Design Decision Support for Healthcare Architecture: A VR-Integrated Approach for Measuring User Perception
Abstract
1. Introduction and Background
1.1. Evidence-Based Design in Healthcare Architecture
1.2. Integrating User Perspectives in Design
1.3. The Traditional Approach to Engaging End-Users Is Limited
1.4. VR as a New Approach for Realistic Virtual Mock-Up with Dynamic Variables
1.5. Building Information Modelling (BIM) and VR as an Approach in EBD for Healthcare Architecture
1.6. Aim
2. Materials and Methods
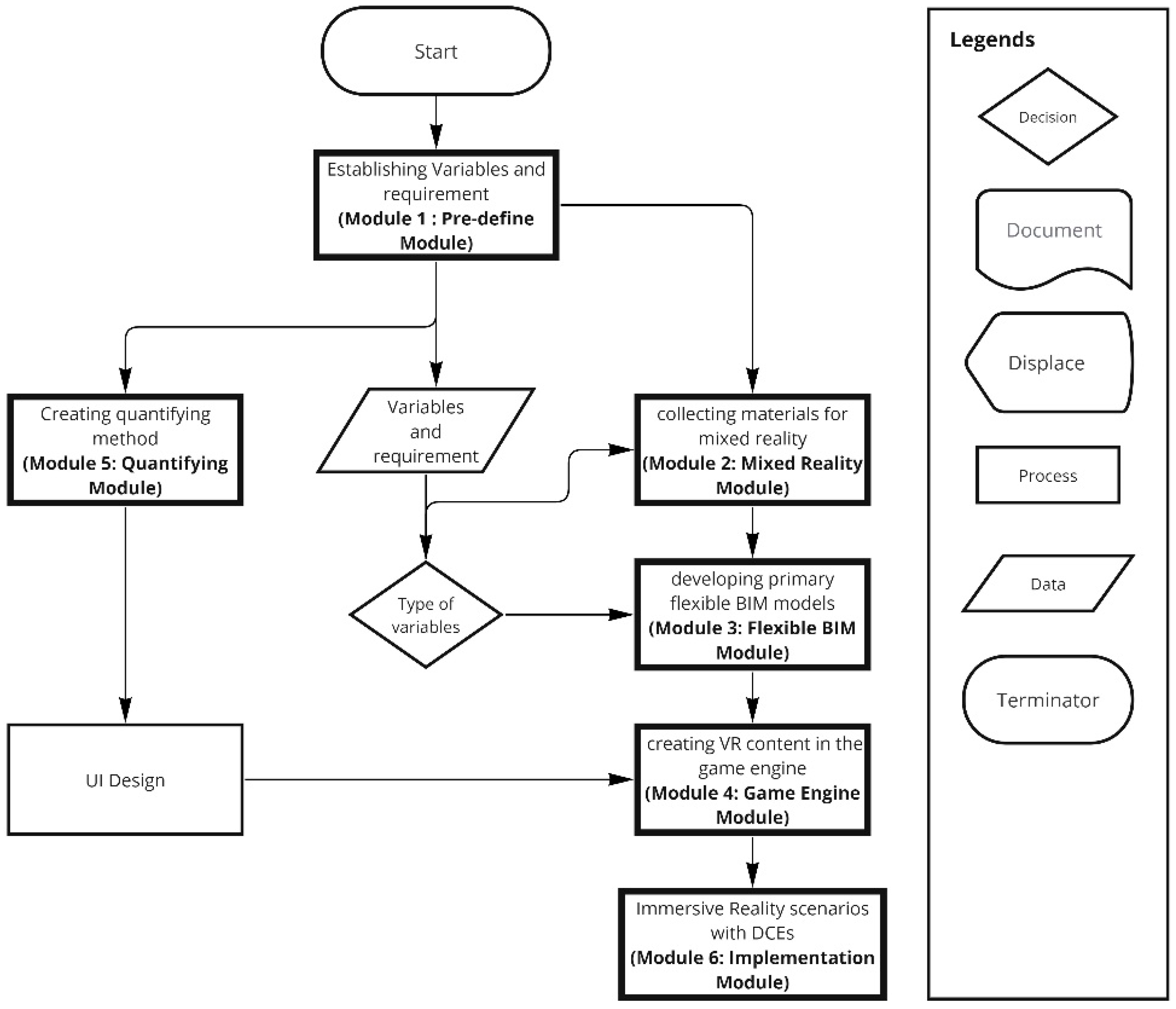
2.1. User-Centered Design Decision Support Approach Modules
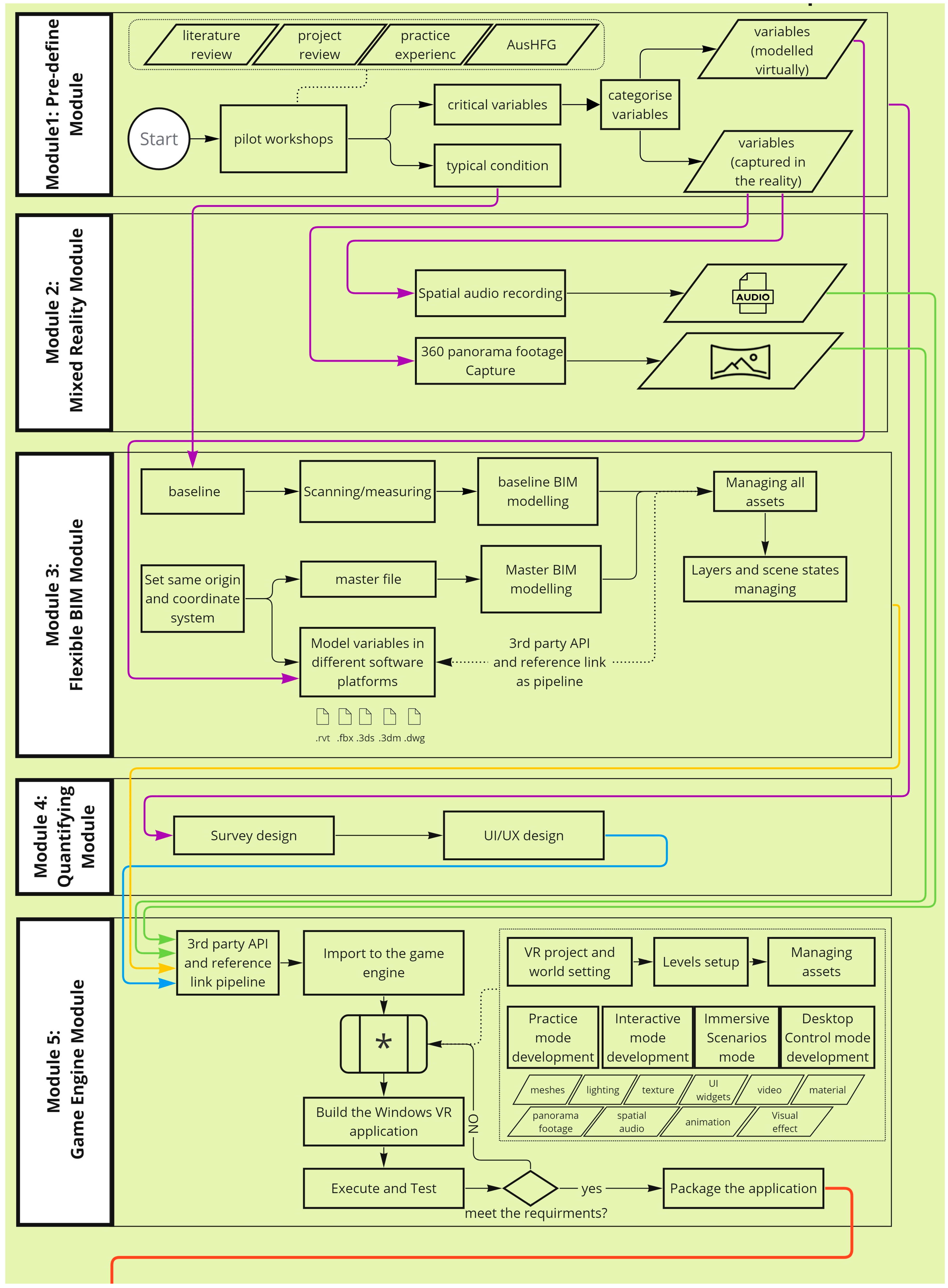
- Pre-define Module: Workshops with researchers, healthcare providers, clinicians, and design team to identify targeted variables and requirements for the specific healthcare environment.
- Mixed Reality Module: Develop an immersive VR environment including outdoor scenery, indoor physical environments, and spatial audio by using drone footage, ambisonics recordings, and the accurate modelling of the reference healthcare facility.
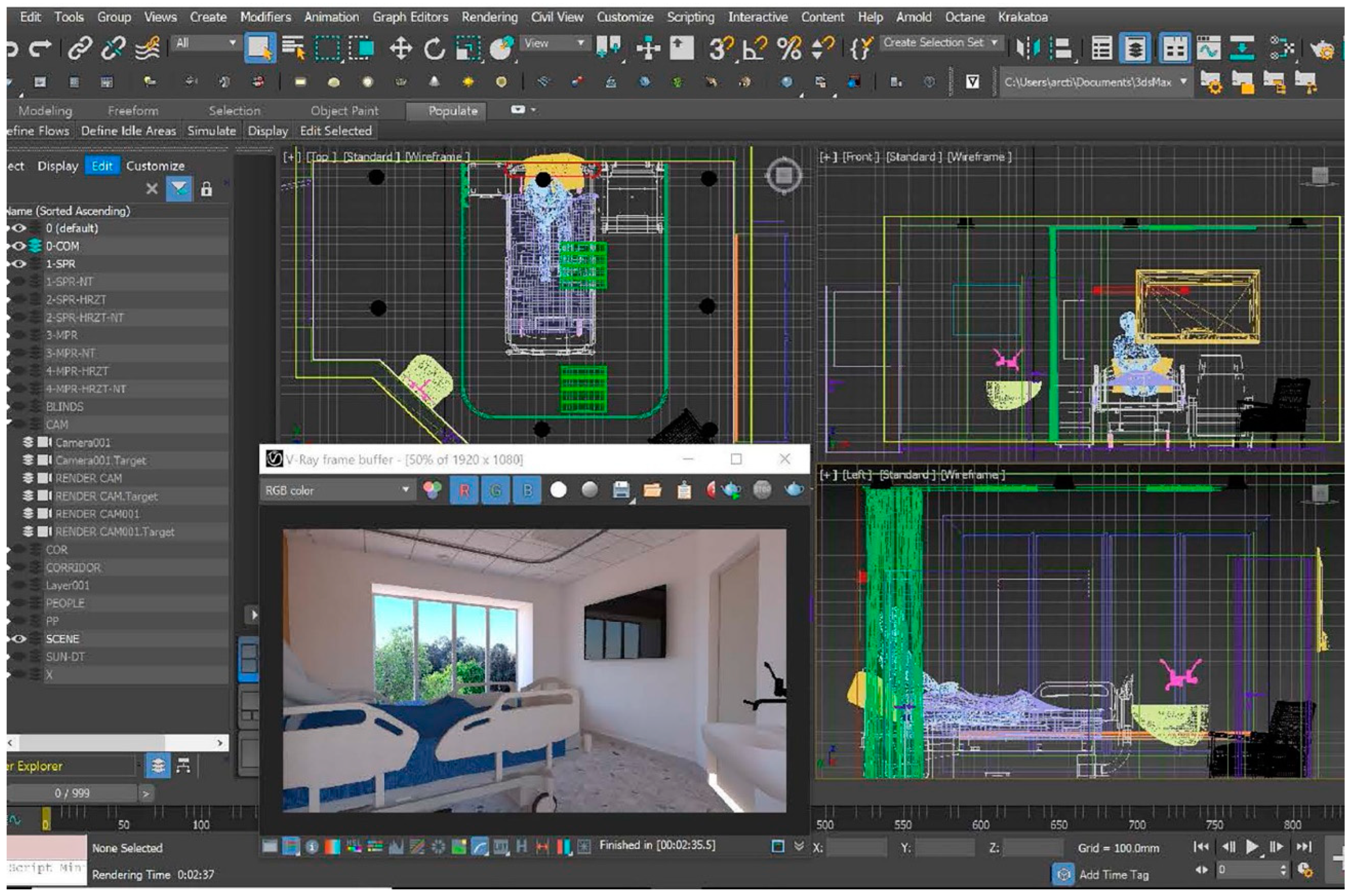
- Flexible BIM Module: This module centers on creating a ‘baseline’ model of the typical targeted healthcare environment, while also establishing a flexible, cross-platform building information modelling (BIM) management system. By leveraging procedural modelling, it facilitates efficient design modifications and comprehensive scenario testing.
- Quantifying Module: Design a method to measure and quantify participants’ perceptions using standardized response options with a user interface (UI) tailored to specific needs and abilities of the participants.
- Game Engine Module: Combine all assets in a game engine to develop a Windows VR application with four modes (practice mode, immersive scenario mode, interactive mode, and desktop control mode).
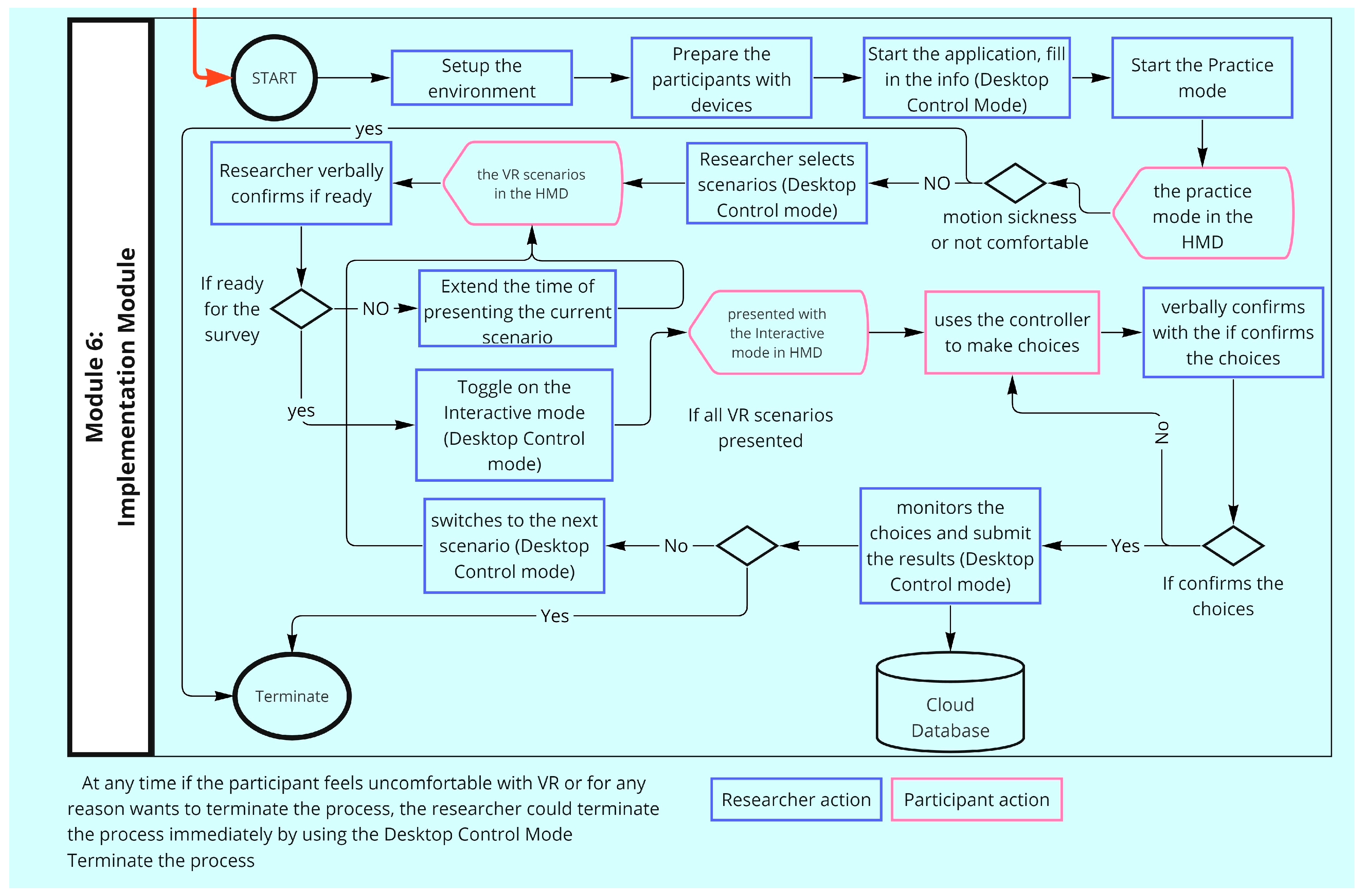
- Implementation Module: Elicit responses from target healthcare end-users. Establish a VR testing environment for the recruited participants, introduce them to the system through ‘practice mode’ and then immerse them in various ‘VR scenarios’ operated on a VR head-mounted display (HMD), while capturing their preferences and emotional responses through interactive response options, followed by semi-structured interviews.
2.2. Test Case Context—Stroke Rehabilitation Architecture
- Cognitive Challenges and Broad Applicability: Stroke survivors often face significant cognitive and physical challenges, making them a pertinent group to test the potential level of efficiency, feasibility, immersion, and presence in VR environments. Success in this group suggests a high likelihood of applicability to other populations with unique needs and abilities.
- Under-researched Area: Despite its importance, stroke rehabilitation facility design has not been extensively studied, presenting an opportunity to contribute to an area with substantial evidence gaps.
- Significance and Long-term Stay: Stroke rehabilitation is a critical and often long-term process. Stroke survivors’ prolonged stay in such facilities accentuates the importance of their perceptions of the space, making it a significant area to study.
- Global Relevance and Emerging Needs: Stroke is one of the leading causes of disability worldwide. With advancements in acute care leading to higher survival rates post-stroke, there is an increasing need for effective long-term rehabilitation [31]. Our study addresses this emerging need by focusing on the post-acute rehabilitation environment, aiming to fill the current research gaps identified by Ruby Lipson-Smith et al. [32] in rehabilitation architecture design.
2.3. Hardware and 2019 Costs
2.4. Personnel
3. Results
- Pre-define Module.
- 2.
- Mixed Reality Module—Developing Mixed Reality Using 360-Degree View.
- 3.
- Flexible BIM Module.
- 4.
- Quantifying Module.
- 5.
- Game Engine Module.
- 6.
- Implementation Module—Eliciting End-User Responses.
3.1. Participants
3.2. Scenario Sessions
3.3. Presence Feedback
3.4. Quantitative Analysis of Stroke Survivor Responses to Varied Physical Environments Using VR
4. Discussion
4.1. Novelty of the Method
4.2. Immersion and Presence
4.3. Feasibility
4.3.1. Financial Feasibility
4.3.2. Feasibility of Using VR with Vulnerable Group
4.3.3. Feasibility of Collecting Evidence to Inform Design Decisions
4.4. Limitations
4.5. Future Research Direction
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Day Scenarios | |
| #1 | Baseline Single Baseline single-patient room with low amount of greenery outlook, small horizontal room width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #2 | Wide Single Baseline single-patient room, with low amount of greenery outlook, large horizontal room width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #3 | Green-view Single Baseline single-patient room, with lots of greenery outlook, small horizontal room width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #4 | Wide Green-view Single Baseline single-patient room, with lots of greenery outlook, large horizontal room width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #5 | Baseline Multi Baseline multi-patient room, with low amount of greenery outlook, with other stroke patient present at their own bedside looking at iPad/book; small horizontal width; window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #6 | Wide Multi Baseline multi-patient room, with low amount of greenery outlook, with other stroke patient present at their own bedside looking at iPad/book; large horizontal width; window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #7 | Green-view Multi Baseline multi-patient room, with lots of greenery outlook, with other stroke patient present at their own bedside looking at iPad/book; small horizontal width; window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #8 | Wide Green-view Multi Baseline multi-patient room, with lots of greenery outlook, with other stroke patient present at their own bedside looking at iPad/book; large horizontal width; window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #9 | Social Single Baseline Single-patient room, with low amount of greenery outlook, small horizontal room width, social connectivity with own family present; participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #10 | Wide Social Single Baseline Single-patient room, with low amount of greenery outlook, large horizontal room width, social connectivity with own family present; participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #11 | Green-view Social Single Baseline Single-patient room, with lots of greenery outlook, small horizontal room width, social connectivity with own family present; participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #12 | Wide Green-view Social Single Baseline Single-patient room, with lots of greenery outlook, large horizontal room width, social connectivity with own family present; participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background |
| #13 | Social Multi Baseline multi-patient room, with low amount of greenery outlook, small horizontal room width, social connectivity with own family AND other patient family present; window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background (participants will be told that VR people represent THEIR family members) |
| #14 | Wide Social Multi Baseline multi-patient room, with low amount of greenery outlook, large horizontal room width, social connectivity with own family AND other patient family present; window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background (participants will be told that VR people represent THEIR family members) |
| #15 | Green-view Social Multi Baseline multi-patient room, with lots of greenery outlook, small horizontal room width, social connectivity with own family AND other patient family present; window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background (participants will be told that VR people represent THEIR family members) |
| #16 | Wide Green-view Social Multi Baseline multi-patient room, with lots of greenery outlook, large horizontal room width, social connectivity with own family AND other patient family present; window located on façade wall, ensuite on corridor wall, interior window with blind and door; non-meaningful hospital sounds in background (participants will be told that VR people represent THEIR family members) |
| Night Scenarios | |
| #1 | Baseline Single Baseline single-patient room with no greenery outlook, small horizontal width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn, external voices and noisy alarms in room. Low light conditions. |
| #2 | Wide Single Baseline single-patient room with no greenery outlook, large horizontal width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn, external voices and noisy alarms in room. Low light conditions. |
| #3 | Quiet Single Baseline single-patient room with no greenery outlook, small horizontal width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn, low ambient sounds in background. Low light conditions. |
| #4 | Wide Quiet Single Baseline single-patient room with no greenery outlook, large horizontal width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn, low ambient sounds in background. Low light conditions. |
| #5 | Baseline Multi Baseline multi-patient room, with no greenery outlook, small horizontal width, with other stroke patient present at their own bedside looking at iPad/book, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; external voices and noisy alarms in room. Low light conditions. |
| #6 | Wide Multi Baseline multi-patient room, with no greenery outlook, large horizontal width, with other stroke patient present at their own bedside looking at iPad/book, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; external voices and noisy alarms in room. Low light conditions. |
| #7 | Quiet Multi Baseline multi-patient room, with no greenery outlook, small horizontal width, with other stroke patient present at their own bedside looking at iPad/book, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; low ambient sounds in background. Low light conditions. |
| #8 | Wide Quite Multi Baseline multi-patient room, with no greenery outlook, large horizontal width, with other stroke patient present at their own bedside looking at iPad/book, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; low ambient sounds in background. Low light conditions. |
| #9 | Social Single Baseline single-patient room with no greenery outlook, small horizontal width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; external voices and noisy alarms in room. Low light conditions. More social connectivity with staff coming into room. |
| #10 | Wide Social Single Baseline single-patient room with no greenery outlook, large horizontal width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; external voices and noisy alarms in room. Low light conditions. More social connectivity with staff coming into room. |
| #11 | Quiet Social Single Baseline single-patient room with no greenery outlook, small horizontal width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; low ambient sounds in background. Low light conditions. More social connectivity with staff coming into room. |
| #12 | Wide Social Single Baseline single-patient room with no greenery outlook, large horizontal width, participant bed only, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; low ambient sounds in background. Low light conditions. More social connectivity with staff coming into room. |
| #13 | Social Multi Baseline multi-patient room, with no greenery outlook, small horizontal width, with other stroke patient present at their own bedside looking at iPad/book, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; external voices and noisy alarms in room. More social connectivity with staff coming into room. Low light conditions. |
| #14 | Wide Social Multi Baseline multi-patient room, with no greenery outlook, large horizontal width, with other stroke patient present at their own bedside looking at iPad/book, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn, external voices and noisy alarms in room. More social connectivity with staff coming into room. Low light conditions. |
| #15 | Quiet Social Multi Baseline multi-patient room, with no greenery outlook, small horizontal width, with other stroke patient present at their own bedside looking at iPad/book, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; low ambient sounds in background. More social connectivity with staff coming into room. Low light conditions. |
| #16 | Wide Quiet Social Multi Baseline multi-patient room, with no greenery outlook, large horizontal width, with other stroke patient present at their own bedside looking at iPad/book, window located on façade wall, ensuite on corridor wall, interior window with blind and door drawn; low ambient sounds in background. More social connectivity with staff coming into room. Low light conditions. |
| All other physical factors, i.e., luminosity/illuminance, temp (N/A), light fixtures, window size, and number and type of furnishings were constant (baseline SR (single patient room), baseline MPR (multi-patient room)). | |
References
- Ulrich, R.; Quan, X.; Zimring, C.; Joseph, A.; Choudbary, R. The Role of the Physical Environment in the Hospital of the 21st Century: A Once-in-a-Lifetime Opportunity; The Center for Health Design: Concord, CA, USA, 2004; p. 69. [Google Scholar]
- Chias, P.; Abad, T.; de-Miguel-Sánchez, M.; Gonzalez-Fierro, G.; Valiente, E. 3D Modelling and Virtual Reality Applied to Complex Architectures: An Application to Hospitals’ Design. ISPRS—Int. Arch. Photogramm. Remote Sens. Spat. Inf. Sci. 2019, 42, 255–260. [Google Scholar] [CrossRef]
- Durham, J.; Kenyon, A. Mock-Ups: Using Experiential Simulation Models in the Healthcare Design Process. HERD Health Environ. Res. Des. J. 2019, 12, 11–20. [Google Scholar] [CrossRef]
- Phiri, M.; Chen, B. Sustainability and Evidence-Based Design in the Healthcare Estate; SpringerBriefs in Applied Sciences and Technology; Springer: Berlin/Heidelberg, Germany, 2014; ISBN 978-3-642-39202-3. [Google Scholar]
- Ulrich, R.S.; Berry, L.L.; Quan, X.; Parish, J.T. A Conceptual Framework for the Domain of Evidence-Based Design. HERD Health Environ. Res. Des. J. 2010, 4, 95–114. [Google Scholar] [CrossRef]
- Halawa, F.; Madathil, S.C.; Gittler, A.; Khasawneh, M.T. Advancing Evidence-Based Healthcare Facility Design: A Systematic Literature Review. Health Care Manag. Sci. 2020, 23, 453–480. [Google Scholar] [CrossRef] [PubMed]
- Zimring, C.; Denham, M.; Jacob, J.; Cowan, D.; Do, E.; Hall, K.; Kamerow, D.; Kasalı, A.; Steinberg, J. Evidence-Based Design of Healthcare Facilities: Opportunities for Research and Practice in Infection Prevention. Infect. Control. Hosp. Epidemiol. Off. J. Soc. Hosp. Epidemiol. Am. 2013, 34, 514–516. [Google Scholar] [CrossRef] [PubMed]
- Thórarinsdóttir, K.; Kristjánsson, K. Patients’ Perspectives on Person-Centred Participation in Healthcare: A Framework Analysis. Nurs. Ethics 2014, 21, 129–147. [Google Scholar] [CrossRef]
- Kwame, A.; Petrucka, P.M. A Literature-Based Study of Patient-Centered Care and Communication in Nurse-Patient Interactions: Barriers, Facilitators, and the Way Forward. BMC Nurs. 2021, 20, 158. [Google Scholar] [CrossRef]
- Copeland, D.; Chambers, M. Effects of Unit Design on Acute Care Nurses’ Walking Distances, Energy Expenditure, and Job Satisfaction: A Pre–Post Relocation Study. HERD Health Environ. Res. Des. J. 2017, 10, 22–36. [Google Scholar] [CrossRef]
- Freihoefer, K.; Kaiser, L.; Vonasek, D.; Bayramzadeh, S. Setting the Stage: A Comparative Analysis of an Onstage/Offstage and a Linear Clinic Modules. HERD Health Environ. Res. Des. J. 2018, 11, 89–103. [Google Scholar] [CrossRef]
- Das, A.; Brunsgaard, C.; Madsen, C.B. Understanding the AR-VR Based Architectural Design Workflow among Selected Danish Architecture Practices. In Proceedings of the International Conference on Education and Research in Computer Aided Architectural Design in Europe, Ghent, Belgium, 13–16 September 2022; pp. 381–388. [Google Scholar]
- Lu, J.; Fu, C.; Zhou, T.; Xie, J.; Loo, Y.M. A Review of Physical and Digital Mock-Up Applications in Healthcare Building Development. Buildings 2022, 12, 745. [Google Scholar] [CrossRef]
- Cai, H.; Zimring, C. Cultural Impacts on Nursing Unit Design: A Comparative Study on Chinese Nursing Unit Typologies and Their, U.S. Counterparts Using Space Syntax. Environ. Plan. B Urban Anal. City Sci. 2019, 46, 573–594. [Google Scholar] [CrossRef]
- Haq, S.; Luo, Y. Space Syntax in Healthcare Facilities Research: A Review. HERD Health Environ. Res. Des. J. 2012, 5, 98–117. [Google Scholar] [CrossRef]
- Dunston, P.S.; Arns, L.L.; McGlothlin, J.D. Virtual Reality Mock-Ups for Healthcare Facility Design and a Model for Technology Hub Collaboration. J. Build. Perform. Simul. 2010, 3, 185–195. [Google Scholar] [CrossRef]
- Shultz, J.; Jha, R. Using Virtual Reality (VR) Mock-Ups for Evidence-Based Healthcare Facility Design Decisions. Int. J. Environ. Res. Public Health 2021, 18, 11250. [Google Scholar] [CrossRef]
- Gosavi, A.; Cudney, E.; Murray, S.; Masek, C. Analysis of Clinic Layouts and Patient-Centered Procedural Innovations Using Discrete-Event Simulation. Eng. Manag. J. 2016, 28, 134–144. [Google Scholar] [CrossRef]
- Kasali, A.; Nersessian, N.J. Architects in Interdisciplinary Contexts: Representational Practices in Healthcare Design. Des. Stud. 2015, 41, 205–223. [Google Scholar] [CrossRef]
- Loomis, J.M.; Blascovich, J.J.; Beall, A.C. Immersive Virtual Environment Technology as a Basic Research Tool in Psychology. Behav. Res. Methods Instrum. Comput. 1999, 31, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Frost, P.; Warren, P. Virtual Reality Used in a Collaborative Architectural Design Process. In Proceedings of the 2000 IEEE Conference on Information Visualization. An International Conference on Computer Visualization and Graphics, London, UK, 19–21 July 2000; pp. 568–573. [Google Scholar]
- Jouppila, T.; Tiainen, T. Nurses’ Participation in the Design of an Intensive Care Unit: The Use of Virtual Mock-Ups. HERD Health Environ. Res. Des. J. 2021, 14, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Liddicoat, S. Mental Health Facility Codesign: A New Research Method for Integrating the Service User Voice in Design Processes Using Virtual Reality. Gen. Psychiatr. 2019, 32, e100061. [Google Scholar] [CrossRef] [PubMed]
- Charles, D.; Holmes, D.; Charles, T.; McDonough, S. Virtual Reality Design for Stroke Rehabilitation. Adv. Exp. Med. Biol. 2020, 6, 53–87. [Google Scholar] [CrossRef]
- Bouška, R. Evaluation of Maturity of BIM Tools across Different Software Platforms. Procedia Eng. 2016, 164, 481–486. [Google Scholar] [CrossRef]
- Chen, L. Agent-Based Modeling in Urban and Architectural Research: A Brief Literature Review. Front. Archit. Res. 2012, 1, 166–177. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Chen, Y.-P.; Yien, H.-W.; Huang, C.-Y.; Su, Y.-C. Integrated BIM, Game Engine and VR Technologies for Healthcare Design: A Case Study in Cancer Hospital. Adv. Eng. Inform. 2018, 36, 130–145. [Google Scholar] [CrossRef]
- Borkowski, A.S. A Literature Review of BIM Definitions: Narrow and Broad Views. Technologies 2023, 11, 176. [Google Scholar] [CrossRef]
- Chapin, N. Flowcharting with the ANSI Standard: A Tutorial. ACM Comput. Surv. 1970, 2, 119–146. [Google Scholar] [CrossRef]
- White, M.; Langenheim, N.M.; Yang, T.; Paay, J. Informing Streetscape Design with Citizen Perceptions of Safety and Place: An Immersive Virtual Environment e-Participation Method. Int. J. Environ. Res. Public Health 2023, 20, 1341. [Google Scholar] [CrossRef]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke Rehabilitation. Lancet 2011, 377, 1693–1702. [Google Scholar] [CrossRef]
- Lipson-Smith, R.; Pflaumer, L.; Elf, M.; Blaschke, S.-M.; Davis, A.; White, M.; Zeeman, H.; Bernhardt, J. Built Environments for Inpatient Stroke Rehabilitation Services and Care: A Systematic Literature Review. BMJ Open 2021, 11, e050247. [Google Scholar] [CrossRef]
- Shannon, M. Exploring the Physical Design of Hospital Interiors for People with Stroke; University of Melbourne: Melbourne, VIC, Australia, 2022. [Google Scholar]
- Huisman, E.R.C.M.; Morales, E.; van Hoof, J.; Kort, H.S.M. Healing Environment: A Review of the Impact of Physical Environmental Factors on Users. Build. Environ. 2012, 58, 70–80. [Google Scholar] [CrossRef]
- Jue, K.; Nathan-Roberts, D. How Noise Affects Patients in Hospitals. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting, Los Angeles, CA, USA, 27–31 October 2019; Volume 63, pp. 1510–1514. [Google Scholar] [CrossRef]
- Dlesk, A.; Vach, K.; Šedina, J.; Pavelka, K. Comparison of Leica Blk360 and Leica Blk2go on Chosen Test Objects. In Proceedings of the International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences, Prague, Czech Republic, 7–8 February 2022; Copernicus GmbH: Göttingen, Germany; Volume XLVI-5-W1-2022, pp. 77–82. [Google Scholar]
- Watson, D.; Tellegen, A. Toward a Consensual Structure of Mood. Psychol. Bull. 1985, 98, 219–235. [Google Scholar] [CrossRef]
- Desmet, P.; Vastenburg, M.; Romero, N. Pick-A-Mood Manual: Pictorial Self-Report Scale for Measuring Mood States; Delft University of Technology: Delft, Netherlands, 2016. [Google Scholar]
- Jimenez, J.C.; Romero, N.; Keyson, D. Capturing Patients’ Daily Life Experiences after Total Hip Replacement. In Proceedings of the 5th International ICST Conference on Pervasive Computing Technologies for Healthcare, Dublin, Republic of Ireland, 23–26 May 2011. [Google Scholar]
- Vastenburg, M.H.; Romero Herrera, N.A. Experience Tags: Enriching Sensor Data in an Awareness Display for Family Caregivers. In Ambient Intelligence; Keyson, D.V., Maher, M.L., Streitz, N., Cheok, A., Augusto, J.C., Wichert, R., Englebienne, G., Aghajan, H., Kröse, B.J.A., Eds.; Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2011; Volume 7040, pp. 285–289. ISBN 978-3-642-25166-5. [Google Scholar]
- Arruda, J.E.; Stern, R.A.; Somerville, J.A. Measurement of Mood States in Stroke Patients: Validation of the Visual Analog Mood Scales. Arch. Phys. Med. Rehabil. 1999, 80, 676–680. [Google Scholar] [CrossRef]
- Caixeta, M.C.B.F.; Fabricio, M.M. Physical-Digital Model for Co-Design in Healthcare Buildings. J. Build. Eng. 2021, 34, 101900. [Google Scholar] [CrossRef]
- Castronovo, F.; Nikolic, D.; Liu, Y.; Messner, J. An Evaluation of Immersive Virtual Reality Systems for Design Reviews. In Proceedings of the 13th International Conference on Construction Applications of Virtual Reality, London, UK, 30–31 October 2013. [Google Scholar]
- Kasali, A.; Nersessian, N.J.; Zimring, C.M. Making Evidence Visible: Using Mock-Ups in Healthcare Design. ARCC Conf. Repos. 2013, 8. [Google Scholar]
- Kalantari, S.; Xu, T.B.; Mostafavi, A.; Lee, A.; Barankevich, R.; Boot, W.; Czaja, S. Using a Nature-Based Virtual Reality Environment for Improving Mood States and Cognitive Engagement in Older Adults: A Mixed-Method Feasibility Study. Innov. Aging 2022, 6, igac015. [Google Scholar] [CrossRef] [PubMed]
- Qi, F.; Lu, Z.; Chen, Y. Investigating the Influences of Healthcare Facility Features on Wayfinding Performance and Associated Stress Using Virtual Reality. HERD Health Environ. Res. Des. J. 2022, 15, 131–151. [Google Scholar] [CrossRef] [PubMed]
- Wingler, D.; Machry, H.; Bayramzadeh, S.; Joseph, A.; Allison, D. Comparing the Effectiveness of Four Different Design Media in Communicating Desired Performance Outcomes with Clinical End Users. HERD Health Environ. Res. Des. J. 2019, 12, 87–99. [Google Scholar] [CrossRef]
- Lipson-Smith, R.; Churilov, L.; Newton, C.; Zeeman, H.; Bernhardt, J. A Framework for Designing Inpatient Stroke Rehabilitation Facilities: A New Approach Using Interdisciplinary Value-Focused Thinking. HERD Health Environ. Res. Des. J. 2019, 12, 142–158. [Google Scholar] [CrossRef]
- Ulrich, R.S. View Through a Window May Influence Recovery from Surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef]




| Equipment | Model/Specification | Price (AUD) | Date of Price Check |
|---|---|---|---|
| Head-mounted headset | HTC VIVE with controllers | 900 | 19 November |
| Headphones | Sennheiser HD 500A | 165 | 19 November |
| Laptop | NVIDIA GeForce GTX 1080 | 1399 | 19 November |
| Drone | DJI Mavic Pro | 820 | 19 November |
| Handy Recorder | ZOOM H2n | 299 | 19 November |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, T.; White, M.; Lipson-Smith, R.; Shannon, M.M.; Latifi, M. Design Decision Support for Healthcare Architecture: A VR-Integrated Approach for Measuring User Perception. Buildings 2024, 14, 797. https://doi.org/10.3390/buildings14030797
Yang T, White M, Lipson-Smith R, Shannon MM, Latifi M. Design Decision Support for Healthcare Architecture: A VR-Integrated Approach for Measuring User Perception. Buildings. 2024; 14(3):797. https://doi.org/10.3390/buildings14030797
Chicago/Turabian StyleYang, Tianyi, Marcus White, Ruby Lipson-Smith, Michelle M. Shannon, and Mehrnoush Latifi. 2024. "Design Decision Support for Healthcare Architecture: A VR-Integrated Approach for Measuring User Perception" Buildings 14, no. 3: 797. https://doi.org/10.3390/buildings14030797
APA StyleYang, T., White, M., Lipson-Smith, R., Shannon, M. M., & Latifi, M. (2024). Design Decision Support for Healthcare Architecture: A VR-Integrated Approach for Measuring User Perception. Buildings, 14(3), 797. https://doi.org/10.3390/buildings14030797








