Predictive Factors Correlated with Successful Early Endoscopic Removal of Pancreaticolithiasis in Chronic Pancreatitis after Extracorporeal Shock Wave Lithotripsy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
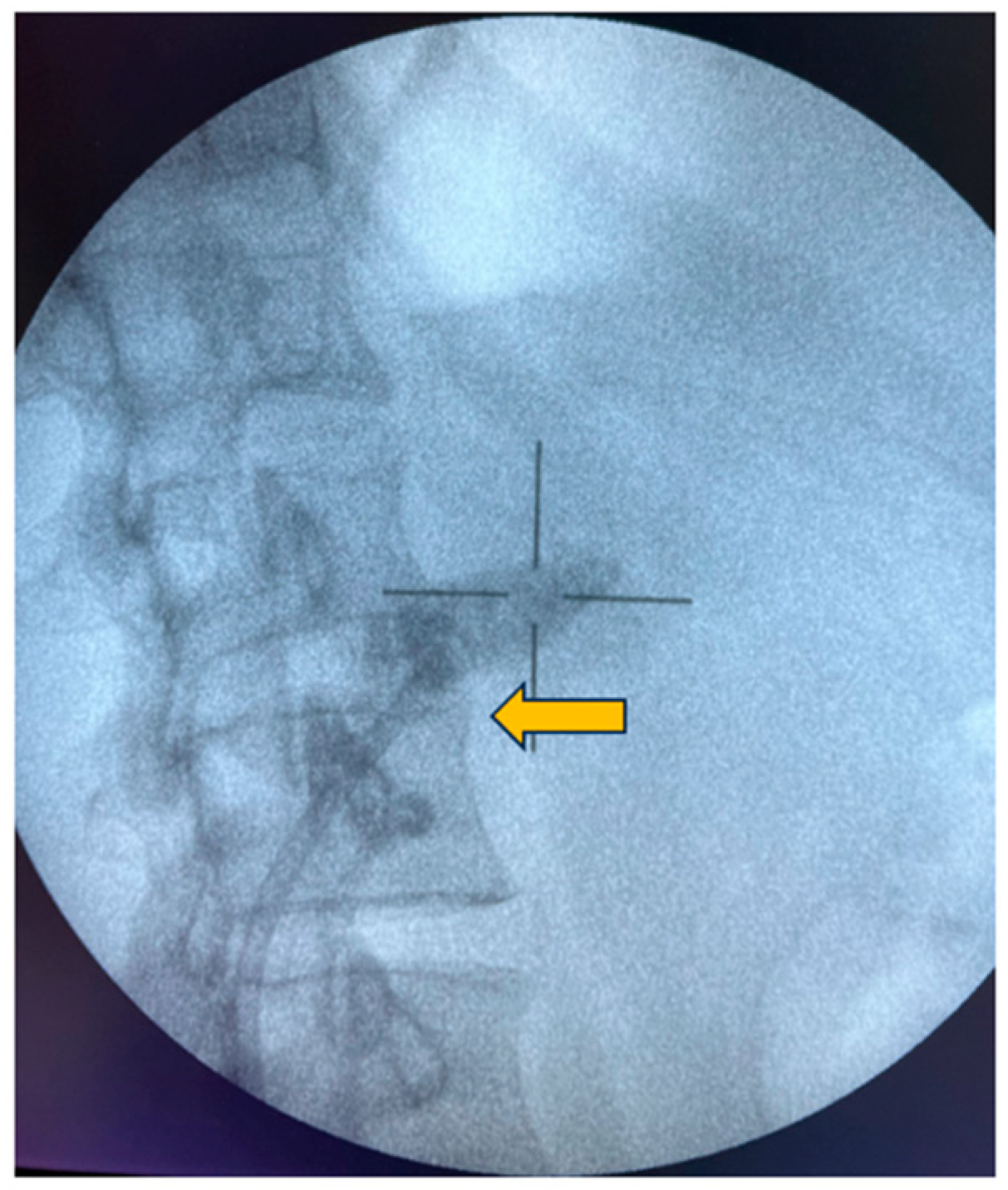
2.2. Extracorporeal Shock Wave Lithotripsy
2.3. Post-ESWL ERCP
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Majumder, S.; Chari, S.T. Chronic pancreatitis. Lancet 2016, 387, 1957–1966. [Google Scholar] [CrossRef] [PubMed]
- Ushio, J.; Kanno, A.; Ikeda, E.; Ando, K.; Nagai, H.; Miwata, T.; Kawasaki, Y.; Tada, Y.; Yokoyama, K.; Numao, N.; et al. Pancreatic Ductal Adenocarcinoma: Epidemiology and Risk Factors. Diagnostics 2021, 11, 562. [Google Scholar] [CrossRef]
- Garg, P.K.; Tandon, R.K. Survey on chronic pancreatitis in the Asia–Pacific region. J. Gastroenterol. Hepatol. 2004, 19, 998–1004. [Google Scholar] [CrossRef] [PubMed]
- Lévy, P.; Domínguez-Muñoz, E.; Imrie, C.; Löhr, M.; Maisonneuve, P. Epidemiology of chronic pancreatitis: Burden of the disease and consequences. United Eur. Gastroenterol. J. 2014, 2, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Stevens, T.; Conwell, D.L.; Zuccaro, G. Pathogenesis of chronic pancreatitis: An evidence-based review of past theories and recent developments. Off. J. Am. Coll. Gastroenterol. 2004, 99, 2256–2270. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, C.M.; Yadav, D.; Ye, T.; Gardner, T.B.; Gelrud, A.; Sandhu, B.S.; Lewis, M.D.; Al-Kaade, S.; Cote, G.A.; Forsmark, C.E. Chronic pancreatitis pain pattern and severity are independent of abdominal imaging findings. Clin. Gastroenterol. Hepatol. 2015, 13, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Li, B.-R.; Pan, J.; Du, T.-T.; Liao, Z.; Ye, B.; Zou, W.-B.; Chen, H.; Ji, J.-T.; Zheng, Z.-H.; Wang, D. Risk factors for steatorrhea in chronic pancreatitis: A cohort of 2153 patients. Sci. Rep. 2016, 6, 21381. [Google Scholar] [CrossRef] [PubMed]
- Frøkjær, J.B.; Olesen, S.S.; Drewes, A.M. Fibrosis, atrophy, and ductal pathology in chronic pancreatitis are associated with pancreatic function but independent of symptoms. Pancreas 2013, 42, 1182–1187. [Google Scholar] [CrossRef]
- Machicado, J.D.; Chari, S.T.; Timmons, L.; Tang, G.; Yadav, D. A population-based evaluation of the natural history of chronic pancreatitis. Pancreatology 2018, 18, 39–45. [Google Scholar] [CrossRef]
- Mokrowiecka, A.; Pińkowski, D.; Małecka-Panas, E. Assessment of quality of life in patients with chronic pancreatitis. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2011, 17, CR583. [Google Scholar]
- Tandan, M.; Reddy, D.N.; Santosh, D.; Vinod, K.; Ramchandani, M.; Rajesh, G.; Rama, K.; Lakhtakia, S.; Banerjee, R.; Pratap, N. Extracorporeal shock wave lithotripsy and endotherapy for pancreatic calculi—A large single center experience. Indian J. Gastroenterol. 2010, 29, 143–148. [Google Scholar] [CrossRef]
- Rösch, T.; Daniel, S.; Scholz, M.; Huibregtse, K.; Smits, M.; Schneider, T.; Ell, C.; Haber, G.; Riemann, J.; Jakobs, R. European Society of Gastrointestinal Endoscopy Research Group: Endoscopic treatment of chronic pancreatitis: A multicenter study of 1000 patients with long-term follow-up. Endoscopy 2002, 34, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Maydeo, A.; Soehendra, N.; Reddy, N.; Bhandari, S. Endotherapy for chronic pancreatitis with intracanalar stones. Endoscopy 2007, 39, 653–658. [Google Scholar] [CrossRef]
- Ammann, R.; Muench, R.; Otto, R.; Buehler, H.; Freiburghaus, A.; Siegenthaler, W. Evolution and regression of pancreatic calcification in chronic pancreatitis: A prospective long-term study of 107 patients. Gastroenterology 1988, 95, 1018–1028. [Google Scholar] [CrossRef] [PubMed]
- Tandan, M.; Talukdar, R.; Reddy, D.N. Management of pancreatic calculi: An update. Gut Liver 2016, 10, 873. [Google Scholar] [CrossRef] [PubMed]
- Tandan, M.; Reddy, D.N. Extracorporeal shock wave lithotripsy for pancreatic and large common bile duct stones. World J. Gastroenterol. WJG 2011, 17, 4365. [Google Scholar] [CrossRef] [PubMed]
- Dumonceau, J.-M.; Delhaye, M.; Tringali, A.; Arvanitakis, M.; Sanchez-Yague, A.; Vaysse, T.; Aithal, G.P.; Anderloni, A.; Bruno, M.; Cantú, P. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) guideline–updated August 2018. Endoscopy 2019, 51, 179–193. [Google Scholar] [CrossRef]
- Tandan, M.; Reddy, D. ESWL of large pancreatic calculi: A decades experience. United Eur. Gastroenterol. J. 2014, 2, A7. [Google Scholar]
- Seven, G.; Schreiner, M.A.; Ross, A.S.; Lin, O.S.; Gluck, M.; Gan, S.I.; Irani, S.; Brandabur, J.J.; Patterson, D.; Kuhr, C. Long-term outcomes associated with pancreatic extracorporeal shock wave lithotripsy for chronic calcific pancreatitis. Gastrointest. Endosc. 2012, 75, 997–1004.e1001. [Google Scholar] [CrossRef]
- Tadenuma, H.; Ishihara, T.; Yamaguchi, T.; Tsuchiya, S.; Kobayashi, A.; Nakamura, K.; Sakurada, R.; Saisho, H. Long-term results of extracorporeal shockwave lithotripsy and endoscopic therapy for pancreatic stones. Clin. Gastroenterol. Hepatol. 2005, 3, 1128–1135. [Google Scholar] [CrossRef]
- Liu, R.; Su, W.; Wang, J.; Gong, J.; Lu, J. Quantitative factors of unenhanced CT for predicting fragmenting efficacy of extracorporeal shock wave lithotripsy on pancreatic duct stones. Clin. Radiol. 2019, 74, 408.e1–408.e7. [Google Scholar] [CrossRef]
- Lapp, R.T.; Wolf Jr, J.S.; Faerber, G.J.; Roberts, W.W.; McCarthy, S.T.; Anderson, M.A.; Wamsteker, E.-J.; Elta, G.H.; Scheiman, J.M.; Kwon, R.S. Duct diameter and size of stones predict successful extracorporeal shock wave lithotripsy and endoscopic clearance in patients with chronic pancreatitis and pancreaticolithiasis. Pancreas 2016, 45, 1208–1211. [Google Scholar] [CrossRef] [PubMed]
- Howell, D.A.; Dy, R.M.; Hanson, B.L.; Nezhad, S.F.; Broaddus, S.B. Endoscopic treatment of pancreatic duct stones using a 10F pancreatoscope and electrohydraulic lithotripsy. Gastrointest. Endosc. 1999, 50, 829–833. [Google Scholar] [CrossRef] [PubMed]
- Attwell, A.R.; Patel, S.; Kahaleh, M.; Raijman, I.L.; Yen, R.; Shah, R.J. ERCP with per-oral pancreatoscopy–guided laser lithotripsy for calcific chronic pancreatitis: A multicenter US experience. Gastrointest. Endosc. 2015, 82, 311–318. [Google Scholar] [CrossRef] [PubMed]
- van der Wiel, S.E.; Stassen, P.M.; Poley, J.-W.; De Jong, D.M.; de Jonge, P.J.F.; Bruno, M.J. Pancreatoscopy-guided electrohydraulic lithotripsy for the treatment of obstructive pancreatic duct stones: A prospective consecutive case series. Gastrointest. Endosc. 2022, 95, 905–914.e2. [Google Scholar] [CrossRef]
- Ohyama, H.; Mikata, R.; Ishihara, T.; Tsuyuguchi, T.; Sakai, Y.; Sugiyama, H.; Yasui, S.; Ishii, K.; Itoh, S.; Nishikawa, T. Efficacy of stone density on noncontrast computed tomography in predicting the outcome of extracorporeal shock wave lithotripsy for patients with pancreatic stones. Pancreas 2015, 44, 422–428. [Google Scholar] [CrossRef]
- Lee, T.H.; Park, D.H. Endoscopic prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis. World J. Gastroenterol. WJG 2014, 20, 16582. [Google Scholar] [CrossRef]
- Inui, K.; Tazuma, S.; Yamaguchi, T.; Ohara, H.; Tsuji, T.; Miyagawa, H.; Igarashi, Y.; Nakamura, Y.; Atomi, Y. Treatment of pancreatic stones with extracorporeal shock wave lithotripsy: Results of a multicenter survey. Pancreas 2005, 30, 26–30. [Google Scholar]
- Dumonceau, J.-M.; Costamagna, G.; Tringali, A.; Vahedi, K.; Delhaye, M.; Hittelet, A.; Spera, G.; Giostra, E.; Mutignani, M.; De Maertelaer, V. Treatment for painful calcified chronic pancreatitis: Extracorporeal shock wave lithotripsy versus endoscopic treatment: A randomised controlled trial. Gut 2007, 56, 545–552. [Google Scholar] [CrossRef]
- Sherman, S.; Lehman, G.A.; Hawes, R.H.; Ponich, T.; Miller, L.S.; Cohen, L.B.; Kortan, P.; Haber, G.B. Pancreatic ductal stones: Frequency of successful endoscopic removal and improvement in symptoms. Gastrointest. Endosc. 1991, 37, 511–517. [Google Scholar] [CrossRef]
- Li, B.-R.; Liao, Z.; Du, T.-T.; Ye, B.; Zou, W.-B.; Chen, H.; Ji, J.-T.; Zheng, Z.-H.; Hao, J.-F.; Jiang, Y.-Y. Risk factors for complications of pancreatic extracorporeal shock wave lithotripsy. Endoscopy 2014, 46, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
- Fockens, P.; Besselink, M.G.; Boermeester, M.A.; Arvanitakis, M.; van Hooft, J.E. Success of extracorporeal shock wave lithotripsy and ERCP in symptomatic pancreatic duct stones: A systematic review and meta-analysis. Endosc. Int. Open 2020, 8, E1070–E1085. [Google Scholar]



| Variables | Total (n = 27) | Early Endoscopic Removal ≤ 3 (n = 20) | Late Endoscopic Removal > 3 (n = 7) | p-Value |
|---|---|---|---|---|
| Characteristics of patients | ||||
| Age, mean (SD), y | 44 (9.6) | 44.1 (9.7) | 43.9 (9.9) | 0.963 |
| Male, sex, n (%) | 20 (74.1) | 16 (80) | 4 (57.1) | 0.328 |
| BMI, mean (SD), kg/m2 | 20.6 (3.7) | 20.3 (4.1) | 21.6 (2.6) | 0.443 |
| Etiology of pancreatitis, n (%) | ||||
| Alcohol | 16 (59.3) | 12 (60) | 4 (57.1) | 0.902 |
| Others | 11 (40.3) | 8 (40) | 3 (42.9) | |
| Symptoms, n (%) | ||||
| Abdominal pain | 27 (100%) | 20 (100%) | 7 (100%) | N/A |
| Weight loss | 11 (40.7) | 10 (50%) | 1 (14.3%) | 0.183 |
| Steatorrhea | 6 (22.2) | 4 (20%) | 2 (28.6) | 0.633 |
| Interventions, n (%) | ||||
| Pre-ESWL ERCP | 15 (55.6%) | 10 (50%) | 5 (71.4%) | 0.408 |
| PD stent placement | 23 (85.2%) | 18 (90%) | 5 (71.4%) | 0.269 |
| MPD stricture | 18 (66.7%) | 13 (65%) | 5 (71.4%) | 1 |
| Total No. of post-ESWL ERCP, median (IQR) | 2 (2–3) | 2 (2–2.2) | 4 (3–5.5) | <0.001 |
| Total No. of ESWL, median (IQR) | 2 (1–4) | 2 (1–2.5) | 4 (2.5–5.5) | 0.122 |
| No. of shock, median (IQR) | 4501 (3000–5000) | 4750 (3000–5000) | 3856 (3071–4875) | 0.749 |
| Variables | Both Cohorts (n = 27) | Early Endoscopic Removal ≤ 3 (n = 20) | Late Endoscopic Removal > 3 (n = 7) | p-Value |
|---|---|---|---|---|
| No. of calculi, n (%) | 0.29 | |||
| Few (<3) | 6 (22.2%) | 3 (15%) | 3 (42.9%) | |
| Multiple (≥3) | 21 (77.8%) | 17 (85%) | 4 (58.1%) | |
| Location of calculi | ||||
| Head | 14 (51.9%) | 10 (50%) | 4 (57.1%) | 1 |
| Body | 5 (18.5%) | 5 (25%) | 0 (0) | 0.283 |
| Diffuse | 9 (33.3%) | 6 (30%) | 3 (42.9%) | 0.653 |
| Maximum diameter of calculi, median (IQR), mm | 9 (7.5,13.5) | 8.5 (7,13) | 19 (11.5,19.5) | 0.012 |
| Stone density, mean (SD), HU | 1055 (393.4) | 964.6 (382.3) | 1313.3 (320.6) | 0.041 |
| MPD size, mean (SD), mm | 9.4 (3.5) | 8.9 (2.9) | 10.7 (4.9) | 0.248 |
| Splenic vein thrombosis, n (%) | 22 (81.5%) | 5 (25) | 0 (0) | 0.283 |
| Pancreatic tail atrophy, n (%) | 15 (55.6%) | 10 (50) | 5 (71.4) | 0.408 |
| Factors | OR (95% CI) | p-Value |
|---|---|---|
| Calculus density < 1300 HU | 10 (1.39–71.86) | 0.032 |
| Maximum calculus size < 10 mm | 14 (1.37–142.89) | 0.029 |
| Pre-ESWL ERCP | 0.4 (0.06–2.57) | 0.095 |
| Etiology of alcohol | 1.12 (0.2–6.43) | 0.239 |
| PD stricture | 0.74 (0.11–4.87) | 0.754 |
| PD stent placement | 3.6 (0.4–32.37) | 0.259 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, T.; Pattarapuntakul, T.; Netinatsunton, N.; Ovartlarnporn, B.; Sottisuporn, J.; Yaowmaneerat, T.; Attasaranya, S.; Cattapan, K.; Sripongpun, P. Predictive Factors Correlated with Successful Early Endoscopic Removal of Pancreaticolithiasis in Chronic Pancreatitis after Extracorporeal Shock Wave Lithotripsy. Diagnostics 2024, 14, 172. https://doi.org/10.3390/diagnostics14020172
Wong T, Pattarapuntakul T, Netinatsunton N, Ovartlarnporn B, Sottisuporn J, Yaowmaneerat T, Attasaranya S, Cattapan K, Sripongpun P. Predictive Factors Correlated with Successful Early Endoscopic Removal of Pancreaticolithiasis in Chronic Pancreatitis after Extracorporeal Shock Wave Lithotripsy. Diagnostics. 2024; 14(2):172. https://doi.org/10.3390/diagnostics14020172
Chicago/Turabian StyleWong, Thanawin, Tanawat Pattarapuntakul, Nisa Netinatsunton, Bancha Ovartlarnporn, Jaksin Sottisuporn, Thanapon Yaowmaneerat, Siriboon Attasaranya, Kamonwon Cattapan, and Pimsiri Sripongpun. 2024. "Predictive Factors Correlated with Successful Early Endoscopic Removal of Pancreaticolithiasis in Chronic Pancreatitis after Extracorporeal Shock Wave Lithotripsy" Diagnostics 14, no. 2: 172. https://doi.org/10.3390/diagnostics14020172





