Differences in Anatomic Adaptation and Injury Patterns Related to Valgus Extension Overload in Overhead Throwing Athletes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Retrospective Review of MRI/MRA Images
2.3. Statistical Analysis
3. Results
3.1. Qualitative Changes
3.2. Quantitative Changes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Werner, S.L.; Murray, T.A.; Hawkins, R.J.; Gill, T.J. Relationship between throwing mechanics and elbow valgus in professional baseball pitchers. J. Shoulder Elbow Surg. 2002, 11, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, J.E. Adaptive Pathology: New Insights into the Physical Examination and Imaging of the Thrower’s Shoulder and Elbow. J. Shoulder Elbow Surg. 2023, 33, 474–493. [Google Scholar] [CrossRef] [PubMed]
- Triplet, J.J.; Labott, J.R.; Leland, D.P.; Cheema, A.; Till, S.E.; Kaufman, K.R.; Camp, C.L. Factors that Increase Elbow Stress in the Throwing Athlete: A Systematic Review of Biomechanical and Motion Analysis Studies of Baseball Pitching and Throwing. Curr. Rev. Musculoskelet. Med. 2023, 16, 115–122. [Google Scholar] [CrossRef]
- Dugas, J.R. Valgus extension overload: Diagnosis and treatment. Clin. Sports Med. 2010, 29, 645–654. [Google Scholar] [CrossRef]
- Patel, R.M.; Lynch, T.S.; Amin, N.H.; Calabrese, G.; Gryzlo, S.M.; Schickendantz, M.S. The thrower’s elbow. Orthop. Clin. N. Am. 2014, 45, 355–376. [Google Scholar] [CrossRef] [PubMed]
- Paulino, F.E.; Villacis, D.C.; Ahmad, C.S. Valgus Extension Overload in Baseball Players. Am. J. Orthop. 2016, 45, 144–151. [Google Scholar] [PubMed]
- Cain, E.L., Jr.; Dugas, J.R.; Wolf, R.S.; Andrews, J.R. Elbow injuries in throwing athletes: A current concepts review. Am. J. Sports Med. 2003, 31, 621–635. [Google Scholar] [CrossRef]
- Fleisig, G.S.; Andrews, J.R.; Dillman, C.J.; Escamilla, R.F. Kinetics of Baseball Pitching with Implications About Injury Mechanisms. Am. J. Sports Med. 1995, 23, 233–239. [Google Scholar] [CrossRef]
- Atanda, A., Jr.; Buckley, P.S.; Hammoud, S.; Cohen, S.B.; Nazarian, L.N.; Ciccotti, M.G. Early Anatomic Changes of the Ulnar Collateral Ligament Identified by Stress Ultrasound of the Elbow in Young Professional Baseball Pitchers. Am. J. Sports Med. 2015, 43, 2943–2949. [Google Scholar] [CrossRef]
- Makihara, T.; Okamoto, Y.; Yoshizawa, T.; Tanaka, K.; Ogawa, T.; Minami, M.; Yamazaki, M. Change in MRI findings of medial collateral ligament injury in adolescent baseball players with no clinical symptoms over time. Skeletal Radiol. 2019, 48, 1925–1932. [Google Scholar] [CrossRef]
- Marshall, N.E.; Keller, R.A.; Van Holsbeeck, M.; Moutzouros, V. Ulnar Collateral Ligament and Elbow Adaptations in High School Baseball Pitchers. Sports Health 2015, 7, 484–488. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Okamoto, Y.; Makihara, T.; Maehara, K.; Yoshizawa, T.; Minami, M.; Yamazaki, M. Clinical interpretation of asymptomatic medial collateral ligament injury observed on magnetic resonance imaging in adolescent baseball players. Jpn. J. Radiol. 2017, 35, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Yoshizawa, T.; Okamoto, Y.; Tanaka, K.; Makihara, T.; Tonoe, T.; Minami, M.; Yamazaki, M. Normal imaging laterality on magnetic resonance imaging of the medial epicondyle of the elbow on the dominant side of adolescent male baseball players. Skeletal Radiol. 2018, 47, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Sada, K.; Chiba, K.; Kajiyama, S.; Okazaki, N.; Yonekura, A.; Tomita, M.; Osaki, M. Bone Mineral Density and Microstructure of the Elbow in Baseball Pitchers: An Analysis by Second-Generation HR-pQCT. J. Clin. Densitom. 2020, 23, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Gustas, C.N.; Lee, K.S. Multimodality Imaging of the Painful Elbow: Current Imaging Concepts and Image-Guided Treatments for the Injured Thrower’s Elbow. Radiol. Clin. N. Am. 2016, 54, 817–839. [Google Scholar] [CrossRef] [PubMed]
- Ouellette, H.; Bredella, M.; Labis, J.; Palmer, W.E.; Torriani, M. MR imaging of the elbow in baseball pitchers. Skeletal Radiol. 2008, 37, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Furushima, K.; Itoh, Y.; Iwabu, S.; Yamamoto, Y.; Koga, R.; Shimizu, M. Classification of Olecranon Stress Fractures in Baseball Players. Am. J. Sports Med. 2014, 42, 1343–1351. [Google Scholar] [CrossRef] [PubMed]
- Logli, A.L.; Bernard, C.D.; O’Driscoll, S.W.; Sanchez-Sotelo, J.; Morrey, M.E.; Krych, A.J.; Camp, C.L. Osteochondritis dissecans lesions of the capitellum in overhead athletes: A review of current evidence and proposed treatment algorithm. Curr. Rev. Musculoskelet. Med. 2019, 12, 1–12. [Google Scholar] [CrossRef]
- Wei, A.S.; Khana, S.; Limpisvasti, O.; Crues, J.; Podesta, L.; Yocum, L.A. Clinical and magnetic resonance imaging findings associated with Little League elbow. J. Pediatr. Orthop. 2010, 30, 715–719. [Google Scholar] [CrossRef]
- Osbahr, D.C.; Dines, J.S.; Breazeale, N.M.; Deng, X.H.; Altchek, D.W. Ulnohumeral chondral and ligamentous overload: Biomechanical correlation for posteromedial chondromalacia of the elbow in throwing athletes. Am. J. Sports Med. 2010, 38, 2535–2541. [Google Scholar] [CrossRef]
- Kooima, C.L.; Anderson, K.; Craig, J.V.; Teeter, D.M.; van Holsbeeck, M. Evidence of subclinical medial collateral ligament injury and posteromedial impingement in professional baseball players. Am. J. Sports Med. 2004, 32, 1602–1606. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.B.; Valko, C.; Zoga, A.; Dodson, C.C.; Ciccotti, M.G. Posteromedial elbow impingement: Magnetic resonance imaging findings in overhead throwing athletes and results of arthroscopic treatment. Arthroscopy 2011, 27, 1364–1370. [Google Scholar] [CrossRef] [PubMed]
- Del Grande, F.; Aro, M.; Farahani, S.J.; Wilckens, J.; Cosgarea, A.; Carrino, J.A. Three-Tesla MR imaging of the elbow in non-symptomatic professional baseball pitchers. Skeletal Radiol. 2015, 44, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Regan, W.D.; Korinek, S.L.; Morrey, B.F.; An, K.N. Biomechanical study of ligaments around the elbow joint. Clin. Orthop. Relat. Res. 1991, 271, 170–179. [Google Scholar] [CrossRef]
- Bruce, J.R.; Hess, R.; Joyner, P.; Andrews, J.R. How much valgus instability can be expected with ulnar collateral ligament (UCL) injuries? A review of 273 baseball players with UCL injuries. J. Shoulder Elbow Surg. 2014, 23, 1521–1526. [Google Scholar] [CrossRef] [PubMed]
- Funakoshi, T.; Furushima, K.; Momma, D.; Endo, K.; Abe, Y.; Itoh, Y.; Fujisaki, K.; Tadano, S.; Iwasaki, N. Alteration of Stress Distribution Patterns in Symptomatic Valgus Instability of the Elbow in Baseball Players: A Computed Tomography Osteoabsorptiometry Study. Am. J. Sports Med. 2016, 44, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Hurd, W.J.; Jazayeri, R.; Mohr, K.; Limpisvasti, O.; ElAttrache, N.S.; Kaufman, K.R. Pitch Velocity Is a Predictor of Medial Elbow Distraction Forces in the Uninjured High School–Aged Baseball Pitcher. Sports Health 2012, 4, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Garcia, G.H.; Gowd, A.K.; Cabarcas, B.C.; Liu, J.N.; Meyer, J.R.; White, G.M.; Romeo, A.A.; Verma, N.N. Magnetic Resonance Imaging Findings of the Asymptomatic Elbow Predict Injuries and Surgery in Major League Baseball Pitchers. Orthop. J. Sports Med. 2019, 29, 2325967118818413. [Google Scholar] [CrossRef]
- Patel, H.; Lala, S.; Helfner, B.; Wong, T.T. Tennis overuse injuries in the upper extremity. Skeletal Radiol. 2021, 50, 629–644. [Google Scholar] [CrossRef]
- Rossy, W.H.; Oh, L.S. Pitcher’s elbow: Medial elbow pain in the overhead-throwing athlete. Curr. Rev. Musculoskelet. Med. 2016, 9, 207–214. [Google Scholar] [CrossRef]







| Mechanism | Anatomic Structures and Patterns of Injury |
|---|---|
| Medial tension overload | Medial epicondylar apophysitis Medial epicondylar avulsion injury Medial epicondylar bone marrow edema Ulnar collateral ligament thickness Ulnar collateral ligament (anterior bundle) injury and grade Heterotopic ossification related to prior UCL injury Ulnar neuropathy Flexor–pronator tendinopathy or injury Ulnar traction spur at the insertion of the UCL into the sublime tubercle |
| Lateral compressive forces | Panner’s disease (osteochondrosis of the humeral capitellum) Osteochondritis dissecans (fragmentation of the humeral capitellar articular surface) Osteochondral lesion Thickened radiocapitellar plica Subchondral sclerosis along the radial head Radiocapitellar osteoarthrosis and presence of joint bodies |
| Posteromedial shear forces | Olecranon apophysitis Olecranon stress reaction or fracture Subchondral sclerosis along the humeral trochlea and olecranon Humeroulnar chondral injury and/or joint bodies Humeral trochlear or olecranon bone marrow edema Humeroulnar osteophytes Fluid and/or synovitis in the posteromedial humeroulnar recess Scarring in the olecranon fat pad |
| Other | Lateral ligamentous injury Common extensor tendinopathy or injury Triceps tendinopathy or injury Biceps/brachialis tendinopathy or injury |
| Mechanism | Subgroup ≤16 Years (26 Subjects) | Subgroup 17–19 Years (25 Subjects) | Subgroup ≥20 Years (35 Subjects) | Total (86 Subjects) |
|---|---|---|---|---|
| Medial tension overload | ||||
| Medial epicondylar apophysitis | 6 (23%) | 0 (0%) | 0 (0%) | 6 (7%) |
| Medial epicondylar avulsion injury | 3 (12%) | 3 (12%) | 1 (3%) | 7 (8%) |
| Medial epicondylar bone marrow edema | 8 (31%) | 12 (48%) | 9 (26%) | 29 (34%) |
| Ulnar collateral ligament injury | 17 (65%) | 22 (88%) | 32 (91%) | 71 (83%) |
| Grade 1 (low grade sprain) | 11 (42%) | 10 (40%) | 11 (31%) | 32 (37%) |
| Grade 2 (partial tear) | 6 (23%) | 12 (48%) | 17 (49%) | 35 (41%) |
| Grade 3 (complete disruption) | 0 (0%) | 0 (0%) | 4 (11%) | 4 (5%) |
| Heterotopic ossification due to prior UCL injury | 0 (0%) | 1 (4%) | 0 (0%) | 1 (1%) |
| Ulnar neuropathy | 7 (27%) | 10 (40%) | 15 (43%) | 32 (37%) |
| Flexor–pronator tendinopathy or injury | 11 (42%) | 9 (36%) | 20 (57%) | 40 (47%) |
| Ulnar traction spur | 12 (46%) | 15 (60%) | 21 (60%) | 48 (56%) |
| Lateral compressive forces | ||||
| Panner’s disease | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Osteochondritis dissecans | 4 (15%) | 0 (0%) | 0 (0%) | 4 (5%) |
| Osteochondral lesion | 1 (4%) | 0 (0%) | 1 (3%) | 2 (2%) |
| Thickened radiocapitellar plica | 2 (8%) | 0 (0%) | 1 (3%) | 3 (3%) |
| Radiocapitellar osteoarthrosis, joint bodies | 5 (19%) | 1 (4%) | 1 (3%) | 7 (8%) |
| Posteromedial shear forces | ||||
| Olecranon apophysitis | 5 (19%) | 0 (0%) | 1 (3%) | 6 (7%) |
| Olecranon stress reaction or fracture | 3 (12%) | 5 (20%) | 1 (3%) | 9 (10%) |
| Humeroulnar chondral injury, joint bodies | 5 (19%) | 12 (48%) | 12 (34%) | 29 (34%) |
| Trochlear or olecranon subchondral bone marrow edema/reactive change | 9 (35%) | 11 (44%) | 7 (20%) | 27 (31%) |
| Humeroulnar osteophytes | 16 (62%) | 18 (72%) | 26 (74%) | 60 (70%) |
| Fluid and/or synovitis in the humeroulnar posteromedial recess | 6 (23%) | 12 (48%) | 12 (34%) | 30 (35%) |
| Scarring in the olecranon fat pad | 12 (46%) | 14 (56%) | 12 (34%) | 38 (44%) |
| Other | ||||
| Lateral ligamentous injury | 1 (4%) | 1 (4%) | 2 (6%) | 4 (5%) |
| Common extensor tendinopathy or injury | 4 (15%) | 4 (16%) | 11 (31%) | 19 (22%) |
| Triceps tendinopathy or injury | 3 (12%) | 6 (24%) | 17 (49%) | 26 (30%) |
| Biceps/brachialis tendinopathy or injury | 0 (0%) | 1 (4%) | 2 (6%) | 3 (3%) |
| Imaging Finding | Athletes (86 Total) | Control Subjects (23 Total) |
|---|---|---|
| Ulnar collateral ligament injury (any grade) | 71 (83%) | 0 (0%) |
| Humeroulnar osteophytes | 60 (70%) | 4 (17%) |
| Ulnar traction spur | 48 (56%) | 6 (26%) |
| Flexor–pronator tendinopathy or injury | 40 (47%) | 0 (0%) |
| Scarring in the olecranon fat pad | 38 (44%) | 2 (9%) |
| Ulnar neuropathy (total) | 32 (37%) | 4 (17%) |
| Symptomatic ulnar neuropathy | 9 (10%) | 4 (17%) |
| Anatomic Adaptation | Athletes | Control Subjects | p-Value |
|---|---|---|---|
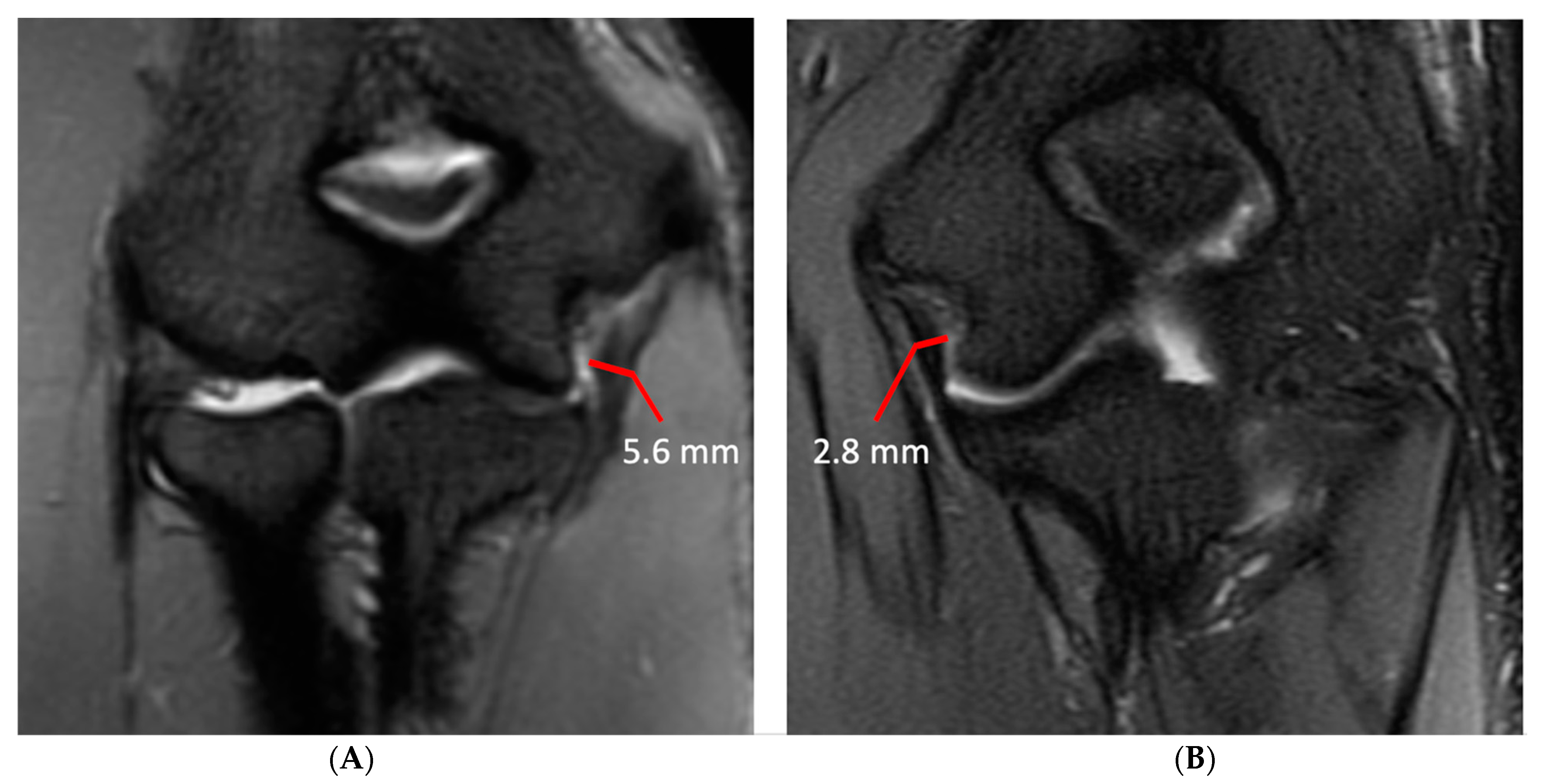
| Ulnar collateral ligament thickness (mm) | 5.1 ± 1.8 | 2.3 ± 0.8 | <0.001 |
| Subchondral sclerosis thickness radial head (mm) | 1.9 ± 0.8 | 1.0 ± 0.6 | <0.001 |
| Subchondral sclerosis humeral trochlea (mm) | 2.5 ± 1.0 | 1.3 ± 0.6 | <0.001 |
| Subchondral sclerosis olecranon process (mm) | 2.6 ± 1.1 | 1.3 ± 0.7 | <0.001 |
| Anatomic Adaptation | Subgroup ≤16 Years | Subgroup 17–19 Years | Subgroup ≥20 Years | p-Value ** |
|---|---|---|---|---|
| Ulnar collateral ligament thickness (mm) | 4.4 ± 1.9 | 5.2 ± 1.7 * | 5.7 ± 1.7 * | <0.001 |
| Subchondral sclerosis thickness in radial head (mm) | 1.8 ± 0.8 | 1.8 ± 0.7 | 2.0 ± 0.7 | 0.09 |
| Subchondral sclerosis in humeral trochlea (mm) | 2.2 ± 1.0 | 2.6 ± 1.1 | 2.9 ± 1.1 | 0.27 |
| Subchondral sclerosis in olecranon process (mm) | 2.3 ± 1.1 | 2.6 ± 0.9 * | 2.5 ± 0.9 * | 0.002 |
| Concordance Correlation Coefficient | p-Value | Bias | 95% Limits of Agreement | |
|---|---|---|---|---|
| Ulnar collateral ligament thickness (mm) | 0.97 | 0.84 | 0.06 | ±0.98 |
| Subchondral sclerosis thickness in radial head (mm) | 0.88 | 0.86 | 0.02 | ±0.77 |
| Subchondral sclerosis in humeral trochlea (mm) | 0.91 | 0.94 | 0.01 | ±0.94 |
| Subchondral sclerosis in olecranon process (mm) | 0.93 | 0.90 | −0.02 | ±0.75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stevens, K.J.; Chaudhari, A.S.; Kuhn, K.J. Differences in Anatomic Adaptation and Injury Patterns Related to Valgus Extension Overload in Overhead Throwing Athletes. Diagnostics 2024, 14, 217. https://doi.org/10.3390/diagnostics14020217
Stevens KJ, Chaudhari AS, Kuhn KJ. Differences in Anatomic Adaptation and Injury Patterns Related to Valgus Extension Overload in Overhead Throwing Athletes. Diagnostics. 2024; 14(2):217. https://doi.org/10.3390/diagnostics14020217
Chicago/Turabian StyleStevens, Kathryn J., Akshay S. Chaudhari, and Karin J. Kuhn. 2024. "Differences in Anatomic Adaptation and Injury Patterns Related to Valgus Extension Overload in Overhead Throwing Athletes" Diagnostics 14, no. 2: 217. https://doi.org/10.3390/diagnostics14020217





