Initial Imaging of Pregnant Patients in the Trauma Bay—Discussion and Review of Presentations at a Level-1 Trauma Centre
Abstract
1. Introduction
2. Radiation Dose Considerations
3. Imaging Modalities for Initial Assessment of the Pregnant Trauma Patient
3.1. Radiography
3.2. Computed Tomography (CT)
3.3. Ultrasound
3.4. Magnetic Resonance Imaging (MRI)
3.5. Fluoroscopy
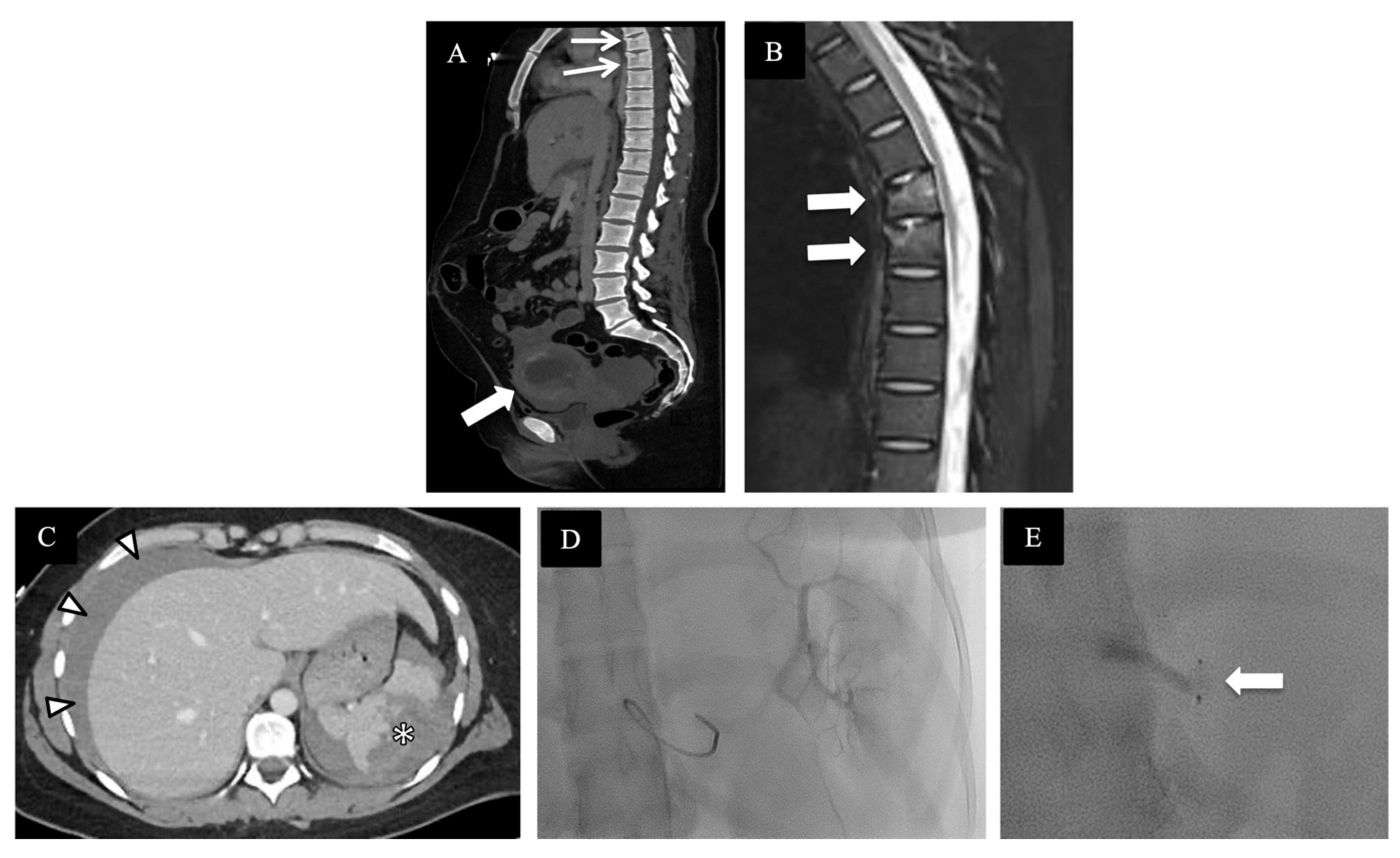
4. Review of Local Presentations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jain, V.; Chari, R.; Maslovitz, S.; Farine, D.; Bujold, E.; Gagnon, R.; Basso, M.; Bos, H.; Brown, R.; Cooper, S.; et al. Guidelines for the Management of a Pregnant Trauma Patient. J. Obs. Gynaecol. Can. 2015, 37, 553–574. [Google Scholar] [CrossRef] [PubMed]
- Mattox, K.L.; Goetz, L. Trauma in pregnanty. Crit. Care Med. 2005, 33, S385–S389. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, N.A.; Kucirka, L.M.; Smith, R.N.; Oxford, C.M. Pregnant trauma victims experience nearly 2-fold higher mortality compared to their nonpregnant counterparts. Am. J. Obstet. Gynecol. 2017, 217, 590.e1–590.e9. [Google Scholar] [CrossRef] [PubMed]
- Tenami, S.; Tankel, J.; Schwarz, A.D.; Ornoy, A.; Goldberg, S.; Grisaru-Granovsky, S.; Dror, Y.F.; Merin, O. The impact of minor trauma during pregnancy on maternal and neonatal outcomes: A tertiary centre experience. Surg. Pract. Sci. 2023, 13, 100160. [Google Scholar] [CrossRef]
- Baker, S.P.; o’Neill, B.; Haddon, W., Jr.; Long, W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 1974, 14, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Bochicchio, G.V.; Napolitano, L.M.; Haan, J.; Champion, H.; Scalea, T. Incidental pregnancy in trauma patients. J. Am. Coll. Surg. 2001, 192, 566–569. [Google Scholar] [CrossRef]
- Goo, H.W. CT Radiation Dose Optimization and Estimation: An Update for Radiologists. Korean J. Radiol. 2012, 13, 1–11. [Google Scholar] [CrossRef]
- Kalra, M.K.; Maher, M.M.; Toth, T.L.; Hamberg, L.M.; Blake, M.A.; Shepard, J.A.; Saini, S. Strategies for CT radiation dose optimization. Radiology 2004, 230, 619–628. [Google Scholar] [CrossRef]
- Hiles, P.; Gilligan, P.; Damilakis, J.; Briers, E.; Candela-Juan, C.; Faj, D.; Foley, S.; Frija, G.; Granata, C.; de las Heras Gala, H.; et al. European consensus on patient contact shielding. Insights Imaging 2021, 12, 194. [Google Scholar] [CrossRef]
- Canadian Association of Radiologists Position Statement. Discontinuing the Use of Gonadal and Fetal Shielding for Patients. Available online: https://car.ca/wp-content/uploads/2021/05/210518-CAR-Position-Statement-Gonadal-Shielding-e.pdf (accessed on 26 November 2023).
- Nguyen, C.P.; Goodman, L.H. Fetal risk in diagnostic radiology. Semin. Ultrasound CT MR 2012, 33, 4–10. [Google Scholar] [CrossRef]
- American College of Radiology and the Society for Pediatric Radiology. ACR-SPR Practice Guideline for Imaging Pregnant or Potentially Pregnant Adolescents and Women with Ionizing Radiation. Available online: https://www.acr.org/-/media/acr/files/practice-parameters/pregnant-pts.pdf (accessed on 16 January 2013).
- American College of Obstetrics and Gynecology Committee on Obstetric Practice. ACOG committee opinion: Guidelines for diagnostic imaging during pregnancy. Obstet. Gynecol. 2004, 104, 647–651. [Google Scholar] [CrossRef]
- American College of Radiology. ACR Manual on Contrast Media. Available online: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf (accessed on 11 October 2023).
- National Council on Radiation Protection and Measurements. Medical Radiation Exposure of Pregnant and Potentially Pregnant Women; Report no. 54; National Council on Radiation Protection and Measurements: Bethesda, MD, USA, 1977. [Google Scholar]
- McCollough, C.H.; Schueler, B.A.; Atwell, T.D. Radiation exposure and pregnancy: When should we be concerned? RadioGraphics 2007, 27, 909–917. [Google Scholar] [CrossRef] [PubMed]
- Angel, E.; Wellnitz, C.V.; Goodsitt, M.M.; Yaghmai, N.; DeMarco, J.J.; Cagnon, C.H.; Sayre, J.W.; Cody, D.D.; Stevens, D.M.; Primak, A.N.; et al. Radiation dose to the fetus for pregnant patients undergoing multidetector CT imaging: Monte Carlo simulations estimating fetal dose for a range of gestational age and patient size. Radiology 2008, 249, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, E.; DeBenedectis, C.; North, D.; Spencer, P.K.; Mayo-Smith, W.W. Utilization of imaging in pregnant patients: 10-year review of 5270 examinations in 3285 patients—1997–2006. Radiology 2009, 251, 517–624. [Google Scholar] [CrossRef] [PubMed]
- Juliusson, G.; Thorvaldsdottir, B.; Kristjansson, J.M.; Hannesson, P. Diagnostic imaging trends in the emergency department: An extensive single-center experience. Acta Radiol. Open 2019, 8, 2058460119860404. [Google Scholar] [CrossRef] [PubMed]
- Hong, A.S.; Levin, D.; Parker, L.; Rao, V.M.; Ross-Degnan, D.; Wharam, J.F. Trends in Diagnostic imaging utilization among medicare and commercially insured adults from 2003 through 2016. Radiology 2019, 294, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Bourjeily, G.; Chalhoub, M.; Phornphutkul, C.; Alleyne, T.C.; Woodfield, C.A.; Chen, K.K. Neonatal thyroid function: Effect of a single exposure to iodinated contrast medium in utero. Radiology 2010, 256, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Atwell, T.D.; Lteif, A.N.; Brown, D.L.; McCann, M.; Townsend, J.E.; LeRoy, A.J. Neonatal thyroid function after administration of IV iodinated contrast agent o 21 pregnant patients. Am. J. Roentgenol. 2008, 191, 268–271. [Google Scholar] [CrossRef] [PubMed]
- Kochi, M.H.; Kaloudis, E.V.; Ahmed, W.; Moore, W.H. Effect of in utero exposure of iodinated intravenous contrast on neonatal thyroid function. J. Comput. Assist. Tomogr. 2012, 36, 165–169. [Google Scholar] [CrossRef]
- Iball, G.R.; Kennedy, E.V.; Brettle, D.S. Modelling the effect of lead and other materials for shielding of the fetus in CT pulmonary angiography. Br. J. Radiol. 2008, 81, 499–503. [Google Scholar] [CrossRef]
- Pearl, W.S.; Todd, K.H. Ultrasonography for the initial evaluation of blunt abdominal trauma: A review of prospective trials. Ann. Emerg. Med. 1996, 27, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.S. Ultrasound in abdominal trauma. Emerg. Med. Clin. N. Am. 2004, 22, 581–599. [Google Scholar] [CrossRef] [PubMed]
- Branney, S.W.; Wolfe, R.E.; Moore, E.E.; Albert, N.P.; Heinig, M.; Mestek, M.; Eule, J. Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid. J. Trauma 1995, 39, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Shackford, S.R.; Rogers, F.B.; Osler, T.M.; Trabulsy, M.E.; Clauss, D.W.; Vane, D.W. Focused abdominal sonogram for trauma: The learning curve of non-radiologist clinicians in detecting hemoperitoneum. J. Trauma 1999, 46, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Richards, J.R.; Ormsby, E.L.; Romo, M.V.; Gillen, M.A.; McGahan, J.P. Blunt abdominal injury in the pregnant patient: Detection with US. Radiology 2004, 233, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, H.; Holmes, J.F.; Wisner, D.H. Abdominal ultrasound examination in pregnant blunt trauma patients. J. Trauma 2001, 50, 689–693. [Google Scholar] [CrossRef] [PubMed]
- Kok, R.D.; de Vries, M.M.; Heerschap, A.; van den Berg, P.P. Absence of harmful effects of magnetic resonance exposure at 1.5 T in utero during the third trimester of pregnancy: A follow-up study. Magn. Imaging 2004, 22, 851–854. [Google Scholar] [CrossRef] [PubMed]
- Kanal, E.; Barkovich, A.J.; Bell, C.; Borgstede, J.P.; Bradley, W.G., Jr.; Froelich, J.W.; Gilk, T.; Gimbel, J.R.; Gosbee, J.; Kuhni-Kaminski, E.; et al. ACR guidance document for safe MR practices: 2007. Am J. Roentgenol. 2007, 188, 1447–1474. [Google Scholar] [CrossRef]
- Sensakovic, W.F.; Royall, I.; Hough, M.; Potrebko, P.; Grekoski, V.; Vicenti, R. Fetal Dosimetry at CT: A Primer. Radiographics 2020, 40, 1061–1070. [Google Scholar] [CrossRef]
- Chaparian, A.; Aghabagheri, M. Fetal radiation doses and subsequent risks from X-ray examinations: Should we be concerned? Iran. J. Reprod. Med. 2013, 11, 899–904. [Google Scholar]
- Raptis, C.A.; Mellnick, V.M.; Raptis, D.A.; Kitchin, D.; Fowler, K.J.; Lubner, M.; Bhalla, S.; Menias, C.O. Imaging of Trauma in the pregnant patient. Radiographies 2014, 34, 3. [Google Scholar] [CrossRef]





| Examinations Using Ionizing Radiation | Estimated Fetal Dose [mGy] |
|---|---|
| Radiography | |
| Cervical spine [AP, lateral] | <0.001 |
| Extremities | <0.001 |
| Chest [PA, lateral] | 0.002 |
| Thoracic spine | 0.003 |
| Lumbar spine [AP, lateral] | 1 |
| Pelvis | 1.2 |
| Computed Tomography (CT) | |
| CT Head | 0 |
| CT Chest | 0.2 |
| CT Abdomen | 4 |
| CT Abdomen and pelvis | 25 |
| CT Angiography aorta | 34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
MacDermott, R.; Berger, F.H.; Phillips, A.; Robins, J.A.; O’Keeffe, M.E.; Mughli, R.A.; MacLean, D.B.; Liu, G.; Heipel, H.; Nathens, A.B.; et al. Initial Imaging of Pregnant Patients in the Trauma Bay—Discussion and Review of Presentations at a Level-1 Trauma Centre. Diagnostics 2024, 14, 276. https://doi.org/10.3390/diagnostics14030276
MacDermott R, Berger FH, Phillips A, Robins JA, O’Keeffe ME, Mughli RA, MacLean DB, Liu G, Heipel H, Nathens AB, et al. Initial Imaging of Pregnant Patients in the Trauma Bay—Discussion and Review of Presentations at a Level-1 Trauma Centre. Diagnostics. 2024; 14(3):276. https://doi.org/10.3390/diagnostics14030276
Chicago/Turabian StyleMacDermott, Roisin, Ferco H. Berger, Andrea Phillips, Jason A. Robins, Michael E. O’Keeffe, Rawan Abu Mughli, David B. MacLean, Grace Liu, Heather Heipel, Avery B. Nathens, and et al. 2024. "Initial Imaging of Pregnant Patients in the Trauma Bay—Discussion and Review of Presentations at a Level-1 Trauma Centre" Diagnostics 14, no. 3: 276. https://doi.org/10.3390/diagnostics14030276
APA StyleMacDermott, R., Berger, F. H., Phillips, A., Robins, J. A., O’Keeffe, M. E., Mughli, R. A., MacLean, D. B., Liu, G., Heipel, H., Nathens, A. B., & Qamar, S. R. (2024). Initial Imaging of Pregnant Patients in the Trauma Bay—Discussion and Review of Presentations at a Level-1 Trauma Centre. Diagnostics, 14(3), 276. https://doi.org/10.3390/diagnostics14030276






