Diagnosis, Management, and Prognosis of Cystic Fibrosis-Related Liver Disease in Children
Abstract
1. Introduction
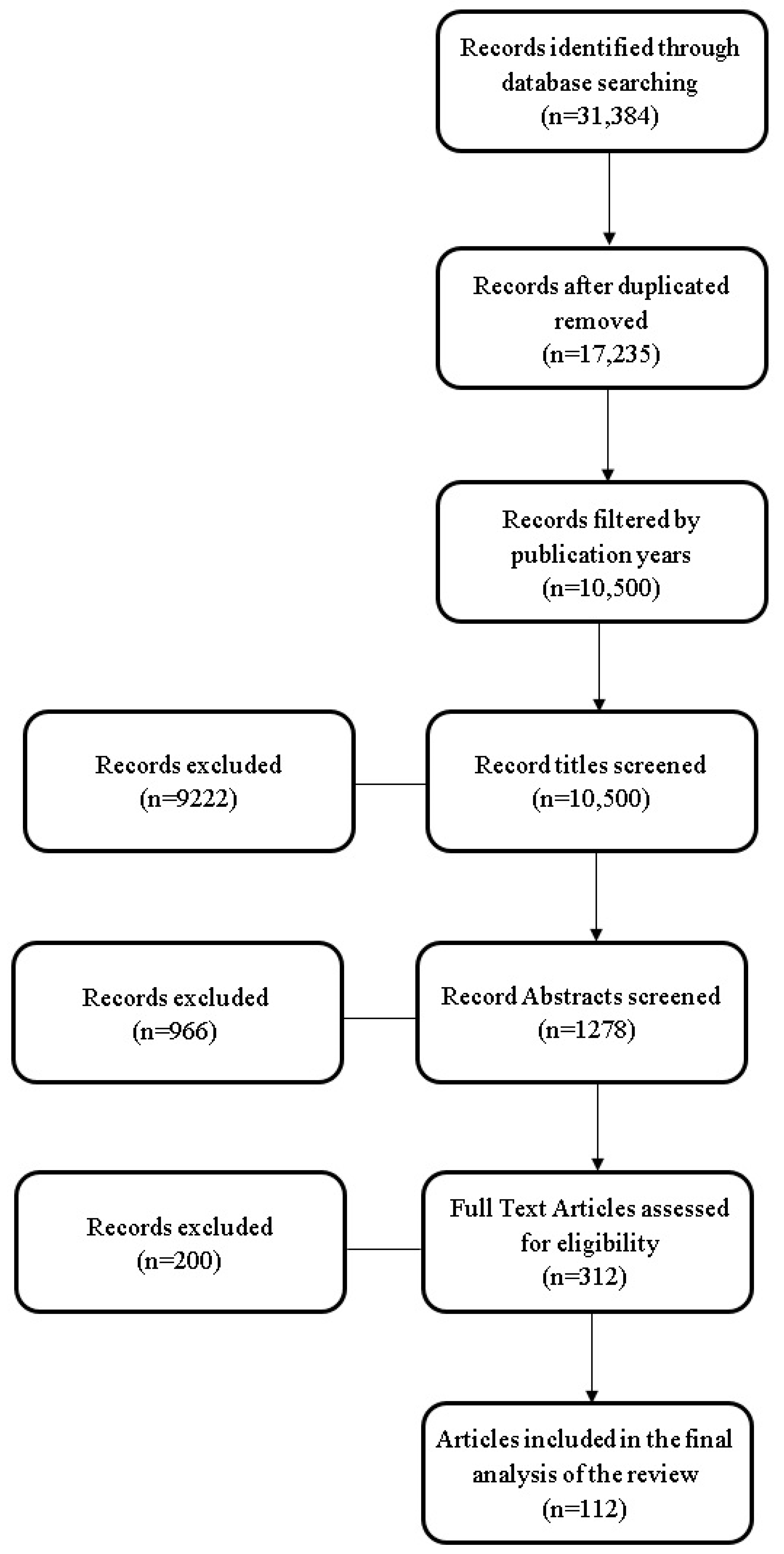
2. Methods and Search Strategy
3. Results
3.1. General Data
3.1.1. Definition
3.1.2. Epidemiology
3.1.3. Pathophysiology of CFLD
3.2. Diagnosis
3.2.1. Clinical Data
- CFLD and meconium ileus
- B.
- Liver disease without portal hypertension
- C.
- Liver disease with cirrhosis/portal hypertension
- D.
- Hepatopulmonary syndrome
- E.
- Gallbladder and biliary tract involvement
- F.
- CFLD and association with endocrine diseases
- G.
- The occurrence of Distal Intestinal Obstructive Syndrome (DIOS) in CFLD post-transplant children
3.2.2. Laboratory and Paraclinical Findings
- A.
- Laboratory Tests
- B.
- Liver Fibrosis Index
- The GGT-to-platelet ratio (GPR) serves as a predictor of CFLD, with a value between 0.20 and 0.32 associated with moderate hepatic fibrosis, while a value exceeding 0.68, coupled with a heterogeneous liver appearance on ultrasound, predicts CFLD risk [11].
- The albumin–bilirubin score (ALBI) proves superior to the Child–Pugh score in assessing liver disease severity in CF patients, according to Poetter-Lang et al.’s study (2019) [52].
- The AST-to-platelet ratio index (APRI) is considered a reliable marker for hepatic fibrosis and is recommended for annual assessment. A value of ≥0.5 necessitates further imaging evaluation, while a value ≥ 1 warrants additional investigations, including biopsy.
- The Fibrosis-4 index (FIB-4).
- Other pertinent parameters in liver fibrosis diagnosis include aminopeptides type III procollagen, collagen I and IV, laminin, hyaluronic acid, cytokines, and chemokines [25].
- C.
- Paraclinical Investigations
- (a)
- Liver Ultrasound
- (b)
- Computer Tomography (CT) and Magnetic Resonance Imaging (MRI)
- (c)
- Elastography
- (d)
- Liver Scintigraphy
- (e)
- Endoscopic Retrograde Cholangiography (ERCP)
- (f)
- Liver Biopsy
- (g)
- Esophagogastroduodenoscopy (EGD)
3.2.3. Differential Diagnosis
- Non-alcoholic fatty liver disease, where hepatic steatosis is the predominant hepatic manifestation, observed in 20–60% of cases;
- Primary sclerosing cholangitis, characterized by inflammation and fibrosis of the intra- and extrahepatic bile ducts, presenting similar histological and radiological features;
3.3. CFLD Management
3.3.1. Therapeutic Approaches
- A.
- Nutritional Interventions
- Increase daily food intake by 150%, emphasizing a higher percentage of fats, occasionally supplemented with carbohydrates (glucose polymers) cautiously due to the risk of cystic fibrosis-related diabetes (CFRD).
- Allocate 40–50% of caloric intake to fats, supplemented with medium-chain triglycerides (MCT) and polyunsaturated fatty acids (PUFAs). Research on CFTR+/+ and CFTR−/− mice demonstrated that a diet rich in MCT facilitated gallbladder emptying without significant postprandial differences in gallbladder volumes between the two groups of mice [27].
- Consume proteins at a rate of 3 g/kg body weight/day for those without indications of liver failure.
- Administer fat-soluble vitamins as supplements: vitamin A at 5000–15,000 IU/day, vitamin E at 100–500 mg alpha-tocopherol/day, vitamin D at 50 ng/kg body weight/day (up to 1 μg), and vitamin K at 1–10 mg/day, with regular plasma level monitoring to prevent deficiency or toxicity.
- B.
- Pharmacological Interventions
- C.
- CFLD and CFTR Modulators
- (a)
- Impact of CFTR Modulators on CFLD
- (b)
- Hepatotoxicity Associated with CFTR Modulators
- D.
- The Role of Probiotics in CFLD
- E.
- Surgical Management of CFLD
- F.
- Liver Transplantation
- Liver dysfunction or advanced portal hypertension;
- Progressive liver failure marked by hypoalbuminemia (below 3 g/dL), coagulopathy (INR over 1.5), jaundice, escalating ascites, and recurrent variceal bleeding;
- Hepatopulmonary, portopulmonary, and hepatorenal syndrome;
- Recurrent peritonitis;
- FEV1/FVC below 50% and severe malnutrition (contentious indication);
- Presence of extrahepatic malignancies;
- Multiorgan disease;
- Severe pulmonary hypertension unresponsive to treatment;
- Pulmonary exacerbations;
- Hepatocarcinoma, CFRD, severe cardiopulmonary disease, colonization, or infections with multi-resistant bacteria (relative contraindications) [20].
- For patients at low risk of DIOS: administration of N-acetylcysteine, senna, electrolyte GI lavage solution, and nasogastric tube in those with delayed gastric emptying.
- G.
- Future Therapies
- Gene transfer via adenoviruses or liposomes;
- Chlorine channel agonists (purinogenic nucleotides);
- Colchicine, antioxidants, steroids, interferon, growth factor modulators to reduce fibrogenesis;
- Anti-inflammatory agents to mitigate the inflammatory response;
- Antiviral prophylaxis to diminish hepatocellular destruction;
- Glutathione to stimulate bile flow in hepatocytes;
- Src tyrosine kinases targeting TLR4-mediated inflammation to reduce pro-inflammatory state in human CF cholangiocytes;
- FGF19 analogues and other fibroblast growth factors, such as FGF1 (PPARγ target), with potential therapeutic efficacy;
- Vitamin D to inhibit liver fibrosis via the TGFβ1/SMAD signaling pathway;
- Antifibrotic substances (farnesoid X receptor agonist) acting at liver and intestinal levels, participating in bile acid homeostasis [18,24,40,98,99,100,101]. In the event of persistent symptoms despite treatment, it is advisable to reassess treatment adherence, consider altering the enzyme preparation, adjust the timing of administration, address gastric acidity, and conduct investigations to rule out other gastrointestinal disorders [102].
3.3.2. Monitoring
- Annual consultations with gastroenterologists/hepatologists to evaluate cirrhosis severity, portal hypertension, and associated complications.
- Biochemical assessments (ALT, AST, GGT, ALP, prothrombin time, platelets, bilirubin) every 6 months; platelet monitoring is recommended, even if values do not suggest thrombocytopenia, due to early splenic sequestration in portal hypertension. Elevations exceeding 1.5 times normal values for transaminases, alkaline phosphatase, GGT, and bilirubin necessitate repeated analyses every 3–6 months and an abdominal ultrasound [8].
- Activation of abdominal ultrasound plus elastography annually, alternated with CT/MRI.
- Endoscopy every 2–3 years for individuals with cirrhosis or splenomegaly.
- Alpha-fetoprotein assessment every 6 months for those with cirrhosis.
- Semiannual screening for hepatocellular carcinoma.
- Liver function tests before initiating CFTR modulator therapy, followed by monthly assessments for the first year, and subsequently on an annual basis.
- Liver stiffness monitoring during CFTR modulator therapy for early detection of CFLD response or progression.
- Periodic monitoring of vitamins A, D, E, and prothrombin to prevent deficiencies or toxicity.
3.4. Disease Progression and Prognosis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Anton-Păduraru, D.T.; Trandafir, L. Fibroza chistică (mucoviscidoza). In Pediatrie; Ingrith, M., Ed.; Editura “Gr.T. Popa”, UMF: Iaṣi, Romania, 2016; pp. 300–308. [Google Scholar]
- Fiorotto, R.; Strazzabosco, M. Pathophysiology of Cystic Fibrosis Liver Disease: A Channelopathy Leading to Alterations in Innate Immunity and in Microbiota. Cell. Mol. Gastroenterol. Hepatol. 2019, 8, 197–207. [Google Scholar] [CrossRef]
- CFDB—Cystic Fibrosis DataBase. Liver Diseases. 2023. Available online: https://www.cfdb.eu/en/topics/detail/code/173 (accessed on 15 December 2023).
- FitzSimmons, S.C. The changing epidemiology of cystic fibrosis. J. Pediatr. 1993, 122, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Wasuwanich, P.; Karnsakul, W. Cystic fibrosis-associated liver disease in children. Minerva Pediatr. 2020, 72, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulou, A.; Pouriki, S.; Vasilieva, L.; Alexopoulos, T.; Filaditaki, V.; Gioka, M.; Diamantea, F.; Dourakis, S.P. Evaluation of noninvasive markers for the diagnosis of Cystic Fibrosis liver disease. Scand. J. Gastroenterol. 2018, 53, 1547–1552. [Google Scholar] [CrossRef] [PubMed]
- Sellers, Z.; Lee, L.; Barth, R.; Milla, C. New Algorithm for the Integration of Ultrasound Into Cystic Fibrosis Liver Disease Screening. JPGN 2019, 69, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Stana, B.; Bozomitu, L.; Grigoraṣ, S.; Popovici, P. Liver Involvement in Cystic Fibrosis in Children. Available online: https://www.medichub.ro/reviste-de-specialitate/pediatru-ro/liver-involvement-in-cystic-fibrosis-in-children-id-8304-cmsid-64 (accessed on 17 December 2023).
- Sellers, Z.M. Barrier to using APRI and GPR as identifiers of cystic fibrosis liver disease. J. Cyst. Fibros. 2021, 20, 551. [Google Scholar] [CrossRef]
- Debray, D.; Kelly, D.; Houwen, R.; Strandvik, B.; Colombo, C. Best practice guidance for the diagnosis and management of cystic fibrosis-associated liver disease. J. Cyst. Fibros. 2011, 10 (Suppl. 2), S29–S36. [Google Scholar] [CrossRef] [PubMed]
- Leung, H.D.; Narkewicz, R.M.; Cystic Fibrosis: Hepatobiliary Disease. UpToDate. 2023. Available online: https://medilib.ir/uptodate/show/99126 (accessed on 17 December 2023).
- Koh, C.; Sakiani, S.; Surana, P.; Zhao, X.; Eccleston, J.; Kleiner, D.E.; Herion, D.; Liang, T.J.; Hoofnagle, J.H.; Chernick, M.; et al. Adult-onset cystic fibrosis liver disease: Diagnosis and characterization of an underappreciated entity. Hepatology 2017, 66, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, I.; Streckenbach, C.; Dingemann, C.; Pfister, E.D.; di Nanni, A.; Zapf, A.; Baumann, U. Application and limitations of transient liver elastography in children. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 109–113. [Google Scholar] [CrossRef]
- Boëlle, P.Y.; Debray, D.; Guillot, L.; Clement, A.; Corvol, H. French CF Modifier Gene Study Investigators. Cystic Fibrosis Liver Disease: Outcomes and Risk Factors in a Large Cohort of French Patients. Hepatology 2019, 69, 1648–1656. [Google Scholar] [CrossRef]
- Betapudi, B.; Aleem, A.; Kothadia, J.P. Cystic Fibrosis and Liver Disease; Stat Pearls Publishing: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK556086 (accessed on 16 December 2023).
- Colombo, C.; Russo, M.C.; Zazzeron, L.; Romano, G. Liver Disease in Cystic Fibrosis. J. Pediatr. Gastroenterol. Nutr. 2006, 43, S49–S55. [Google Scholar] [CrossRef]
- Slieker, M.G.; Deckers-Kocken, J.M.; Uiterwaal, C.S.; van der Ent, C.K.; Houwen, R.H. Risk factors for the development of cystic fibrosis related liver disease. Hepatology 2003, 38, 775–776. [Google Scholar] [CrossRef]
- Staufer, K. Current Treatment Options for Cystic Fibrosis-Related Liver Disease. Int. J. Mol. Sci. 2020, 21, 8586. [Google Scholar] [CrossRef]
- Thavamani, A.; Salem, I.; Sferra, T.; Sankararaman, S. Impact of Altered Gut Microbiota and Its Metabolites in Cystic Fibrosis. Metabolites 2011, 11, 123. [Google Scholar] [CrossRef]
- Valamparampil, J.J.; Gupte, G.L. Cystic fibrosis associated liver disease in children. World J. Hepatol. 2021, 13, 1727–1742. [Google Scholar] [CrossRef]
- Bartlett, J.R.; Friedman, K.J.; Ling, S.C.; Pace, R.G.; Bell, S.C.; Bourke, B.; Castaldo, G.; Castellani, C.; Cipolli, M.; Colombo, C.; et al. Genetic modifiers of liver disease in cystic fibrosis. JAMA 2009, 302, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Hercun, J.; Alvarez, F.; Vincent, C.; Bilodeau, M. Cystic Fibrosis liver disease: A condition in need of structured transition and continuity of care. Can. Liver J. 2019, 9, 22–33. [Google Scholar] [CrossRef]
- Kianifar, H.R.; Rezaei, Y.; Khakshour, A.; Karami, H.; Khalesi, M.; Jafari, S.A.; Kiani, M.A.; Vakili, V.; Alamdaran, S.A. Cystic Fibrosis-associated Liver Disease: A Review Article. Rev. Clin. Med. 2018, 5, 146–149. [Google Scholar] [CrossRef]
- Kobelska-Dubiel, N.; Klincewicz, B.; Cichy, W. Liver Disease in Cystic Fibrosis. Prz. Gastroenterol. 2014, 9, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Wiecek, S. Liver Changes in the Course of Cystic Fibrosis. In Cystic Fibrosis—Heterogeneity and Personalized Treatment; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef]
- Van Mourik, I. Liver disease in cystic fibrosis. Pediatr. Child Health 2017, 27, 552–555. [Google Scholar] [CrossRef]
- Debray, D.; El Mourabit, H.; Merabtene, F.; Brot, L.; Ulveling, D.; Chrétien, Y.; Rainteau, D.; Moszer, I.; Wendum, D.; Sokol, H.; et al. Diet-Induced Dysbiosis and Genetic Background Synergize with Cystic Fibrosis Transmembrane Conductance Regulator Deficiency to Promote Cholangiopathy in Mice. Hepatol. Commun. 2018, 2, 153301549. [Google Scholar] [CrossRef]
- Ciucă, I.M.; Pop, L.; Ranetti, A.E.; Popescu, I.; Almăjan-Guță, B.; Malița, I.M.; Anghel, I. Ursodeoxycholic acid effects on Cystic Fibrosis liver disease. Farmacia 2015, 63, 543–547. [Google Scholar]
- Albillos, A.; de Gottardi, A.; Rescigno, M. The gut-liver axis in liver disease: Pathophysiological basis for therapy. J. Hepatol. 2020, 72, 558–577. [Google Scholar] [CrossRef]
- Anand, S.; Mande, S.S. Host-microbiome interactions: Gut-Liver axis and its connection with other organs. NPJ Biofilms Microbiomes 2022, 8, 89. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Ji, F.; Guo, J.; Shi, D.; Fang, D.; Li, L. Dysbiosis of small intestinal microbiota in liver cirrhosis and its association with etiology. Sci. Rep. 2016, 6, 34055. [Google Scholar] [CrossRef] [PubMed]
- Shao, L.; Ling, Z.; Chen, D.; Liu, Y.; Yang, F.; Li, L. Disorganized gut microbiome contributed to liver cirrhosis progression: A meta-omics-based study. Front. Microbiol. 2018, 9, 3166. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Zhao, Q.; Wei, H. Characteristics of intestinal bacteria with fatty liver diseases and cirrhosis. Ann. Hepatol. 2019, 18, 796–803. [Google Scholar] [CrossRef]
- Rager, S.L.; Zeng, M.Y. The Gut–Liver Axis in Pediatric Liver Health and Disease. Microorganisms 2023, 11, 597. [Google Scholar] [CrossRef] [PubMed]
- Kliewer, S.A.; Mangelsdorf, D.J. Bile Acids as Hormones: The FXR-FGF15/19 Pathway. Dig. Dis. 2015, 33, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Scirpo, R.; Fiorotto, R.; Villani, A.; Amenduni, M.; Spirli, C.; Strazzabosco, M. Stimulation of nuclear receptor peroxisome proliferator-activated receptor-γ limits NF-κB-dependent inflammation in mouse cystic fibrosis biliary epithelium. Hepatology 2015, 62, 1551–1562. [Google Scholar] [CrossRef]
- Ye, W.; Narkevicz, M.; Leung, D.; Karnsakul, W.; Murray, K.; Alonso, E.; Magee, J.C.; Schwarzenberg, S.J.; Weymann, A.; Molleston, J.P. Variceal Hemmmmorhage and Adverse Liver Outcomes in Patients with Cystic Fibrosis Cirrhosis. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 122–127. [Google Scholar] [CrossRef]
- Egan, M.; Schechter, M.; Voynov, J. Cystic fibrosis. In Nelson Textbook of Pediatrics, 21st ed.; Kliegman, R., St Gene, J., III, Blum, N., Shah, S., Tasker, R., Karen, W., Eds.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 2282–2297. [Google Scholar]
- Lavelle, L.; McEvoy, S.; Gibney, R.; McMahon, C.; Heffernan, E.; Malone, D. Cystic Fibrosis below the Diaphragm: Abdominal Findings in Adult Patients. Radio Graph. 2015, 35, 680–695. [Google Scholar] [CrossRef]
- Ledder, O.; Haller, W.; Couper, R.T.; Lewindon, P.; Oliver, M. Cystic fibrosis: An update for clinicians. Part 2: Hepatobiliary and pancreatic manifestations. J. Gastroenterol. Hepatol. 2014, 29, 1954–1962. [Google Scholar] [CrossRef]
- Leung, H.D.; Narkewicz, R.M. Cystic Fibrosis-related cirrhosis. J. Cyst. Fibros. 2017, 16, S50–S61. [Google Scholar] [CrossRef]
- Robertson, M.; Choe, K.; Joseph, P. Review of the abdominal manifestations of cystic Fibrosis in the adult patient. Radiographics 2006, 26, 679–690. [Google Scholar] [CrossRef]
- Lin, H.; Zhou, C.; Hou, Y.; Li, Q.; Qiao, G.; Wang, Y.; Huang, Z.; Niu, J. Paracrine fibroblast growth factor 1 functions as potent therapeutic agent for intrahepatic cholestasis by downregulating synthesis of bile acid. Front. Pharmacol. 2019, 10, 1515. [Google Scholar] [CrossRef] [PubMed]
- Sherwood, J.S.; Ullal, J.; Kutney, K.; Hughan, K.S. Cystic fibrosis related liver disease and endocrine considerations. J. Clin. Transl. Endocrinol. 2021, 27, 100283. [Google Scholar] [CrossRef] [PubMed]
- Kayani, K.; Mohammed, R.; Mohiaddin, H. Cystic Fibrosis-Related Diabetes. Front. Endocrinol. 2018, 9, 20. [Google Scholar] [CrossRef] [PubMed]
- Morton, J.R.; Ansari, N.; Glanville, A.R.; Meagher, A.P.; Lord, R.V. Distal intestinal obstruction syndrome (DIOS) in patients with cystic fibrosis after lung transplantation. J. Gastrointest. Surg. 2009, 13, 1448–1453. [Google Scholar] [CrossRef] [PubMed]
- Gilljam, M.; Chaparro, C.; Tullis, E.; Chan, C.; Keshavjee, S.; Hutcheon, M. GI complications after lung transplantation in patients with cystic fibrosis. Chest 2003, 123, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Dowman, J.K.; Watson, D.; Loganathan, S.; Gunson, B.K.; Hodson, J.; Mirza, D.F.; Clarke, J.; Lloyd, C.; Honeybourne, D.; Whitehouse, J.L.; et al. Long-term impact of liver transplantation on respiratory function and nutritional status in children and adults with cystic fibrosis. Am. J. Transplant. 2012, 12, 954–964. [Google Scholar] [CrossRef]
- Gelfond, D.; Borowitz, D. Gastrointestinal Complications of Cystic Fibrosis. Clin. Gastroenterol. Hepatol. 2013, 11, 333–342. [Google Scholar] [CrossRef]
- Bodewes, F.A.; van der Doef, H.P.; Houwen, R.H.; Verkade, H.J. Increase of Serum γ-Glutamyltransferase Associated with Development of Cirrhotic Cystic Fibrosis Liver Disease. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, S.A.; Sontag, M.K.; Accurso, F.J.; Sokol, R.J.; Narkewicz, M.R. Prevalence of elevated liver enzymes in children with cystic fibrosis diagnosed by newborn screen. J. Cyst. Fibros. 2017, 16, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Poetter-Lang, S.; Staufer, K.; Baltzer, P.; Tamandl, D.; Muin, D.; Bastati, N.; Halilbasic, E.; Hodge, J.C.; Trauner, M.; Kazemi-Shirazi, L.; et al. The Efficacy of MRI in the diagnostic workup of cystic fibrosis-associated liver disease: A clinical observational cohort study. Eur. Radiol. 2019, 29, 1048–1058. [Google Scholar] [CrossRef] [PubMed]
- Siegel, M.J.; Freeman, A.J.; Ye, W.; Palermo, J.J.; Molleston, J.P.; Paranjape, S.M.; Stoll, J.; Leung, D.H.; Masand, P.; Karmazyn, B.; et al. Heterogeneous Liver on Research Ultrasound Identifies Children with Cystic Fibrosis at High Risk of Advanced Liver Disease: Interim Results of a Prospective Observational Case-Controlled Study. J. Pediatr. 2020, 219, 62–69.e4. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, S.K.; Torbenson, M.S. Liver fibrosis quantification. Abdom. Radiol. 2022, 47, 1032–1052. [Google Scholar] [CrossRef] [PubMed]
- de Lédinghen, V.; Le Bail, B.; Rebouissoux, L.; Fournier, C.; Foucher, J.; Miette, V.; Castéra, L.; Sandrin, L.; Merrouche, W.; Lavrand, F.; et al. Liver stiffness measurement in children using FibroScan: Feasibility study and comparison with Fibrotest, aspartate transaminase to platelets ratio index, and liver biopsy. J. Pediatr. Gastroenterol. Nutr. 2007, 45, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Gominon, A.L.; Frison, E.; Hiriart, J.B.; Vergniol, J.; Clouzeau, H.; Enaud, R.; Bui, S.; Fayon, M.; de Ledinghen, V.; Lamireau, T. Assessment of Liver Disease Progression in Cystic Fibrosis Using Transient Elastography. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 455–460. [Google Scholar] [CrossRef]
- Loomba, R.; Adams, L.A. Advances in non-invasive assessment of hepatic fibrosis. Gut 2020, 69, 1343–1352. [Google Scholar] [CrossRef]
- Lewindon, P.J.; Puertolas-Lopez, M.V.; Ramm, L.E.; Noble, C.; Pereira, T.N.; Wixey, J.A.; Hartel, G.F.; Calvopina, D.A.; Leung, D.H.; Ramm, G.A. Accuracy of Transient Elastography Data Combined with APRI in Detection and Staging of Liver Disease in Pediatric Patients with Cystic Fibrosis. Clin. Gastroenterol. Hepatol. 2019, 17, 2561–2569.e5. [Google Scholar] [CrossRef]
- Rath, T.; Menendez, K.M.; Kügler, M.; Hage, L.; Wenzel, C.; Schulz, R.; Graf, J.; Nährlich, L.; Roeb, E.; Roderfeld, M. TIMP-1/-2 and transient elastography allow non invasive diagnosis of cystic fibrosis associated liver disease. Dig. Liver Dis. 2012, 44, 780–787. [Google Scholar] [CrossRef]
- Karlas, T.; Neuschulz, M.; Oltmanns, A.; Güttler, A.; Petroff, D.; Wirtz, H.; Mainz, J.G.; Mössner, J.; Berg, T.; Tröltzsch, M.; et al. Non-invasive evaluation of cystic fibrosis related liver disease in adults with ARFI, transient elastography and different fibrosis scores. PLoS ONE 2012, 7, e42139. [Google Scholar] [CrossRef]
- Van Biervliet, S.; Verdievel, H.; Vande Velde, S.; De Bruyne, R.; De Looze, D.; Verhelst, X.; Geerts, A.; Robberecht, E.; Van Vlierberghe, H. Longitudinal Transient Elastography Measurements Used in Follow-up for Patients with Cystic Fibrosis. Ultrasound Med. Biol. 2016, 42, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Kitson, M.T.; Kemp, W.W.; Iser, D.M.; Paul, E.; Wilson, J.W.; Roberts, S.K. Utility of transient elastography in the non-invasive evaluation of cystic fibrosis liver disease. Liver Int. 2013, 33, 698–705. [Google Scholar] [CrossRef]
- Sadler, M.D.; Crotty, P.; Fatovich, L.; Wilson, S.; Rabin, H.R.; Myers, R.P. Noninvasive methods, including transient elastography, for the detection of liver disease in adults with cystic fibrosis. Can. J. Gastroenterol. Hepatol. 2015, 29, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Friedrich-Rust, M.; Schlueter, N.; Smaczny, C.; Eickmeier, O.; Rosewich, M.; Feifel, K.; Herrmann, E.; Poynard, T.; Gleiber, W.; Lais, C.; et al. Non-invasive measurement of liver and pancreas fibrosis in patients with cystic fibrosis. J. Cyst. Fibros. 2013, 12, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Wiecek, S.; Fabrowicz, P.; Wos, H.; Kordys-Darmolinska, B.; Cebula, M.; Gruszczynska, K.; Grzybowska-Chlebowczyk, U. Assessment of Liver Fibrosis with the Use of Elastography in Paediatric Patients with Diagnosed Cystic Fibrosis. Dis. Markers 2022, 2022, 4798136. [Google Scholar] [CrossRef] [PubMed]
- Højte, C.; Jørgensen, M.H.; Jensen, F.; Katzenstein, T.L.; Skov, M. Extended Screening for Cystic Fibrosis-related Liver Disease Including Elastography in Children and Adolescents. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 663–668. [Google Scholar] [CrossRef] [PubMed]
- van de Peppel, I.P.; Bertolini, A.; Jonker, J.W.; Bodewes, F.A.J.A.; Verkade, H.J. Diagnosis, follow-up and treatment of cystic fibrosis-related liver disease. Curr. Opin. Pulm. Med. 2017, 23, 562–569. [Google Scholar] [CrossRef] [PubMed]
- Colombo, C.; Battezzati, P.M.; Crosignani, A.; Morabito, A.; Costantini, D.; Padoan, R.; Giunta, A. Liver disease in cystic fibrosis: A prospective study on incidence, risk factors, and outcome. Hepatology 2002, 36, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Dana, J.; Debray, D.; Beaufrère, A.; Hillaire, S.; Fabre, M.; Reinhold, C.; Baumert, T.F.; Berteloot, L.; Vilgrain, V. Cystic fibrosis-related liver disease: Clinical presentations, diagnostic and monitoring approaches in the era of CFTR modulator therapies. J. Hepatol. 2022, 76, 420–434. [Google Scholar] [CrossRef] [PubMed]
- Palaniappan, S.K.; Than, N.N.; Thein, A.W.; van Mourik, I. Interventions for preventing and managing advanced liver disease in cystic fibrosis. Cochrane Database Syst. Rev. 2020, 3, CD012056. [Google Scholar] [CrossRef] [PubMed]
- Colli, A.; Gana, J.C.; Turner, D.; Yap, J.; Adams-Webber, T.; Ling, S.C.; Casazza, G. Capsule endoscopy for the diagnosis of oesophageal varices in people with chronic liver disease or portal vein thrombosis. Cochrane Database Syst. Rev. 2014, 2014, CD008760. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.B.; Xu, J.Y.; Tantai, X.X.; Li, H.; Xiao, C.L.; Yang, C.F.; Zhang, H.; Dong, L.; Zhao, G. Non-invasive prediction model for high-risk esophageal varices in the Chinese population. World J. Gastroenterol. 2020, 26, 2839–2851. [Google Scholar] [CrossRef]
- Shimokura, G.H.; McGill, J.M.; Schlenker, T.; Fitz, J.G. Ursodeoxycholate increases cytosolic 472 calcium concentration and activates Cl-currents in a biliary cell line. Gastroenterology 1995, 109, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Fiorotto, R.; Strazzabosco, M. Cystic Fibrosis-related Liver Diseases: New Paradigm for Treatment Based on Pathophysiology. Clin. Liver Dis. 2016, 8, 113–116. [Google Scholar] [CrossRef]
- Colombo, C.; Crosignani, A.; Assaisso, M.; Battezzati, P.M.; Podda, M.; Giunta, A.; Zimmer-Nechemias, L.; Setchell, K.D. Ursodeoxycholic acid therapy in cystic fibrosis-associated liver disease: A dose-response study. Hepatology 1992, 16, 924–930. [Google Scholar] [CrossRef]
- Mujtaba, G.; Greally, P.; Elnazir, B. Ursodeoxycholic Acid for Cystic Fibrosis Related Liver Disease, Our Experience. Pediatr. Res. 2011, 70 (Suppl. 5), 534. [Google Scholar] [CrossRef]
- Colombo, C.; Crosignani, A.; Alicandro, G.; Zhang, W.; Biffi, A.; Motta, V.; Corti, F.; Setchell, K.D.R. Long-Term Ursodeoxycholic Acid Therapy Does Not Alter Lithocholic Acid Levels in Patients with Cystic Fibrosis with Associated Liver Disease. J. Pediatr. 2016, 177, 59–65.e1. [Google Scholar] [CrossRef]
- van der Feen, C.; van der Doef, H.P.; van der Ent, C.K.; Houwen, R.H. Ursodeoxycholic acid treatment is associated with improvement of liver stiffness in cystic fibrosis patients. J. Cyst. Fibros. 2016, 15, 834–838. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.; Ashby, D.; Smyth, R.L. Ursodeoxycholic acid for cystic fibrosis-related liver disease. Cochrane Database Syst. Rev. 2017, 9, CD000222. [Google Scholar] [CrossRef]
- Colombo, C.; Alicandro, G.; Oliver, M.; Lewindon, P.J.; Ramm, G.A.; Ooi, C.Y.; Alghisi, F.; Kashirskaya, N.; Kondratyeva, E.; Corti, F.; et al. Ursodeoxycholic acid and liver disease associated with cystic fibrosis: A multicenter cohort study. J. Cyst. Fibros. 2022, 21, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Sinakos, E.; Marschall, H.U.; Kowdley, K.V.; Befeler, A.; Keach, J.; Lindor, K. Bile acid changes after high-dose ursodeoxycholic acid treatment in primary sclerosing cholangitis: Relation to disease progression. Hepatology 2010, 52, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Lindor, K.D.; Kowdley, K.V.; Luketic, V.A.; Harrison, M.E.; McCashland, T.; Befeler, A.S.; Harnois, D.; Jorgensen, R.; Petz, J.; Keach, J.; et al. High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis. Hepatology 2009, 50, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, C.E.; Elborn, J.S.; Ramsey, B.W.; Marigowda, G.; Huang, X.; Cipolli, M.; Colombo, C.; Davies, J.C.; De Boeck, K.; Flume, P.A.; et al. Lumacaftor-Ivacaftor in Patients with Cystic Fibrosis Homozygous for Phe508del CFTR. N. Engl. J. Med. 2015, 373, 220–231. [Google Scholar] [CrossRef]
- Davies, J.C.; Cunningham, S.; Harris, W.T.; Lapey, A.; Regelmann, W.E.; Sawicki, G.S.; Southern, K.W.; Robertson, S.; Green, Y.; Cooke, J.; et al. Safety, pharmacokinetics, and pharmacodynamics of ivacaftor in patients aged 2–5 years with cystic fibrosis and a CFTR gating mutation (KIWI): An open-label, single-arm study. Lancet Respir. Med. 2016, 4, 107–115, Erratum in Lancet Respir. Med. 2016, 4, e57. [Google Scholar] [CrossRef]
- Rowe, S.M.; Daines, C.; Ringshausen, F.C.; Kerem, E.; Wilson, J.; Tullis, E.; Nair, N.; Simard, C.; Han, L.; Ingenito, E.P.; et al. Tezacaftor-Ivacaftor in Residual-Function Heterozygotes with Cystic Fibrosis. N. Engl. J. Med. 2017, 377, 2024–2035. [Google Scholar] [CrossRef]
- Heijerman, H.G.M.; McKone, E.F.; Downey, D.G.; Van Braeckel, E.; Rowe, S.M.; Tullis, E.; Mall, M.A.; Welter, J.J.; Ramsey, B.W.; McKee, C.M.; et al. Efficacy and safety of the elexacaftor plus tezacaftor plus ivacaftor combination regimen in people with cystic fibrosis homozygous for the F508del mutation: A double-blind, randomised, phase 3 trial. Lancet 2019, 394, 1940–1948, Erratum in Lancet 2020, 395, 1694. [Google Scholar] [CrossRef]
- Kutney, K.; Donnola, S.B.; Flask, C.A.; Gubitosi-Klug, R.; O’Riordan, M.; McBennett, K.; Sferra, T.J.; Kaminski, B. Lumacaftor/ivacaftor therapy is associated with reduced hepatic steatosis in cystic fibrosis patients. World J. Hepatol. 2019, 11, 761–772. [Google Scholar] [CrossRef]
- van de Peppel, I.P.; Doktorova, M.; Berkers, G.; de Jonge, H.R.; Houwen, R.H.J.; Verkade, H.J.; Jonker, J.W.; Bodewes, F.A.J.A. IVACAFTOR restores FGF19 regulated bile acid homeostasis in cystic fibrosis patients with an S1251N or a G551D gating mutation. J. Cyst. Fibros. 2019, 18, 286–293. [Google Scholar] [CrossRef]
- Paluck, F.; Power, N.; Lynch, C.; Cox, D.; McNally, P.; Rowland, M.; Bourke, B.; Linnane, B. Liver function tests in F508del homozygous paediatric patients with cystic fibrosis taking lumacaftor/ivacaftor combination therapy. Ir. Med. J. 2021, 114, 259. [Google Scholar]
- Drummond, D.; Dana, J.; Berteloot, L.; Schneider-Futschik, E.K.; Chedevergne, F.; Bailly-Botuha, C.; Nguyen-Khoa, T.; Cornet, M.; Le Bourgeois, M.; Debray, D.; et al. Lumacaftor-ivacaftor effects on cystic fibrosis-related liver involvement in adolescents with homozygous F508 del-CFTR. J. Cyst. Fibros. 2022, 21, 212–219. [Google Scholar] [CrossRef]
- Levitte, S.; Fuchs, Y.; Wise, R.; Sellers, Z.M. Effects of CFTR modulators on serum biomarkers of liver fibrosis in children with cystic fibrosis. Hepatol. Commun. 2023, 7, e0010. [Google Scholar] [CrossRef]
- Kennedy, L.; Hodgson, S.; Devenny, A.; Kafka, S.; Thomson, L.; Davis, J. Evaluation of the impact of cystic fibrosis modifier therapies on liver function in children and young adults. Arch. Dis. Child. 2023, 108 (Suppl. 2), A219–A220. [Google Scholar] [CrossRef]
- Romanian Ministery of Health. Raport de Evaluare a Tehnologiilor Medicale DCI: Ivacaftorum + Ivacaftorum/Tezacaftorum/Elexacaftrorum. Available online: https://www.anm.ro/_/EVALUARE%20TEHNOLOGII%20MEDICALE/MUTARI/10005_2022_Kalydeco+Kaftrio.pdf (accessed on 29 December 2023).
- De Cassya Lopes, N.L.; Taminato, M.; DaSilva Filho, L.V.R.F. Systematic Review of Probiotics for Cystic Fibrosis Patients: Moving Forward. Minerva Pediatr. 2020, 72, 440–447. [Google Scholar] [CrossRef]
- Prete, R.; Long, S.L.; Gallardo, A.L.; Gahan, C.G.; Corsetti, A.; Joyce, S.A. Beneficial bile acid metabolism from Lactobacillus plantarum of food origin. Sci. Rep. 2020, 10, 1165. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Testa, I.; Mariotti Zani, E.; Cunico, D.; Torelli, L.; Grandinetti, R.; Fainardi, V.; Pisi, G.; Principi, N. Probiotics Administration in Cystic Fibrosis: What Is the Evidence? Nutrients 2022, 14, 3160. [Google Scholar] [CrossRef] [PubMed]
- Freeman, A.J.; Sellers, Z.M.; Mazariegos, G.; Kelly, A.; Saiman, L.; Mallory, G.; Ling, S.C.; Narkewicz, M.R.; Leung, D.H. A Multidisciplinary Approach to Pretransplant and Posttransplant Management of Cystic Fibrosis-Associated Liver Disease. Liver Transpl. 2019, 25, 640–657. [Google Scholar] [CrossRef] [PubMed]
- Jonker, J.W.; Suh, J.M.; Atkins, A.R.; Ahmadian, M.; Li, P.; Whyte, J.; He, M.; Juguilon, H.; Yin, Y.Q.; Phillips, C.T.; et al. A PPARc–FGF1 axis is required for adaptive adipose remodelling and metabolic homeostasis. Nature 2012, 485, 391–394. [Google Scholar] [CrossRef]
- Ding, N.; Yu, R.T.; Subramaniam, N.; Sherman, M.H.; Wilson, C.; Rao, R.; Leblanc, M.; Coulter, S.; He, M.; Scott, C.; et al. A vitamin D receptor/SMAD genomic circuit gates hepatic fibrotic response. Cell 2013, 153, 601–613. [Google Scholar] [CrossRef] [PubMed]
- Fiorotto, R.; Scirpo, R.; Trauner, M.; Fabris, L.; Hoque, R.; Spirli, C.; Strazzabosco, M. Loss of CFTR affects biliary epithelium innate immunity and causes TLR4-NF-κB-mediated inflammatory response in mice. Gastroenterology 2011, 141, 1498–1508. [Google Scholar] [CrossRef] [PubMed]
- Fiorotto, R.; Amenduni, M.; Mariotti, V.; Fabris, L.; Spirli, C.; Strazzabosco, M. Src kinase inhibition reduces inflammatory and cytoskeletal changes in ΔF508 human cholangiocytes and improves cystic fibrosis transmembrane conductance regulator correctors efficacy. Hepatology 2018, 67, 972–988. [Google Scholar] [CrossRef] [PubMed]
- Littlewood, J.; Wolfe, S.; Conway, S. Diagnosis and treatment of intestinal malabsorption in cystic fibrosis. Pediatr. Pulmonol. 2006, 41, 35–49. [Google Scholar] [CrossRef] [PubMed]
- Green, J.; Gilchrist, F.; Carroll, W. Interventions for treating distal intestinal obstruction syndrome (DIOS) in Cystic Fibrosis. Cochrane Database Syst. Rev. 2018, 8, CD012798. [Google Scholar] [CrossRef] [PubMed]
- Schwarzenberg, S.J.; Palermo, J.J.; Ye, W.; Huang, S.; Magee, J.C.; Alazraki, A.; Freeman, A.J.; Harned, R.; Karmazyn, B.; Karnsakul, W.; et al. Health-related Quality of Life in a Prospective Study of Ultrasound to Detect Cystic Fibrosis-related Liver Disease in Children. J. Pediatr. Gastroenterol. Nutr. 2022, 75, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Gulati, R.; Radhakrishnan, K.R.; Hupertz, V.; Wyllie, R.; Alkhouri, N.; Worley, S.; Feldstein, A.E. Health-related quality of life in children with autoimmune liver disease. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 444–450. [Google Scholar] [CrossRef]
- Rodrigue, J.R.; Balistreri, W.; Haber, B.; Jonas, M.M.; Mohan, P.; Molleston, J.P.; Murray, K.F.; Narkewicz, M.; Rosenthal, P.; Smith, L.J.; et al. Impact of hepatitis C virus infection on children and their caregivers: Quality of life, cognitive, and emotional outcomes. J. Pediatr. Gastroenterol. Nutr. 2009, 48, 341–347. [Google Scholar] [CrossRef]
- Calvopina, D.A.; Noble, C.; Weis, A.; Hartel, G.F.; Ramm, L.E.; Balouch, F.; Fernandez-Rojo, M.A.; Coleman, M.A.; Lewindon, P.J.; Ramm, G.A. Supersonic shear-wave elastography and APRI for the detection and staging of liver disease in pediatric cystic fibrosis. J. Cyst. Fibros. 2019, 19, 449–457. [Google Scholar] [CrossRef]
- Scott, J.A.; Jones, A.M.; Jokl, E.; Gordon-Walker, T.; Barry, P.J.; Hanley, N.A.; Piper Hanley, K.; Athwal, V.S. Improving detection of cystic fibrosis related liver disease using liver fibrosis assessment tools. Heliyon 2023, 9, e21861. [Google Scholar] [CrossRef]
- Colomba, J.; Netedu, S.R.; Lehoux-Dubois, C.; Coriati, A.; Boudreau, V.; Tremblay, F.; Cusi, K.; Rabasa-Lhoret, R.; Leey, J.A. Hepatic enzyme ALT as a marker of glucose abnormality in men with cystic fibrosis. PLoS ONE 2019, 14, e0219855. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, A.; Volovets, A.; Haber, P.; Jo, H.; Visser, S.; Yozghatlian, V.; Taylor, N.; Nolan, S.; Dentice, R.; Malouf, M.; et al. ELX/TEZ/IVA use in cystic fibrosis liver disease: Is the perspective of improved lung function worth the risk? J. Cyst. Fibros. 2022, 21, 881–884. [Google Scholar] [CrossRef] [PubMed]
- Jardine, J.; Glinianaia, S.V.; McConachie, H.; Embleton, N.D.; Rankin, J. Self-reported quality of life of young children with conditions from early infancy: A systematic review. Pediatrics 2014, 134, e1129-48. [Google Scholar] [CrossRef] [PubMed]
- Williet, N.; Sandborn, W.J.; Peyrin-Biroulet, L. Patient-reported outcomes as primary end points in clinical trials of inflammatory bowel disease. Clin. Gastroenterol. Hepatol. 2014, 12, 1246–1256.e6. [Google Scholar] [CrossRef]

| Stages of Liver Fibrosis | METAVIR Score | Stiffness (kPa) |
|---|---|---|
| No fibrosis or portal fibrosis without septa | F0–F1 | <3.95 |
| Portal fibrosis with a few septa | F2 | ≤3.95, <7.0 |
| Septal fibrosis with many septa but no cirrhosis | F3 | ≤7.0, <9.7 |
| Cirrhosis | F4 | ≥9.7 |
| Authors | Year | Type of the Study | Aim | Results |
|---|---|---|---|---|
| Colombo et al. [75] | 1992 | Dose– response | To establish whether improved efficacy could be obtained with higher doses |
|
| Mujtaba et al. [76] | 2011 | Retrospective | To evaluate effectiveness and safety of UDCA in CFLD |
|
| Ciucă et al. [28] | 2015 | Prospective | To evaluate the efficiency of UDCA on CFLD evolution |
|
| Colombo et al. [77] | 2016 | Observational | To evaluate the fasting and postprandial serum bile acid composition in patients with CFLD after chronic administration of UDCA | Enhanced biotransformation of UDCA to the hepatotoxic secondary bile acid lithocholic acid occurs when the patients are treated with high doses |
| van derFeen et al. [78] | 2016 | Observational | To measure liver stiffness in CF patients treated with UDCA and in those without UDCA | UDCA reduced liver stiffness in patients with mild liver disease |
| Cheng et al. [79] | 2017 | Randomized controlled trials | To analyze if UDCA improves indices of liver function, reduces the risk of developing chronic liver disease, improves outcomes in CF |
|
| Colombo et al. [80] | 2022 | Retrospective multicenter cohort | To evaluate the incidence of severe liver disease in patients who received UDCA compared with those who do not receive it | Did not show a lower incidence of portal hypertension in CF patients treated with UDCA |
| Author | Year | CFTR Modulator | Type of Study | Aim | Results |
|---|---|---|---|---|---|
| Wainwright et al. [83] | 2015 | LUMA/IVA | Double-blind, placebo-controlled, phase 3, randomized | To evaluate the incidence of adverse events in children ≥ 12 years old with CF | 5.2% cases: elevation of ALT, AST > 3 × ULN |
| Davies et al. [84] | 2016 | IVA | Open-label, single-arm | To assess the safety, pharmacokinetics, and pharmacodynamics in children 2–5 years old |
|
| Rowe et al. [85] | 2017 | IVA IVA/TEZ | Double-blind, placebo-controlled, phase 3, randomized | To evaluate the efficacy and safety in CF heterozygous, Phe508 del mutation | No clinically adverse events in the level of ALT, AST, total bilirubin |
| Heijerman et al. [86] | 2019 | IVA/TEZ ETI | Double-blind, randomized, phase 3 | To evaluate the safety |
|
| Kutney et al. [87] | 2019 | LUMA/IVA | Cross-sectional | To explore the impact of LUMA/IVA on hepatic steatosis in patients 11.3–39 years old |
|
| van de Peppel et al. [88] | 2019 | IVA | Observational | To assess the effect of IVA on the enterohepatic circulation by assessing markers of bile acids homeostasis | IVA partially restored this disruption of bile acids homeostasis |
| Paluck et al. [89] | 2021 | LUMA/IVA | Retrospective chart review | To assess whether F508 del homozygous CF patients ≥ 12 years old have a derangement of LTs | Significant decrease in ALT, GGT, total bilirubin levels and no change in AST after 3 months of treatment |
| Drummond et al. [90] | 2022 | LUMA/IVA | Observational | Effects on features of liver involvement in F508 del homozygous CF adolescents |
|
| Levite et al. [91] | 2023 | LUMA/IVA | Retrospective | To observe alterations in LTs and fibrosis index |
|
| ETI | No differences | ||||
| Kennedy et al. [92] | 2023 | ETI | Retrospective observational | To evaluate LTs |
|
| To evaluate the aspect of the liver by ultrasound | No patients with significant changes on liver US | ||||
| To evaluate the safety | CFTR modulators are safe |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anton-Păduraru, D.-T.; Azoicăi, A.N.; Trofin, F.; Murgu, A.M.; Mîndru, D.E.; Bocec, A.S.; Halițchi, C.O.I.; Zota, G.R.; Păduraru, D.; Nastase, E.V. Diagnosis, Management, and Prognosis of Cystic Fibrosis-Related Liver Disease in Children. Diagnostics 2024, 14, 538. https://doi.org/10.3390/diagnostics14050538
Anton-Păduraru D-T, Azoicăi AN, Trofin F, Murgu AM, Mîndru DE, Bocec AS, Halițchi COI, Zota GR, Păduraru D, Nastase EV. Diagnosis, Management, and Prognosis of Cystic Fibrosis-Related Liver Disease in Children. Diagnostics. 2024; 14(5):538. https://doi.org/10.3390/diagnostics14050538
Chicago/Turabian StyleAnton-Păduraru, Dana-Teodora, Alice Nicoleta Azoicăi, Felicia Trofin, Alina Mariela Murgu, Dana Elena Mîndru, Ana Simona Bocec, Codruța Olimpiada Iliescu Halițchi, Gabriela Rusu Zota, Diana Păduraru, and Eduard Vasile Nastase. 2024. "Diagnosis, Management, and Prognosis of Cystic Fibrosis-Related Liver Disease in Children" Diagnostics 14, no. 5: 538. https://doi.org/10.3390/diagnostics14050538
APA StyleAnton-Păduraru, D.-T., Azoicăi, A. N., Trofin, F., Murgu, A. M., Mîndru, D. E., Bocec, A. S., Halițchi, C. O. I., Zota, G. R., Păduraru, D., & Nastase, E. V. (2024). Diagnosis, Management, and Prognosis of Cystic Fibrosis-Related Liver Disease in Children. Diagnostics, 14(5), 538. https://doi.org/10.3390/diagnostics14050538






