Abstract
The diagnosis of neck pain is challenging. Many visceral disorders are known to cause it, and clinical practice guidelines recommend to rule them out during neck pain diagnosis. However, the absence of suspicion of any cause impedes one from establishing that specific aetiology as the final diagnosis. To investigate the degree of consideration given to visceral aetiology, a systematic search of trials about neck pain was carried out to evaluate their selection criteria. The search yielded 309 eligible articles, which were screened by two independent reviewers. The PEDro scale score was used to assess the methodological quality of the studies. The following information was retrieved: number of authors affiliated to a clinical or non-clinical institution, number of citations in the Web of Science, study aims, characteristics of participants, and eligibility criteria. The top 15 most cited trials, and the 15 most recent studies about treatment efficacy in neck pain, published in first quartile journals of the Journal Citation Reports, were selected. Females represented 67.5% of participants. A single study was of poor methodological quality (4/10). Based on the eligibility criteria of the articles that were systematically reviewed, it would appear that visceral aetiology was not considered in eighty percent of the trials on neck pain, showing a low level of suspicion both in research and clinical settings.
1. Introduction
Neck pain (NP) constitutes a major health problem. Its prevalence varies from 4.8% to 79.5%, and is more common in females and in high-incomes countries [1]. It is ranked the 4th most disabling condition as measured by years lived with disability [2]; hence, it poses a substantial economic burden due to extended periods of sick leave and high use of health services [3]. Those individuals with a precise pathoanatomical cause for their NP, e.g., radiculopathy [4,5], facet joint pain [6], chronic rheumatic diseases [7], or cancer, are categorized as having specific NP. Yet, patients without a well identified source for their NP are labelled as having idiopathic, mechanical, or non-specific NP, which is the most common type [8].
As a sign of visceral suffering, pain originating in internal organs is amongst the most frequent forms of pain experienced by individuals in the course of life, and pain involving internal organs is a major occurrence in the clinical setting [9,10]. The rule in visceral nociception is that pain is referred to somatic tissues, being felt at a site other than the affected viscera [10]. Visceral referred pain (VRP) occurs, as secondary hyperalgesia, in somatic areas neuromerically connected with the affected organs [10]. The overlap of somatic and visceral afferent information into a shared neural pathway seems to be related to a misinterpretation at peripheral, spinal, or supraspinal levels [10,11]. The precise substrate underlying this phenomenon remains unknown [12]; it has been stated that it might explain the strong association between back pain and digestive disorders [13].
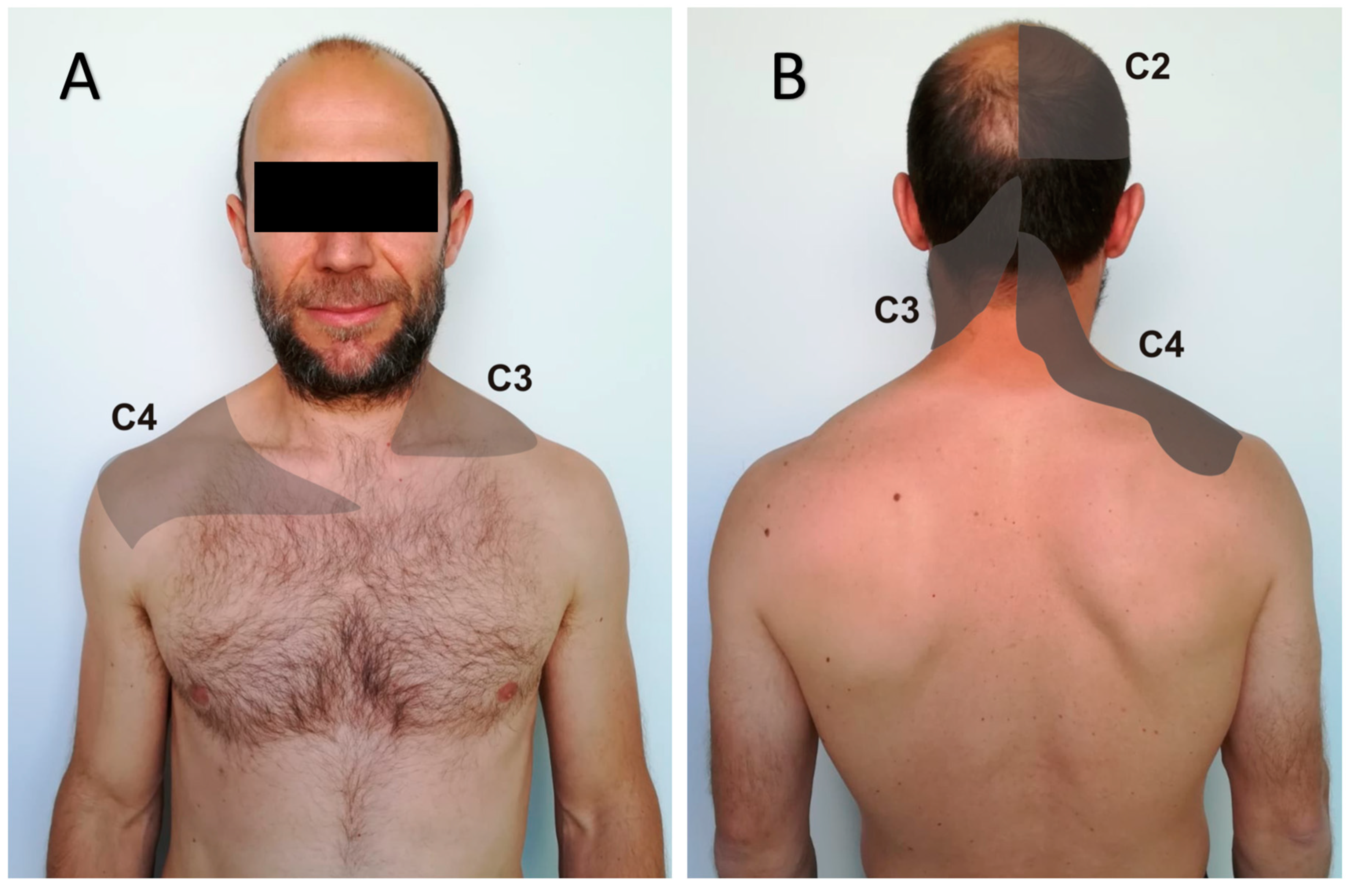
Understanding and awareness of referred pain is key for a precise diagnosis of the pain source [14]. Previous evidence shows that gastrointestinal, biliary, renal, hepatic, heart, and pulmonary disorders may evoke referred pain to the upper quadrant of the body, including the neck region [15]. The discrimination between visceral and somatic sources of pain is not always evident, and if it is not achieved, it may lead to extensive diagnostic procedures and ineffective treatment approaches [16]. Visceral disorders may evoke referred altered sensitivity, e.g., hyperalgesia or allodynia [17]. For instance, the radiation of pain to the neck and/or upper extremity that occurs during acute coronary syndromes [18] is experienced in more than 65% of cases [19]. Eighty-eight percent of patients with colonoscopy-induced splenic injury complain of pain along the C3–C4 dermatomes due to irritation of the diaphragm or distention of the splenic capsule [20] (Figure 1) [21]. That happens during attempts at sheath insertion into the right or middle hepatic vein in liver biopsy as well [22]. Further, it can also be caused by more common, frequently long-lasting, and not so life-threatening conditions, such as hiatal hernias and gastroesophageal reflux disease [23].
Figure 1.
Pattern of visceral referred pain along the C2–C3–C4 dermatomes. (A) Anterior view; (B) posterior view.
When routinely evaluating patients with NP, it is easy to miss manifestations of an underlying disease, and misdiagnose neck disorders of visceral origin [15,24]. Clinical practice guidelines for the management of NP recommend a detailed physical examination to rule out the possibility of VRP in individuals with NP [25]. Hence, clinical trials assessing treatment efficacy in NP should exclude participants with suspected VRP after a comprehensive evaluation. Otherwise, this selection bias would show an underconsideration of that source of NP, and in addition, result in a likely incorrect estimation of the treatment’s effect size. Therefore, the aim of the systematic review was to investigate to what extent the top 15 most cited and the 15 most recent clinical trials published in high impact journals, by November 2018, that assessed treatment outcomes in patients with NP, took into account VRP when establishing their eligibility criteria.
2. Materials and Methods
The present systematic review was performed according to the Preferred Reporting Item for Systematic Reviews and Meta-Analyses extension for Scoping Reviews guidelines [26]. It has been registered in the International Prospective Register of Systematic Reviews (PROSPERO), with registration number CRD42018101987.
2.1. Data Sources and Search Strategy
One author (C.G.-G.) conducted a systematic computerized search between November and December 2018 using the Web of Science database. The search used the key terms neck pain and trial, and considered the following limitations: both key terms being included in the title of the article; language—English/Spanish/Italian/French; and having a publication date between January 1995 and November 2018.
2.2. Study Selection
In order to obtain the information from high-quality studies, eligible articles were the top 15 most cited clinical trials published between 1995 and 2018, and the 15 most recent studies included in high impact journals (first quartile of the Journal Citation Reports in the year of publication of the study), which assessed any therapy for subjects suffering from NP. Those articles with any of the following characteristics were excluded: NP patients with only a traumatic, surgical, or neurological origin for the condition; study protocols for clinical trials; studies including only elderly adults (older than 65 years), or including adolescents or children (younger than 18 years); or a lack of a clear description of the eligibility criteria. All relevant titles were saved in a reference manager (EndNote®, version X8.2, Thomson Reuters). Two researchers (C.G.-G. and Á.O.-P.-V.) independently performed the assessment of the studies in a blinded and standardized manner, taking into account the eligibility criteria previously set out. In the case of a disagreement, the issue was discussed together with a third member of the research team (A.M.H.-R.) until a final consensus was reached.
2.3. Assessment of the Methodological Quality
The Physiotherapy Evidence Database (PEDro) scale score was used to assess the methodological quality of the clinical trials. The PEDro scale is an 11-item tool where items are scored as either absent (0) or present (1), except for item 1 that refers to external validity of the study. A final score from 0 to 10 is given. The PEDro scale is a valid [27] and reliable [28] tool to rate the methodological quality of clinical trials. A cut-off of at least 5 or 6 points is required for a study to be of adequate quality [29]. PEDro scores were extracted from the PEDro database. Two independent raters (J.C.F.-D. and A.F.-G.) evaluated, with the PEDro scale, those trials not included in the PEDro database. A final consensus about the final score was reached, together with a third member of the research team (A.M.H.-R.), whenever necessary.
2.4. Data Extraction
Once the studies were selected, two authors (C.G.-G. and J.O.-P.-V.) independently retrieved the following information from each article following a standardized form: the number of authors affiliated with a clinical institution, e.g., hospital, private practice, or health-center, and the number affiliated with a non-clinical institution, e.g., a university or research center; total number of citations in the Web of Science; the PEDro scale score; aims of the study; sample size and characteristics of participants (distribution by sex, mean age and pain duration); and eligibility criteria (inclusion and exclusion criteria). Data collected from the studies we included were pooled into tables.
3. Results
3.1. Study Selection
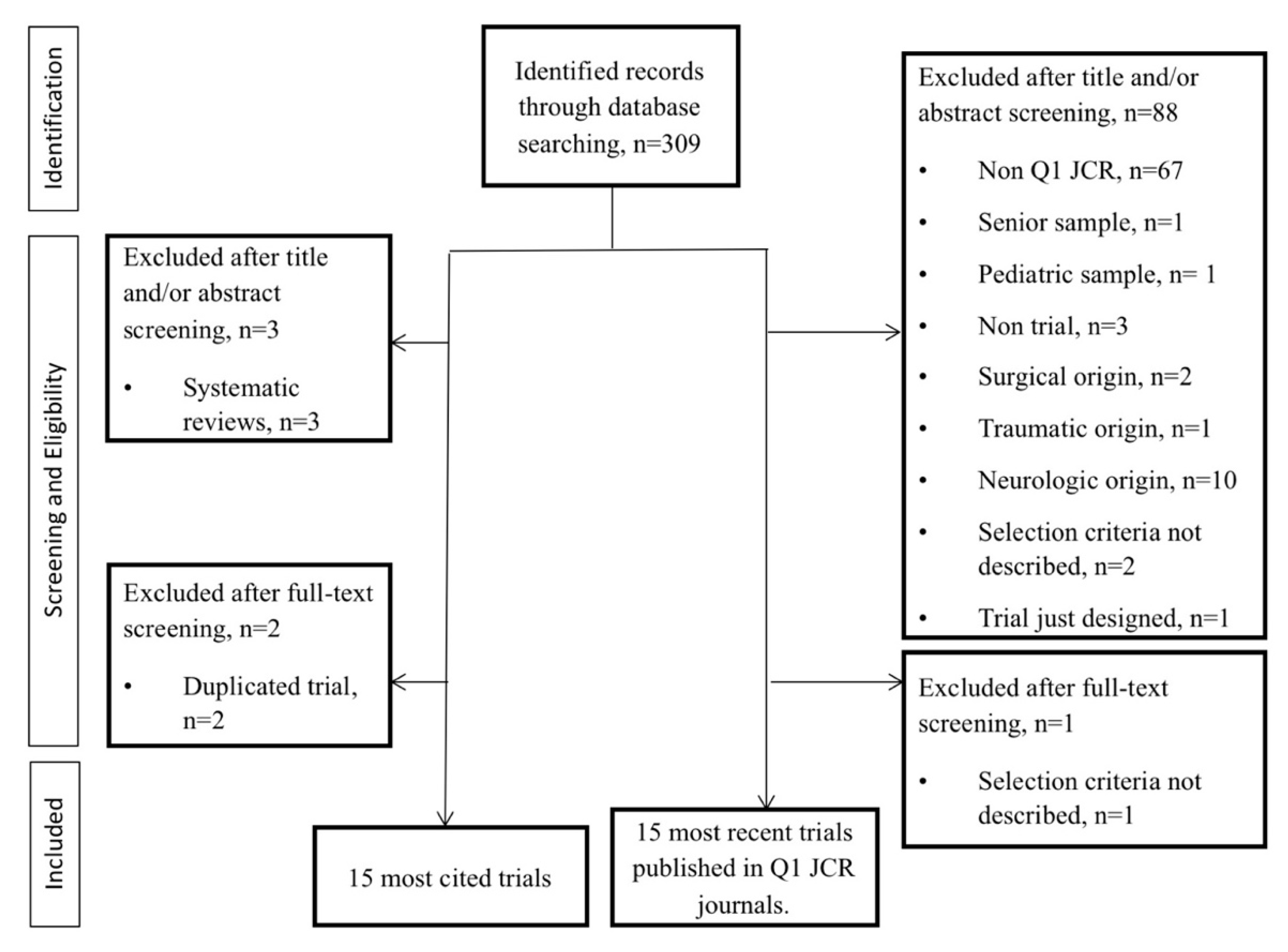
The search strategy resulted in a total of 309 relevant articles that were retrieved through the Web of Science database. Then, 94 studies were excluded for not matching the eligibility criteria. From the remaining 215 articles, 30 of them were finally included. All selected studies were written in English. Two of the top 15 most cited articles were excluded and replaced by the next most cited clinical trials in the list. The reason was that the sample population and the eligibility criteria used were the same as in other studies with a higher number of citations that were published by the same research groups and that had been already included for further analysis. Figure 2 shows the flow diagram for the study selection process.
Figure 2.
Flowchart diagram of the study selection process (Preferred Reporting Item for Systematic Reviews and Meta-Analyses, PRISMA, guidelines). Q1, first quartile; JCR, Journal Citation Reports.
3.2. Study Characteristics
All of the clinical trials which were included were randomized and controlled. Detailed descriptions of articles included in this systematic review are presented in Table 1; Table 2. Researchers from non-clinical institutions authored more than 90% of the studies (28 out of 30), while authors from clinical institutions, e.g., hospitals, health-centers, and private practices, participated in 79% of trials (21 out of 30). The studies included a total of 4467 participants, with females representing 67.5% of the total (3017 females). One clinical trial did not clearly specify the sex distribution of the study sample [30]. Two studies recruited exclusively females [31,32], and only two of them selected more male than female individuals [33,34]. The mean age of participants was between 35 and 53 years, with one study including younger participants (mean age of 21 years) [35].

Table 1.
Top 15 most cited clinical trials about treatment efficacy in neck pain published between 1995 and 2018. NP, neck pain; Clinical, number of authors belonging to clinical institutions; Non-Clinical, number of authors belonging to academic institutions; SM, spinal manipulation; PT, physical therapy; GP, general practitioner.

Table 2.
List of the fifteen most recent clinical trials, by November 2018, about treatment efficacy in neck pain published in high impact journals. NP, neck pain; Clinical, number of authors belonging to clinical institutions; Non-Clinical, number of authors belonging to academic institutions; NDI, neck disability index; PT, physical therapy; VAS, visual analogue scale; SM, spinal manipulation; N/S, non-clearly specified.
3.3. Methodological Quality of Studies
The assessment of the methodological quality by means of the PEDro scale revealed that, in general, the top 15 most cited clinical trials denoted adequate to good methodological quality, with a final score of six points or higher, except for one study that scored five out of 10 points (Table 1) [36]. Similar findings were observed amongst the 15 most recent articles published in high impact journals (Table 2), although one study denoted poor methodological quality (four out of 10) [37]. One of all studies included achieved excellent methodological quality (10 out of 10) [38]. The reliability between coders for those studies whose scores were not available in the PEDro database was almost perfect (Kappa = 0.84) [39].
3.4. Eligibility Criteria (Inclusion and Exclusion Criteria) Used by Trials
Of all trials analyzed, a single study [38] defined stringent inclusion criteria to avoid the recruitment of participants with possible VRP. This study included patients with a positive response to cervical facet joint nerve blockers; e.g., 80% pain relief and the ability to perform previously painful movements. With regard to the exclusion criteria, five clinical trials listed them to avoid the selection of individuals with suspected VRP as the cause of their NP. Two studies explicitly excluded participants with “NP referred from peripheral joints or viscera” [47,50]. The other three studies excluded individuals who suffered from NP with a “non-mechanical cause” [45], reported “any medical sign suggestive of a non-musculoskeletal aetiology” for their NP [43], or were diagnosed with a “specific cause for the neck pain”; e.g., organic disorders or systemic diseases [48]. A “clear aetiology” [57] or a “specific cause” [57,58] for the NP was also listed as an exclusion criterion in three other trials. Yet, none of the latter studies mentioned visceral or organic disorders as possible specific causes for the NP. Some other visceral sources of NP were enumerated in other clinical trials: (a) hepatitis [37]; (b) systemic disorders, including metabolic disease [30,35,36,41,46,57,58]; (c) abuse of alcohol and drugs [37,54]; (d) rheumatic disease [31,32,33,35,37,46,49,51,52,53,55,56,58]; (e) cancer [30,31,35,37,42,51,52,53,55,56,57]; (f) HIV [37]; and (g) infection [30,33,34,40,45,47,57]. Pregnancy was also included as exclusion criteria in almost half of the trials [30,32,34,37,38,40,46,50,51,52,54,55,56,59]. Two clinical trials did not refer to any possible visceral aetiology of neck pain in their inclusion and exclusion criteria [44,60].
4. Discussion
The present findings suggest that amongst the most cited and the most recently published clinical trials assessing treatment efficacy in NP there is a lack of consideration for VRP as a plausible source of NP. This appears to be the case when the eligibility criteria for recruiting participants are analyzed. Only 20% of all selected trials (six out of 30) defined stringent enough criteria to avoid the recruitment of individuals with a suspected visceral referred NP. All these studies were amongst the top 15 most cited articles. Three other trials excluded patients with a specific aetiology or cause for their NP, although authors did not even mention the visceral area. This implies that most of the assessed trials might have included patients with a visceral source of NP despite the fact that the visceral disorder would not be the target of the treatment. Therefore, it might show an underconsideration of this neck pain aetiology; in addition, incorrect estimations of the effects or efficacies of the interventions could have occurred.
4.1. Eligibility Criteria Used by Trials to Select NP Patients
Manchikanti et al. [38] considered as eligible, those patients with a positive response to cervical facet joint nerve blockers, which excluded individuals with visceral referred NP. The rest of the clinical trials, however, established general inclusion criteria; e.g., neck stiffness; mechanical pain with reproducibility of symptoms during physical examination, neck movement, or posture maintenance; and myofascial pain syndrome, among others. All these symptoms mainly refer to increased local sensitization and muscle tension, which can be due to a visceral issue. A primary visceral disorder may also be accompanied by hyperalgesia of the painful area, and is often associated with sustained muscle contraction [61], and it may extend to subcutaneous tissues when the visceral disorder is persistent [62]. Furthermore, the increased muscle tone may explain mechanical symptoms and lead, in the long-term, to the presence of myofascial trigger points and myofascial pain syndrome [63,64]. Hence, visceral pain can evoke many different neck symptoms, including muscle spasms in addition to pain [15], and when sustained, may help to develop central sensitization and cortical changes [61]. Despite all this, surprisingly, the visceral aetiology of NP was only properly considered in six clinical trials [38,43,45,47,48,50]. These findings may imply a general misdiagnosis of NP in research and clinical scopes, thus patients with visceral referred NP might not receive the most accurate therapeutic approach. Visceral pain shares many features with pain from deep somatic structures and requires well-developed propedeutics to avoid inadequate diagnosis and treatment [65]. The test for cutaneous allodynia appears to have the greatest likelihood of identifying a visceral source of pain compared to somatic sources of pain [16]. Therefore, a detailed clinical history, physical examination, and supplemental laboratory and imaging examination is needed to diagnose the primary source of pain [61,64], because the somatic manifestation will persist until the visceral disorder resolves by itself or has been discovered and treated [23,66]. This discovery is more likely to happen in subjects with constant neck pain and/or aggravation of visceral symptoms, but is less likely in recurrent, episodic NP and/or subtle visceral symptoms [15]. Additionally, in cases of chronic NP, the right diagnosis can be favored along the course of the disease by the obtaining of abnormalities in blood, urine, digestive, heart… tests, either developed ad hoc to diagnose the origin of NP or during medical assessments for other reasons. Since many of the visceral disorders which may trigger NP are chronic, they enable the presence of either episodic (due to episodic aggravation of the visceral disorder), recurrent (due to frequent aggravation of the visceral disorder), or chronic NP.
4.2. Somatic Consequences of Visceral Disorders
Visceral referred NP is linked to the involvement of the vagus and/or phrenic nerves. The nociceptive input from any of the organs innervated by the vagus nerve sensitizes the trigeminocervical nuclear complex that descends to C3 or C4 levels, and may trigger a headache [67] and/or NP [14]. The phrenic nerve is a motor and sensitive nerve formed by C3–C4 roots, with C5 as an accessory root. Either directly or through celiac connections, it supplies the diaphragm, pleura, right atrium [68] pericardium [68,69], esophagus [70], peritoneum [68,71], stomach [15], falciform and coronary ligaments of the liver [72], the Glisson capsule [72,73], the hepatic vein [74], the inferior vena cava [68,70,74], the liver [68,72,75] (parenchyma) [74], the gallbladder [72,76,77] and the rest of the biliary tract [71,72,77]—including the duodenal papilla and the sphincter of Oddi [77,78] —, the pancreas [15], the small intestine [15], and the suprarenal glands [68,70,71]. Hence, disorders of many of these structures, such as the pancreas, or even the spleen or kidneys, can evoke referred pain along the C3–C4 dermatomes either due to the autonomic connections, diaphragmatic pressure, or peritoneal irritation [15]. This has been described as “phrenic pain” [23].
To date, there is no data about the prevalence of NP of visceral origin in general practice or musculoskeletal settings. Nevertheless, in a previous study [79] that seemed not to consider the visceral aetiology, a well identified cause of the NP was not found in 32% of patients receiving a complete evaluation in a private pain clinic, where, probably, those NP patients with the most severe symptoms are a majority. As well, a history of previous trauma was present in most of the patients. However, the authors do not clarify if the inability to achieve a specific cause was more frequent in patients who had previous trauma or in those who did not.
It is important to consider the prevalence of the causes of any condition, because that determines the pretest probability, the order of the investigations, and it can also affect to prognosis. The prevalence of visceral disorders that may trigger pain in the neck-shoulder area is high. It is estimated that the one-year prevalence of gastroesophageal reflux with weekly symptoms is 14% [80], and 15% of Americans have silent gallstones, 10–18% of whom develop biliary pain [81]. Besides, non-alcoholic fatty liver is present in around 30% of the population in western countries [82]. Females are more prone than males to have widespread hyperalgesia from recurrent visceral pain [61], and also NP is more prevalent in females. Further, NP of high intensity/low disability or high disability is strongly related to cardiovascular and digestive disorders [83]. That may suggest, eventually, a visceral origin for the pain, which together with cervical spasms have been observed in animal models [84] and in humans [23] with gastric or esophageal disorders. It is also known that NP is highly associated with obesity [85], LDL cholesterol [86], and metabolic syndrome [87]. For instance, the prevalence of NP in those with metabolic syndrome ranges between 16% for males and 25% for females [87]. This is remarkably important because fatty liver, obesity, and metabolic syndromes entail hepatic suffering; e.g., increased pressure, swelling, and hepatomegaly. Phrenic afferents in the hepatic parenchyma, hepatic veins, and the inferior vena cava just need light pressure to respond [74,88]. Further, all this can stretch and sensitize the Glisson capsule, which is known to evoke phrenic pain [72]. However, most patients do not relate their NP and the concomitant visceral disorder, or fail to report gastrointestinal or hepatic/biliary symptoms [15], which contributes to the misdiagnosis of NP as mechanical or non-specific.
It is interesting to note that experimental research of gastric sensitivity is performed in rats by means of gastric distension, which is very common in obesity, and is related to dyspepsia. This gastric distension triggers an increase in the electromyographic activity of the neck muscles and also affects to the neck posture [89]. The addition of substances which increase the insult to the stomach enhances this visceromotor response [84]. The same mechanisms have been used to experimentally study the gastric hypersensitivity frequently observed in patients with long-standing diabetes [90]. The increase of muscle tone in the area of referred hyperalgesia does not appear only when the stomach is injured, since it has also been demonstrated by artificial ureteric stones [91]. Moreover, the neck muscles’ tone decreased in these models when the viscera was treated by means of electrical stimulation [92,93]. Likewise, manual visceral treatment has also been shown to improve NP and electromyographic recordings of the upper trapezius muscles of subjects suffering from chronic non-specific NP and dyspepsia [94], and has improved neck mobility and NP thresholds in subjects suffering from gastroesophageal reflux disease [95]. On the contrary, the likely participation of patients with NP of visceral origin might contribute to explaining the scarce success of usual treatments for NP, achieving at most moderate effects in the short-term [96].
Therefore, the visceral origin of NP might be more easily diagnosed if it only triggers VRP, because there will be no modification of pain related to activity or posture. However, as previously exposed, mechanical consequences can be also elicited in case of visceral aetiology of NP [15,24,61,63,64,66,84,89,90,91,92,93], hindering the correct diagnosis. The presence of muscle hypertonus, myofascial trigger points, and/or myofascial pain syndrome may increase symptoms during musculoskeletal activity. Similarly, pain modification related to movement and/or postures has also been described during the affectation of the spleen [97], gallbladder [72,98], kidney [99,100], and heart [15,101].
4.3. Needs for the Future
Our results suggest that clinical trials about NP fail to suspect a visceral origin of NP. This poor consideration seems to be shared in the research and clinical settings, considering that authors from clinical institutions participated in nearly 80% of the studies reviewed. Thus, our study points out the need to further develop the knowledge of somatic consequences of visceral disorders, at least when related to NP. Additionally, it shows the need for more research to get to know the prevalence of NP of visceral origin in different settings (primary care, clinics of rehabilitation, chiropractic, osteopathy, and physiotherapy).
4.4. Limitations
The present findings should be carefully interpreted for several reasons. First, the search strategy was conducted in a single database. The aim was to select those trials with higher impacts, based on the number of citations or on the publication in first quartile journals of the Journal Citation Reports. This strategy was set in order to select those trials which could be representative of the best research about neck pain; i.e., the most cited (showing that they are used as a reference by many researchers) and those published in the best quality journals (which are supposed to publish the best studies). The Web of Science database provides the number of citations and the quartile, and it is considered of high prestige in the Health Sciences field. Other databases such as Medline do not provide numbers of citations nor journal impact factors. Other reviews used different strategies to show a general overview about a subject, such as random selection of studies and/or selection of specific major journals [102,103,104,105]. Second, with respect to sample size, it could be argued that our sample size (30 studies) is not big enough to be representative. The right sample size to perform this kind of study has not been established. In the literature, systematic reviews about research bias can be found with sample sizes ranging between 10 and 44 studies [106,107,108,109,110,111]. Third, despite the high prevalence of visceral disorders, it is not possible to conclude that these studies actually included patients with VRP to the neck area. Therefore, the influence of this issue on the results of each trial remains unknown.
5. Conclusions
In conclusion, it seems that most of the top cited and most recent clinical trials assessing treatments in NP lacked the consideration of visceral referred NP according to their eligibility criteria, showing that neck pain of visceral origin is underestimated. Although NP referred from viscera is difficult to diagnose, more stringent inclusion and exclusion criteria may be required in clinical trials. Otherwise, this may imply an incorrect estimation of the usefulness of the interventions.
Author Contributions
Conceptualization, Á.O.-P.-V. and F.P.-P.; methodology, J.C.F.-D. and A.M.H.-R.; formal analysis, C.G.-G. and A.F.-G.; investigation, C.G.-G., A.F.-G., J.C.F.-D., J.O.-P.-V., Á.O.-P.-V., and A.M.H.-R.; data curation, C.G.-G.; writing—original draft preparation, Á.O.-P.-V. and A.M.H.-R.; writing—review and editing, F.P.-P. and J.O.-P.-V.; supervision, Á.O.-P.-V.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hoy, D.G.; Protani, M.; De, R.; Buchbinder, R. The epidemiology of neck pain. Best Pract. Res. Clin. Rheumatol. 2010, 24, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Hoy, D.; March, L.; Woolf, A.; Blyth, F.; Brooks, P.; Smith, E.; Vos, T.; Barendregt, J.; Blore, J.; Murray, C.; et al. The global burden of neck pain: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Driessen, M.T.; Lin, C.W.; van Tulder, M.W. Cost-effectiveness of conservative treatments for neck pain: A systematic review on economic evaluations. Eur. Spine J. 2012, 21, 1441–1450. [Google Scholar] [CrossRef] [PubMed]
- Bono, C.M.; Ghiselli, G.; Gilbert, T.J.; Kreiner, D.D.; Reitman, C.; Summers, J.T.; Baisden, J.T.; Easa, J.; Fernand, R.; Lamer, T.; et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 2011, 11, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Kjaer, P.; Kongsted, A.; Hartvigsen, J.; Isenberg-Jorgensen, A.; Schiottz-Christensen, B.; Soborg, B.; Krog, C.; Moller, C.M.; Halling, C.M.B.; Lauridsen, H.H.; et al. National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy. Eur. Spine J. 2017, 26, 2242–2257. [Google Scholar] [CrossRef] [PubMed]
- Falco, F.J.; Erhart, S.; Wargo, B.W.; Bryce, D.A.; Atluri, S.; Datta, S.; Hayek, S.M. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician 2009, 12, 323–344. [Google Scholar] [PubMed]
- Ambrose, N.L.; Cunnane, G. Importance of full evaluation in patients who complain of neck pain. Ir. J. Med. Sci. 2009, 178, 209–210. [Google Scholar] [CrossRef] [PubMed]
- Childs, J.D.; Cleland, J.A.; Elliott, J.M.; Teyhen, D.S.; Wainner, R.S.; Whitman, J.M.; Sopky, B.J.; Godges, J.J.; Flynn, T.W. Neck pain: Clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2008, 38, A1–A34. [Google Scholar] [CrossRef] [PubMed]
- Giamberardino, M.A.; Costantini, R.; Affaitati, G.; Fabrizio, A.; Lapenna, D.; Tafuri, E.; Mezzetti, A. Viscero-visceral hyperalgesia: Characterization in different clinical models. Pain 2010, 151, 307–322. [Google Scholar] [CrossRef] [PubMed]
- Giamberardino, M.; Affaitati, G.; Costantini, R. Visceral referred pain. J. Musculoskelet. Pain 2010, 18, 403–410. [Google Scholar] [CrossRef]
- Ruch, T.; Patton, H. Pathophysiology of Pain: Physiology and Biophysics; Saunders: Philadelpia, PA, USA, 1965. [Google Scholar]
- Luz, L.L.; Fernandes, E.C.; Sivado, M.; Kokai, E.; Szucs, P.; Safronov, B.V. Monosynaptic convergence of somatic and visceral C-fiber afferents on projection and local circuit neurons in lamina I: A substrate for referred pain. Pain 2015, 156, 2042–2051. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.D.; Russell, A.; Hodges, P.W. How common is back pain in women with gastrointestinal problems? Clin. J. Pain 2008, 24, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.G.; Chang, M.C. Neck-to-shoulder pain as an unusual presentation of pulmonary embolism in a patient with cervical spinal cord injury: A case report. Medicine 2017, 96, e8288. [Google Scholar] [CrossRef] [PubMed]
- Goodman, C.C. Screening for gastrointestinal, hepatic/biliary, and renal/urologic disease. J. Hand Ther. 2010, 23, 140–156. [Google Scholar] [CrossRef] [PubMed]
- Jarrell, J.; Giamberardino, M.A.; Robert, M.; Nasr-Esfahani, M. Bedside testing for chronic pelvic pain: Discriminating visceral from somatic pain. Pain Res. Treat. 2011, 2011, 692102. [Google Scholar] [CrossRef] [PubMed]
- Head, H. On disturbances of sensation with especial reference to the pain of visceral disease. Brain 1893, 16, 1–133. [Google Scholar] [CrossRef]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; Casey, D.E.; Ganiats, T.G.; Holmes, D.R.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.; et al. 2014 AHA/ACC Guideline for the management of patients with non-st-elevation acute coronary syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 64, e139–e228. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; James, D.; Petrie, K.; Weinman, J.; Vincent, R. Patients’ interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart 2000, 83, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Saad, A.; Rex, D.K. Colonoscopy-induced splenic injury: Report of 3 cases and literature review. Dig. Dis. Sci. 2008, 53, 892–898. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.W.L.; McPhee, R.W.; Stringer, M.D. An evidence-based approach to human dermatomes. Clin. Anat. 2008, 21, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Khosa, F.; McNulty, J.G.; Hickey, N.; O’Brien, P.; Tobin, A.; Noonan, N.; Ryan, B.; Keeling, P.W.; Kelleher, D.P.; McDonald, G.S. Transvenous liver biopsy via the femoral vein. Clin. Radiol. 2003, 58, 487–491. [Google Scholar] [CrossRef]
- Flanagin, B.A.; Mitchell, M.T.; Thistlethwaite, W.A.; Alverdy, J.C. Diagnosis and treatment of atypical presentations of hiatal hernia following bariatric surgery. Obes. Surg. 2010, 20, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Lehwald, N.; Krausch, M.; Franke, C.; Assmann, B.; Adam, R.; Knoefel, W.T. Sandifer syndrome: A multidisciplinary diagnostic and therapeutic challenge. Eur. J. Pediatr. Surg. 2007, 17, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Iovine, R.; de Sena, G.; Rovere, G.; Uliano, D.; Arioli, G.; Bonaiuti, D.; Brugnoni, G.; Ceravolo, G.; Cerri, C.; et al. The Italian Society of Physical and Rehabilitation Medicine (SIMFER) recommendations for neck pain. G. Ital. Med. Lav. Ergon. 2013, 35, 36–50. [Google Scholar] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O´Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Int. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [PubMed]
- Armijo-Olivo, S.; da Costa, B.R.; Cummings, G.G.; Ha, C.; Fuentes, J.; Saltaji, H.; Egger, M. PEDro or Cochrane to assess the quality of clinical trials? A Meta-Epidemiological Study. PLoS ONE 2015, 10, e0132634. [Google Scholar] [CrossRef] [PubMed]
- Cerezo-Téllez, E.; Torres-Lacomba, M.; Fuentes-Gallardo, I.; Perez-Munoz, M.; Mayoral-del-Moral, O.; Lluch-Girbes, E.; Prieto-Valiente, L.; Falla, D. Effectiveness of dry needling for chronic nonspecific neck pain: A randomized, single-blinded, clinical trial. Pain 2016, 157, 1905–1917. [Google Scholar] [CrossRef] [PubMed]
- Viljanen, M.; Malmivaara, A.; Uitti, J.; Rinne, M.; Palmroos, R.; Laippala, P. Effectiveness of dynamic muscle training, relaxation training, or ordinary activity for chronic neck pain: Randomised controlled trial. BMJ 2003, 327, 475. [Google Scholar] [CrossRef] [PubMed]
- Ylinen, J.; Takala, E.P.; Nykänen, M.; hakkinen, A.; Malkia, E.; Pohjolainen, T.; Karppi, S.-L.; Kautiainen, H.; Airaksinen, O. Active neck muscle training in the treatment of chronic neck pain in women: A randomized controlled trial. JAMA 2003, 289, 2509–2516. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.P.; Oldham, J.A.; Woby, S.R. Does adding cognitive-behavioural physiotherapy to exercise improve outcome in patients with chronic neck pain? A randomised controlled trial. Physiotherapy 2016, 102, 170–177. [Google Scholar] [CrossRef] [PubMed]
- De Araujo Cazotti, L.; Jones, A.; Roger-Silva, D.; Ribeiro, L.H.C.; Natour, J. Effectiveness of the Pilates method in the treatment of chronic mechanical neck pain: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2018, 99, 1740–1746. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Carnero, J.; Sierra-Silvestre, E.; Beltran-Alacreu, H.; Gil-Martinez, A.; La Touche, R. Neural tension technique improves immediate conditioned pain modulation in patients with chronic neck pain: A randomized clinical trial. Pain Med. 2019, 20, 1227–1235. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; Bendix, T.; Nielsen, H.; Hansen, F.R.; Host, D.; Winkel, A. Intensive training, physiotherapy, or manipulation for patients with chronic neck pain. A prospective, single-blinded, randomized clinical trial. Spine 1998, 23, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Essex, H.; Parrott, S.; Atkin, K.; Ballard, K.; Blanda, M.; Eldred, J.; Hewitt, C.; Hopton, A.; Keding, A.; Lansdown, H.; et al. An economic evaluation of Alexander Technique lessons or acupuncture sessions for patients with chronic neck pain: A randomized trial (ATLAS). PLoS ONE 2017, 12, e0178918. [Google Scholar] [CrossRef] [PubMed]
- Manchikanti, L.; Singh, V.; Falco, F.J.; Cash, K.A.; Fellows, B. Comparative outcomes of a 2-year follow-up of cervical medial branch blocks in management of chronic neck pain: A randomized, double-blind controlled trial. Pain Physician 2010, 13, 437–450. [Google Scholar] [PubMed]
- Viera, A.J.; Garrett, J.M. Understanding interobserver agreement: The kappa statistic. Fam. Med. 2005, 37, 360–363. [Google Scholar] [PubMed]
- Cleland, J.A.; Childs, J.D.; McRae, M.; palmer, J.A.; Stowell, T. Immediate effects of thoracic manipulation in patients with neck pain: A randomized clinical trial. Man. Ther. 2005, 10, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Irnich, D.; Behrens, N.; Molzen, H.; Konig, A.; Gleditsch, J.; Krauss, M.; Natalis, M.; Senn, E.; Beyer, A.; Schops, P. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ 2001, 322, 1574–1578. [Google Scholar] [CrossRef] [PubMed]
- Korthals-de Bos, I.B.; Hoving, J.L.; van Tulder, M.W.; Rutten-van-Molken, M.P.M.H.; Ader, H.J.; de Vet, H.C.M.; Koes, B.W.; Vondeling, H.; Bouter, L.M. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: Economic evaluation alongside a randomised controlled trial. BMJ 2003, 326, 911. [Google Scholar] [PubMed]
- Cleland, J.A.; Glynn, P.; Whitman, J.M.; Eberhart, S.L.; MacDonald, C.; Childs, J.D. Short-term effects of thrust versus nonthrust mobilization/manipulation directed at the thoracic spine in patients with neck pain: A randomized clinical trial. Phys. Ther. 2007, 87, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Irnich, D.; Behrens, N.; Gleditsch, J.M.; Stor, W.; Schreiber, M.A.; Schops, P.; Vickers, A.J.; Beyer, A. Immediate effects of dry needling and acupuncture at distant points in chronic neck pain: Results of a randomized, double-blind, sham-controlled crossover trial. Pain 2002, 99, 83–89. [Google Scholar] [CrossRef]
- Hurwitz, E.L.; Morgenstern, H.; Harber, P.; Koniski, G.F.; Yu, F.; Adams, A.H. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: Clinical outcomes from the UCLA neck-pain study. Am. J. Public Health 2002, 92, 1634–1641. [Google Scholar] [CrossRef] [PubMed]
- White, P.; Lewith, G.; Prescott, P.; Conway, J. Acupuncture versus placebo for the treatment of chronic mechanical neck pain: A randomized, controlled trial. Ann. Intern. Med. 2004, 141, 911–919. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.; Bronfort, G.; Nelson, B.; Goldsmith, C.H. Two-year follow-up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine 2002, 27, 2383–2389. [Google Scholar] [CrossRef] [PubMed]
- Hoving, J.L.; de Vet, H.C.; Koes, B.W.; van Mameren, H.; Deville, W.L.J.M.; van der Windt, D.A.W.M.; Assendelft, W.J.J.; Pool, J.J.M.; Scholten, R.J.P.M.; Korthals-deBos, I.B.C.; et al. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: Long-term results from a pragmatic randomized clinical trial. Clin. J. Pain 2006, 22, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.T.; Lam, T.H.; Hedley, A.J. A randomized controlled trial on the efficacy of exercise for patients with chronic neck pain. Spine 2005, 30, E1–E7. [Google Scholar] [CrossRef] [PubMed]
- Bronfort, G.; Evans, R.; Anderson, A.V.; Svendsen, K.H.; Bracha, Y.; Grimm, R.H. Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: A randomized trial. Ann. Intern. Med. 2012, 156, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Celenay, S.T.; Kaya, D.O.; Akbayrak, T. Cervical and scapulothoracic stabilization exercises with and without connective tissue massage for chronic mechanical neck pain: A prospective, randomised controlled trial. Man. Ther. 2016, 21, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Celenay, S.T.; Akbayrak, T.; Kaya, D.O. A comparison of the effects of stabilization exercises plus manual therapy to those of stabilization exercises alone in patients with nonspecific mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2016, 46, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Griswold, D.; Learman, K.; Kolber, M.J.; O’Halloran, B.; Cleland, J.A. Pragmatically applied cervical and thoracic nonthrust manipulation versus thrust manipulation for patients with mechanical neck pain: A multicenter randomized clinical trial. J. Orthop. Sports Phys. Ther. 2018, 48, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Krøll, L.S.; Hammarlund, C.S.; Linde, M.; Gard, G.; Jensen, R.H. The effects of aerobic exercise for persons with migraine and co-existing tension-type headache and neck pain. A randomized, controlled, clinical trial. Cephalalgia 2018, 38, 1805–1816. [Google Scholar] [CrossRef] [PubMed]
- Lauche, R.; Stumpe, C.; Fehr, J.; Cramer, H.; Cheng, Y.W.; Wayne, P.M.; Rampp, T.; Langhorst, J.; Dobos, G. The effects of Tai Chi and neck exercises in the treatment of chronic nonspecific neck pain: A randomized controlled trial. J. Pain. 2016, 17, 1013–1027. [Google Scholar] [CrossRef] [PubMed]
- Lauche, R.; Schuth, M.; Schwickert, M.; Ludtke, R.; Musial, F.; Michalsen, A.; Dobos, G.; Choi, K.E. Efficacy of the Alexander Technique in treating chronic non-specific neck pain: A randomized controlled trial. Clin. Rehabil. 2016, 30, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Ambrosini, E.; Rocca, B.; Cazzaniga, D.; Liquori, V.; Pedrocchi, A.; Vernon, H. Group-based multimodal exercises integrated with cognitive-behavioural therapy improve disability, pain and quality of life of subjects with chronic neck pain: A randomized controlled trial with one-year follow-up. Clin. Rehabil. 2017, 31, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Pillastrini, P.; de Lima E Sá Resende, F.; Banchelli, F.; Burioli, A.; Di CIaccio, E.; Guccione, A.A.; Villafañe, J.H.; Vanti, C. Effectiveness of Global Postural Re-education in patients with chronic nonspecific neck pain: Randomized controlled trial. Phys. Ther. 2016, 96, 1408–1416. [Google Scholar] [CrossRef] [PubMed]
- Ris, I.; Søgaard, K.; Gram, B.; Agerbo, K.; Boyle, E.; Juul-Kristensen, B. Does a combination of physical training, specific exercises and pain education improve health-related quality of life in patients with chronic neck pain? A randomised control trial with a 4-month follow up. Man. Ther. 2016, 26, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Tunwattanapong, P.; Kongkasuwan, R.; Kuptniratsaikul, V. The effectiveness of a neck and shoulder stretching exercise program among office workers with neck pain: A randomized controlled trial. Clin. Rehabil. 2016, 30, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Giamberardino, M.A. Clinical Updates. Visceral Pain. Pain 2005, 12, 1–6. [Google Scholar]
- Giamberardino, M.A. Recent and forgotten aspects of visceral pain. Eur. J. Pain 1999, 3, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Gerwin, R. Myofascial and visceral pain syndromes: Visceral-somatic pain representations. J. Musculoskelet. Pain 2002, 10, 65–75. [Google Scholar] [CrossRef]
- Srbely, J.Z. New trends in the treatment and management of myofascial pain syndrome. Curr. Pain Headache Rep. 2010, 14, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Campos Kraychete, D.; Tesseroli de Siqueira, J.; Batista García, J.; Kimiko Sakata, R.; Sousa, A.M.; de Andrade, D.C.; Mariotto Zakka, T.R.; Jacobsen Teixeira, M. Clinical evidence on visceral pain. Systematic review. Rev. Dor 2017, 18, 65–71. [Google Scholar] [CrossRef]
- Rana, A.Q.; Yousuf, M.S.; Joian, S. A chronic case of adult-onset Sandifer syndrome. Neurol. Sci. 2013, 34, 405–406. [Google Scholar] [CrossRef] [PubMed]
- Han, D.G.; Lee, C.J. Headache associated with visceral disorders is “parasympathetic referred pain”. Med. Hypotheses 2009, 73, 561–563. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.; Bannister, L.; Berry, M. Gray’s Anatomy, 38th ed.; Churchill Livingstone: New York, NY, USA, 1995. [Google Scholar]
- Kostreva, D.R.; Pontus, S.P. Pericardial mechanoreceptors with phrenic afferents. Am. J. Physiol. 1993, 264, H1836–H1846. [Google Scholar] [CrossRef] [PubMed]
- Loukas, M.; Du Plessis, M.; Louis, R.G.; Tubbs, R.S.; Wartmann, C.T.; Apaydin, N. The subdiaphragmatic part of the phrenic nerve—Morphometry and connections to autonomic ganglia. Clin. Anat. 2016, 29, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Rusu, M.C. Considerations on the phrenic ganglia. Ann. Anat. 2006, 188, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Netter, F. Atlas of Human Anatomy; Saunders/Elsevier: Philadelphia, PA, USA, 2011. [Google Scholar]
- Hartmann, H.; Beckh, K. Nerve supply and nervous control of liver function. In Textbook of Clinical Hematology; McIntyre, N., Benhamou, J., Bircher, J., Eds.; Oxford University Press: Oxford, UK, 1992; p. 93. [Google Scholar]
- Kostreva, D.R.; Pontus, S.P. Hepatic vein, hepatic parenchymal, and inferior vena caval mechanoreceptors with phrenic afferents. Am. J. Physiol. 1993, 265, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Misih, S.R.; Bloomston, M. Liver anatomy. Surg. Clin. N. Am. 2010, 90, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Iwahashi, K.; Matsuda, R.; Tsunekawa, K. Afferent innervation of the gallbladder in the cat, studied by the horseradish peroxidase method. J. Auton. Nerv. Syst. 1991, 32, 145–151. [Google Scholar] [CrossRef]
- Yi, S.Q.; Ohta, T.; Tsuchida, A.; Terayama, H.; Naito, M.; Li, J.; Wang, H.X.; Yi, N.; Tanaka, S.; Itoh, M. Surgical anatomy of innervation of the gallbladder in humans and Suncus murinus with special reference to morphological understanding of gallstone formation after gastrectomy. World J. Gastroenterol. 2007, 13, 2066–2071. [Google Scholar] [CrossRef] [PubMed]
- Yi, S.Q.; Ren, K.; Kinoshita, M.; Takano, M.; Itoh, M.; Ozaki, N. Innervation of extrahepatic biliary tract, with special reference to the direct bidirectional neural connections of the gall bladder, sphincter of Oddi and duodenum in Suncus murinus, in whole-mount immunohistochemical study. Anat. Histol. Embryol. 2016, 45, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Yin, W.; Bogduk, N. The nature of neck pain in a private pain clinic in the United States. Pain. Med. 2008, 9, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Eusebi, L.H.; Ratnakumaran, R.; Yuan, Y.; Solaymani-DOdaran, M.; Bazzoli, F.; Ford, A.C. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: A meta-analysis. Gut 2018, 67, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Knab, L.M.; Boller, A.M.; Mahvi, D.M. Cholecystitis. Surg. Clin. N. Am. 2014, 94, 455–470. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, G.; Miglioli, L.; Masutti, F.; Tiribelli, C.; Marchesini, G.; Bellentani, S. Prevalence of and risk factors for nonalcoholic fatty liver disease: The Dionysos nutrition and liver study. Hepatology 2005, 42, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Côté, P.; Cassidy, J.D.; Carroll, L. The factors associated with neck pain and its related disability in the Saskatchewan population. Spine 2000, 25, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Ozaki, N.; Bielefeldt, K.; Sengupta, J.N.; Gebhart, G.F. Models of gastric hyperalgesia in the rat. Am. J. Physiol. Gastrointest. Liver Physiol. 2002, 283, G666–G676. [Google Scholar] [CrossRef] [PubMed]
- Palacios-Ceña, D.; Alonso-Blanco, C.; Hernández-Barrera, V.; Carrasco-Garrido, P.; Jimenez-Garcia, R.; Fernandez-de-las-Penas, C. Prevalence of neck and low back pain in community-dwelling adults in Spain: An updated population-based national study (2009/10–2011/12). Eur. Spine J. 2015, 24, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, G.; Wada, K.; Tanaka, T.; Kudo, H.; Asari, T.; Chiba, D.; Ota, S.; Nakaji, S.; Ishibayi, I. Associations between neck symptoms and LDL cholesterol in a cross-sectional population-based study. J. Orthop. Sci. 2018, 23, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Mäntyselkä, P.; Kautiainen, H.; Vanhala, M. Prevalence of neck pain in subjects with metabolic syndrome: A cross-sectional population-based study. BMC Musculoskelet. Disord. 2010, 11, 171. [Google Scholar] [CrossRef] [PubMed]
- Nair, J.; Streeter, K.A.; Turner, S.M.F.; Sunshine, M.D.; Bolser, D.C.; Fox, E.J.; Davenport, P.W.; Fuller, D.D. Anatomy and physiology of phrenic afferent neurons. J. Neurophysiol. 2017, 118, 2975–2990. [Google Scholar] [CrossRef] [PubMed]
- Rouzade, M.L.; Fioramonti, J.; Bueno, L. A model for evaluation of gastric sensitivity in awake rats. Neurogastroenterol. Motil. 1998, 10, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.H.; Hu, J.; Zhou, Y.L.; Hu, S.F.; Wang, Y.M.; Chen, W.; Xiao, Y.; Huang, L.Y.M.; Jiang, X.H.; Xu, G.Y. Promoted interaction of nuclear factor -kB with demethylated cystathione-β-synthetase gene contributes to gastric hypersensitivity in diabetic rats. J. Neurosci. 2013, 33, 9028–9038. [Google Scholar] [CrossRef] [PubMed]
- Giamberardino, M.A.; Affaitati, G.; Lerza, R.; fano, G.; Fulle, S.; Belia, S.; Lapenna, D.; Vecchiet, L. Evaluation of indices of skeletal muscle contraction in areas of referred hyperalgesia from an artificial ureteric stone in rats. Neurosci. Lett. 2003, 338, 213–216. [Google Scholar] [CrossRef]
- Sun, Y.; Tan, Y.; Song, G. Effects and mechanisms of gastric electrical stimulation on visceral pain in a rodent model of gastric hyperalgesia secondary to chemically induced mucosal ulceration. Neurogastroenterol. Motil. 2014, 26, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Li, S.; Yin, J.; Chen, J.D.Z. Ameliorating effects of optimized gastric electrical stimulation and mechanisms involving nerve growth factor opioids in a rodent model of gastric hypersensitivity. Neurogastroenterol. Motil. 2019, 31, e13551. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.C.O.; Biasotto-Gonzalez, D.A.; Oliveira, F.H.M.; Andrade, A.O.; Gomes, C.A.F.D.; Lanza, F.D.; Amorim, C.F.; Politti, F. Effect of osteopathic visceral manipulation on pain, cervical range of motion, and upper trapezius muscle activity in patients with chronic nonspecific neck pain and functional dispepsia: A randomized, doublé-blind, placebo-controlled pilot study. Evid. Based Complement. Alternat. Med. 2018, 2018, 4929271. [Google Scholar] [CrossRef] [PubMed]
- Eguaras, N.; Rodriguez-Lopez, E.S.; Lopez-Dicastillo, O.; Franco-Sierra, M.A.; Ricard, F.; Oliva-Pascual-Vaca, A. Effects of osteopathic visceral treatment in patients with gastroesophageal reflux: A randomized controlled trial. J. Clin. Med. 2019, 8, 1738. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M.; de Zoete, R.M.J.; Coppieters, I.; Farrell, S.C. Best evidence rehabilitation for chronic pain Part 4: Neck pain. J. Clin. Med. 2019, 8, 1219. [Google Scholar] [CrossRef] [PubMed]
- Sergent, S.R.; Johnson, S.M.; Ashurst, J.; Johnston, G. Epstein-Barr virus associated atraumatic spleen laceration presenting with neck and shoulder pain. Am. J. Case Rep. 2015, 16, 774–777. [Google Scholar] [CrossRef] [PubMed]
- Carter, C.T. Acute thoracolumbar pain due to pholecystitis: A case study. Chiropr. Man. Ther. 2015, 23, 34. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Srirangam, S.J.; Pollard, A.J.; Adeyoju, A.A.; O’Reilly, P.H. Nephroptosis: Seriously misunderstood? Bju Int. 2009, 103, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Hoenig, D.M.; Hemal, A.K.; Shalhav, A.L.; Clayman, R.V. Nephroptosis: A “disparaged” condition revisited. Urology 1999, 54, 590–596. [Google Scholar] [CrossRef]
- Luong, C.; Starovoytov, A.; Heydari, M.; Sedlak, T.; Aymong, E.; Saw, J. Clinical presentation of patients with spontaneous coronary artery dissection. Catheter. Cardiovasc. Interv. 2017, 89, 1149–1154. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Xu, C.; Deng, K.; Zhou, X.; Liu, Z.B.; Busse, J.W.; Ren, Y.; Zou, K.; Sun, X. The reporting of safety among drug systematic reviews was poor before the implementation of the PRISMA harms checklist. J. Clin. Epidemiol. 2019, 105, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Prasad, V.; Gall, V.; Cifu, A. The frequency of medical reversal. Arch. Intern. Med. 2011, 171, 1675–1676. [Google Scholar] [CrossRef] [PubMed]
- Crutzen, R.; Viechtbauer, W.; Spigt, M.; Kotz, D. Differential attrition in health behaviour change trials: A systematic review and meta-analysis. Psychol. Health. 2015, 30, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Mbuagbaw, L.; Thabane, M.; Vanniyasingam, T.; Debono, V.B.; Kosa, S.; Zhang, S.Y.; Ye, C.L.; Parpia, S.; Dennis, B.B.; Thabane, L. Improvement in the quality of abstracts in major clinical journals since CONSORT extension for abstracts: A systematic review. Contemp. Clin. Trials 2014, 38, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Kho, M.E.; Duffet, M.; Willison, D.J.; Cook, D.J.; Brouwers, M.C. Written informed consent and selection bias in observational studies using medical records: Systematic review. BMJ 2009, 338, b866. [Google Scholar] [CrossRef] [PubMed]
- Hrobjartsson, A.; Skou, A.S.; Emanuelsson, F.; Tendal, B.; Hilden, J.; Boutron, I.; Ravaud, P.; Brorson, S. Observer bias in randomised clinical trials with binary outcomes: Systematic review of trials with both blinded and non-blinded outcome assessors. BMJ 2012, 334, e1119. [Google Scholar] [CrossRef] [PubMed]
- Hrobjartsson, A.; Skou, A.S.; Emanuelsson, F.; Tendal, B.; Hilden, J.; Boutron, I.; Ravaud, P.; Brorson, S. Observer bias in randomized clinical trials with measurement scale outcomes: A systematic review of trials with both blinded and nonblinded outcome assessors. CMAJ 2013, 185, E201–E211. [Google Scholar] [CrossRef] [PubMed]
- Grimm, N.L.; Shea, K.G.; Leaver, R.W.; Aoki, S.K.; Carey, J.L. Efficacy and degree of bias in knee injury prevention studies: A systematic review of RCTs. Clin. Orthop. Relat. Res. 2013, 471, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Thaler, K.; Kien, C.; Nussbaumer, B.; Van Noord, M.G.; Griebler, U.; Klerings, I.; Gartlehner, G. Inadequate use and regulation of intervention against publication bias decreases their effectiveness: A systematic review. J. Clin. Epidemiol. 2015, 68, 792–802. [Google Scholar] [CrossRef] [PubMed]
- Farzanfar, D.; Abumuamar, A.; Kim, J.; Sirotich, E.; Wang, Y.; Pullenayegum, E. Longitudinal studies that use data collected as part of usual care risk reporting biased results: A systematic review. BMC Med. Res. Methodol. 2017, 17, 133. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).