Analysis of the Sagittal Root Position of the Maxillary and Mandibular Anterior Teeth in the Alveolar Bone Using Cone-Beam Computed Tomography
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Calculation
2.3. Study Sample
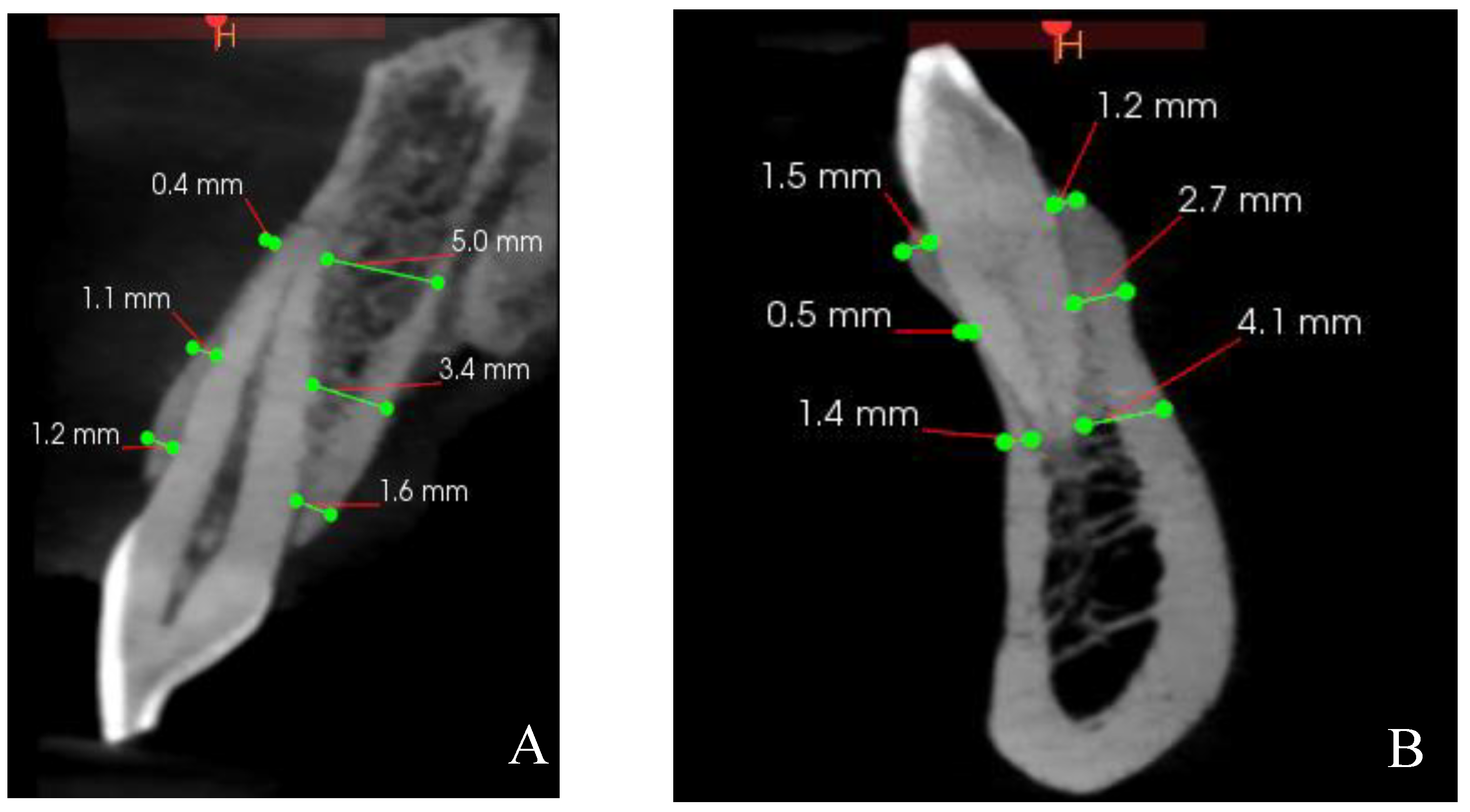
2.4. CBCT Measurements
2.5. Reliability Test
2.6. Statistical Analysis
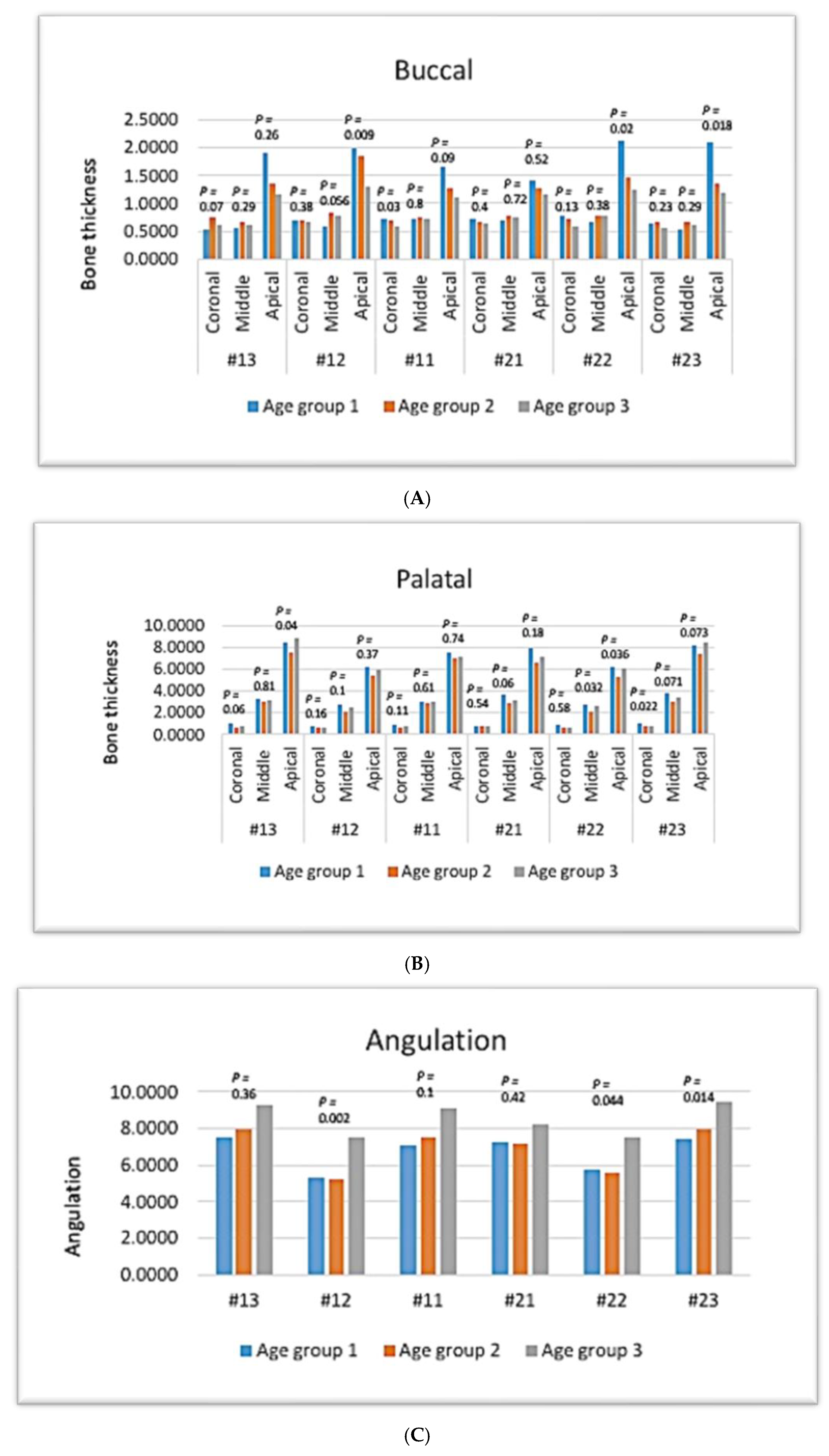
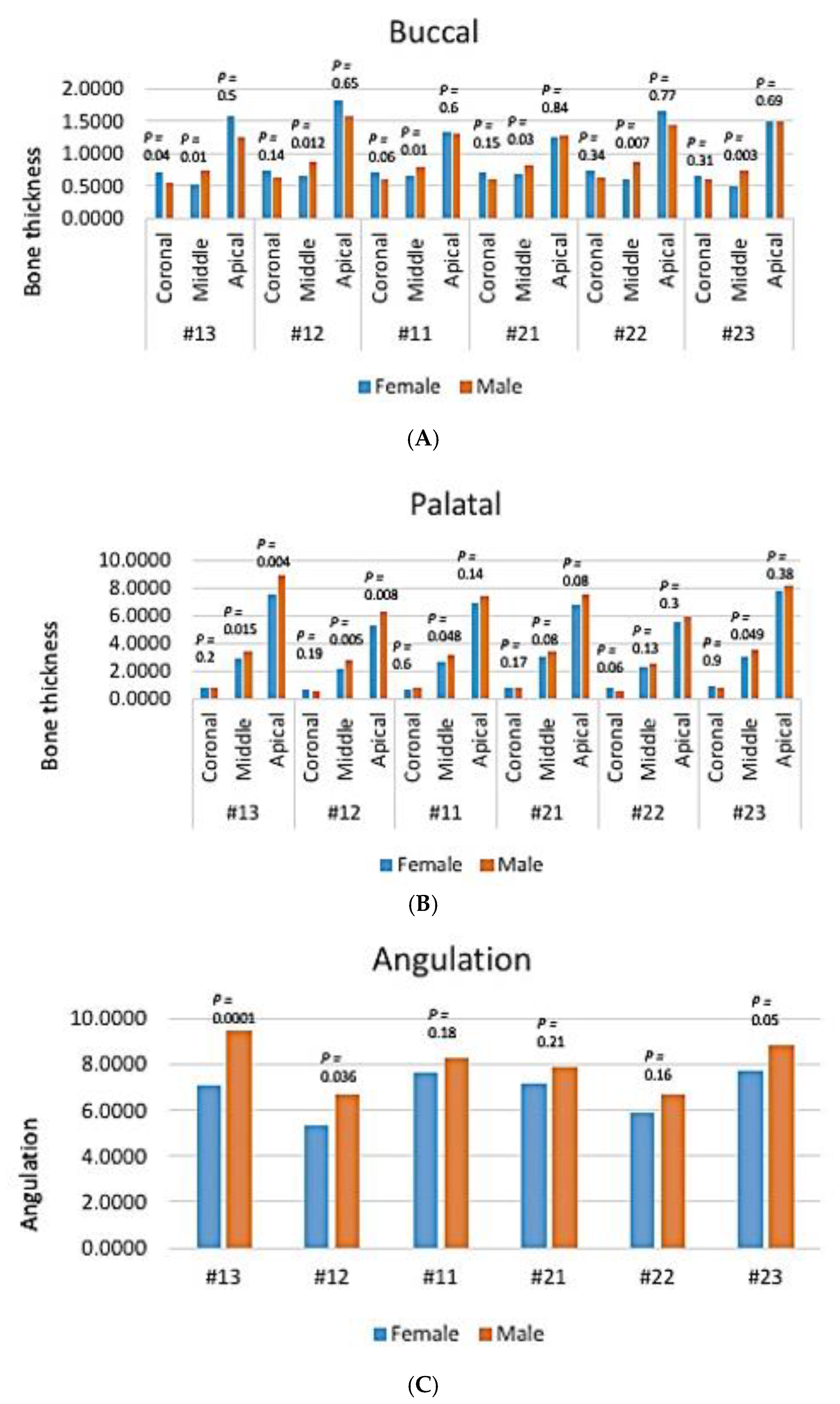
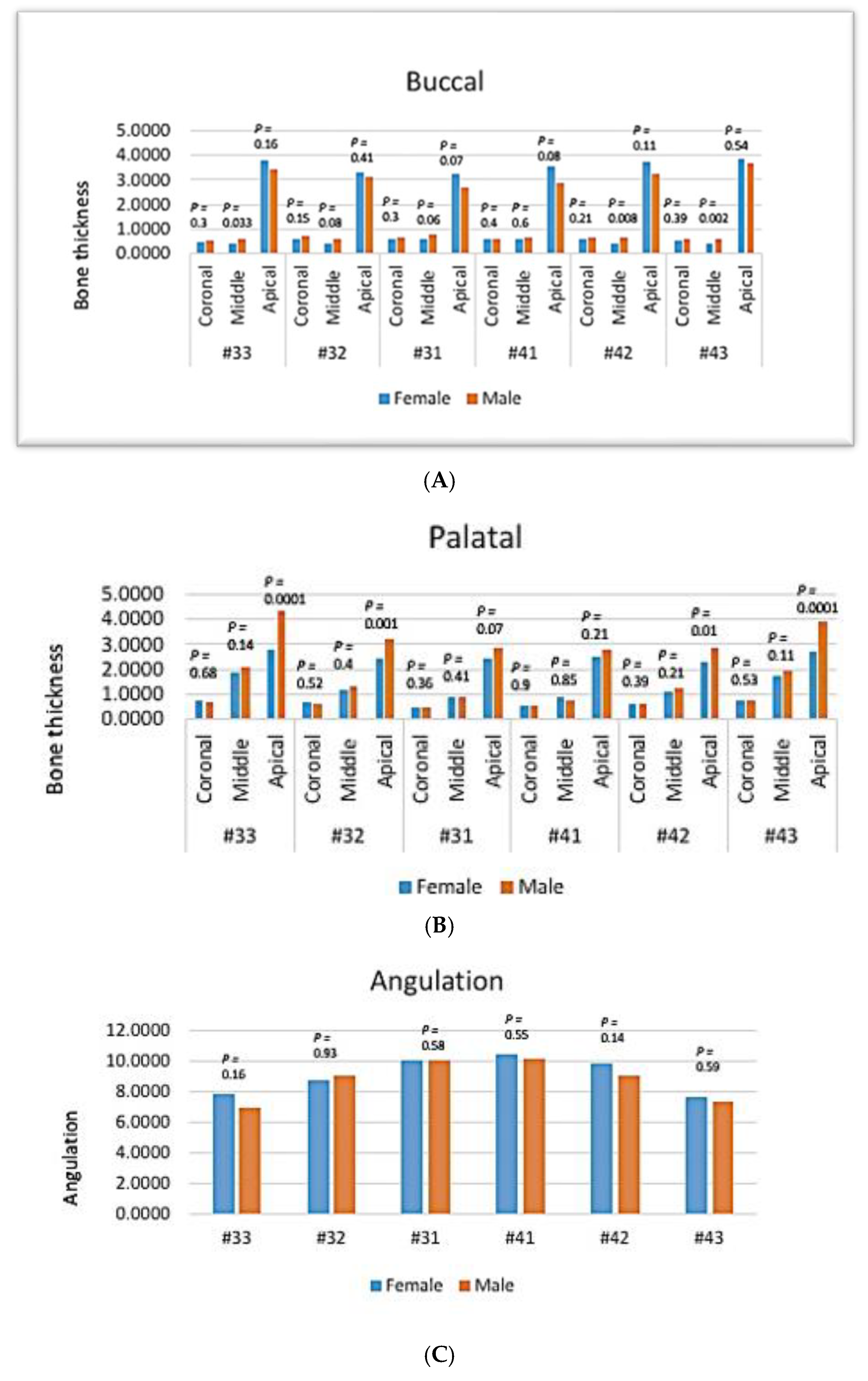
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Chan, H.L.; Garaicoa-Pazmino, C.; Suarez, F.; Monje, A.; Benavides, E.; Oh, T.J.; Wang, H.L. Incidence of implant buccal plate fenestration in the esthetic zone: A cone beam computed tomography study. Int. J. Oral Maxillofac. Implant. 2014, 29, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Lau, S.L.; Chow, J.; Li, W.; Chow, L.K. Classification of maxillary central incisors-implications for immediate implant in the esthetic zone. J. Oral Maxillofac. Surg. 2011, 69, 142–153. [Google Scholar] [CrossRef]
- Wang, H.M.; Shen, J.W.; Yu, M.F.; Chen, X.Y.; Jiang, Q.H.; He, F.M. Analysis of facial bone wall dimensions and sagittal root position in the maxillary esthetic zone: A retrospective study using cone beam computed tomography. Int. J. Oral Maxillofac. Implant. 2014, 29, 1123. [Google Scholar] [CrossRef] [PubMed]
- Srebrzyńska-Witek, A.; Koszowski, R.; Różyło-Kalinowska, I. Relationship between anterior mandibular bone thickness and the angulation of incisors and canines-a CBCT study. Clin. Oral Investig. 2018, 22, 1567–1578. [Google Scholar] [CrossRef] [PubMed]
- Braut, V.; Bornstein, M.M.; Belser, U.; Buser, D. Thickness of the anterior maxillary facial bone wall-a retrospective radiographic study using cone beam computed tomography. Int. J. Periodontics Restor. Dent. 2011, 31, 125. [Google Scholar]
- Bulyalert, A.; Pimkhaokham, A. A novel classification of anterior alveolar arch forms and alveolar bone thickness: A cone-beam computed tomography study. Imaging Sci. Dent. 2018, 48, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Januário, A.L.; Duarte, W.R.; Barriviera, M.; Mesti, J.C.; Araújo, M.G.; Lindhe, J. Dimension of the facial bone wall in the anterior maxilla: A cone-beam computed tomography study. Clin. Oral Implant. Res. 2011, 22, 1168–1171. [Google Scholar] [CrossRef]
- Zekry, A.; Wang, R.; Chau, A.C.; Lang, N.P. Facial alveolar bone wall width—A cone-beam computed tomography study in Asians. Clin. Oral Implant. Res. 2014, 25, 194–206. [Google Scholar] [CrossRef]
- Zhang, W.; Skrypczak, A.; Weltman, R. Anterior maxilla alveolar ridge dimension and morphology measurement by cone beam computerized tomography (CBCT) for immediate implant treatment planning. BMC Oral Health 2015, 15, 65–73. [Google Scholar] [CrossRef]
- Araújo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Medikeri, R.S.; Sinha, K.A.; Chandak, S.; Ghogare, P. Evaluation of sagittal root positions and bone perforation in anterior teeth using cone beam computed tomography: An observational study. J. Oral Implantol. 2021, 47, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.; Read-Fuller, A. Cone beam computed tomography in oral and maxillofacial surgery: An evidence-based review. Dent. J. 2019, 7, 52. [Google Scholar] [CrossRef] [PubMed]
- López-Jarana, P.; Díaz-Castro, C.M.; Falcão, A.; Falcão, C.; Ríos-Santos, J.V.; Herrero-Climent, M. Thickness of the buccal bone wall and root angulation in the maxilla and mandible: An approach to cone beam computed tomography. BMC Oral Health 2018, 18, 194–203. [Google Scholar] [CrossRef]
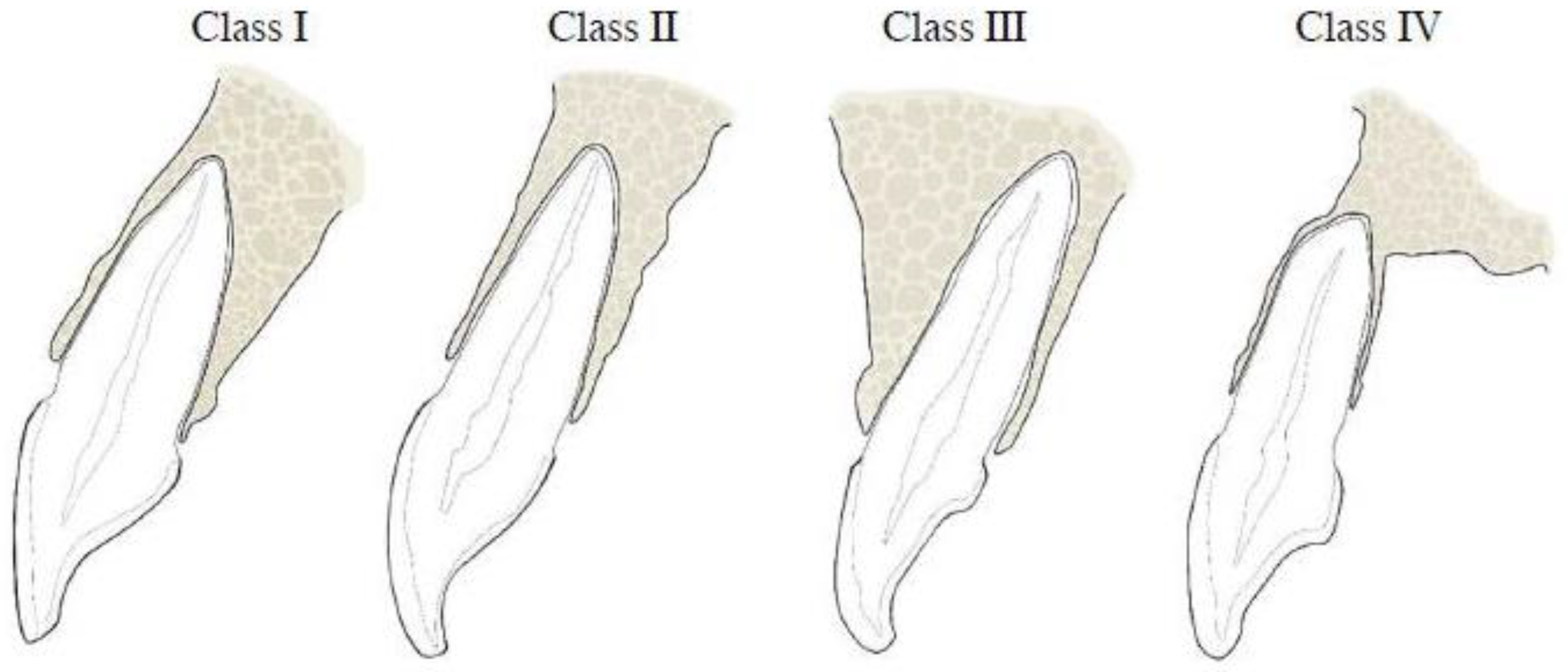
- Kan, J.Y.; Roe, P.; Rungcharassaeng, K.; Patel, R.D.; Waki, T.; Lozada, J.L.; Zimmerman, G. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: A cone beam computed tomography study. Int. J. Oral Maxillofac. Implant. 2011, 26, 873–876. [Google Scholar]
- Zhang, L.Q.; Zhao, Y.N.; Zhang, Y.Q.; Zhang, Y.; Liu, D.G. Morphologic analysis of alveolar bone in maxillary and mandibular incisors on sagittal views. Surg. Radiol. Anat. 2021, 43, 1009–1018. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Xie, C.; Yu, H.; Zhang, Z.; Zheng, J.; Xu, S. Evaluation of factors affecting alveolar ridge height and facial bone thickness in Chinese maxillary central incisors by cone beam CT. J. Dent. Sci. 2021, 16, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.C.; Kang, D.U.; Baek, H.; Hong, J.Y.; Shin, S.Y.; Chung, J.H.; Herr, Y.; Shin, S.I. Cone-beam computed tomographic analysis of the alveolar ridge profile and virtual implant placement for the anterior maxilla. J. Periodontal. Implant Sci. 2019, 49, 299–309. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Gluckman, H.; Pontes, C.C.; Du Toit, J. Radial plane tooth position and bone wall dimensions in the anterior maxilla: A CBCT classification for immediate implant placement. J. Prosthet. Dent. 2018, 120, 50–56. [Google Scholar] [CrossRef]
- Lang, N.P.; Pun, L.; Lau, K.Y.; Li, K.Y.; Wong, M.C. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin. Oral Implant. Res. 2012, 23, 39–66. [Google Scholar] [CrossRef]
- Ikbal, M.; Shen, Y.W.; Ruslin, M.; Fuh, L.J.; Hsu, J.T. Assessment of sagittal root position, alveolar bone concavity, and labial bone perforation in the mandibular anterior tooth region for immediate implant placement. J. Dent. Sci. 2023, 18, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.H.; Cho, B.H.; Hwang, J.J. Analysis of the root position of the maxillary incisors in the alveolar bone using cone-beam computed tomography. Imaging Sci. Dent. 2017, 47, 181–187. [Google Scholar] [CrossRef]
- Rodrigues, D.M.; Petersen, R.L.; Montez, C.; de Moraes, J.R.; Ferreira, V.; Barboza, E.P. The relationship between tomographic sagittal root position of maxillary anterior teeth and the bone housing. J. Prosthet. Dent. 2023, 130, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Kong, H.J. A study on sagittal root position of maxillary anterior teeth in Korean. J. Dent. Rehabil. Appl. Sci. 2020, 36, 88–94. [Google Scholar] [CrossRef]
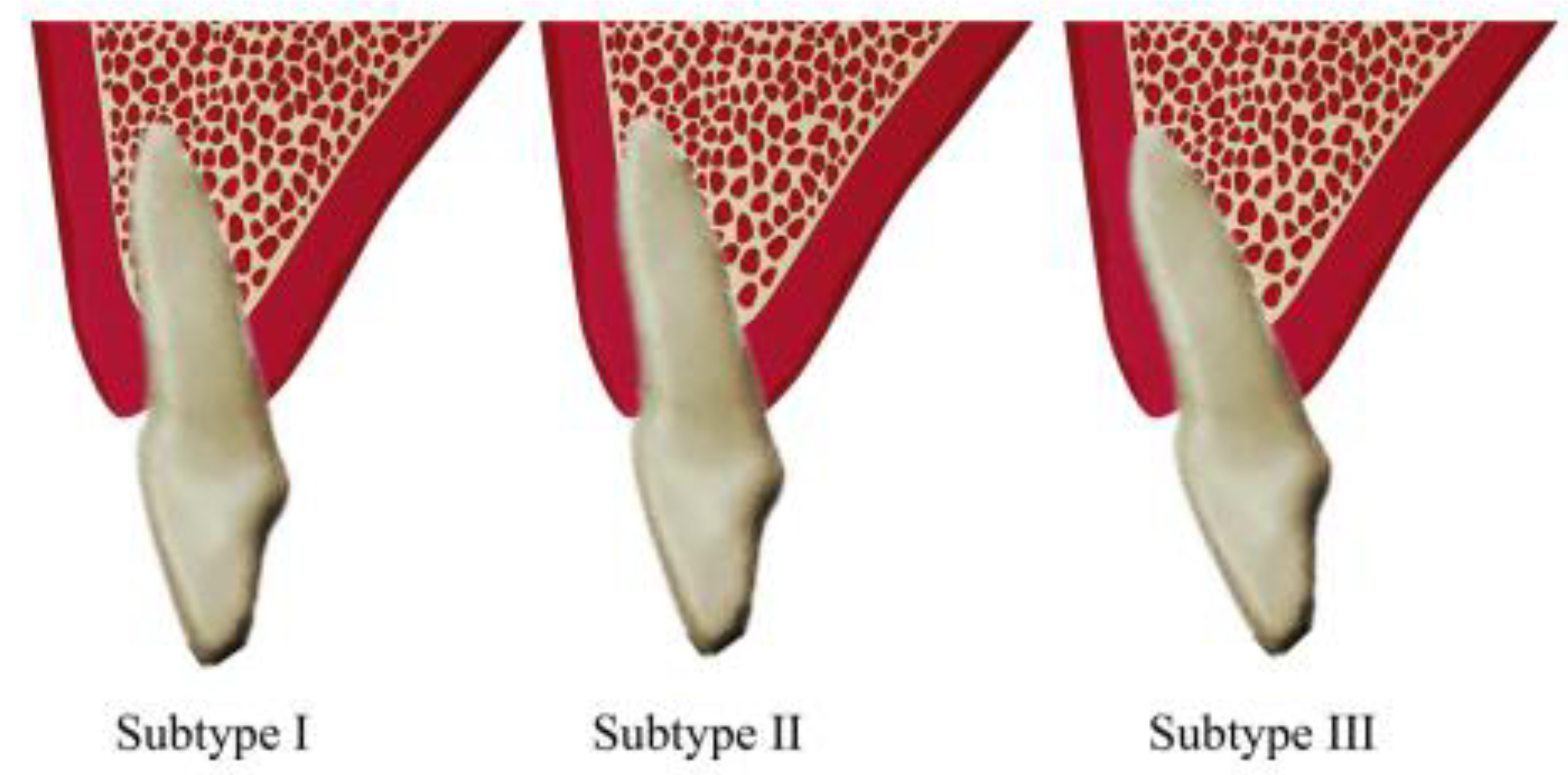
- Affendi, N.H.K.; Babiker, J.; Mohd Yusof, M.Y.P. CBCT assessment of alveolar bone wall morphology and its correlation with tooth angulation in the anterior mandible: A new classification for immediate implant placement. J. Periodontal. Implant Sci. 2023, 53, 453–466. [Google Scholar] [CrossRef]
- Xu, D.; Wang, Z.; Sun, L.; Lin, Z.; Wan, L.; Li, Y.; Lin, X.; Peng, W.; Zhang, Z.; Gao, Y. Classification of the root position of the maxillary central incisors and its clinical significance in immediate implant placement. Implant Dent. 2016, 25, 520–524. [Google Scholar] [CrossRef] [PubMed]
- Moghaddas, O.; Behravan, I. A new classification of the sagittal root positioning of the mandibular anterior teeth in relation to their anterior buccal bone using cone-beam computed tomography (CBCT). J. Adv. Periodontol. Implant Dent. 2020, 17, 65–71. [Google Scholar] [CrossRef]
- Al-Khawaja, N.F.K.; Nahidh, M.; Abdulsaheb, R.J. Assessment of maxillary incisors’ angulation and position in different types of malocclusions using Cone-Beam Computed Tomography. Contemp. Clin. Dent. 2021, 12, 401–407. [Google Scholar] [CrossRef]
- Kumar, A.; Medikeri, R.S.; Sutar, A.A.; Waingade, M.; Lahane, P.V. Evaluation of anterior tooth-ridge angulation, root position and labial bone perforation using dental cone-beam computed tomography: An observational study. J. Indian Soc. Periodontol. 2023, 27, 57–62. [Google Scholar] [CrossRef]
- Shafizadeh, M.; Tehranchi, A.; Shirvani, A.; Motamedian, S.R. Alveolar bone thickness overlying healthy maxillary and mandibular teeth: A systematic review and meta-analysis. Int. Orthod. 2021, 19, 389–405. [Google Scholar] [CrossRef]
- Tsigarida, A.; Toscano, J.; de Brito Bezerra, B.; Geminiani, A.; Barmak, A.B.; Caton, J.; Papaspyridakos, P.; Chochlidakis, K. Buccal bone thickness of maxillary anterior teeth: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47, 1326–1343. [Google Scholar] [CrossRef]
- Gakonyo, J.; Mohamedali, A.J.; Mungure, E.K. Cone beam computed tomography assessment of the buccal bone thickness in anterior maxillary teeth: Relevance to Immediate Implant Placement. Int. J. Oral Maxillofac. Implant. 2018, 33, 880–887. [Google Scholar] [CrossRef] [PubMed]
- Somvasoontra, S.; Tharanon, W.; Serichetaphongse, P.; Pimkhaokham, A. Associations among the anterior maxillary dental arch form, alveolar bone thickness, and the sagittal root position of the maxillary central incisors in relation to immediate implant placement: A cone-beam computed tomography analysis. Imaging Sci. Dent. 2022, 52, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Almahdi, R.A.; Alasqah, M. Assessment of buccal bone thickness in the maxillary and mandibular canine using cone-beam computed tomography. Int. J. Med. Dent. 2021, 25, 331–338. [Google Scholar]
- Nowzari, H.; Molayem, S.; Chiu, C.H.; Rich, S.K. Cone beam computed tomographic measurement of maxillary central incisors to determine prevalence of facial alveolar bone width ≥2 mm. Clin. Implant Dent. Relat. Res. 2012, 14, 595–602. [Google Scholar] [CrossRef]
- Aljabr, A.A.; Almas, K.; Aljofi, F.E.; Aljabr, A.A.; Alzaben, B.; Alqanas, S. A CBCT study of labial alveolar bone thickness in the maxillary anterior region in a Teaching Hospital Population in the Eastern Province of Saudi Arabia. Biomedicines 2023, 11, 1571. [Google Scholar] [CrossRef]
- Ozdemir, F.; Tozlu, M.; Germec-Cakan, D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 190–196. [Google Scholar] [CrossRef]
- Ohiomoba, H.; Sonis, A.; Yansane, A.; Friedland, B. Quantitative evaluation of maxillary alveolar cortical bone thickness and density using computed tomography imaging. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 82–91. [Google Scholar] [CrossRef]




| Sagittal Root Position | Frequencies in Percentages | ||||||
|---|---|---|---|---|---|---|---|
| Tooth | 13# | 12# | 11# | 21# | 22# | 23# | |
| Classification | Class I | 63% | 69% | 90% | 85% | 76% | 84% |
| Class II | 35% | 29% | 10% | 15% | 22% | 14% | |
| Class III | 0% | 1% | 0% | 0% | 0% | 0% | |
| Class IV | 2% | 1% | 0% | 0% | 2% | 2% | |
| Total | 100% | 100% | 100% | 100% | 100% | 100% | |
| Sub-classification | Subtype I | 34% | 14% | 13% | 8% | 8% | 3% |
| Subtype II | 5% | 12% | 7% | 7% | 13% | 10% | |
| Subtype III | 61% | 74% | 80% | 85% | 79% | 87% | |
| Total | 100% | 100% | 100% | 100% | 100% | 100% | |
| Sagittal Root Position | Frequencies in Percentages | ||||||
|---|---|---|---|---|---|---|---|
| Tooth | 33# | 32# | 31# | 41# | 42# | 43# | |
| Classification | Class I | 7% | 5% | 2% | 3% | 1% | 10% |
| Class II | 10% | 7% | 3% | 8% | 5% | 13% | |
| Class III | 7% | 4% | 1% | 2% | 2% | 3% | |
| Class IV | 76% | 84% | 94% | 87% | 92% | 74% | |
| Total | 100% | 100% | 100% | 100% | 100% | 100% | |
| Sub-classification | Class I | 26% | 14% | 31% | 37% | 37% | 26% |
| Class II | 54% | 74% | 62% | 47% | 56% | 57% | |
| Class III | 20% | 12% | 7% | 16% | 7% | 17% | |
| Total | 100% | 100% | 100% | 100% | 100% | 100% | |
| Tooth Type | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #13 | #12 | #11 | #21 | #22 | #23 | #33 | #32 | #31 | #41 | #42 | #43 | |
| Mean | 8.2 | 5.9 | 7.9 | 7.5 | 6.2 | 8.2 | 7.4 | 8.9 | 10.0 | 10.3 | 9.4 | 7.5 |
| Median | 8.0 | 6.0 | 8.0 | 8.0 | 6.0 | 8.0 | 8.0 | 9.0 | 10.0 | 10.0 | 10.0 | 8.0 |
| St. Dev. | 2.86 | 3.1 | 3.7 | 3.6 | 3.3 | 2.9 | 2.8 | 3.3 | 4.03 | 3.6 | 2.9 | 2.6 |
| Range | 15.0 | 18.0 | 23.0 | 21.0 | 20.0 | 17.0 | 17.0 | 17.1 | 19.5 | 17.0 | 14.0 | 12.0 |
| Tooth Type | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #13 | #12 | #11 | #21 | #22 | #23 | #33 | #32 | #31 | #41 | #42 | #43 | ||
| Coronal | Mean | 0.64 | 0.69 | 0.66 | 0.66 | 0.69 | 0.63 | 0.50 | 0.63 | 0.61 | 0.58 | 0.59 | 0.55 |
| Median | 0.60 | 0.60 | 0.70 | 0.70 | 0.65 | 0.60 | 0.50 | 0.60 | 0.60 | 0.60 | 0.60 | 0.60 | |
| St. Dev. | 0.45 | 0.35 | 0.29 | 0.29 | 0.33 | 0.31 | 0.31 | 0.40 | 0.34 | 0.37 | 0.33 | 0.30 | |
| Range | 2.90 | 1.70 | 1.60 | 1.70 | 1.60 | 1.50 | 1.60 | 2.30 | 1.50 | 1.60 | 1.30 | 1.20 | |
| Middle | Mean | 0.63 | 0.75 | 0.73 | 0.74 | 0.74 | 0.61 | 0.47 | 0.50 | 0.67 | 0.60 | 0.52 | 0.49 |
| Median | 0.50 | 0.60 | 0.70 | 0.70 | 0.60 | 0.55 | 0.30 | 0.40 | 0.50 | 0.50 | 0.40 | 0.40 | |
| St. Dev. | 0.46 | 0.62 | 0.33 | 0.35 | 0.57 | 0.39 | 0.45 | 0.43 | 0.52 | 0.45 | 0.41 | 0.37 | |
| Range | 2.10 | 3.60 | 1.60 | 2.00 | 2.80 | 1.90 | 2.60 | 2.30 | 3.0 | 2.10 | 1.90 | 2.00 | |
| Apical | Mean | 1.43 | 1.71 | 1.31 | 1.27 | 1.55 | 1.49 | 3.61 | 3.22 | 2.98 | 3.22 | 3.48 | 3.76 |
| Median | 1.25 | 1.50 | 1.15 | 1.05 | 1.30 | 1.30 | 3.75 | 3.20 | 3.05 | 3.00 | 3.40 | 3.90 | |
| St. Dev. | 1.15 | 1.22 | 0.86 | 0.80 | 1.10 | 1.17 | 1.54 | 1.34 | 1.54 | 1.57 | 1.38 | 1.33 | |
| Range | 7.20 | 8.40 | 5.40 | 4.40 | 8.40 | 6.80 | 7.30 | 7.80 | 9.90 | 9.40 | 7.70 | 8.20 | |
| Tooth Type | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #13 | #12 | #11 | #21 | #22 | #23 | #33 | #32 | #31 | #41 | #42 | #43 | ||
| Coronal | Mean | 0.78 | 0.66 | 0.74 | 0.79 | 0.68 | 0.85 | 0.70 | 0.65 | 0.47 | 0.51 | 0.63 | 0.74 |
| Median | 0.70 | 0.60 | 0.70 | 0.75 | 0.60 | 0.80 | 0.70 | 0.60 | 0.40 | 0.45 | 0.60 | 0.70 | |
| St. Dev. | 0.51 | 0.40 | 0.36 | 0.37 | 0.53 | 0.66 | 0.33 | 0.37 | 0.27 | 0.32 | 0.37 | 0.33 | |
| Range | 3.30 | 3.20 | 1.90 | 2.10 | 4.80 | 5.90 | 2.40 | 2.90 | 1.10 | 1.90 | 3.10 | 1.90 | |
| Middle | Mean | 3.14 | 2.42 | 2.95 | 3.18 | 2.44 | 3.33 | 1.99 | 1.21 | 0.91 | 0.83 | 1.14 | 1.85 |
| Median | 3.20 | 2.30 | 3.00 | 3.10 | 2.35 | 3.20 | 1.90 | 1.10 | 0.70 | 0.60 | 1.10 | 1.70 | |
| St. Dev. | 1.12 | 1.09 | 1.18 | 1.18 | 1.10 | 1.29 | 0.98 | 0.72 | 0.68 | 0.58 | 0.64 | 1.09 | |
| Range | 6.80 | 5.00 | 6.20 | 5.50 | 6.50 | 7.0 | 4.50 | 3.0 | 4.60 | 2.60 | 3.10 | 7.30 | |
| Apical | Mean | 8.20 | 5.84 | 7.16 | 7.15 | 5.77 | 7.95 | 3.51 | 2.79 | 2.64 | 2.62 | 2.54 | 3.30 |
| Median | 8.25 | 5.75 | 7.0 | 6.85 | 5.50 | 8.0 | 3.30 | 2.75 | 2.70 | 2.50 | 2.45 | 3.30 | |
| St. Dev. | 2.48 | 1.96 | 2.16 | 2.24 | 1.86 | 2.23 | 1.84 | 1.19 | 1.26 | 1.12 | 1.05 | 1.41 | |
| Range | 12.7 | 9.80 | 10.2 | 12.5 | 8.0 | 10.0 | 9.40 | 6.10 | 8.30 | 5.30 | 5.70 | 6.80 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdul, R.J.; Abdulateef, D.S.; Fattah, A.O.; Talabani, R.M. Analysis of the Sagittal Root Position of the Maxillary and Mandibular Anterior Teeth in the Alveolar Bone Using Cone-Beam Computed Tomography. Diagnostics 2024, 14, 2756. https://doi.org/10.3390/diagnostics14232756
Abdul RJ, Abdulateef DS, Fattah AO, Talabani RM. Analysis of the Sagittal Root Position of the Maxillary and Mandibular Anterior Teeth in the Alveolar Bone Using Cone-Beam Computed Tomography. Diagnostics. 2024; 14(23):2756. https://doi.org/10.3390/diagnostics14232756
Chicago/Turabian StyleAbdul, Rawa Jamal, Darwn Saeed Abdulateef, Ara Omer Fattah, and Ranjdar Mahmood Talabani. 2024. "Analysis of the Sagittal Root Position of the Maxillary and Mandibular Anterior Teeth in the Alveolar Bone Using Cone-Beam Computed Tomography" Diagnostics 14, no. 23: 2756. https://doi.org/10.3390/diagnostics14232756
APA StyleAbdul, R. J., Abdulateef, D. S., Fattah, A. O., & Talabani, R. M. (2024). Analysis of the Sagittal Root Position of the Maxillary and Mandibular Anterior Teeth in the Alveolar Bone Using Cone-Beam Computed Tomography. Diagnostics, 14(23), 2756. https://doi.org/10.3390/diagnostics14232756





