Clinical and MRI-Based Assessment of Patients with Temporomandibular Disorders Treated by Controlled Mandibular Repositioning
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of Patients
2.2. Clinical Examinations
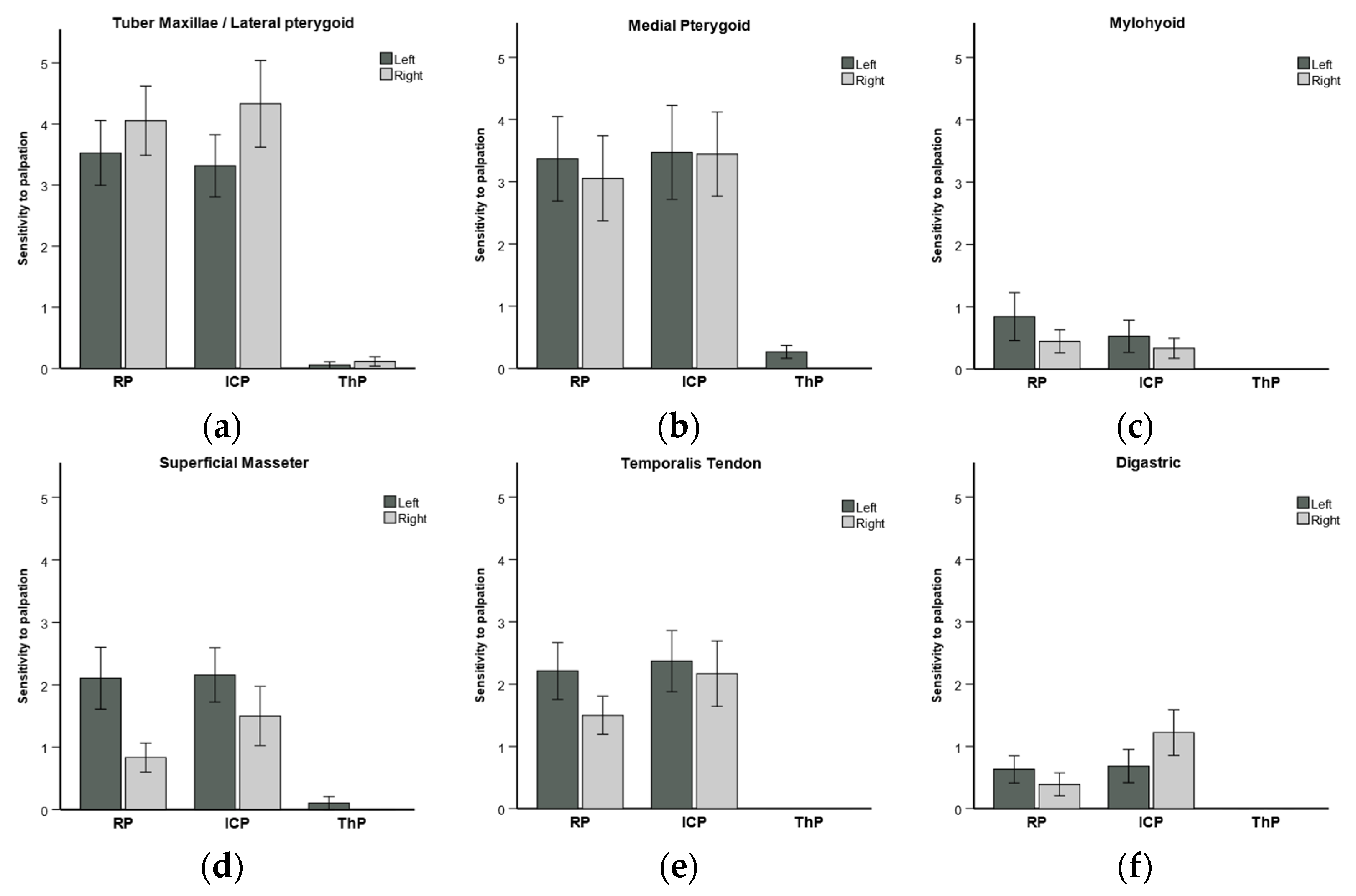
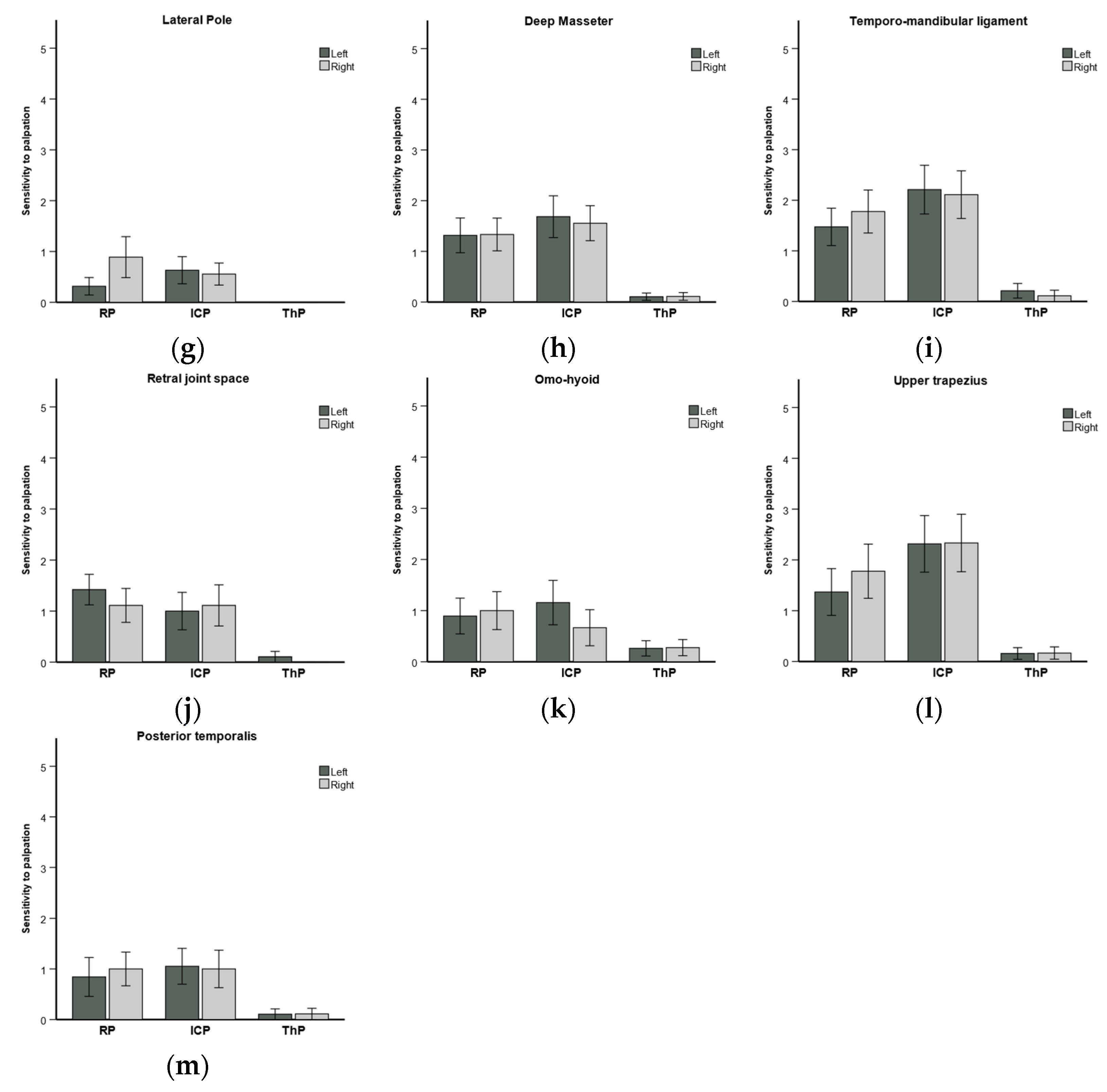
2.2.1. Sensitivity to Palpation of Muscles and Ligaments

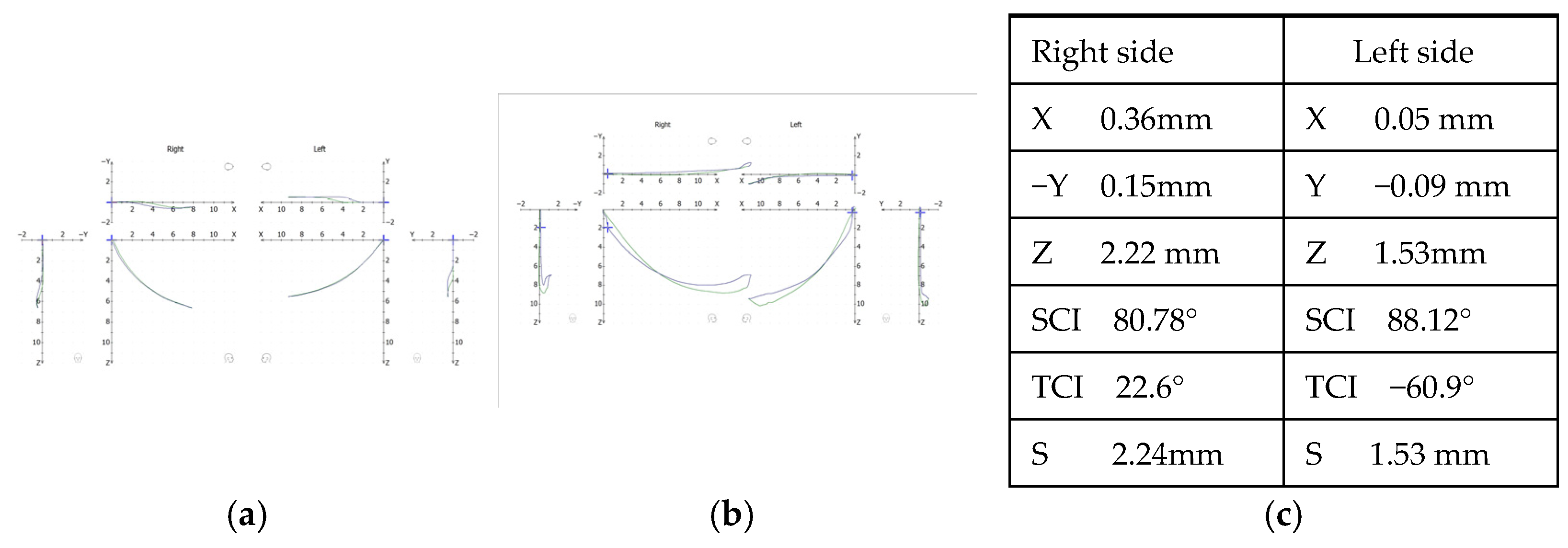
2.2.2. Condylography
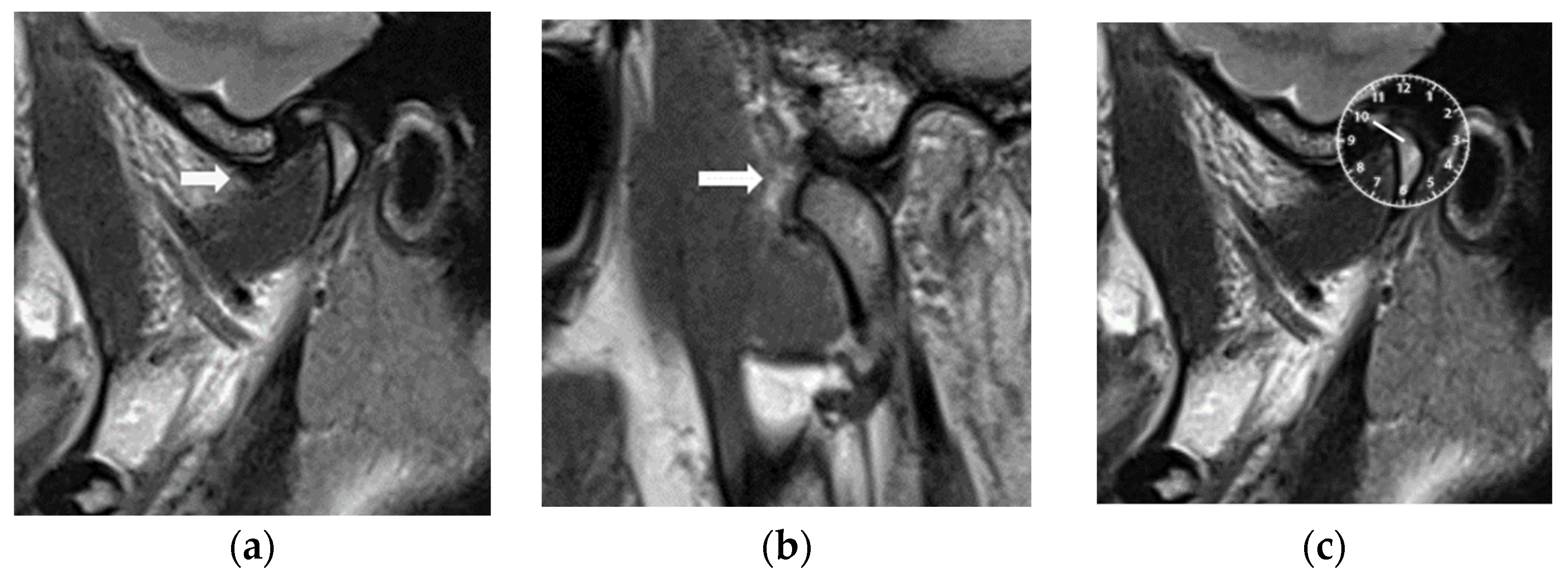
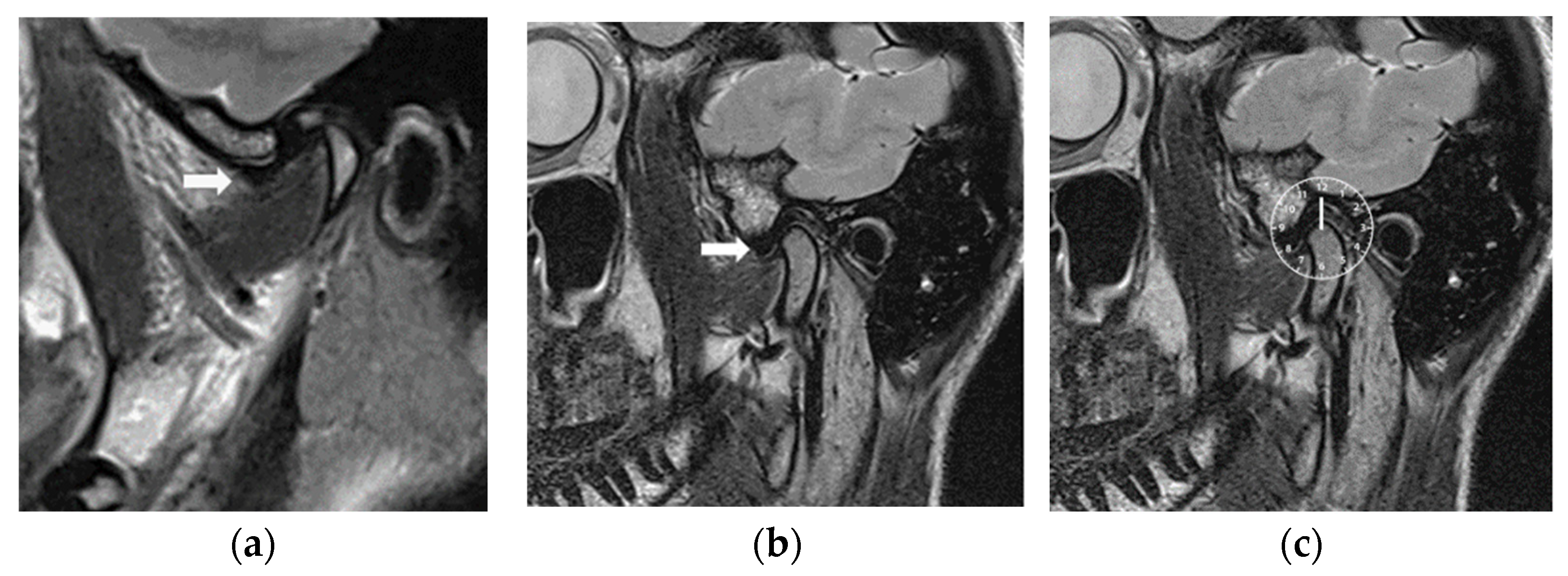
2.2.3. Magnetic Resonance Imaging
2.3. Controlled Mandibular Repositioning
2.4. Clinical Follow-Up Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Dimitroulis, G. Temporomandibular Disorders: A Clinical Update. BMJ 1998, 317, 190–194. [Google Scholar] [CrossRef]
- Larheim, T.A. Role of Magnetic Resonance Imaging in the Clinical Diagnosis of the Temporomandibular Joint. Cells Tissues Organs 2005, 180, 6–21. [Google Scholar] [CrossRef]
- Litko, M.; Szkutnik, J.; Berger, M.; Różyło-Kalinowska, I. Correlation between the Lateral Pterygoid Muscle Attachment Type and Temporomandibular Joint Disc Position in Magnetic Resonance Imaging. Dentomaxillofac. Radiol. 2016, 45, 20160229. [Google Scholar] [CrossRef]
- Schmid-Schwap, M.; Drahanowsky, W.; Bristela, M.; Kundi, M.; Piehslinger, E.; Robinson, S. Diagnosis of Temporomandibular Dysfunction Syndrome—Image Quality at 1.5 and 3.0 Tesla Magnetic Resonance Imaging. Eur. Radiol. 2009, 19, 1239–1245. [Google Scholar] [CrossRef]
- Sano, T.; Westesson, P.L. Magnetic Resonance Imaging of the Temporomandibular Joint: Increased T2 Signal in the Retrodiskal Tissue of Painful Joints. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995, 79, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.; Hollender, L.; Anderson, Q.; Kartha, K.; Ohrbach, R.; Truelove, E.L.; John, M.T.; Schiffman, E.L. Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD): Development of Image Analysis Criteria and Examiner Reliability for Image Analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 844–860. [Google Scholar] [CrossRef] [PubMed]
- Provenzano, M.d.M.; Chilvarquer, I.; Fenyo-Pereira, M. How Should the Articular Disk Position Be Analyzed? J. Oral Maxillofac. Surg. 2012, 70, 1534–1539. [Google Scholar] [CrossRef]
- Tasaki, M.M.; Westesson, P.L.; Isberg, A.M.; Ren, Y.F.; Tallents, R.H. Classification and Prevalence of Temporomandibular Joint Disk Displacement in Patients and Symptom-Free Volunteers. Am. J. Orthod. Dentofac. Orthop. 1996, 109, 249–262. [Google Scholar] [CrossRef] [PubMed]
- Rammelsberg, P.; Pospiech, P.R.; Jäger, L.; Pho Duc, J.M.; Böhm, A.O.; Gernet, W. Variability of Disk Position in Asymptomatic Volunteers and Patients with Internal Derangements of the TMJ. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1997, 83, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Tasaki, M.M.; Westesson, P.L. Temporomandibular Joint: Diagnostic Accuracy with Sagittal and Coronal MR Imaging. Radiology 1993, 186, 723–729. [Google Scholar] [CrossRef]
- Tognini, F.; Manfredini, D.; Montagnani, G.; Bosco, M. Is Clinical Assessment Valid for the Diagnosis of Temporomandibular Joint Disk Displacement? Minerva Stomatol. 2004, 53, 439–448. [Google Scholar] [PubMed]
- Schmid-Schwap, M.; Briedl, J.G.; Robinson, S.; Piehslinger, E. Correlation between Disk Morphology on MRI and Time Curves Using Electronic Axiography. Cranio 2005, 23, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Piancino, M.G.; Cirillo, S.; Frongia, G.; Cena, F.; Bracco, A.A.; Dalmasso, P.; Bracco, P. Sensitivity of Magnetic Resonance Imaging and Computed Axiography in the Diagnosis of Temporomandibular Joint Disorders in a Selected Patient Population. Int. J. Prosthodont. 2012, 25, 120–126. [Google Scholar] [PubMed]
- Manfredini, D.; Favero, L.; Federzoni, E.; Cocilovo, F.; Guarda-Nardini, L. Kinesiographic Recordings of Jaw Movements Are Not Accurate to Detect Magnetic Resonance-Diagnosed Temporomandibular Joint (TMJ) Effusion and Disk Displacement: Findings from a Validation Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Emshoff, R.; Brandlmaier, I.; Bösch, R.; Gerhard, S.; Rudisch, A.; Bertram, S. Validation of the Clinical Diagnostic Criteria for Temporomandibular Disorders for the Diagnostic Subgroup—Disc Derangement with Reduction. J. Oral Rehabil. 2002, 29, 1139–1145. [Google Scholar] [CrossRef] [PubMed]
- Talmaceanu, D.; Bolog, N.; Leucuta, D.; Tig, I.A.; Buduru, S. Diagnostic Use of Computerized Axiography in TMJ Disc Displacements. Exp. Ther. Med. 2022, 23, 213. [Google Scholar] [CrossRef]
- Parlett, K.; Paesani, D.; Tallents, R.H.; Hatala, M.A. Temporomandibular Joint Axiography and MRI Findings: A Comparative Study. J. Prosthet. Dent. 1993, 70, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Piehslinger, E.; Schimmerl, S.; Celar, A.; Crowley, C.; Imhof, H. Comparison of Magnetic Resonance Tomography with Computerized Axiography in Diagnosis of Temporomandibular Joint Disorders. Int. J. Oral Maxillofac. Surg. 1995, 24 Pt 1, 13–19. [Google Scholar] [CrossRef]
- Gsellmann, B. Diagnostische Schritte Bei Diskusluxationen Und Anderen Häufigen Erkrankungen Des Temporomandibulargelenks. Radiologe 2001, 41, 730–733. [Google Scholar] [CrossRef]
- Dimitroulis, G. Management of Temporomandibular Joint Disorders: A Surgeon’s Perspective. Aust. Dent. J. 2018, 63 (Suppl. S1), S79–S90. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Farea, R.; Qasem, K.A.; Al-Wadeai, M.S.; Al-Sabahi, M.E.; Al-Iryani, G.M. Effectiveness of Occlusal Splint Therapy in the Management of Temporomandibular Disorders: Network Meta-Analysis of Randomized Controlled Trials. Int. J. Oral Maxillofac. Surg. 2020, 49, 1042–1056. [Google Scholar] [CrossRef]
- Albagieh, H.; Alomran, I.; Binakresh, A.; Alhatarisha, N.; Almeteb, M.; Khalaf, Y.; Alqublan, A.; Alqahatany, M. Occlusal Splints-Types and Effectiveness in Temporomandibular Disorder Management. Saudi Dent. J. 2023, 35, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Greene, C.S.; Menchel, H.F. The Use of Oral Appliances in the Management of Temporomandibular Disorders. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Shao, B.; Chong, D.Y.R.; Liu, Z. Morphological Analysis of the Temporomandibular Joint in Patients with Anterior Disc Displacement. Comput. Methods Biomech. Biomed. Eng. 2023, 27, 521–530. [Google Scholar] [CrossRef]
- Mehra, P.; Wolford, L.M. The Mitek Mini Anchor for TMJ Disc Repositioning: Surgical Technique and Results. Int. J. Oral Maxillofac. Surg. 2001, 30, 497–503. [Google Scholar] [CrossRef]
- Dhar, S.; Kumar, N.; Ashrafullah; Dhaded, N.; Hegde, P.; Chhabaria Peswani, K. Assessing the Efficacy of Anterior Repositioning Splints in the Management of Temporomandibular Disc Displacement: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e47689. [Google Scholar] [CrossRef]
- Dylina, T.J. A Common-Sense Approach to Splint Therapy. J. Prosthet. Dent. 2001, 86, 539–545. [Google Scholar] [CrossRef]
- Riley, P.; Glenny, A.-M.; Worthington, H.V.; Jacobsen, E.; Robertson, C.; Durham, J.; Davies, S.; Petersen, H.; Boyers, D. Oral Splints for Temporomandibular Disorder or Bruxism: A Systematic Review. Br. Dent. J. 2020, 228, 191–197. [Google Scholar] [CrossRef]
- Alkhutari, A.S.; Alyahya, A.; Rodrigues Conti, P.C.; Christidis, N.; Al-Moraissi, E.A. Is the Therapeutic Effect of Occlusal Stabilization Appliances More than Just Placebo Effect in the Management of Painful Temporomandibular Disorders? A Network Meta-Analysis of Randomized Clinical Trials. J. Prosthet. Dent. 2021, 126, 24–32. [Google Scholar] [CrossRef]
- Seifeldin, S.A.; Elhayes, K.A. Soft versus Hard Occlusal Splint Therapy in the Management of Temporomandibular Disorders (TMDs). Saudi Dent. J. 2015, 27, 208–214. [Google Scholar] [CrossRef]
- Chen, H.M.; Liu, M.Q.; Yap, A.U.J.; Fu, K.Y. Physiological Effects of Anterior Repositioning Splint on Temporomandibular Joint Disc Displacement: A Quantitative Analysis. J. Oral Rehabil. 2017, 44, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Fayed, M.M.S.; El-Mangoury, N.H.; El-Bokle, D.N.; Belal, A.I. Occlusal Splint Therapy and Magnetic Resonance Imaging. World J. Orthod. 2004, 5, 133–140. [Google Scholar] [PubMed]
- Kurita, H.; Kurashina, K.; Baba, H.; Ohtsuka, A.; Kotani, A.; Kopp, S. Evaluation of Disk Capture with a Splint Repositioning Appliance: Clinical and Critical Assessment with MR Imaging. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 85, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Yap, A.U.-J.; Liu, M.-Q.; Fu, K.-Y. Condylar Repair and Regeneration in Adolescents/Young Adults with Early-Stage Degenerative Temporomandibular Joint Disease: A Randomised Controlled Study. J. Oral Rehabil. 2019, 46, 704–714. [Google Scholar] [CrossRef]
- Ma, Z.; Xie, Q.; Yang, C.; Zhang, S.; Shen, Y.; Abdelrehem, A. Can Anterior Repositioning Splint Effectively Treat Temporomandibular Joint Disc Displacement? Sci. Rep. 2019, 9, 534. [Google Scholar] [CrossRef]
- Chen, H.; Fu, K.; Li, Y.; Zhang, Z. Positional Changes of Temporomandibular Joint Disk and Condyle with Insertion of Anterior Repositioning Splint. Hua Xi Kou Qiang Yi Xue Za Zhi 2009, 27, 408–412. [Google Scholar]
- Zamburlini, I.; Austin, D. Long-Term Results of Appliance Therapies in Anterior Disk Displacement with Reduction: A Review of the Literature. Cranio 1991, 9, 361–368. [Google Scholar] [CrossRef]
- Lundh, H.; Westesson, P.L.; Kopp, S.; Tillström, B. Anterior Repositioning Splint in the Treatment of Temporomandibular Joints with Reciprocal Clicking: Comparison with a Flat Occlusal Splint and an Untreated Control Group. Oral Surg. Oral Med. Oral Pathol. 1985, 60, 131–136. [Google Scholar] [CrossRef]
- Li, H.; Shen, D.; Chen, Z.; Li, J. Step-Back Anterior Repositioning Splint Retraction for Temporomandibular Joint Disc Displacement with Reduction in Adult Patients. J. Oral Rehabil. 2023, 50, 965–971. [Google Scholar] [CrossRef]
- Summer, J.D.; Westesson, P.L. Mandibular Repositioning Can Be Effective in Treatment of Reducing TMJ Disk Displacement. A Long-Term Clinical and MR Imaging Follow-Up. Cranio 1997, 15, 107–120. [Google Scholar] [CrossRef] [PubMed]
- Garcia, A.R.; Folli, S.; Zuim, P.R.J.; de Sousa, V. Mandible Protrusion and Decrease of TMJ Sounds: An Electrovibratographic Examination. Braz. Dent. J. 2008, 19, 77–82. [Google Scholar] [CrossRef]
- Okeson, J.P. Nonsurgical Management of Disc-Interference Disorders. Dent. Clin. N. Am. 1991, 35, 29–51. [Google Scholar] [CrossRef]
- Shen, P.; Chen, X.; Xie, Q.; Zhang, S.; Yang, C. Assessment of Occlusal Appliance for the Reposition of Temporomandibular Joint Anterior Disc Displacement with Reduction. J. Craniofac. Surg. 2019, 30, 1140–1143. [Google Scholar] [CrossRef]
- Guo, Y.-N.; Cui, S.-J.; Zhou, Y.-H.; Wang, X.-D. An Overview of Anterior Repositioning Splint Therapy for Disc Displacement-Related Temporomandibular Disorders. Curr. Med. Sci. 2021, 41, 626–634. [Google Scholar] [CrossRef]
- Katzberg, R.W.; Tallents, R.H. Normal and Abnormal Temporomandibular Joint Disc and Posterior Attachment as Depicted by Magnetic Resonance Imaging in Symptomatic and Asymptomatic Subjects. J. Oral Maxillofac. Surg. 2005, 63, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Bristela, M.; Skolka, A.; Eder, J.; Szomolanyi, P.; Weber, M.; Piehslinger, E.; Schmid-Schwap, M.; Trattnig, S. T2 Mapping with 3.0 T MRI of the Temporomandibular Joint Disc of Patients with Disc Dislocation. Magn. Reson. Imaging 2019, 58, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Simmons, H.C.; Board of Directors, American Academy of Craniofacial Pain. Guidelines for Anterior Repositioning Appliance Therapy for the Management of Craniofacial Pain and TMD. Cranio 2005, 23, 300–305. [Google Scholar] [CrossRef]
- Tecco, S.; Festa, F.; Salini, V.; Epifania, E.; D’Attilio, M. Treatment of Joint Pain and Joint Noises Associated with a Recent TMJ Internal Derangement: A Comparison of an Anterior Repositioning Splint, a Full-Arch Maxillary Stabilization Splint, and an Untreated Control Group. Cranio 2004, 22, 209–219. [Google Scholar] [CrossRef]
- Okeson, J.P. Long-Term Treatment of Disk-Interference Disorders of the Temporomandibular Joint with Anterior Repositioning Occlusal Splints. J. Prosthet. Dent. 1988, 60, 611–616. [Google Scholar] [CrossRef]
- Ekberg, E.C.; Sabet, M.E.; Petersson, A.; Nilner, M. Occlusal Appliance Therapy in a Short-Term Perspective in Patients with Temporomandibular Disorders Correlated to Condyle Position. Int. J. Prosthodont. 1998, 11, 263–268. [Google Scholar]
- Wänman, A.; Marklund, S. Treatment Outcome of Supervised Exercise, Home Exercise and Bite Splint Therapy, Respectively, in Patients with Symptomatic Disc Displacement with Reduction: A Randomised Clinical Trial. J. Oral Rehabil. 2020, 47, 143–149. [Google Scholar] [CrossRef]
- Maheshwari, K.; Srinivasan, R.; Singh, B.P.; Tiwari, B.; Kirubakaran, R. Effectiveness of Anterior Repositioning Splint versus Other Occlusal Splints in the Management of Temporomandibular Joint Disc Displacement with Reduction: A Meta-Analysis. J. Indian Prosthodont. Soc. 2024, 24, 15–24. [Google Scholar]
- Kuzmanovic Pficer, J.; Dodic, S.; Lazic, V.; Trajkovic, G.; Milic, N.; Milicic, B. Occlusal Stabilization Splint for Patients with Temporomandibular Disorders: Meta-Analysis of Short and Long Term Effects. PLoS ONE 2017, 12, e0171296. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xu, L.; Wu, D.; Yu, C.; Fan, S.; Cai, B. Effectiveness of Exercise Therapy versus Occlusal Splint Therapy for the Treatment of Painful Temporomandibular Disorders: A Systematic Review and Meta-Analysis. Ann. Palliat. Med. 2021, 10, 6122–6132. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Crimi, S.; Badnjević, A.; Cervino, G.; Bianchi, A.; Cicciù, M. Correlation between Temporomandibular Disorders (TMD) and Posture Evaluated Trough the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): A Systematic Review with Meta-Analysis. J. Clin. Med. 2023, 12, 2652. [Google Scholar] [CrossRef] [PubMed]

| No. Patients | Females | Males | Age in Years Mean ± SD Range | Joints with ADDwR | Excluded Joints |
|---|---|---|---|---|---|
| 20 | 18 | 2 | 28.7 ± 6.4 (18–41) | 37 | 3 * |
| Parameter | β | SE (β) | df | t | p-Value | 95% CI |
|---|---|---|---|---|---|---|
| RP vs. ThP | 1.325 | 0.079 | 1302 | 16.721 | <0.001 * | [1.170; 1.480] |
| ICP vs. ThP | 1.517 | 0.079 | 1302 | 19.147 | <0.001 * | [1.362; 1.673] |
| ThP (Intercept) | 0.081 | 0.088 | 479.2 | 0.921 | 0.358 | [−0.092; 0.253] |
| Right Joint | Left Joint | |
|---|---|---|
| Anterior disc displacement | 5 | 6 |
| Antero-lateral disc displacement | 12 | 12 |
| Antero-medial disc displacement | 1 | 1 |
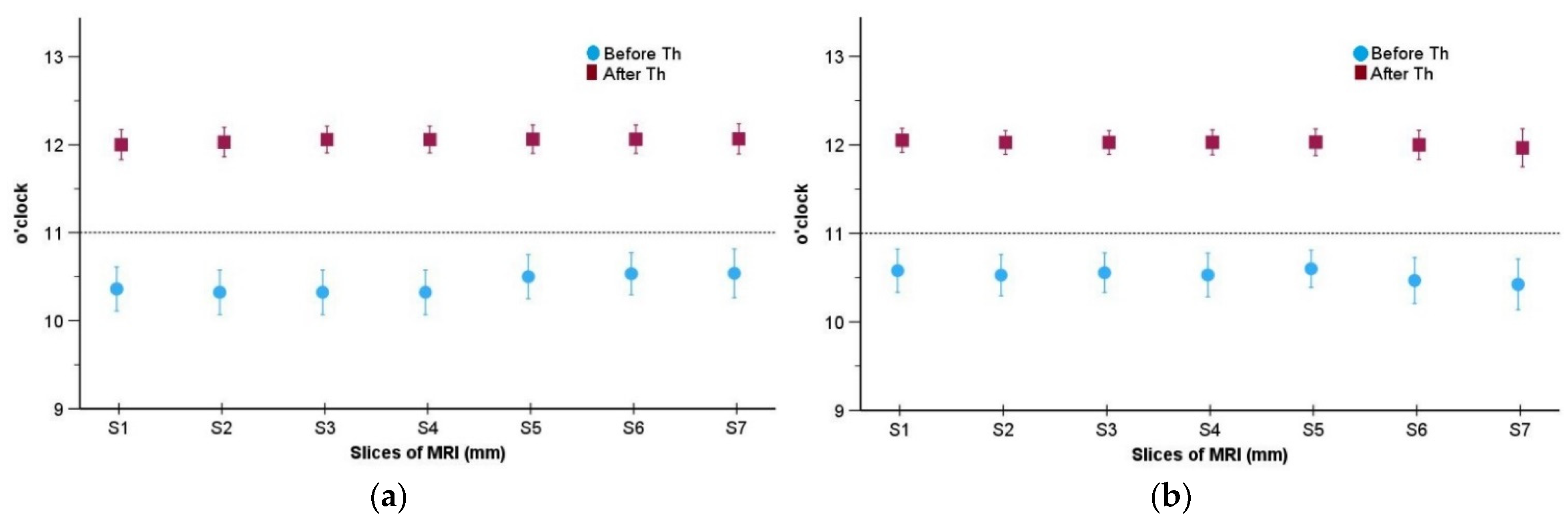
| Joint | MRI Slices | Before | After | |||
|---|---|---|---|---|---|---|
| N | Mean ± SD | N | Mean ± SD | p Value | ||
| Right | 1 | 18 | 10:21 ± 0:30 | 18 | 12:00 ± 0:20 | 0.0002 |
| 2 | 17 | 10:19 ± 0:29 | 18 | 12:01 ± 0:19 | 0.0008 | |
| 3 | 17 | 10:19 ± 0:29 | 17 | 12:03 ± 0:18 | 0.0006 | |
| 4 | 17 | 10:19 ± 0:29 | 17 | 12:03 ± 0:18 | 0.0006 | |
| 5 | 15 | 10:30 ± 0:27 | 16 | 12:03 ± 0:18 | 0.0003 | |
| 6 | 15 | 10:32 ± 0:26 | 16 | 12:03 ± 0:18 | 0.0003 | |
| 7 | 13 | 10:32 ± 0:28 | 15 | 12:04 ± 0:19 | 0.0005 | |
| Left | 1 | 19 | 10:34 ± 0:30 | 19 | 12:03 ± 0:17 | 0.0001 |
| 2 | 18 | 10:31 ± 0:28 | 18 | 12:01 ± 0:16 | 0.0002 | |
| 3 | 18 | 10:33 ± 0:27 | 18 | 12:01 ± 0:16 | 0.0001 | |
| 4 | 17 | 10:31 ± 0:28 | 17 | 12:01 ± 0:16 | 0.0009 | |
| 5 | 15 | 10:36 ± 0:23 | 16 | 12:01 ± 0:17 | 0.0002 | |
| 6 | 15 | 10:28 ± 0:28 | 16 | 12:00 ± 0:18 | 0.0005 | |
| 7 | 13 | 10:25 ± 0:29 | 15 | 11:58 ± 0:23 | 0.0005 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, D.; Landry, A.; Schmid-Schwap, M.; Piehslinger, E.; Gahleitner, A.; Chen, J.; Rausch-Fan, X. Clinical and MRI-Based Assessment of Patients with Temporomandibular Disorders Treated by Controlled Mandibular Repositioning. Diagnostics 2024, 14, 572. https://doi.org/10.3390/diagnostics14060572
Singh D, Landry A, Schmid-Schwap M, Piehslinger E, Gahleitner A, Chen J, Rausch-Fan X. Clinical and MRI-Based Assessment of Patients with Temporomandibular Disorders Treated by Controlled Mandibular Repositioning. Diagnostics. 2024; 14(6):572. https://doi.org/10.3390/diagnostics14060572
Chicago/Turabian StyleSingh, Diwakar, Alain Landry, Martina Schmid-Schwap, Eva Piehslinger, André Gahleitner, Jiang Chen, and Xiaohui Rausch-Fan. 2024. "Clinical and MRI-Based Assessment of Patients with Temporomandibular Disorders Treated by Controlled Mandibular Repositioning" Diagnostics 14, no. 6: 572. https://doi.org/10.3390/diagnostics14060572
APA StyleSingh, D., Landry, A., Schmid-Schwap, M., Piehslinger, E., Gahleitner, A., Chen, J., & Rausch-Fan, X. (2024). Clinical and MRI-Based Assessment of Patients with Temporomandibular Disorders Treated by Controlled Mandibular Repositioning. Diagnostics, 14(6), 572. https://doi.org/10.3390/diagnostics14060572






