from various angles [120,121,122,123].
- Tomographic Imaging: Medical imaging uses tomographic techniques to recreate precise images of organs and tissues. Tomographic techniques are frequently utilized in geophysics to build 3D images of subsurface objects. Examples include X-ray CT and PET scans, where cross-sectional images are produced using information from various angles [124].
- Inverse Problem Solving: Techniques for inverse problem-solving are used to recover data from imperfect or indirect measurements in both geophysics and medicine. This aids in the discovery of subsurface features in geophysics and the reconstruction of images from sparse data in medicine, such as in magnetic resonance spectroscopy (MRS) for the investigation of metabolic processes [122].
Artificial Intelligence (AI) and Machine Learning (ML) Applications
| Algorithm | Description |
|---|---|
| Linear Regression | Application involves predicting patient outcomes based on clinical parameters, such as age, blood pressure, and cholesterol levels. In clinical trials, linear regression aids in analyzing the relationship between treatment dosage and response. The method is also employed for assessing risk factors associated with specific health conditions and modeling disease progression over time. Public health studies benefit from linear regression to understand how environmental factors impact population health. |
| Logistic Regression | Logistic regression can be utilized to assess the probability of a patient developing a particular disease based on various risk factors such as age, genetic predisposition, and lifestyle choices. This method is instrumental in risk assessment and enables healthcare professionals to identify significant predictors for targeted interventions. Logistic regression is also employed in clinical research, analyzing factors influencing treatment success or failure. |
| Decision Tree and Random Forest | Decision trees, being intuitive and easy to interpret, are often applied to predict outcomes such as disease presence or treatment response. For instance, a decision tree might be constructed to assess the likelihood of a patient developing a specific condition based on various medical parameters. Random forests, which are ensembles of decision trees, offer enhanced predictive performance and robustness. In health sciences, random forests find applications in scenarios where complex relationships among multiple variables influence health outcomes. For example, in genomics, random forests can be used to identify genetic markers associated with certain diseases by analyzing large datasets. |
| Support Vector Machines (SVMs) | SVMs find applications in identifying patterns within genetic data, aiding in the classification of patients into distinct subgroups based on their genetic profiles. Additionally, SVMs contribute to personalized medicine by assisting in the prediction of treatment responses. SVMs can be utilized to discern between different medical conditions based on patient data, facilitating accurate disease diagnosis. Their ability to handle high-dimensional data and nonlinear relationships makes SVMs suitable for complex medical datasets. |
| K-Nearest Neighbor (KNN) | KNN is particularly useful in personalized medicine, where it aids in recommending treatments based on the experiences of similar patients. It considers the proximity of an individual’s health profile to others, offering tailored insights for healthcare interventions. Additionally, KNN finds applications in epidemiology, helping identify clusters of diseases or health conditions within a population. |
| Naive Bayes | Naive Bayes is employed for tasks such as disease diagnosis and risk assessment. For instance, it can be applied to evaluate the probability of a patient having a specific medical condition given certain observable symptoms, aiding in efficient and accurate diagnosis. Naive Bayes is commonly used in analyzing electronic health records, patient demographics, and diagnostic test results. |
| K-Means Clustering | This algorithm is commonly used to identify natural groupings or clusters within datasets, enabling the segmentation of patients based on similar characteristics. In healthcare, K-means clustering is applied to stratify patient populations, allowing for personalized treatment approaches and targeted interventions. One notable application involves patient segmentation for risk assessment. K-means clustering can group patients with similar health profiles, aiding healthcare professionals in identifying high-risk populations that may require specific monitoring or preventive measures. |
| Principal Component Analysis (PCA) | AI-driven methods help automate image interpretation, improve image quality, and shorten scan times. AI tools help radiologists spot problems and boost their level of diagnostic assurance. |
| Convolutional Neural Networks (CNNs) | CNNs are adept at extracting intricate patterns and features from visual data, making them invaluable for image classification and recognition. In healthcare, CNNs are extensively applied to analyze medical images such as X-rays, MRIs, and CT scans, aiding in the detection and classification of abnormalities. One significant application involves the automated diagnosis of diseases based on medical images. CNNs excel at discerning subtle patterns indicative of various conditions, contributing to faster and more accurate diagnoses. For instance, in radiology, CNNs can assist in identifying tumors, fractures, or anomalies in scans, enhancing the efficiency. CNNs are employed in pathology image analysis, where they can assist in the classification of tissue samples by identifying cellular structures and anomalies. |
| Recurrent Neural Networks (RNNs) | RNNs can learn temporal dependencies and patterns in a patient’s medical history, facilitating the prediction of disease progression or the likelihood of future health events. RNNs contribute to personalized medicine by tailoring predictions based on individual patient data. They are adept at capturing the dynamic nature of health-related data, allowing for more accurate predictions and timely interventions. |
4. Conclusions
5. Future Challenges and Scopes
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wheeler, J.; Cheadle, M. Geophysics. In Reference Module in Earth Systems and Environmental Sciences; Elsevier: Amsterdam, The Netherlands, 2014; ISBN 978-0-12-409548-9. [Google Scholar]
- Crampin, S.; Gao, Y. The New Geophysics. Terra Nova 2013, 25, 173–180. [Google Scholar] [CrossRef]
- Crampin, S.; Gao, Y. Evidence Supporting New Geophysics. Earth Planet. Phys. 2018, 2, 173–188. [Google Scholar] [CrossRef]
- Witherly, K. Exploration Geophysics: Past Performance and Future Opportunities. Preview 2020, 2020, 11–14. [Google Scholar] [CrossRef]
- Etgen, J.; Gray, S.; Zhang, Y. An Overview of Depth Imaging in Exploration Geophysics. Geophysics 2009, 74, WCA5-17. [Google Scholar] [CrossRef]
- Van Dam, R.L. Landform Characterization Using Geophysics—Recent Advances, Applications, and Emerging Tools. Geomorphology 2012, 137, 57–73. [Google Scholar] [CrossRef]
- Merz, B.; Kuhlicke, C.; Kunz, M.; Pittore, M.; Babeyko, A.; Bresch, D.N.; Domeisen, D.I.V.; Feser, F.; Koszalka, I.; Kreibich, H.; et al. Impact Forecasting to Support Emergency Management of Natural Hazards. Rev. Geophys. 2020, 58, e2020RG000704. [Google Scholar] [CrossRef]
- Singh, R.K.; Patidar, A. A Systematic Approach for Planning a Geochemical Survey for Hydrocarbon Exploration: An Overview. Iran. J. Earth Sci. 2023. [Google Scholar] [CrossRef]
- Ore, T.; Martin, E.; Rubio-Cisneros, I.; Girard, A.; Ma, J.; Kanakiya, S.; Sanuade, O.; Titov, A.; Souza, R. Research Committee Update: Hot Topics in Geophysics: Progress, Trends, and Perspectives. Lead Edge 2023, 42, 360–363. [Google Scholar] [CrossRef]
- Chambers, S. Application of Geophysical Methods in Environmental Monitoring. OAJRC Appl. Phys. 2022, 3, 1–4. [Google Scholar]
- Pantea-Roșan, L.R.; Bungau, S.G.; Radu, A.-F.; Pantea, V.A.; Moisi, M.I.; Vesa, C.M.; Behl, T.; Nechifor, A.C.; Babes, E.E.; Stoicescu, M.; et al. A Narrative Review of the Classical and Modern Diagnostic Methods of the No-Reflow Phenomenon. Diagnostics 2022, 12, 932. [Google Scholar] [CrossRef]
- Lines, L.R.; Symbiosis between Geophysics and Medicine. CREWES Research Report. Available online: https://www.crewes.org/Documents/ResearchReports/2018/CRR201840.pdf (accessed on 1 January 2024).
- Rajiah, P.S.; François, C.J.; Leiner, T. Cardiac MRI: State of the Art. Radiology 2023, 307, e223008. [Google Scholar] [CrossRef] [PubMed]
- Babes, E.E.; Tit, D.M.; Bungau, A.F.; Bustea, C.; Rus, M.; Bungau, S.G.; Babes, V.V. Myocardial Viability Testing in the Management of Ischemic Heart Failure. Life 2022, 12, 1760. [Google Scholar] [CrossRef] [PubMed]
- Fabio, F.; Acocella, V.; Carlton, A.M.; D’Odorico, P.; Duan, Q.; Gettelman, A.; Halekas, J.; Harris, R.; Mollenhauer, G.; Robock, A.; et al. 60 Years and Beyond of Reviews of Geophysics. Rev. Geophys. 2023, 61, e2023RG000807. [Google Scholar]
- Reilly, J.; Aharchaou, M.; Neelamani, R. A Brief Overview of Seismic Resolution in Applied Geophysics. Lead Edge 2023, 42, 8–15. [Google Scholar] [CrossRef]
- Babu, S.B.; Satyakumar, A.V.; Kulkarni, A.V.; Vats, P.K. Structurally Controlled Mineralization in Parts of Aravalli Craton, India: Constraints from Gravity and Magnetic Data. J. Geodyn. 2023, 155, 101954. [Google Scholar] [CrossRef]
- Vozoff, K. Electromagnetic Methods in Applied Geophysics. Geophys. Surv. 1980, 4, 9–29. [Google Scholar] [CrossRef]
- Bock, Y.; Melgar, D. Physical Applications of GPS Geodesy: A Review. Rep. Prog. Phys. 2016, 79, 106801. [Google Scholar] [CrossRef]
- Subbarao, P.; Venkata Vijaya Kumar, P.; Chandrasekharam, D.; Deshmukh, V.; Singh, A. Magnetotelluric Investigations over Geothermal Provinces of India: An Overview. Turk. J. Earth Sci. 2023, 32, 149–162. [Google Scholar] [CrossRef]
- Besedina, A.; Tubanov, T. Microseisms as a Tool for Geophysical Research. A Review. J. Volcanol. Seismol. 2023, 17, 83–101. [Google Scholar] [CrossRef]
- Seton, M.; Williams, S.E.; Domeier, M.; Collins, A.S.; Sigloch, K. Deconstructing Plate Tectonic Reconstructions. Nat. Rev. Earth Environ. 2023, 4, 185–204. [Google Scholar] [CrossRef]
- Zhu, J.-J.; Yang, M.; Ren, Z.J. Machine Learning in Environmental Research: Common Pitfalls and Best Practices. Environ. Sci. Technol. 2023, 57, 17671–17689. [Google Scholar] [CrossRef] [PubMed]
- Lev, E.; Boyce, C.M. Opportunities for Characterizing Geological Flows Using Magnetic Resonance Imaging. iScience 2020, 23, 101534. [Google Scholar] [CrossRef] [PubMed]
- Arnold, T.C.; Freeman, C.W.; Litt, B.; Stein, J.M. Low-Field MRI: Clinical Promise and Challenges. J. Magn. Reson. Imaging 2023, 57, 25–44. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, N.; Fan, L.-F.; Zhao, P.-F.; Li, J.-H.; Huang, L.; Wang, Z.-Y. Robust Electrical Impedance Tomography for Biological Application: A Mini Review. Heliyon 2023, 9, e15195. [Google Scholar] [CrossRef] [PubMed]
- Pennati, F.; Angelucci, A.; Morelli, L.; Bardini, S.; Barzanti, E.; Cavallini, F.; Conelli, A.; Di Federico, G.; Paganelli, C.; Aliverti, A. Electrical Impedance Tomography: From the Traditional Design to the Novel Frontier of Wearables. Sensors 2023, 23, 1182. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Mubeen, I.; Ullah, N.; Shah, S.S.U.D.; Khan, B.A.; Zahoor, M.; Ullah, R.; Khan, F.A.; Sultan, M.A. Modern Diagnostic Imaging Technique Applications and Risk Factors in the Medical Field: A Review. Biomed. Res. Int. 2022, 2022, 5164970. [Google Scholar] [CrossRef]
- Peng, C. President’s Page: Applying Geophysical Methods to Medical Ultrasound Imaging. Lead Edge 2023, 42, 586–587. [Google Scholar] [CrossRef]
- Wang, X.; Bishop, C.; O’Callaghan, J.; Gayhoor, A.; Albani, J.; Theriault, W.; Chappell, M.; Golay, X.; Wang, D.; Becerra, L. MRI Assessment of Cerebral Perfusion in Clinical Trials. Drug Discov. Today 2023, 28, 103506. [Google Scholar] [CrossRef]
- Jimenez, J.V.; Weirauch, A.J.; Culter, C.A.; Choi, P.J.; Hyzy, R.C. Electrical Impedance Tomography in Acute Respiratory Distress Syndrome Management. Crit. Care Med. 2022, 50, 1210–1223. [Google Scholar] [CrossRef]
- Nordli, D.; Galan, F. Pediatric Magnetoencephalography. Ann. Child Neurol. Soc. 2023, 1, 123–128. [Google Scholar] [CrossRef]
- Jiang, Z.; Salcudean, S.E.; Navab, N. Robotic Ultrasound Imaging: State-of-the-Art and Future Perspectives. Med. Image Anal. 2023, 89, 102878. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Savic, L.J.; Hillebrandt, K.H.; Sack, I. MR Elastography in Cancer. Investig. Radiol. 2023, 58, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Kulathilake, S.; Abdullah, N.; Sabri, A.; Lai, K.W. A Review on Deep Learning Approaches for Low-Dose Computed Tomography Restoration. Complex Intell. Syst. 2021, 9, 2713–2745. [Google Scholar] [CrossRef] [PubMed]
- Haq, I.; Mazhar, T.; Nasir, Q.; Razzaq, S.; Mohsan, S.A.; Alsharif, M.H.; Alkahtani, H.K.; Aljarbouh, A.; Mostafa, S.M. Machine Vision Approach for Diagnosing Tuberculosis (TB) Based on Computerized Tomography (CT) Scan Images. Symmetry 2022, 14, 1997. [Google Scholar] [CrossRef]
- Cecil, K.; Huppert, L.; Mukhtar, R.; Dibble, E.H.; O’Brien, S.R.; Ulaner, G.A.; Lawhn-Heath, C. Metabolic Positron Emission Tomography in Breast Cancer. PET Clin. 2023, 18, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Babes, E.E.; Bustea, C.; Ilias, T.I.; Babes, V.V.; Luca, S.-A.; Luca, C.T.; Radu, A.-F.; Tarce, A.G.; Bungau, A.F.; Bustea, C. Multimodality Imaging Diagnosis in Infective Endocarditis. Life 2024, 14, 54. [Google Scholar] [CrossRef]
- Constable, R.T. Challenges in FMRI and Its Limitations BT—Functional Neuroradiology: Principles and Clinical Applications. In Functional Neuroradiology; Faro, S.H., Mohamed, F.B., Eds.; Springer International Publishing: New York, NY, USA, 2023; pp. 497–510. ISBN 978-3-031-10909-6. [Google Scholar]
- Behler, A.; Müller, H.-P.; Ludolph, A.C.; Kassubek, J. Diffusion Tensor Imaging in Amyotrophic Lateral Sclerosis: Machine Learning for Biomarker Development. Int. J. Mol. Sci. 2023, 24, 1911. [Google Scholar] [CrossRef]
- Giraudeau, P. Quantitative NMR Spectroscopy of Complex Mixtures. Chem. Commun. 2023, 59, 6627–6642. [Google Scholar] [CrossRef]
- Baradaran, Y.; Fernandez Rojas, R.; Goecke, R.; Ghahramani, M. A Systematic Review on Functional Near-Infrared Spectroscopy Concurrent with Quantitative Balance Assessment. IEEE Access 2023, 11, 66641–66671. [Google Scholar] [CrossRef]
- Lin, L.; Wang, L.V. The Emerging Role of Photoacoustic Imaging in Clinical Oncology. Nat. Rev. Clin. Oncol. 2022, 19, 365–384. [Google Scholar] [CrossRef]
- Kim, T.H.; Schnitzer, M.J. Fluorescence Imaging of Large-Scale Neural Ensemble Dynamics. Cell 2022, 185, 9–41. [Google Scholar] [CrossRef] [PubMed]
- Castro-Camus, E.; Koch, M.; Mittleman, D.M. Recent Advances in Terahertz Imaging: 1999 to 2021. Appl. Phys. B 2021, 128, 12. [Google Scholar] [CrossRef]
- Mishra, R.N.; Singh, M.K.; Kumar, V. Biomechanical Analysis of Human Femur Using Finite Element Method: A Review Study. Mater. Today Proc. 2022, 56, 384–389. [Google Scholar] [CrossRef]
- Wang, X.; Wang, P.; Zhang, X.; Wan, Y.; Shi, H.; Liu, W. Target Electromagnetic Detection Method in Underground Environment: A Review. IEEE Sens. J. 2022, 22, 1. [Google Scholar] [CrossRef]
- Pathirana, S.; Lambot, S.; Krishnapillai, M.; Cheema, M.; Smeaton, C.; Galagedara, L. Ground-Penetrating Radar and Electromagnetic Induction: Challenges and Opportunities in Agriculture. Remote Sens. 2023, 15, 2932. [Google Scholar]
- Rashed, M.; Atef, A. Mapping Underground Utilities within Conductive Soil Using Multi-Frequency Electromagnetic Induction and Ground Penetrating Radar. Arab. J. Geosci. 2015, 8, 2341–2346. [Google Scholar] [CrossRef]
- Joung, I.S.; Cho, S.O.; Kim, B.; Jeong, J.; Jeong, S.; Jang, H.; Reninger, P.-A.; Nam, M.J. A Review of the Time-Domain Electromagnetic Method: Research Trends and Applications. J. Korean Soc. Miner. Energy Resour. Eng. 2022, 59, 364–378. [Google Scholar] [CrossRef]
- Buddo, I.; Shelokhov, I.; Misyurkeeva, N.; Sharlov, M.; Agafonov, Y. Electromagnetic Surveys for Petroleum Exploration: Challenges and Prospects. Energies 2022, 15, 9646. [Google Scholar] [CrossRef]
- Chen, H.; Han, P.; Hattori, K. Recent Advances and Challenges in the Seismo-Electromagnetic Study: A Brief Review. Remote Sens. 2022, 14, 5893. [Google Scholar] [CrossRef]
- Catapano, I.; Di Napoli, R.; Soldovieri, F.; Bavusi, M.; Loperte, A.; Dumoulin, J. Structural Monitoring via Microwave Tomography-Enhanced GPR: The Montagnole Test Site. J. Geophys. Eng. 2012, 9, S100–S107. [Google Scholar] [CrossRef]
- Porsani, J.L.; Almeida, E.R.; Poluha, B.; dos Santos, V.R.N.; Porsani, J.L.; Almeida, E.R.; Poluha, B.; dos Santos, V.R.N. GPR Tomographic Imaging of Concrete Tubes and Steel/Plastic Tanks Buried in IAG/USP Geophysical Test Site, Brazil. Int. J. Geosci. 2017, 8, 647–658. [Google Scholar] [CrossRef]
- Lin, W.; Yang, B.; Han, B.; Hu, X. A Review of Subsurface Electrical Conductivity Anomalies in Magnetotelluric Imaging. Sensors 2023, 23, 1803. [Google Scholar] [CrossRef] [PubMed]
- Ke, X.-Y.; Hou, W.; Huang, Q.; Hou, X.; Bao, X.-Y.; Kong, W.-X.; Li, C.-X.; Qiu, Y.-Q.; Hu, S.-Y.; Dong, L.-H. Advances in Electrical Impedance Tomography-Based Brain Imaging. Mil. Med. Res. 2022, 9, 10. [Google Scholar] [CrossRef] [PubMed]
- Brookes, M.J.; Leggett, J.; Rea, M.; Hill, R.M.; Holmes, N.; Boto, E.; Bowtell, R. Magnetoencephalography with Optically Pumped Magnetometers (OPM-MEG): The next Generation of Functional Neuroimaging. Trends Neurosci. 2022, 45, 621–634. [Google Scholar] [CrossRef] [PubMed]
- Fred, A.L.; Kumar, S.N.; Kumar Haridhas, A.; Ghosh, S.; Purushothaman Bhuvana, H.; Sim, W.K.J.; Vimalan, V.; Givo, F.A.S.; Jousmäki, V.; Padmanabhan, P.; et al. A Brief Introduction to Magnetoencephalography (MEG) and Its Clinical Applications. Brain Sci. 2022, 12, 788. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhao, L.; Gao, Y.; Liu, C.; Dong, X.; He, X. The Difference between the Effectiveness of Body-Weight-Supported Treadmill Training Combined with Functional Electrical Stimulation and Sole Body-Weight-Supported Treadmill Training for Improving Gait Parameters in Stroke Patients: A Systematic Review and Meta-Analysis. Front. Neurol. 2022, 13, 1003723. [Google Scholar] [PubMed]
- Sousa, A.S.P.; Moreira, J.; Silva, C.; Mesquita, I.; Macedo, R.; Silva, A.; Santos, R. Usability of Functional Electrical Stimulation in Upper Limb Rehabilitation in Post-Stroke Patients: A Narrative Review. Sensors 2022, 22, 1409. [Google Scholar] [CrossRef]
- Ripplinger, C.M.; Glukhov, A.V.; Kay, M.W.; Boukens, B.J.; Chiamvimonvat, N.; Delisle, B.P.; Fabritz, L.; Hund, T.J.; Knollmann, B.C.; Li, N.; et al. Guidelines for Assessment of Cardiac Electrophysiology and Arrhythmias in Small Animals. Am. J. Physiol. Heart Circ. Physiol. 2022, 323, H1137–H1166. [Google Scholar] [CrossRef]
- Ge, X.; Chen, M.; Sha, Z.; Zhang, J. Three-Dimensional Mapping in Cardiac Implantable Electronic Device—A Feasible and Effective Alternative to Fluoroscopy. J. Interv. Card. Electrophysiol. 2023, 66, 783–792. [Google Scholar] [CrossRef]
- Porter, E.; Raterink, A.; Farshkaran, A. Microwave-Based Detection of the Bladder State as a Support Tool for Urinary Incontinence [Bioelectromagnetics]. IEEE Antennas Propag. Mag. 2022, 64, 112–122. [Google Scholar] [CrossRef]
- Gopalakrishnan, K.; Adhikari, A.; Pallipamu, N.; Singh, M.; Nusrat, T.; Gaddam, S.; Samaddar, P.; Rajagopal, A.; Cherukuri, A.S.; Yadav, A.; et al. Applications of Microwaves in Medicine Leveraging Artificial Intelligence: Future Perspectives. Electronics 2023, 12, 1101. [Google Scholar] [CrossRef]
- Mathur, M.; Mathur, D.; Singh, G.; Bhatnagar, S.K.; Nigam, H.; Arora, M. Microwave Imaging Breast Cancer Detection Techniques: A Brief Review. In Proceedings of the Optical and Wireless Technologies; Tiwari, M., Maddila, R.K., Garg, A.K., Kumar, A., Yupapin, P., Eds.; Springer: Singapore, 2022; pp. 203–210. [Google Scholar]
- Singh, R.K.; Sharma, A. Seismic Data Acquisition in Hydrocarbon Exploration. J. Emerg. Technol. Innov. Res. 2021, 8, f559–f569. [Google Scholar]
- Li, Z.-C.; Qu, Y.-M. Research Progress on Seismic Imaging Technology. Pet. Sci. 2022, 19, 128–146. [Google Scholar]
- Kossobokov, V.G.; Nekrasova, A.K.; Schepalina, P.D. Seismic Dynamics in Advance of and After the Largest Earthquakes, 1985–2020. Surv. Geophys. 2022, 43, 423–436. [Google Scholar] [CrossRef]
- Liu, W.; Liu, Y.; Li, S.; Chen, Y. A Review of Variational Mode Decomposition in Seismic Data Analysis. Surv. Geophys. 2023, 44, 323–355. [Google Scholar] [CrossRef]
- Kijko, A.; Vermeulen, P.J.; Smit, A. Estimation Techniques for Seismic Recurrence Parameters for Incomplete Catalogues. Surv. Geophys. 2021, 43, 597–617. [Google Scholar] [CrossRef]
- Ulfers, A.; Zeeden, C.; Wagner, B.; Krastel, S.; Buness, H.; Wonik, T. Borehole Logging and Seismic Data from Lake Ohrid (North Macedonia/Albania) as a Basis for Age-Depth Modelling over the Last One Million Years. Quat. Sci. Rev. 2022, 276, 107295. [Google Scholar] [CrossRef]
- Theis, D.; Bonomi, E. Seismic Imaging of Medical Ultrasound Data: Towards in Vivo Applications. Europhys. Lett. 2023, 142, 52001. [Google Scholar] [CrossRef]
- Zhao, L.; Lediju Bell, M.A. A Review of Deep Learning Applications in Lung Ultrasound Imaging of COVID-19 Patients. BME Front. 2022, 2022, 9780173. [Google Scholar] [CrossRef]
- Naruse, M.; Trappe, S.; Trappe, T.A. Human Skeletal Muscle Size with Ultrasound Imaging: A Comprehensive Review. J. Appl. Physiol. 2022, 132, 1267–1279. [Google Scholar] [CrossRef]
- Ngo, H.-H.-P.; Poulard, T.; Brum, J.; Gennisson, J.-L. Anisotropy in Ultrasound Shear Wave Elastography: An Add-on to Muscles Characterization. Front. Physiol. 2022, 13, 1000612. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Bhatt, M.; Qu, Z.; Zhang, S.; Hartel, M.; Khademhosseini, A.; Cloutier, G. Deep Learning in Ultrasound Elastography Imaging: A Review. Med. Phys. 2022, 49, 5993–6018. [Google Scholar] [CrossRef]
- Muhammad Hussain, N.; Rehman, A.U.; Othman, M.T.; Zafar, J.; Zafar, H.; Hamam, H. Accessing Artificial Intelligence for Fetus Health Status Using Hybrid Deep Learning Algorithm (AlexNet-SVM) on Cardiotocographic Data. Sensors 2022, 22, 5103. [Google Scholar] [CrossRef] [PubMed]
- Rifu, K.; Watanabe, J.; Sasanuma, H.; Taniguchi, N. Evaluation of the Elasticity of the Pancreas Using Acoustic Radiation Force Impulse Elastography in Patients with Acute Pancreatitis: A Systematic Review and Meta-Analysis. Ultrasound Med. Biol. 2022, 48, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-L.; Lin, S.; Lyu, G.-R. Advances in the Clinical Application of Ultrasound Elastography in Uterine Imaging. Insights Imaging 2022, 13, 141. [Google Scholar] [CrossRef] [PubMed]
- Blank, J.; Blomquist, M.; Arant, L.; Cone, S.; Roth, J. Characterizing Musculoskeletal Tissue Mechanics Based on Shear Wave Propagation: A Systematic Review of Current Methods and Reported Measurements. Ann. Biomed. Eng. 2022, 50, 751–768. [Google Scholar] [CrossRef] [PubMed]
- Terreno, E.; Castelli, D.D.; Viale, A.; Aime, S. Challenges for Molecular Magnetic Resonance Imaging. Chem. Rev. 2010, 110, 3019–3042. [Google Scholar] [CrossRef]
- Glover, G.H. Overview of Functional Magnetic Resonance Imaging. Neurosurg. Clin. N. Am. 2011, 22, 133–139. [Google Scholar] [CrossRef]
- Williams, S.N.; McElhinney, P.; Gunamony, S. Ultra-High Field MRI: Parallel-Transmit Arrays and RF Pulse Design. Phys. Med. Biol. 2023, 68, 02TR02. [Google Scholar]
- Shaffer, A.; Kwok, S.S.; Naik, A.; Anderson, A.T.; Lam, F.; Wszalek, T.; Arnold, P.M.; Hassaneen, W. Ultra-High-Field MRI in the Diagnosis and Management of Gliomas: A Systematic Review. Front. Neurol. 2022, 13, 857825. [Google Scholar] [CrossRef]
- Hyodo, R.; Takehara, Y.; Naganawa, S. 4D Flow MRI in the Portal Venous System: Imaging and Analysis Methods, and Clinical Applications. Radiol. Med. 2022, 127, 1181–1198. [Google Scholar] [CrossRef] [PubMed]
- Carreira Figueiredo, I.; Borgan, F.; Pasternak, O.; Turkheimer, F.E.; Howes, O.D. White-Matter Free-Water Diffusion MRI in Schizophrenia: A Systematic Review and Meta-Analysis. Neuropsychopharmacology 2022, 47, 1413–1420. [Google Scholar] [CrossRef] [PubMed]
- Lowrie, W. What Is Geophysics? In Geophysics: A Very Short Introduction; Lowrie, W., Ed.; Oxford University Press: Oxford, UK, 2018; ISBN 9780198792956. [Google Scholar]
- Gallo-Bernal, S.; Bedoya, M.A.; Gee, M.S.; Jaimes, C. Pediatric Magnetic Resonance Imaging: Faster Is Better. Pediatr. Radiol. 2023, 53, 1270–1284. [Google Scholar] [CrossRef] [PubMed]
- Bianchini, E.; Lønnebakken, M.T.; Wohlfahrt, P.; Piskin, S.; Terentes-Printzios, D.; Alastruey, J.; Guala, A. Magnetic Resonance Imaging and Computed Tomography for the Noninvasive Assessment of Arterial Aging: A Review by the VascAgeNet COST Action. J. Am. Heart Assoc. 2023, 12, e027414. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Hu, Y.; Zhang, W.; Wang, J.; Ji, W.; Manza, P.; Volkow, N.D.; Zhang, Y.; Wang, G.-J. Brain Functional and Structural Magnetic Resonance Imaging of Obesity and Weight Loss Interventions. Mol. Psychiatry 2023, 28, 1466–1479. [Google Scholar] [CrossRef] [PubMed]
- Ab Mumin, N.; Ramli Hamid, M.T.; Wong, J.H.D.; Rahmat, K.; Ng, K.H. Magnetic Resonance Imaging Phenotypes of Breast Cancer Molecular Subtypes: A Systematic Review. Acad. Radiol. 2022, 29, S89–S106. [Google Scholar] [CrossRef]
- Mazzacane, F.; Mazzoleni, V.; Scola, E.; Mancini, S.; Lombardo, I.; Busto, G.; Rognone, E.; Pichiecchio, A.; Padovani, A.; Morotti, A.; et al. Vessel Wall Magnetic Resonance Imaging in Cerebrovascular Diseases. Diagnostics 2022, 12, 258. [Google Scholar] [CrossRef]
- Chen, Z.; Pawar, K.; Ekanayake, M.; Pain, C.; Zhong, S.; Egan, G.F. Deep Learning for Image Enhancement and Correction in Magnetic Resonance Imaging-State-of-the-Art and Challenges. J. Digit. Imaging 2023, 36, 204–230. [Google Scholar] [CrossRef]
- Aghayev, A.; Steigner, M. Magnetic Resonance Angiography of the Arteries of the Upper and Lower Extremities. Magn. Reson. Imaging Clin. N. Am. 2023, 31, 361–372. [Google Scholar] [CrossRef]
- Lozano Gonzalez, R.; Singh, R.B.; Virador, G.M.; Barrett, K.M.; Farres, H.; Miller, D.A.; Meschia, J.F.; Sandhu, S.J.S.; Erben, Y. Systematic Review on Magnetic Resonance Angiography with Vessel Wall Imaging for the Characterization of Symptomatic Carotid Artery Plaque. Ann. Vasc. Surg. 2023, 95, 224–232. [Google Scholar] [CrossRef]
- Stamatelatou, A.; Scheenen, T.W.J.; Heerschap, A. Developments in Proton MR Spectroscopic Imaging of Prostate Cancer. Magn. Reson. Mater. Phys. Biol. Med. 2022, 35, 645–665. [Google Scholar] [CrossRef]
- Sharma, U.; Jagannathan, N.R. Magnetic Resonance Imaging (MRI) and MR Spectroscopic Methods in Understanding Breast Cancer Biology and Metabolism. Metabolites 2022, 12, 295. [Google Scholar] [CrossRef] [PubMed]
- Kazama, T.; Takahara, T.; Hashimoto, J. Breast Cancer Subtypes and Quantitative Magnetic Resonance Imaging: A Systemic Review. Life 2022, 12, 490. [Google Scholar] [CrossRef] [PubMed]
- Yao, Z.; Wang, H.; Yan, W.; Wang, Z.; Zhang, W.; Wang, Z.; Zhang, G. Artificial Intelligence-Based Diagnosis of Alzheimer’s Disease with Brain MRI Images. Eur. J. Radiol. 2023, 165, 110934. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.; Fu, Y.; Li, M.; Mu, S.; Chu, X.; Fu, J.; Lin, C.; Zhang, H. MRI-Based Artificial Intelligence in Rectal Cancer. J. Magn. Reson. Imaging 2023, 57, 45–56. [Google Scholar] [CrossRef]
- Chen, Y.; Schonlieb, C.B.; Lio, P.; Leiner, T.; Dragotti, P.L.; Wang, G.; Rueckert, D.; Firmin, D.; Yang, G. AI-Based Reconstruction for Fast MRI-A Systematic Review and Meta-Analysis. Proc. IEEE 2022, 110, 224–245. [Google Scholar] [CrossRef]
- Alao, J.O.; Lawal, K.M.; Dewu, B.B.M.; Raimi, J. The Evolving Roles of Geophysical Test Sites in Engineering, Science and Technology. Acta Geophys. 2023, 1, 1–16. [Google Scholar] [CrossRef]
- Mazhar, T.; Nasir, Q.; Haq, I.; Kamal, M.M.; Ullah, I.; Kim, T.; Mohamed, H.G.; Alwadai, N. A Novel Expert System for the Diagnosis and Treatment of Heart Disease. Electronics 2022, 11, 3989. [Google Scholar] [CrossRef]
- Sonawani, S.; Patil, K.; Natarajan, P. Biomedical Signal Processing for Health Monitoring Applications: A Review. Int. J. Appl. Syst. Stud. 2021, 10, 44–69. [Google Scholar] [CrossRef]
- Azami, H.; Faes, L.; Escudero, J.; Humeau-Heurtier, A.; Silva, L.E.V. Entropy Analysis of Univariate Biomedical Signals: Review and Comparison of Methods. In Frontiers in Entropy Across the Disciplines; World Scientific: Singapore, 2020; pp. 233–286. [Google Scholar]
- Singh, A.K.; Krishnan, S. ECG Signal Feature Extraction Trends in Methods and Applications. Biomed. Eng. Online 2023, 22, 22. [Google Scholar] [CrossRef]
- Yan, Z.; Zhu, L.-G.; Meng, K.; Huang, W.; Shi, Q. THz Medical Imaging: From in Vitro to in Vivo. Trends Biotechnol. 2022, 40, 816–830. [Google Scholar] [CrossRef] [PubMed]
- Medeiros Mirra, R.; Vafidis, J.O.; Smith, J.A.; Thomas, R.J. Teaching Data Analysis to Life Scientists Using “R” Statistical Software: Challenges, Opportunities, and Effective Methods. In Teaching Biostatistics in Medicine and Allied Health Sciences; Farnell, D.J.J., Medeiros Mirra, R., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 167–187. ISBN 978-3-031-26010-0. [Google Scholar]
- Friedrich, S.; Groll, A.; Ickstadt, K.; Kneib, T.; Pauly, M.; Rahnenführer, J.; Friede, T. Regularization Approaches in Clinical Biostatistics: A Review of Methods and Their Applications. Stat. Methods Med. Res. 2023, 32, 425–440. [Google Scholar] [CrossRef] [PubMed]
- Tornero-Costa, R.; Martinez-Millana, A.; Azzopardi-Muscat, N.; Lazeri, L.; Traver, V.; Novillo-Ortiz, D. Methodological and Quality Flaws in the Use of Artificial Intelligence in Mental Health Research: Systematic Review. JMIR Ment. Health 2023, 10, e42045. [Google Scholar] [CrossRef] [PubMed]
- Ardeti, V.A.; Kolluru, V.R.; Varghese, G.T.; Patjoshi, R.K. An Overview on State-of-the-Art Electrocardiogram Signal Processing Methods: Traditional to AI-Based Approaches. Expert Syst. Appl. 2023, 217, 119561. [Google Scholar] [CrossRef]
- Kirubha, S.P.A.; Jayanthi, T.; Santhan, S.T.; Jishna, A. Glance into Effective Electrocardiographic Signal Processing for Automated Arrhythmia Detection and Cardioversion. AIP Conf. Proc. 2023, 2603, 020024. [Google Scholar]
- Musa, N.; Gital, A.Y.; Aljojo, N.; Chiroma, H.; Adewole, K.S.; Mojeed, H.A.; Faruk, N.; Abdulkarim, A.; Emmanuel, I.; Folawiyo, Y.Y.; et al. A Systematic Review and Meta-Data Analysis on the Applications of Deep Learning in Electrocardiogram. J. Ambient Intell. Humaniz. Comput. 2023, 14, 9677–9750. [Google Scholar] [CrossRef]
- Yaqub, M.; Jinchao, F.; Arshid, K.; Ahmed, S.; Zhang, W.; Nawaz, M.Z.; Mahmood, T. Deep Learning-Based Image Reconstruction for Different Medical Imaging Modalities. Comput. Math. Methods Med. 2022, 2022, 8750648. [Google Scholar] [CrossRef]
- Suriyan, K.; Ramalingam, N.; Kumari, J.M.; Chandra Babu, J. Recent Developments of Medical Image Processing Techniques and Challenges. In AI, IoT, and Blockchain Breakthroughs in E-Governance; IGI Global: Hershey, PA, USA, 2023; pp. 188–198. ISBN 9781668476970. [Google Scholar]
- Matthews, J.; Kim, J. Advances in Biosignal Sensing and Signal Processing Methods with Wearable Devices. Anal. Sens. 2022, 3, e202200062. [Google Scholar] [CrossRef]
- Reader, A.J.; Pan, B. AI for PET Image Reconstruction. Br. J. Radiol. 2023, 96, 20230292. [Google Scholar] [CrossRef]
- Casian, T.; Nagy, B.; Kovács, B.; Galata, D.L.; Hirsch, E.; Farkas, A. Challenges and Opportunities of Implementing Data Fusion in Process Analytical Technology—A Review. Molecules 2022, 27, 4846. [Google Scholar] [CrossRef]
- Albahri, A.S.; Duhaim, A.M.; Fadhel, M.A.; Alnoor, A.; Baqer, N.S.; Alzubaidi, L.; Albahri, O.S.; Alamoodi, A.H.; Bai, J.; Salhi, A.; et al. A Systematic Review of Trustworthy and Explainable Artificial Intelligence in Healthcare: Assessment of Quality, Bias Risk, and Data Fusion. Inf. Fusion 2023, 96, 156–191. [Google Scholar] [CrossRef]
- Micucci, M.; Iula, A. Recent Advances in Machine Learning Applied to Ultrasound Imaging. Electronics 2022, 11, 1800. [Google Scholar] [CrossRef]
- Peper, E.S.; van Ooij, P.; Jung, B.; Huber, A.; Gräni, C.; Bastiaansen, J.A.M. Advances in Machine Learning Applications for Cardiovascular 4D Flow MRI. Front. Cardiovasc. Med. 2022, 9, 1052068. [Google Scholar] [CrossRef]
- Sridharan, B.; Goel, M.; Priyakumar, U.D. Modern Machine Learning for Tackling Inverse Problems in Chemistry: Molecular Design to Realization. Chem. Commun. 2022, 58, 5316–5331. [Google Scholar] [CrossRef] [PubMed]
- Haq, I.; Mazhar, T.; Malik, M.A.; Kamal, M.M.; Ullah, I.; Kim, T.; Hamdi, M.; Hamam, H. Lung Nodules Localization and Report Analysis from Computerized Tomography (CT) Scan Using a Novel Machine Learning Approach. Appl. Sci. 2022, 12, 12614. [Google Scholar] [CrossRef]
- Hampel, U.; Babout, L.; Banasiak, R.; Schleicher, E.; Soleimani, M.; Wondrak, T.; Vauhkonen, M.; Lähivaara, T.; Tan, C.; Hoyle, B.; et al. A Review on Fast Tomographic Imaging Techniques and Their Potential Application in Industrial Process Control. Sensors 2022, 22, 2309. [Google Scholar] [CrossRef]
- Jerban, S.; Barrère, V.; Andre, M.; Chang, E.Y.; Shah, S.B. Quantitative Ultrasound Techniques Used for Peripheral Nerve Assessment. Diagnostics 2023, 13, 956. [Google Scholar] [CrossRef]
- Nattabi, H.A.; Sharif, N.M.; Yahya, N.; Ahmad, R.; Mohamad, M.; Zaki, F.M.; Yusoff, A.N. Is Diagnostic Performance of Quantitative 2D-Shear Wave Elastography Optimal for Clinical Classification of Benign and Malignant Thyroid Nodules?: A Systematic Review and Meta-Analysis. Acad. Radiol. 2022, 29, S114–S121. [Google Scholar] [CrossRef]
- Abbasi, S.; Tavakoli, M.; Boveiri, H.R.; Mosleh Shirazi, M.A.; Khayami, R.; Khorasani, H.; Javidan, R.; Mehdizadeh, A. Medical Image Registration Using Unsupervised Deep Neural Network: A Scoping Literature Review. Biomed. Signal Process. Control 2022, 73, 103444. [Google Scholar] [CrossRef]
- Sajjad, M.; Safdar, T.; Khurram, S.; Gardezi, A.; Alassery, F.; Hamam, H.; Cheikhrouhou, O.; Shafiq, M. Efficient Joint Key Authentication Model in E-Healthcare. Comput. Mater. Contin. 2021, 71, 2739–2753. [Google Scholar] [CrossRef]
- Chandra Boro, R.; Kaushal, J.; Nangia, Y.; Wangoo, N.; Bhasin, A.; Suri, C.R. Gold Nanoparticles Catalyzed Chemiluminescence Immunoassay for Detection of Herbicide 2,4-Dichlorophenoxyacetic Acid. Analyst 2011, 136, 2125–2130. [Google Scholar] [CrossRef] [PubMed]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Wangoo, N.; Kaushal, J.; Bhasin, K.K.; Mehta, S.K.; Suri, C.R. Zeta Potential Based Colorimetric Immunoassay for the Direct Detection of Diabetic Marker HbA1c Using Gold Nanoprobes. Chem. Commun. 2010, 46, 5755–5757. [Google Scholar] [CrossRef] [PubMed]
- Mousavi Baigi, S.F.; Sarbaz, M.; Ghaddaripouri, K.; Ghaddaripouri, M.; Mousavi, A.S.; Kimiafar, K. Attitudes, Knowledge, and Skills towards Artificial Intelligence among Healthcare Students: A Systematic Review. Health Sci. Rep. 2023, 6, e1138. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Koundal, D.; Kadyan, V. Image Fusion Techniques: A Survey. Arch. Comput. Methods Eng. 2021, 28, 4425–4447. [Google Scholar] [CrossRef]
- Balagurunathan, Y.; Mitchell, R.; El Naqa, I. Requirements and Reliability of AI in the Medical Context. Phys. Medica 2021, 83, 72–78. [Google Scholar] [CrossRef]
- Hameed, B.M.Z.; Prerepa, G.; Patil, V.; Shekhar, P.; Zahid Raza, S.; Karimi, H.; Paul, R.; Naik, N.; Modi, S.; Vigneswaran, G.; et al. Engineering and Clinical Use of Artificial Intelligence (AI) with Machine Learning and Data Science Advancements: Radiology Leading the Way for Future. Ther. Adv. Urol. 2021, 13, 17562872211044880. [Google Scholar] [CrossRef]
- Venkatesh, D.A.N. Reimagining the Future of Healthcare Industry through Internet of Medical Things (IoMT), Artificial Intelligence (AI), Machine Learning (ML), Big Data, Mobile Apps and Advanced Sensors. SSRN Electron. J. 2019, 9, 3014–3019. [Google Scholar] [CrossRef]
- Khan, Z.F.; Alotaibi, S.R. Applications of Artificial Intelligence and Big Data Analytics in M-Health: A Healthcare System Perspective. J. Healthc. Eng. 2020, 2020, 8894694. [Google Scholar] [CrossRef]
- Saif, S.; Datta, D.; Saha, A.; Biswas, S.; Chowdhury, C. Data Science and AI in IoT Based Smart Healthcare: Issues, Challenges and Case Study BT—Enabling AI Applications in Data Science. In Enabling AI Applications in Data Science; Hassanien, A.-E., Taha, M.H.N., Khalifa, N.E.M., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 415–439. ISBN 978-3-030-52067-0. [Google Scholar]
- Punia, S.; Kumar, M.; Stephan, T.; Deverajan, G.; Patan, R. Performance Analysis of Machine Learning Algorithms for Big Data Classification: ML and AI-Based Algorithms for Big Data Analysis. Int. J. E-Health Med. Commun. 2021, 12, 60–75. [Google Scholar] [CrossRef]
- Parimbelli, E.; Wilk, S.; Cornet, R.; Sniatala, P.; Sniatala, K.; Glaser, S.L.C.; Fraterman, I.; Boekhout, A.H.; Ottaviano, M.; Peleg, M. A Review of AI and Data Science Support for Cancer Management. Artif. Intell. Med. 2021, 117, 102111. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Preininger, A. AI in Health: State of the Art, Challenges, and Future Directions. Yearb. Med. Inform. 2019, 28, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.E. Medical Geology. Encycl. Geol. 2021, 684–702. [Google Scholar] [CrossRef]
- Li, F.; Yu, T.; Huang, Z.; Yang, Z.; Hou, Q.; Tang, Q.; Liu, J.; Wang, L. Linking Health to Geology-a New Assessment and Zoning Model Based on the Frame of Medical Geology. Environ. Geochem. Health 2023, 45, 7145–7159. [Google Scholar] [CrossRef] [PubMed]
- Nichols, N.T.A.; Nelson, L. Health Effects of Exposure to Specific Geologic Materials: Summary of Clinical Findings, Treatment, and Prevention. In Practical Applications of Medical Geology; Siegel, M., Selinus, O., Finkelman, R., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 525–563. ISBN 978-3-030-53893-4. [Google Scholar]



| Application | Description | Refs. |
|---|---|---|
| Seismology | The study of seismic waves produced by earthquakes or other sources is known as seismology. These waves reveal details about the composition of Earth’s inner layers and the characteristics of the materials that constitute them. | [16] |
| Gravity and magnetic surveys | Geophysicists can locate subsurface features like faults, mineral deposits, and even underground water reservoirs by detecting fluctuations in Earth’s gravitational and magnetic fields. | [17] |
| Electromagnetic methods | To determine the electrical conductivity and other characteristics of the subsurface, electromagnetic techniques such as magneto-telluric examine fluctuations in Earth’s electromagnetic field. | [18] |
| Geodesy | The goal of geodesy is to precisely measure the gravitational field, shape, and rotation of Earth. For mapping, navigation, and a general understanding of Earth dynamics, this information is essential. | [19] |
| Geothermal studies | To investigate the distribution of heat on Earth and the possibility of geothermal energy production, geophysicists employ a variety of techniques. | [20] |
| Natural resources exploration | By identifying abnormalities in the subsurface, geophysics is essential in locating important resources like oil, gas, minerals, and groundwater. | [8] |
| Volcanology | Researchers can keep track of and better understand the mechanisms underlying volcanic eruptions, reducing the risks associated with them by examining seismic activity, ground deformation, and other geophysical indicators. | [21] |
| Tectonics and plate movements | Our understanding of tectonic plate movement, the forces that propel it, and the geological events that emerge from it, such as earthquakes and mountain development, is aided by geophysics. | [22] |
| Environmental studies | To research how human activity affects the planet, geophysical techniques are used, including monitoring changes in the surface and subsurface of the planet as a result of things like groundwater extraction, land subsidence, and more. | [23] |
| Technique | Description | Refs. |
|---|---|---|
| Magnetic Resonance Imaging (MRI) | MRI has completely changed medical imaging. Its foundations lay in the concepts of strong magnetic fields employed in geophysics. It produces fine-grained pictures of soft tissues using strong magnets, enabling non-invasive visualization of anatomical features and pathologies inside the human body. | [30] |
| Electrical Impedance Tomography (EIT) | EIT has been modified to track alterations in electrical conductivity within the body. EIT is a technique traditionally used in geophysics to map subsurface electrical conductivity. It might be used for tissue property monitoring and lung imaging. | [31] |
| Magnetoencephalography (MEG) | MEG measures the magnetic fields produced by neural activity in the brain and is derived from techniques for detecting electromagnetic signals from Earth’s magnetic field. It is employed in neuroscience research and offers useful insights into how the brain functions. | [32] |
| Ultrasound Imaging | High-frequency sound waves are used in ultrasound procedures to produce images of soft tissues and organs. These techniques were inspired by seismic approaches. For real-time visualization, it is commonly utilized in obstetrics, cardiology, and other medical disciplines. | [33] |
| Elastography | Elastography techniques, which were adopted from seismic technologies, measure the movement of mechanical waves across the body to determine the stiffness of the tissue. These data are useful for identifying anomalies and evaluating tissue health. | [34] |
| Computerized Tomography (CT) | CT scans, which employ X-rays to create cross-sectional images of the body, are not directly geophysical methods. There are similarities between the reconstruction algorithms used in CT imaging and the tomographic methods used in geophysics. | [35,36] |
| Positron Emission Tomography (PET) | PET imaging picks up injected positron-emitting radionuclides. Although not explicitly a geophysics technique, the concepts of gamma-ray detection are comparable to those of the gamma-ray spectrometry used in geophysics. | [37,38] |
| Functional MRI (fMRI) | fMRI is an advancement above conventional MRI in that it maps brain activity by monitoring changes in blood flow and oxygenation. This method sheds light on the cognitive functions and functional connectivity of the brain. | [39] |
| Diffusion Tensor Imaging (DTI) | DTI, which is based on the diffusion of water molecules, is a technique used in neuroimaging to show the neuronal connections and pathways in the brain. Diffusion-based geophysical techniques serve as the basis for this strategy. | [40] |
| NMR Spectroscopy | NMR spectroscopy, which is derived from NMR methods used to study molecular structures and is utilized in medical settings to examine biological molecules, is an area of study in molecular biology and medicine. | [41] |
| Near-Infrared Spectroscopy (NIRS) | The NIRS technique evaluates the tissues’ near-infrared light absorption, which was first applied in geophysics to examine mineral composition. It is used in the health sciences to measure brain activity, monitor vital signs in neonatal care, and evaluate tissue oxygenation. | [42] |
| Photoacoustic Imaging | Photoacoustic imaging combines optical and ultrasonic approaches and is inspired by seismic methods. By sensing the acoustic waves that tissues emit when they absorb laser-generated light, it creates images. High-resolution imaging of tumors, blood arteries, and other structures is made possible by this method. | [43] |
| Fluorescence Imaging | Despite not being a direct geophysics tool, fluorescence imaging is analogous to how fluorescence is used in geology. Fluorescent molecules are employed to mark certain cells in medical settings, facilitating cellular imaging, cancer diagnosis, and therapeutic development. | [44] |
| Terahertz Imaging | Terahertz imaging uses terahertz radiation, which was first applied to astronomy and atmospheric research, to see inside biological tissues. This method may be used to evaluate tissue characteristics and detect skin malignancies. | [45] |
| Biomechanical Analysis | The ideas of analyzing material qualities and deformation in geophysics have influenced biomechanical analysis in the health sciences; however, this is not a specific geophysics technique. Biomechanical analysis includes determining how organs and tissues react to mechanical forces, assisting in the creation of orthotics and prostheses, and comprehending how people move. | [46] |
| Working | Principle | Applications | Mathematical Expressions | Refs. |
|---|---|---|---|---|
| Electromagnetic Induction | ||||
| A transmitter coil is used to produce a magnetic field that changes over time. Electrical currents are induced in conductive subsurface materials as a result. Receiver coils at the surface detect the secondary magnetic fields that are produced as a result of these induced currents. | Faraday’s law of electromagnetic induction | Groundwater exploration, mineral resource identification | E = − . Where E is the induced electrical field, is electrical conductivity, and is the rate of change of the magnetic field. | [48,49] |
| Ground Penetrating Radar (GPR) | ||||
| Short electromagnetic pulses are released into the ground using GPR. The travel period of these pulses is measured after they reflect off subsurface contacts. Information about the depth and characteristics of subsurface features can be gleaned from the timing of the reflected waves. | EM wave reflection at material boundaries | Archaeology, environmental studies, detecting buried objects | d = Where t is the time taken for the signal to travel to the subsurface and back, ϑ is the wave speed, and d is the depth. | [53,54] |
| Magnetotellurics (MT) | ||||
| Earth’s electromagnetic field naturally varies owing to interactions with the sun and other celestial bodies, as measured by MT. A variety of frequencies are used to record these fluctuations. Earth’s impedance response sheds light on changes in subsurface resistivity. | The penetration of electromagnetic waves is influenced by the conductivity of Earth. | Mapping subsurface structures, understanding geological formations | The ratio of the vertical electric field (Ez) to the horizontal magnetic field (Hy) is used to calculate the impedance (Z) Z = | [20,55] |
| Description | Working | Applications | Refs. |
|---|---|---|---|
| Electrical Impedance Tomography (EIT) | |||
| When using EIT, which is a non-invasive imaging approach, tiny electrical currents are passed through biological tissues and the surface voltage changes that arise are then measured. The electrical conductivity distribution throughout the body can be precisely analyzed by EIT to yield specific information that, in turn, reveals important insights about the interior structures and physiological processes. Electrical techniques are employed in geophysics to examine Earth’s subsurface by observing changes in electrical conductivity. Similarly to this, EIT uses electrical conductivity’s fundamental concepts but applies them to medical imaging. | EIT involves applying electrode arrays to the surface of the body. The voltage distribution that results from the injection of a safe electric current into the body by these electrodes is monitored. EIT reconstructs a tomographic image of the internal conductivity distribution by utilizing various electrode configurations and examining the voltage variations. The anatomy, blood flow, ventilation, and even the ability to spot abnormalities like tumors or edema can all be learned from this image. | Lung imaging, brain and breast imaging | [31,56] |
| Magnetotellurics (MEG) | |||
| Measuring the magnetic fields generated by neural activity in the brain is possible using MEG, a potent neuroimaging technology utilized in the health sciences. With remarkable temporal and spatial resolution, MEG offers useful insights into brain function, connection, and localization of brain activity. Interestingly, geophysics and the study of Earth’s magnetic field are where MEG gets its start. This method aids in mapping the electrical conductivity of Earth’s subsurface in geophysics. Similar to this, MEG uses electromagnetic induction’s basic principles to measure neural activity. | It operates by taking measurements of the weak magnetic fields generated by the electrical activity of brain cells. SQUIDs (superconducting quantum interference devices), the incredibly sensitive sensors used in MEG systems, are capable of detecting these minute magnetic fields. Small electrical currents are produced by activated brain neurons. Beyond the skull and scalp, these currents generate magnetic fields that relate to them. The head is surrounded by MEG sensors that are used to identify these magnetic fields. With exceptional temporal and spatial precision, MEG can map the brain’s activity by carefully examining the timing and distribution of these magnetic signals. | Detecting anomalies in the brain and assisting with pre-surgical planning for diseases like epilepsy | [57,58] |
| Functional Electrical Stimulation (FES) | [59,60] | ||
| FES (FES), a medical treatment used in the health sciences, uses regulated electrical currents to help paralyzed or weak muscles regain or improve their function. Electrical impulses are delivered to specific muscles or nerves during FES, prompting them to contract and produce movement. For people with diseases like spinal cord injuries, strokes, or neuromuscular abnormalities, this method is especially helpful. Although FES is not directly related to geophysics, its basic principles have some loose similarities to geophysical ideas. The fundamentals of electrical currents and their effects on materials are fundamental to both fields and electrical methods are utilized in geophysics to examine subsurface conductivity variations. | FES works by implanting electrodes near the target location or placing electrodes on the skin to provide regulated electrical pulses to muscles or nerves. These electrical impulses cause muscle contractions, enabling people with paralysis or weak muscles to carry out practical motions like standing or walking. | Stroke rehabilitation, neuromuscular disorders, orthopedic rehabilitation, pain management, neuroprosthetics | |
| Cardiac Electrophysiology Mapping | |||
| Cardiac electrophysiology mapping is a sophisticated method used to visualize and examine the electrical activity of the heart. This approach assists in recognizing irregular heart rhythms (arrhythmias), locating their causes, and directing medical procedures like catheter ablation. Cardiac electrophysiology mapping entails mapping the electrical signals of the heart in great detail to diagnose and treat a variety of cardiac diseases. Cardiac electrophysiology mapping and geophysical methods can be broadly compared by understanding how electrical currents spread across a medium, although this is not directly related to geophysics. | To capture the electrical activity of the heart, electrode-equipped catheters are inserted into the organ. Electrical signals go through the heart’s chambers as it beats. These impulses are picked up by the electrodes, which produce fine-grained maps that depict the strength and order of the signals in various heart areas. | Arrhythmia diagnosis, catheter ablation guidance, ventricular tachycardia localization, atrial fibrillation management, Wolff–Parkinson–White syndrome, ventricular fibrillation risk assessment | [61,62] |
| Microwave Imaging | |||
| A developing method in the health sciences called microwave imaging uses electromagnetic radiation in the microwave frequency range to produce images of biological tissues. To visualize internal structures and abnormalities, microwave imaging makes use of the interaction between tissues and microwaves to highlight changes in their dielectric characteristics. The similarities between electromagnetic wave propagation and imaging can be used to create connections between microwave imaging and geophysics. Electromagnetic techniques are used in geophysics to investigate material characteristics and underlying structures. The fundamental idea of employing electromagnetic waves to obtain data is present in both domains, despite the scales and circumstances being different. | This entails sending microwaves into the body and observing how they affect the tissues. Due to differences in composition, different tissues have unique dielectric characteristics. These tissues reflect, absorb, or disperse microwaves differently as they travel through the body. The changing microwave signals are captured by sensitive receivers and the data are processed by sophisticated algorithms to produce images that show the spread of dielectric characteristics. | Breast cancer detection, tumor monitoring, brain imaging, musculoskeletal imaging, monitoring of tissue changes, stroke detection | [63,64,65] |
| Description | Working | Applications | Refs. |
|---|---|---|---|
| Ultrasound Imaging | |||
| Ultrasound imaging is a non-invasive, safe, and extensively used medical imaging technique that employs high-frequency sound waves (ultrasound) to produce real-time images of the body’s internal components. While geophysics studies Earth’s subsurface with seismic waves, ultrasonography visualizes internal structures with sound waves. To reveal concealed information, both areas rely on wave interactions, reflection, and imaging techniques. | The notion of sound wave reflection underpins ultrasound imaging. A transducer sends ultrasonic waves into the body that bounce off tissues and organs to create echoes. These echoes are received by the transducer and converted into electrical impulses. A computer then processes these impulses to generate visuals that are displayed on a monitor. | Obstetrics and gynecology, cardiology, abdominal imaging, musculoskeletal imaging, vascular imaging, breast imaging | [73,74] |
| Elastography | |||
| Elastography is a type of medical imaging that assesses the stiffness or elasticity of tissues. It offers information about the mechanical properties of tissues, assisting in the identification of anomalies and assessing circumstances that affect tissue stiffness. In geophysics, seismic waves move through the subsurface of Earth and interact with various rock layers to disclose details about their characteristics. Like this, elastography interacts with tissues using mechanical waves, assesses their reaction, and reveals information about the characteristics of the tissues. | Elastography is the process of applying mechanical forces to tissues and monitoring how they respond. Elastography techniques include shear-wave elastography, strain elastography, and magnetic resonance elastography. Shear-wave elastography is commonly used to create shear waves within tissues using ultrasound or other mechanical techniques. The speed of these shear waves as they propagate through the tissue is measured. Shear waves are transmitted faster by stiffer tissues than by softer ones. | Cancer detection, liver fibrosis assessment, breast imaging, musculoskeletal disorders, cardiovascular health | [75,76,77] |
| Acoustic Radiation Force Imaging (ARFI) | |||
| Focused ultrasound beams are utilized in this medical imaging approach to cause mechanical vibrations in the tissues. ARFI measures the ensuing tissue displacement to determine the stiffness of the tissue, which helps in the diagnosis of various medical diseases. Seismic waves interact with underground formations in geophysics and provide data on their characteristics. Similar to this, ARFI uses sonic waves to interact with tissues and then measures the response to infer information about the tissues. Both fields make use of the idea of wave interaction to learn more about the structure and properties of a medium. | Short bursts of extremely intense ultrasound waves are used in ARFI to penetrate the body. The acoustic radiation force exerted by these waves causes localized vibrations in the tissues. The displacement of tissue because of these vibrations is then detected by sensors. The amount of tissue displacement is directly correlated with the stiffness of the tissue: softer tissues exhibit greater displacement, whereas stiffer tissues exhibit less. | Liver disease assessment, breast imaging, musculoskeletal disorders | [78,79] |
| Shear-Wave Dispersion Ultrasound Vibrometry | |||
| This is a cutting-edge medical imaging method that evaluates tissue stiffness by examining the shear-wave dispersion within tissues. It aids in the diagnosis of disorders like liver fibrosis by giving insights into the mechanical characteristics of tissues, particularly their viscoelastic behavior. Due to underlying characteristics, different kinds of seismic waves move at varying rates in geophysics. Seismic shear waves, for instance, show dispersion in geological formations. Like this, SDUV uses shear wave dispersion to give details about the mechanical characteristics of the tissue. | Focused ultrasound beams are emitted by SDUV to create shear waves inside tissues. Multiple frequencies are used to measure the pace at which these shear waves move through the tissues. Due to their viscoelastic characteristics, tissues respond to shear waves in different ways and at different frequencies. SDUV gives data on tissue stiffness and viscosity by examining the shear-wave speed dispersion across frequencies. | Liver fibrosis assessment, musculoskeletal disorders | [75,80] |
| Techniques | Description | Refs. |
|---|---|---|
| Functional MRI (fMRI) | fMRI uses blood flow fluctuations to pinpoint the brain’s active regions. It is essential to neuroscience and the comprehension of how the brain processes language, memory, and emotion. In clinical contexts, fMRI aids in the diagnosis of neurological illnesses, assists in mapping brain activity before surgery, and tracks therapeutic responses. | [88,89] |
| Diffusion MRI | This method evaluates how water molecules travel within tissues. It is extremely useful for neuroimaging, especially in the diagnosis of stroke and the investigation of white matter integrity. The use of diffusion MRI enables the early detection of brain injury and sheds light on neurodegenerative illnesses. | [90,91] |
| Perfusion MRI | Perfusion imaging analyzes blood flow to tissues, which helps in tumor evaluation and stroke detection. In ischemic strokes, it aids in separating viable from non-viable tissue and directs therapeutic choices. | [92,93] |
| Magnetic Resonance Angiography (MRA) | MRA reduces the requirement for contrast chemicals by non-invasively visualizing blood vessels. It is employed in determining aneurysms, evaluating vascular anomalies, and organizing interventions. | [94,95] |
| Spectroscopic Imaging | This method determines the chemical composition of tissues, allowing for metabolic evaluations. Spectroscopic imaging improves tumor characterization in oncology by distinguishing between malignant and healthy tissue. | [96,97] |
| 3D and 4D Imaging | Modern imaging methods provide real-time, four-dimensional and three-dimensional views of organs and structures. This makes it easier to visualize dynamic movements, intricate anatomical linkages, and cardiac activity. | [85] |
| Ultra-High Field MRI | Greater spatial and temporal resolution is made possible by stronger magnetic fields (7T and higher). The visualization of small structures, such as blood arteries, joints, and the brain, is enhanced by ultra-high field MRI, which enhances diagnostic precision. | [83,84] |
| Quantitative MRI | By measuring particular tissue characteristics like T1 and T2 relaxation periods, this method makes it easier to distinguish between healthy and sick tissues. It helps determine the severity of diseases including multiple sclerosis and liver fibrosis. | [98] |
| AI Integration | AI-driven methods help automate image interpretation, improve image quality, and shorten scan times. AI tools help radiologists spot problems and boost their level of diagnostic assurance. | [99,100] |
| Challenges | Description |
|---|---|
| Biological variability | Because of variables like age, gender, heredity, and health problems, biological tissues are fundamentally varied. The interpretation of geophysical data may be impacted by this variability, necessitating the use of robust statistical techniques to take this into account and distinguish between normal and aberrant fluctuations |
| Resolution and sensitivity | Compared to geological materials, biological tissues are frequently more delicate and irregular in texture. It might be difficult to achieve great resolution and sensitivity while protecting tissue integrity. To spot tiny changes and anomalies without causing harm, techniques must be improved |
| Signal attenuation and scattering | Signals can attenuate and scatter differently in biological tissues compared with in geological ones. The accuracy of the data gathered may be impacted by diminished signal penetration and distortion as a result. Techniques must be improved to take tissue-specific signal behaviors into account |
| Electromagnetic interference | Electromagnetic interference can be introduced by biological tissues and affect data capture. To obtain accurate results, strategies to reduce or adjust for this interference are essential |
| Biocompatibility and safety | Patient safety is of the utmost concern. Strict safety guidelines must be followed while using geophysical techniques in the health sciences to protect human subjects from radiation exposure, magnetic fields, and other dangers |
| Biological noise | Background noise produced by biological tissues may conceal signals of interest. Techniques for signal processing must be specifically designed to successfully remove biological noise while maintaining important data |
| Multi-modality integration | Geophysical approaches must be seamlessly coordinated with other medical imaging modalities and involve the merging of data from many sources. To offer thorough insights, this necessitates complex software and algorithms |
| Ethical considerations | The use of geophysical methods in the health sciences frequently entails using patient data and human participants. To ensure ethical and accountable research practices, patient consent and data privacy must be taken into account |
| Biological models | It is crucial to create precise models that accurately depict the intricate behavior of actual tissues. These models help with the interpretation of results in the context of biology and assist the adaption of geophysical approaches |
| Interdisciplinary collaboration | Effective teamwork amongst professionals from various backgrounds is necessary to close the gap between geophysics and the health sciences. To overcome obstacles and make use of each field’s strengths, effective communication and shared understanding are vital |
| Scope | Description |
|---|---|
| Enhanced Imaging and Analysis | In geophysics-driven medical imaging, ML and AI algorithms can enhance image quality, resolution, and noise reduction. These methods could correct data flaws, improving the accuracy and clarity of photographs |
| Automated Diagnosis and Detection | To automatically discover patterns linked with different medical disorders in geophysical data, ML algorithms can be taught on large datasets. These algorithms might act as “virtual radiologists,” assisting in the quick and precise diagnosis of diseases |
| Predictive Analytics | AI algorithms could forecast illness progression, identify potential risk factors, and suggest personalized treatment methods by examining previous geophysical and medical data, adding to proactive healthcare initiatives |
| Precision Medicine | Geophysical data analysis powered by AI can assist in customizing medical interventions for specific patients. This could entail anticipating treatment outcomes based on tissue characteristics, improving drug distribution, and reducing adverse effects. |
| Real-Time Monitoring | Geophysical data might be continuously monitored by ML-enabled systems, alerting medical staff to minute changes in tissue qualities. This might come in handy during operations or in critical care settings |
| Cross-Modality Fusion | Geophysical data and other types of medical imaging can be combined using AI algorithms to create a full picture of a patient’s state. This might result in more precise diagnoses and wiser treatment choices |
| Automated Workflow Optimization | Geophysical data processing and gathering in medical applications can be streamlined with ML. It might alter the scanner settings in real-time, speeding up scans and improving patient comfort |
| Novel Biomarkers | Geophysical data analysis powered by AI may produce new biomarkers for tracking the development of disease. These biomarkers may be used to monitor and detect diseases like cancer and neurological illnesses early on |
| Unveiling Complex Interactions | ML can reveal complex connections between geophysical characteristics and biological functions. This may provide a deeper understanding of the progression of diseases and the impact of treatments on tissue characteristics |
| Data-Driven Research | By automating data analysis and hypothesis testing, the use of AI in geophysics-driven medical imaging can speed up research while letting scientists concentrate on analyzing data and formulating studies |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, R.K.; Nayak, N.P.; Behl, T.; Arora, R.; Anwer, M.K.; Gulati, M.; Bungau, S.G.; Brisc, M.C. Exploring the Intersection of Geophysics and Diagnostic Imaging in the Health Sciences. Diagnostics 2024, 14, 139. https://doi.org/10.3390/diagnostics14020139
Singh RK, Nayak NP, Behl T, Arora R, Anwer MK, Gulati M, Bungau SG, Brisc MC. Exploring the Intersection of Geophysics and Diagnostic Imaging in the Health Sciences. Diagnostics. 2024; 14(2):139. https://doi.org/10.3390/diagnostics14020139
Chicago/Turabian StyleSingh, Rahul Kumar, Nirlipta Priyadarshini Nayak, Tapan Behl, Rashmi Arora, Md. Khalid Anwer, Monica Gulati, Simona Gabriela Bungau, and Mihaela Cristina Brisc. 2024. "Exploring the Intersection of Geophysics and Diagnostic Imaging in the Health Sciences" Diagnostics 14, no. 2: 139. https://doi.org/10.3390/diagnostics14020139






